Abstract
Recurrent laryngeal nerve (RLN) injury is an intractable complication of thyroidectomy. Intraoperative nerve monitoring (IONM) was designed to prevent RLN injury. However, the results concerning the protective effect of IONM on RLN injury are still controversial. We searched all eligible databases from 1980 to 2017. Meta-analysis was performed to evaluate the effect of IONM on RLN injury. Sensitivity analysis was also conducted to check the stability of our results. There were 34 studies included in the analysis. Overall analysis found a significant decrease in total injury (RR = 0.68, 95%CI: 0.55 to 0.83), transient injury (RR = 0.71, 95%CI: 0.57 to 0.88), and permanent injury (RD = −0.0026, 95%CI: −0.0039 to −0.0012) with IONM. Subgroup analysis found IONM played a preventive role of total, transient and permanent injury in patients undergoing bilateral thyroidectomy. IONM also reduced the incidence of total and transient injury for malignancy cases. Operations with IONM were associated with fewer total and transient RLN injuries in operation volume < 300 NARs per year and fewer total and permanent RLN injuries in operation volume ≥ 300 NARs per year. The application of IONM could reduce the RLN injury of thyroidectomy. Particularly, we recommend routine IONM for use in bilateral operations and malignancy operations.
Introduction
Recurrent laryngeal nerve (RLN) injury is the most severe complication of thyroid surgery, leading to transient or permanent voice changes, which is one of the most common causes for medical litigation1. According to reported data, the incidence of transient RLN injury and permanent RLN injury in thyroidectomy are 2–11% and 0.6–1.6%, respectively2–4. In certain situations, the risk of RLN injury is relatively high, including thyroid surgery for malignant tumors, history of neck operation, and surgery of toxic goiter or substernal goiter5,6.
Routine visual identification of RLN is applied in thyroid surgery to prevent RLN injury, which serves as a conventional measure to reduce vocal cord paralysis. Dionigi et al. found that the causes of RLN injury included transection, clamping, ligatures, suction, traction, thermal injuries and physical compression7. Intraoperative nerve monitoring systems (IONM) use the electromyographic signal of vocal muscle movement to reflect the function of the RLN8,9. IONM increases the identification rate of RLN, reduces the time of IONM identification and predicts the postoperative function of the vocal cords10,11. IONM can be divided into 2 generations, non-continuous intraoperative nerve monitoring (NCIONM) and continuous intraoperative nerve monitoring (CIONM). NCIONM is still the most common method of nerve monitoring, and CIONM is a recent surgical trend that could prevent RLN injury though real-time monitoring.
Although IONM is designed to reduce the incidence of RLN injury, the effect of IONM on RLN injury prevention in thyroid surgery is still controversial12,13. Some results found that IONM could reduce transient RLN injury, while other results revealed non-significant help of IONM in RLN injury prevention4,14,15. Several meta-analyses have been conducted to discuss this topic12,13,16–18. Most of these studies found that IONM was not superior to visual identification in preventing permanent RLN injury12,18. Some results indicated that IONM could decrease RLN injury incidence in high risk thyroid surgery, particularly in cancer operations or in those with a previous history of neck operation17. For operative sites, incidence of bilateral injury under IONM was relatively higher (0.2%), and staged thyroidectomy was recommended when one-side RLN injury occurred to prevent further bilateral RLN injury19,20.
During the last 2 years, many large clinical trials emerged on this topic, which made it necessary to update the data for further conclusion10,11,21–26. Considering the existing controversial results and new data, we conducted this meta-analysis to clarify the effects of IONM in thyroidectomy. Subgroup analysis was performed to identify the effects of IONM in bilateral operation, malignancy operation, reoperation group and operation volume.
Materials and Methods
Search strategy and selection criteria
We performed a comprehensive literature search in MEDLINE (PubMed), BIOSIS Previews (ISI Web of Knowledge) and Cochrane library from January 1980 to July 2017. We also manually added relevant articles by reviewing the references. Search terms included: “Neuromonitoring” or “nerve monitoring”, “thyroidectomy” or “thyroid surgery”, and “recurrent laryngeal nerve” or “RLN”. Studies included were confined to randomized controlled trials, case control studies and cohort studies, with convertible effects data of IONM in thyroidectomy. If there were several papers extracting from the same population, we would only include the most recent publication. We used the criterion of 6 months to distinguish transient RLN injury from permanent RLN injury, which was consistent with relevant studies10,27.
Data extraction and quality assessment
Data were extracted by two authors (BL Bai and WZ Chen) independently. Detailed information was recorded on first author, year of publication, title, location, study type, diagnosis, inclusion and exclusion criteria, allocation method, study duration, device used, outcome measurement, definition of permanent injury, number of case and control groups, the event of transient and permanent RLN injury, the population type, multicenter research or not, main conclusion and Newcastle-Ottawa Scale (NOS) score. Nerve at risk (NAR) was calculated based on number of lobectomy (1 NAR for each side), subtotal thyroidectomy (2 NARs) and total thyroidectomy (2 NARs). In the section of operation volume, we omitted multicenter research studies for the unavailability of hospital volume data and would discuss the effects of IONM under open surgical operation because of insufficient sample size of endoscopic surgery. The Newcastle-Ottawa Scale for Quality was used to assess the included cohort studies28.
Statistical Methods
Meta-analysis was performed under R environment 3.4.1 through meta package 4.8–329. According to the Cochrane Collaboration, risk ratio (RR), risk difference (RD) and confidence interval (CI) were estimated from the median of the posterior distribution and calculated by the random-effects model with inverse variance weight30–32. If zero events occurred in both experimental and control group, the pooled RD estimates and 95% CIs were applied. Otherwise, RR was applied. RR below one or RD below zero indicated a benefit of the experimental intervention. We estimated 95%CI from the 2.5th and 97.5th percentiles of the posterior distribution, and calculated two-sided p values from the posterior distribution. If the 95%CI did not contain the valid value 1, the result was considered to have significant difference. Publication bias was assessed using Begg’s test and Egger’s regression asymmetry test33. The heterogeneity between trials was estimated from the median between-trial variance (τ²) observed in the posterior.
