Abstract
Background and Aim
Fractional CO2 lasers have been shown to provide improvement of vulvovaginal atrophy (VVA). The aim of the current study was to assess the early effect of a fractional CO2 laser system in treating postmenopausal women with clinical symptoms of VVA.
Methods
28 healthy post-menopausal women (mean age 60.1 ± 5.55 years) with VVA-related symptoms were treated with fractional CO2 laser 3 times, in 4-week intervals. At each study visit, VHIS score and VVA symptom severity were recorded. Sexual function was assessed with the Female Sexual Function Index (FSFI).
Results
One month following the first laser treatment, the mean VHIS score was significantly improved (13.89 ± 4.25 vs. baseline 11.93 ± 3.82; p < 0.