Availability of supporting data
All data are fully available without restriction.
Results
Description of studies
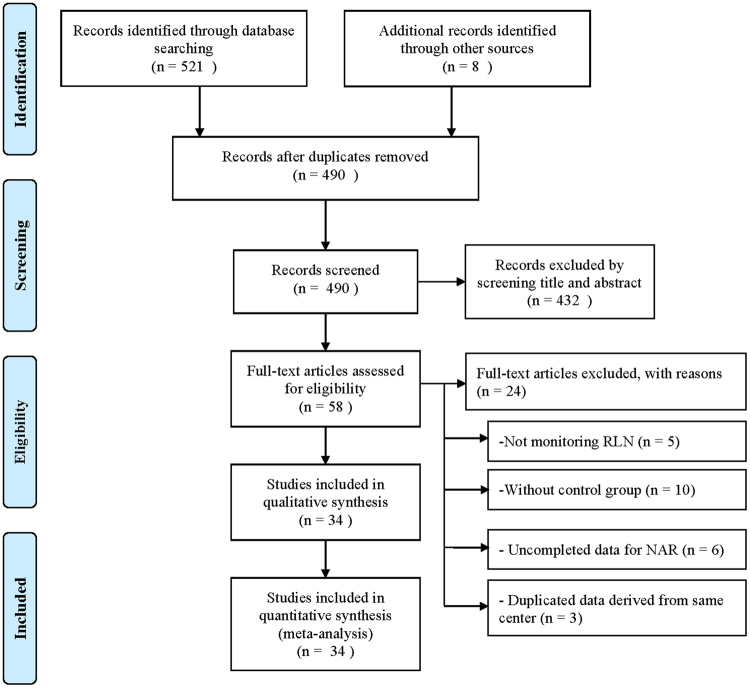
A total of 529 articles were identified through literature research. After duplicates were removed, 490 articles were included for screening. Among these, 58 eligible full-text articles were selected after carefully checking the titles and abstracts. However, we excluded 24 from these 58 articles because of monitoring other nerve (5 articles), no control group (10 articles), incomplete data for NAR (6 articles), or duplicated data derived from same center (3 articles) (Fig. 1)34. Finally, 34 articles were included for systematical review and meta-analysis2–6,8,10,11,14,15,21–26,35–52. Details on first author, year of publication, title, location, study type, allocation method, study duration, device used, outcome measurement and definition of permanent injury were recorded (Table 1). There were 3 randomized controlled trials40,42,52 and 31 non-randomized trials2–6,8,10,11,14,15,21–26,35–39,41,43–51 included in our study. The number of case and control groups and the event of total, transient and permanent RLN injury were also recorded (Appendix Table 1). The NOS of included research studies ranged from 6 to 9, suggesting an acceptable quality of the studies.
Figure 1.
Flow diagram of study selection according to PRISMA statement34. Abbreviation: RLN = recurrent laryngeal nerve; NAR = nerves at risk.
Table 1.
Main characteristic of included studies.
| Author | Year | Location | Study type | Allocation method | Study duration | Device used | Outcome measurement | Permanent injury definition |
|---|---|---|---|---|---|---|---|---|
| Brauckhoff51 | 2002 | Germany | NCT | Non-IONM:1995–1997; IONM:1998–2001 | 1995–2001 | NS | Laryngoscopy | NS |
| Thomusch2 | 2002 | Germany | NCT | NS | January 1 - December 31, 1998 | Neurosign 100 | Laryngoscopy | 6 months |
| Dralle5 | 2004 | Germany | NCT | Choice of surgeon and Device availability | January 1, 1998 - January 15, 2001 | Neurosign 100 | Laryngoscopy | 6 months |
| Robertson3 | 2004 | USA | NCT | NS | April 1999 - December 2002 | NIM-2.0 | Laryngoscopy | NS |
| Yarbrough4 | 2004 | USA | NCT | Non-IONM:1998–2000; IONM:2000–2003 | October 1998 - January 2003 | NS | Laryngoscopy | NS |
| Witt35 | 2005 | USA | NCT | NS | 1998–2003 | NIM | Laryngoscopy | 12 months |
| Chan6 | 2006 | Hong Kong | NCT | Choice of surgeon and Device availability | January 2002 - August 2005 | Neurosign 100 | Laryngoscopy | 12 months |
| Netto36 | 2007 | Brazil | NCT | IONM: November 2003 - January 2006; Non-IONM: May 2003 - September 2003 | November 2003 and January 2006 | NIM-2.0 | Laryngoscopy | 3 months |
| Shindo37 | 2007 | USA | NCT | Non-IONM:1998–2002; IONM:2002–2005 | 1998–2005 | NS | Laryngoscopy | 6 months |
| Terris38 | 2007 | USA | NCT | NS | January of 2004 - November of 2006 | NIM-2.0 | Laryngoscopy | 6 months |
| Atallah39 | 2009 | France | NCT | Non-IONM: November 2003-December 2005; IONM: December 2005-July 2007 | November 2003 - July 2007 | NIM-2.0 | Laryngoscopy | 12 months |
| Barczynski52 | 2009 | Poland | RCT | Randomized | January 2006 - June 2007 | Neurosign 100 | Laryngoscopy | 12 months |
| Dionigi40 | 2009 | Italy | RCT | Randomized | 2007 | NIM-2.0 | Laryngoscopy | NS |
| Frattini41 | 2010 | Italy | NCT | NS | NS | NIM-2.0 | Laryngoscopy | 12 months |
| Sari42 | 2010 | Turkey | RCT | Randomized | September 2007 - September 2009 | NIM | Laryngoscopy | 12 months |
| Barczynski43 | 2011 | Poland | NCT | Non-IONM:2003–2004;IONM:2005–2009 | January 2003 - June 2009 | Neurosign 100 NIM-2.0 | Laryngoscopy | 12 months |
| Alesina8 | 2012 | Germany | NCT | NS | November 1999 - April 2011 | Neurosign NIM-3.0 | Laryngoscopy | 6 months |
| Gremillion44 | 2012 | USA | NCT | NS | 2007–2010 | NS | NS | NS |
| Chuang45 | 2013 | Taiwan | NCT | NS | 2001–2010 | NIM | NS | NS |
| Prokopakis46 | 2013 | Greece | NCT | Incidentally | 2004–2011 | NIM | Laryngoscopy | 4 months |
| Alesina47 | 2014 | Germany | NCT | NS | January 2005 - December 2012 | Neurosign NIM-3.0 | Laryngoscopy | 6 months |
| Barczynski14 | 2014 | Poland | NCT | NS | 1993–2012 | Neurosign 100 NIM 2.0/3.0 | Laryngoscopy | 12 months |
| De Falco48 | 2014 | Italy | NCT | Non-IONM:1 October 2009–31 July 2010; IONM:1 September 2010–31 October 2011 | 1 October 2009–31 October 2011 | NS | Laryngoscopy | 6 months |
| Sanguinetti49 | 2014 | Italy | NCT | NS | 2012 | NS | Laryngoscopy | NS |
| de Danschutter50 | 2015 | Netherlands | NCT | Non-IONM: September 2009 - July 2010; IONM: July 2010 - October 2012 | September 2009 - October 2012 | NIM-3.0 | Laryngoscopy | 12 months |
| Page15 | 2015 | France | NCT | Non-IONM:2001–2004;IONM: 2005–2010 | January 2001 - January 2010 | Neurosign 400 | Laryngoscopy | 12 months |
| Anuwong10 | 2016 | Italy | NCT | Non-IONM: 1995–2005; IONM: 2006–2013 | January 2002 - December 2014 | NIM-2.0/3.0 | Laryngoscopy | 12 months |
| Brajcich21 | 2016 | USA | NCT | Non-IONM:2009–2013; IONM:2013–2015 | 2009–2015 | NIM-3.0 | Laryngoscopy | 12 months |
| Calo22 | 2016 | Italy | NCT | Device availability | June 2007 - December 2013 | NIM-2.0/3.0 | Laryngoscopy | 12 months |
| Hei11 | 2016 | China | NCT | Randomly allocated | October 2009 - August 2011 | NIM-2.0 | Laryngoscopy | 6 months |
| Lv23 | 2016 | China | NCT | Non-IONM:2010–2012; IONM:2012–2014 | January 2010 - January 2014 | NIM-3.0 | Laryngoscopy | 6 months |
| Vasileiadis24 | 2016 | Greece | NCT | Device availability | January 2002 - December 2012 | NIM-2.0 | Laryngoscopy | 12 months |
| Xie25 | 2016 | China | NCT | NS | January 2012 - September 2014 | NIM-3.0 | Laryngoscopy | 6 months |
| Kai26 | 2017 | China | NCT | NS | 1 January 2013–30 June 2016 | NIM-3.0 | Laryngoscopy | 6 months |
Abbreviation: NCT, non-randomized comparative trial; RCT, randomized controlled trial; NS, not stated.
There were mainly three types of devices used in the studies, including Neurosign 100, NIM 2.0 and NIM 3.0. Except for some papers that had not declared the outcome measurement, the majority of the included studies applied laryngoscopy to check the movement of vocal cords. 29 studies were conducted under general operation, 3 studies were based on minimally invasive thyroidectomy, and the other 2 studies were based on total endoscopic thyroidectomy (Appendix Table 2). Most of the studies were single-center trials except for 2 multi-center trials. In subgroup analysis, we focused on major influence factors, such as bilateral operation, malignancy, reoperation and operation volume (Appendix Table 3).
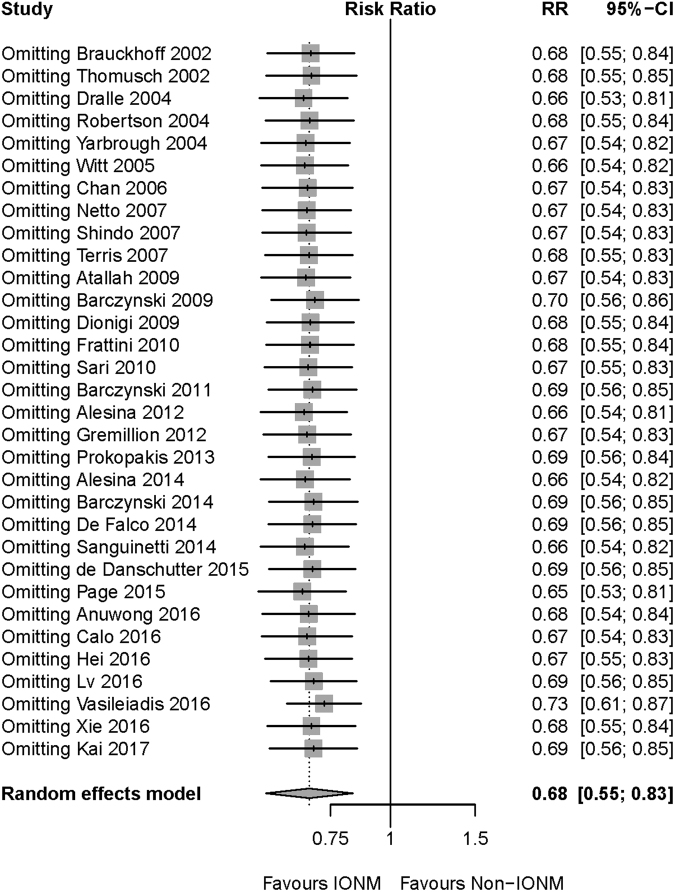
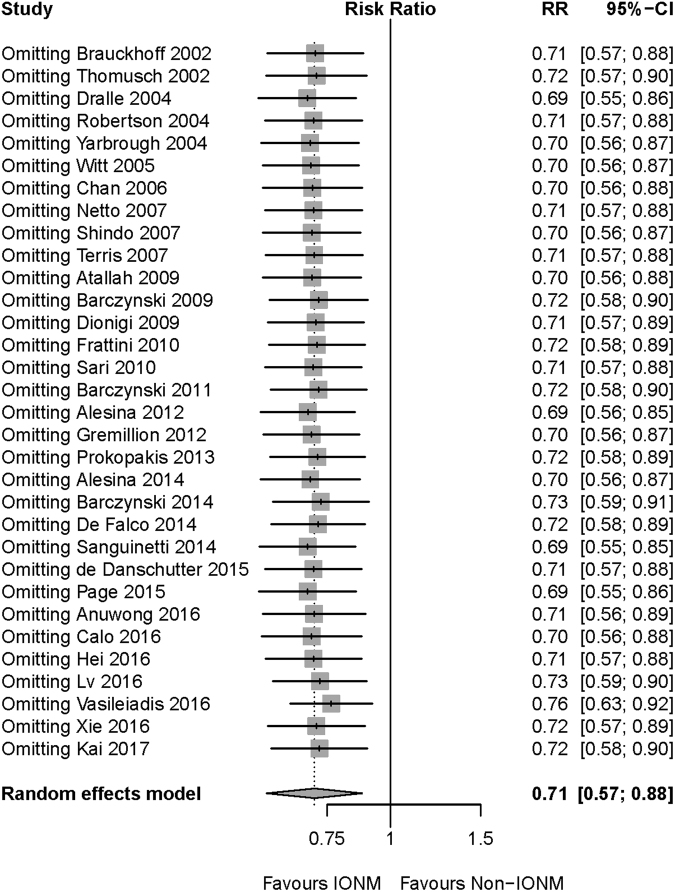
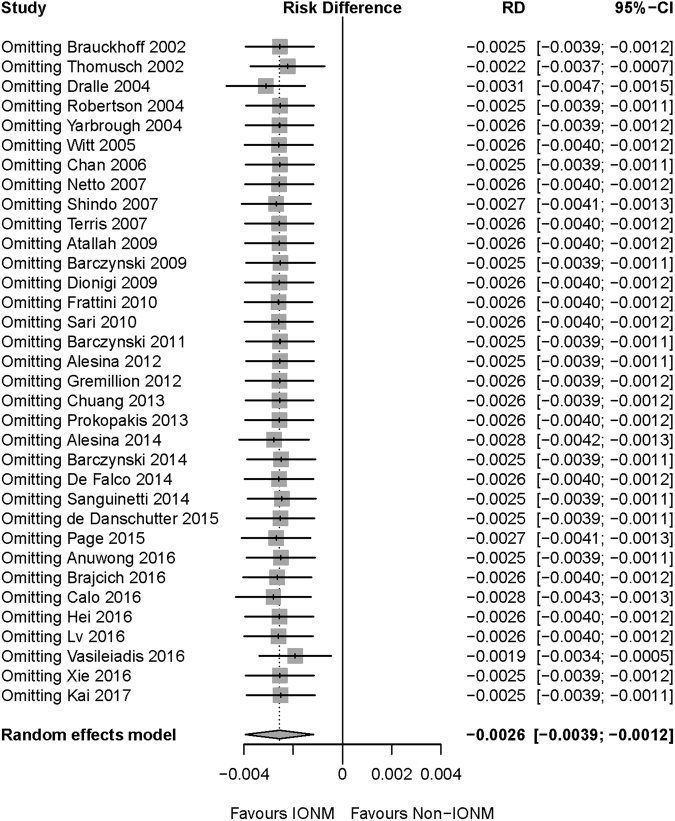
Publication bias and sensitivity analysis
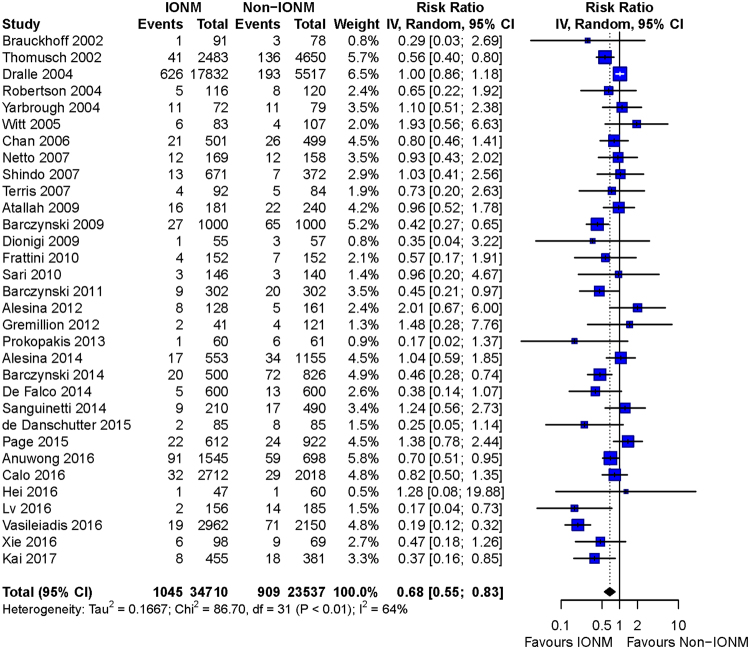
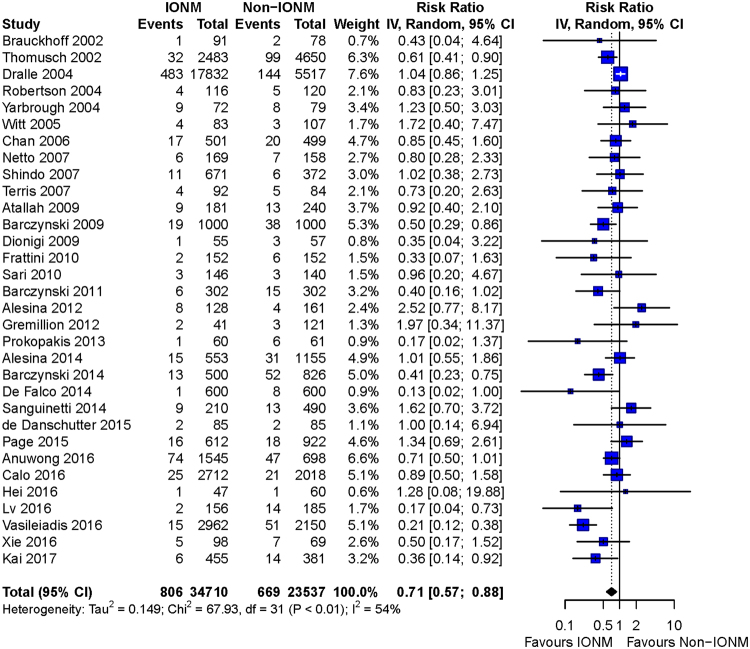
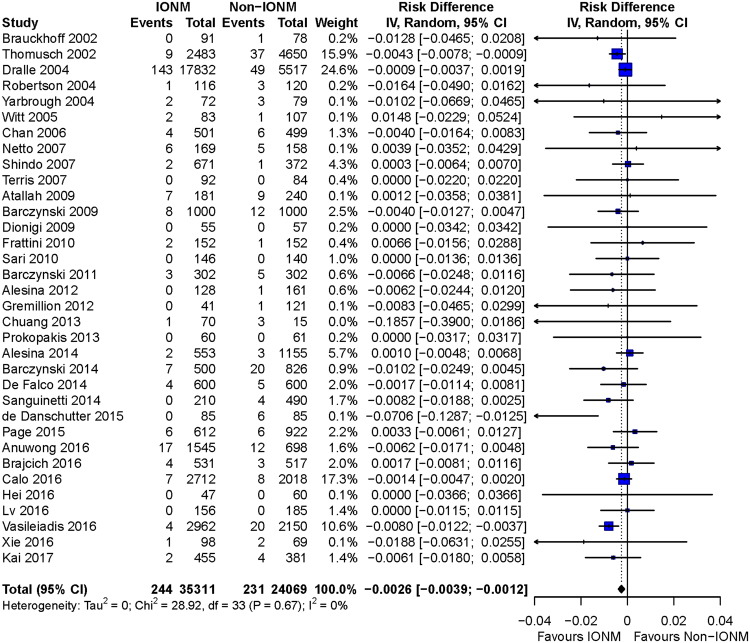
Begg’s and Egger’s test were conducted to assess the publication bias in this meta-analysis. None of the tests was statistically significant in total injury (Begg’s p = 0.97 and Egger’s p = 0.14), transient injury (Begg’s p = 0.79 and Egger’s p = 0.15) and permanent injury (Begg’s p = 0.012 and Egger’s p = 0.19). Meta-analysis was recalculated after omitting every record included in the analysis to check the sensitivity of our overall results. As shown in Figs 2, 3 and 4, the results of total, transient and permanent injury were robust after omitting any record.
Figure 2.
Sensitivity analysis of total RLN injury. After omitting any of the included studies, the meta-analysis result of total RLN injury was still robust. Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Figure 3.
Sensitivity analysis of transient RLN injury. After omitting any of the included studies, the meta-analysis result of transient RLN injury was still robust. Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Figure 4.
Sensitivity analysis of permanent RLN injury. After omitting any of the included studies, the meta-analysis result of permanent RLN injury was still robust. Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Overall meta-analysis
Overall meta-analysis found a significant decrease of total RLN injury (RR = 0.68, 95%CI: 0.55 to 0.83; p = 0.0002), transient injury (RR = 0.71, 95%CI: 0.57 to 0.88; p = 0.0017), and permanent injury (RD = −0.0026, 95%CI: −0.0039 to −0.0012; p = 0.0003) by IONM (Figs 5, 6 and 7).
Figure 5.
Forest plot of total RLN injury. Less total RLN injuries were found in IONM group than in non-IONM group by pooled analysis (p = 0.0002). Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Figure 6.
Forest plot of transient RLN injury. Meta-analysis showed a preventive effect of IONM on transient RLN injury (p = 0.0017). Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Figure 7.
Forest plot of permanent RLN injury. Meta-analysis demonstrated a 0.26% reduction of permanent RLN injury with IONM (p = 0.0003). Abbreviation: IONM = intraoperative nerve monitoring; RLN = recurrent laryngeal nerve.
Subgroup analysis for bilateral operation
A total of 11 studies were included in the analysis, of which 2 studies were without transient injury data. Subgroup analysis demonstrated IONM group had a lower incidence of total, transient and permanent injury than non-IONM group. (IONM group: total injury 1.46%, transient injury 1.07%, permanent injury 0.50%; non-IONM group: total injury 3.01%, transient injury 2.12%, permanent injury 0.75%).
Subgroup analysis for malignancy operation
A total of 8 studies were included in the analysis. Data showed that IONM had protective effects in total injury and in transient injury. (Total injury: RR = 0.61, 95% CI: 0.42 to 0.91; p = 0.02; Transient injury RR = 0.61, 95% CI: 0.38 to 0.97; p = 0.04) However, IONM had no significant protective effect in permanent injury. (RD = −0.0009, 95%CI: −0.0063 to 0.0044; p = 0.73).
Subgroup analysis for reoperation group
A total of 9 studies were included in the analysis. The rate of total (RR = 0.64, 95% CI: 0.33–1.24; p = 0.1843), transient (RD = −0.0113, 95% CI: −0.0502 to 0.0276; p = 0.5687) or permanent injury (RD = −0.0082, 95% CI: −0.0176 to 0.0013; p = 0.0906) had no difference between IONM and non-IONM in the reoperation subgroup.
Subgroup analysis of operation volume
To evaluate the effect of operation volume, we used the criteria of 300 NARs as the cut off to divide operation volume, as consistent with relevant studies5,53. IONM could reduce the incidence of total (RR = 0.78, 95%CI: 0.63 to 0.97; p = 0.0271) and transient (RR = 0.79, 95%CI: 0.63 to 0.99; p = 0.0454) injury in the group with operation volume < 300 NARs per year. Analysis also found a preventive effect of IONM on total and permanent injury in the group with operation volume > 300 NARs per year. (p = 0.0292 and p = 0.0247, correspondingly).
Discussion
IONM had received widespread acceptance in the field of thyroid surgery for its role in RLN identification. However, the protective effect of IONM on RLN injury remained controversial. Zheng et al. proposed that IONM could reduce total and transient RLN injury in thyroidectomy13, but the results of transient injury had been proven to be hypersensitive13. Lombardi et al. gave a negative conclusion about the protective effects of IONM on permanent injury18. Wong et al. demonstrated that high-risk subpopulations might benefit from IONM, especially in reoperation and malignancy subgroups17. Several large studies were recently published in the past year; Some studies found preventive effects of IONM on total and transient injury23,24,26, while others declared an insignificant result on this topic10,11,22,25. To identify the protective effect of IONM on RLN function and explore more subgroups which could benefit from IONM, we conducted a meta-analysis that included the most recent developments in this field. Additionally, our meta-analysis was the first to investigate the protective effect of IONM on the topic of bilateral operation and operation volume and revealed the preventive effect of IONM on permanent injury in these subgroups.
Our meta-analysis found preventive effects of IONM on total, transient and permanent RLN injury. The result was still robust after sensitivity analysis. Previous meta-analyses found a decrease of total and transient injury in IONM cases, but for permanent injury the result was not statistically significant12,13. The negative results might result from small data sample size (NARs less than 40,000). A total of 59,380 NAR involved in this analysis was enough to reveal IONM’s effect on permanent injury. Lombardi et al. mentioned the influence of permanent injury definition and measurement18. In this study, both the permanent injury definition (over 6 months) and laryngoscopy measurement were included and did not influence the final results (Appendix Table 3). Based on existing results, we recommended IONM as a routine measurement to be used in thyroidectomy.
In subgroup analyses, the study revealed preventive effects of IONM on total and transient RLN injury in bilateral operation and malignancy operation subgroups. However, for permanent injury, a similar effect was only found in bilateral operation cases. Bilateral thyroidectomy requires relative large operation extent and long operation duration. Previous studies revealed RLN injury incidence in bilateral operation was 1.2–2.3%2,5. In this study, pooled incidences of total, transient and permanent injury in bilateral operation were 2.3%, 1.6% and 0.61%. Our results supported the recommendation of IONM application in bilateral operation. Above all, bilateral operation might induce bilateral RLN injury, which could lead to airway obstruction. To avoid this fatal complication, someone proposed routine IONM application in bilateral operation and a staged thyroidectomy would be needed for cases with intraoperative RLN signal loss19.
Previous meta-analyses only showed positive results in transient injury for malignancy operation. Our analysis included 3 new studies11,21,25 and 1 study with updated data22. The results demonstrated a statistically significant decrease of total and transient injury in malignancy operation cases with IONM. Malignancy operation might contain potential risk of malignancy invasion of RLN and lymph node dissection, which increase the risk of RLN injury. IONM might reduce the risk by real-time monitor of RLN function.
Reoperation of the thyroid has higher risks than normal thyroidectomy, for local conglutination and anatomical changes can result in RLN injury. Local conglutination makes the identification of RLN difficult and the anatomical position of RLN might change due to a previous operation. Wong et al. found a decreased incidence of total injury in the reoperation group with IONM. However, our study demonstrated a negative result in the reoperation group with IONM, with 2 new studies21,45 and 1 study with updated data22 included. The effect of IONM in this subgroup still needs to be identified. Further large size randomized trials need to be conducted to clarify this debate.
The impact of operation volume was also emphasized in several studies. In a German retrospective multicenter trial, a large operation volume medical center had a lower rate of permanent RLN injury, and thus IONM might be more helpful in small operation volume centers than in large operation volume centers5. However, in our subgroup analysis, we found IONM could help both small and large operation volume medical centers. IONM reduced total and transient RLN injury in small operation volume centers, and decreased total and permanent RLN injury in large operation volume centers. With the aid of IONM, inexperienced surgeons could avoid hazardous surgical situations near or on the RLN with real-time identification of the RLN54.
There were several limitations in our study. First, there were still several studies didn’t declare the outcome measurement or follow up for enough duration. The robust test had been passed including all the studies with laryngoscopy measurement and more than 6 months of follow-up. Second, there still existed confounders and heterogeneity in our analysis. Some studies included cases that involved intentional RLN transection. The influence of lymph node dissection could also not be eliminated. The sensitivity analysis, subgroup analysis, and random-effects model was applied to address this.
Conclusions
This meta-analysis indicated that IONM could reduce the incidence of total, transient and permanent RLN injury compared with conventional visual identification. We also recommended IONM in bilateral operations and malignancy operations. IONM could help surgeons perform a better thyroidectomy regardless of the medical center’s operation volume. The benefit of IONM in reoperation cases needs to be further explored. We hope our findings can be assessed by large prospective, randomized clinical trials in the future with a standardized IONM application and outcome measurement.
Electronic supplementary material
Acknowledgements
We thank Dr. Zhiyu Li, Dr. Mao Ye and Dr. Dapeng Xiang for their helpful comments. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author Contributions
Binglong Bai designed the study, coordinated the data acquisition, planned statistical analysis, and wrote the first draft of the manuscript. Wuzhen Chen helped to design the study, draft and revise the manuscript. All authors read and approved the final manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-26219-5.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abadin, S. S., Kaplan, E. L. & Angelos, P. Malpractice litigation after thyroid surgery: the role of recurrent laryngeal nerve injuries, 1989–2009. Surgery148, 718–722; discussion 722–713, 10.1016/j.surg.2010.07.019 (2010). [DOI] [PubMed]
- 2.Thomusch O, Sekulla C, Walls G, Machens A, Dralle H. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg. 2002;183:673–678. doi: 10.1016/S0002-9610(02)00856-5. [DOI] [PubMed] [Google Scholar]
- 3.Robertson ML, Steward DL, Gluckman JL, Welge J. Continuous laryngeal nerve integrity monitoring during thyroidectomy: does it reduce risk of injury? Otolaryngol Head Neck Surg. 2004;131:596–600. doi: 10.1016/j.otohns.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 4.Yarbrough DE, Thompson GB, Kasperbauer JL, Harper CM, Grant CS. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery. 2004;136:1107–1115. doi: 10.1016/j.surg.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Dralle H, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136:1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Chan, W. F., Lang, B. H. & Lo, C. Y. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery140, 866–872; discussion 872–863, 10.1016/j.surg.2006.07.017 (2006). [DOI] [PubMed]
- 7.Dionigi G, et al. Severity of Recurrent Laryngeal Nerve Injuries in Thyroid Surgery. World J Surg. 2016;40:1373–1381. doi: 10.1007/s00268-016-3415-3. [DOI] [PubMed] [Google Scholar]
- 8.Alesina PF, et al. Intraoperative neuromonitoring does not reduce the incidence of recurrent laryngeal nerve palsy in thyroid reoperations: results of a retrospective comparative analysis. World J Surg. 2012;36:1348–1353. doi: 10.1007/s00268-012-1548-6. [DOI] [PubMed] [Google Scholar]
- 9.Duclos A, et al. Influence of intraoperative neuromonitoring on surgeons’ technique during thyroidectomy. World J Surg. 2011;35:773–778. doi: 10.1007/s00268-011-0963-4. [DOI] [PubMed] [Google Scholar]
- 10.Anuwong A, et al. Recurrent laryngeal nerve management in thyroid surgery: consequences of routine visualization, application of intermittent, standardized and continuous nerve monitoring. Updates Surg. 2016;68:331–341. doi: 10.1007/s13304-016-0393-9. [DOI] [PubMed] [Google Scholar]
- 11.Hei H, Zhai Y, Qin J, Song Y. Intermittent Intraoperative Neural Monitoring Technology in Minimally Invasive Video-Assisted Thyroidectomy: A Preliminary Study. J Invest Surg. 2016;29:93–97. doi: 10.3109/08941939.2015.1073411. [DOI] [PubMed] [Google Scholar]
- 12.Yang S, et al. Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg. 2017;39:104–113. doi: 10.1016/j.ijsu.2017.01.086. [DOI] [PubMed] [Google Scholar]
- 13.Zheng S, Xu Z, Wei Y, Zeng M, He J. Effect of intraoperative neuromonitoring on recurrent laryngeal nerve palsy rates after thyroid surgery–a meta-analysis. J Formos Med Assoc. 2013;112:463–472. doi: 10.1016/j.jfma.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Barczynski M, et al. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: results of a retrospective cohort study. World J Surg. 2014;38:599–606. doi: 10.1007/s00268-013-2260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page C, Cuvelier P, Biet A, Strunski V. Value of intra-operative neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy for benign goitre. J Laryngol Otol. 2015;129:553–557. doi: 10.1017/S0022215115001152. [DOI] [PubMed] [Google Scholar]
- 16.Pisanu A, Porceddu G, Podda M, Cois A, Uccheddu A. Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J Surg Res. 2014;188:152–161. doi: 10.1016/j.jss.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 17.Wong KP, Mak KL, Wong CK, Lang BH. Systematic review and meta-analysis on intra-operative neuro-monitoring in high-risk thyroidectomy. Int J Surg. 2017;38:21–30. doi: 10.1016/j.ijsu.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 18.Lombardi CP, et al. The final countdown”: Is intraoperative, intermittent neuromonitoring really useful in preventing permanent nerve palsy? Evidence from a meta-analysis. Surgery. 2016;160:1693–1706. doi: 10.1016/j.surg.2016.06.049. [DOI] [PubMed] [Google Scholar]
- 19.Goretzki PE, Schwarz K, Brinkmann J, Wirowski D, Lammers BJ. The impact of intraoperative neuromonitoring (IONM) on surgical strategy in bilateral thyroid diseases: is it worth the effort? World J Surg. 2010;34:1274–1284. doi: 10.1007/s00268-009-0353-3. [DOI] [PubMed] [Google Scholar]
- 20.Pardal-Refoyo JL, Ochoa-Sangrador C. Bilateral recurrent laryngeal nerve injury in total thyroidectomy with or without intraoperative neuromonitoring. Systematic review and meta-analysis. Acta Otorrinolaringol Esp. 2016;67:66–74. doi: 10.1016/j.otorri.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Brajcich BC, McHenry CR. The utility of intraoperative nerve monitoring during thyroid surgery. J Surg Res. 2016;204:29–33. doi: 10.1016/j.jss.2016.04.039. [DOI] [PubMed] [Google Scholar]
- 22.Calo PG, et al. Interpretation of intraoperative recurrent laryngeal nerve monitoring signals: The importance of a correct standardization. Int J Surg. 2016;28(Suppl 1):S54–58. doi: 10.1016/j.ijsu.2015.12.039. [DOI] [PubMed] [Google Scholar]
- 23.Lv B, Zhang B, Zeng QD. Total Endoscopic Thyroidectomy with Intraoperative Laryngeal Nerve Monitoring. Int J Endocrinol. 2016;2016:7381792. doi: 10.1155/2016/7381792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vasileiadis I, et al. Association of Intraoperative Neuromonitoring With Reduced Recurrent Laryngeal Nerve Injury in Patients Undergoing Total Thyroidectomy. JAMA Otolaryngol Head Neck Surg. 2016;142:994–1001. doi: 10.1001/jamaoto.2016.1954. [DOI] [PubMed] [Google Scholar]
- 25.Xie Q, Wang P, Yan H, Wang Y. Feasibility and Effectiveness of Intraoperative Nerve Monitoring in Total Endoscopic Thyroidectomy for Thyroid Cancer. J Laparoendosc Adv Surg Tech A. 2016;26:109–115. doi: 10.1089/lap.2015.0401. [DOI] [PubMed] [Google Scholar]
- 26.Kai, H. et al. Intraoperative nerve monitoring reduces recurrent laryngeal nerve injury in geriatric patients undergoing thyroid surgery. Acta Otolaryngol 1–6, 10.1080/00016489.2017.1354397 (2017). [DOI] [PubMed]
- 27.Chandrasekhar SS, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg. 2013;148:S1–37. doi: 10.1177/0194599813487301. [DOI] [PubMed] [Google Scholar]
- 28.Wells, G. A. S. B. et al The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2012).
- 29.Schwarzer G. Meta: An R package for meta-analysis. R news. 2007;7:40–45. [Google Scholar]
- 30.Collaboration, C. Cochrane handbook for systematic reviews of interventions 5.0. 0. (Cochrane Collaboration, 2008).
- 31.Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev. 1987;9:1–30. doi: 10.1093/oxfordjournals.epirev.a036298. [DOI] [PubMed] [Google Scholar]
- 32.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Witt RL. Recurrent laryngeal nerve electrophysiologic monitoring in thyroid surgery: the standard of care? J Voice. 2005;19:497–500. doi: 10.1016/j.jvoice.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Netto Ide P, et al. Vocal fold immobility after thyroidectomy with intraoperative recurrent laryngeal nerve monitoring. Sao Paulo Med J. 2007;125:186–190. doi: 10.1590/S1516-31802007000300011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007;133:481–485. doi: 10.1001/archotol.133.5.481. [DOI] [PubMed] [Google Scholar]
- 38.Terris DJ, Anderson SK, Watts TL, Chin E. Laryngeal nerve monitoring and minimally invasive thyroid surgery: complementary technologies. Arch Otolaryngol Head Neck Surg. 2007;133:1254–1257. doi: 10.1001/archotol.133.12.1254. [DOI] [PubMed] [Google Scholar]
- 39.Atallah I, et al. Role of intraoperative neuromonitoring of the recurrent laryngeal nerve in high-risk thyroid surgery. J Otolaryngol Head Neck Surg. 2009;38:613–618. [PubMed] [Google Scholar]
- 40.Dionigi G, Boni L, Rovera F, Bacuzzi A, Dionigi R. Neuromonitoring and video-assisted thyroidectomy: a prospective, randomized case-control evaluation. Surg Endosc. 2009;23:996–1003. doi: 10.1007/s00464-008-0098-3. [DOI] [PubMed] [Google Scholar]
- 41.Frattini F, et al. Intraoperative neuromonitoring for thyroid malignancy surgery: technical notes and results from a retrospective series. Updates Surg. 2010;62:183–187. doi: 10.1007/s13304-010-0036-5. [DOI] [PubMed] [Google Scholar]
- 42.Sari S, et al. Evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg. 2010;8:474–478. doi: 10.1016/j.ijsu.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 43.Barczynski M, et al. Clinical value of intraoperative neuromonitoring of the recurrent laryngeal nerves in improving outcomes of surgery for well-differentiated thyroid cancer. Pol Przegl Chir. 2011;83:196–203. doi: 10.2478/v10035-011-0030-8. [DOI] [PubMed] [Google Scholar]
- 44.Gremillion G, Fatakia A, Dornelles A, Amedee RG. Intraoperative recurrent laryngeal nerve monitoring in thyroid surgery: is it worth the cost? Ochsner J. 2012;12:363–366. [PMC free article] [PubMed] [Google Scholar]
- 45.Chuang YC, Huang SM. Protective effect of intraoperative nerve monitoring against recurrent laryngeal nerve injury during re-exploration of the thyroid. World J Surg Oncol. 2013;11:94. doi: 10.1186/1477-7819-11-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prokopakis E, et al. Intraoperative recurrent laryngeal nerve monitoring in revision thyroidectomy. Eur Arch Otorhinolaryngol. 2013;270:2521–2524. doi: 10.1007/s00405-012-2338-3. [DOI] [PubMed] [Google Scholar]
- 47.Alesina PF, et al. Intraoperative neuromonitoring for surgical training in thyroid surgery: its routine use allows a safe operation instead of lack of experienced mentoring. World J Surg. 2014;38:592–598. doi: 10.1007/s00268-013-2372-3. [DOI] [PubMed] [Google Scholar]
- 48.De Falco M, Santangelo G, Del Giudice S, Gallucci F, Parmeggiani U. Double probe intraoperative neuromonitoring with a standardized method in thyroid surgery. Int J Surg. 2014;12(Suppl 1):S140–144. doi: 10.1016/j.ijsu.2014.05.026. [DOI] [PubMed] [Google Scholar]
- 49.Sanguinetti A, et al. Intraoperative recurrent laryngeal nerve monitoring in thyroid surgery Evaluation of its use in terms of “spending review”. Ann Ital Chir. 2014;85:418–421. [PubMed] [Google Scholar]
- 50.de Danschutter SJ, Schreinemakers JM, Smit LH, van der Laan L, Nuytinck HK. Thyroid surgery and the usefulness of intraoperative neuromonitoring, a single center study. J Invest Surg. 2015;28:86–94. doi: 10.3109/08941939.2014.975876. [DOI] [PubMed] [Google Scholar]
- 51.Brauckhoff M, et al. First experiences in intraoperative neurostimulation of the recurrent laryngeal nerve during thyroid surgery of children and adolescents. J Pediatr Surg. 2002;37:1414–1418. doi: 10.1053/jpsu.2002.35403. [DOI] [PubMed] [Google Scholar]
- 52.Barczynski M, Konturek A, Cichon S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009;96:240–246. doi: 10.1002/bjs.6417. [DOI] [PubMed] [Google Scholar]
- 53.Chung TK, et al. Examining national outcomes after thyroidectomy with nerve monitoring. J Am Coll Surg. 2014;219:765–770. doi: 10.1016/j.jamcollsurg.2014.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pragacz K, Barczynski M. Evaluation of the learning curve for intraoperative neural monitoring of the recurrent laryngeal nerves in thyroid surgery. Pol Przegl Chir. 2015;86:584–593. doi: 10.1515/pjs-2015-0005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.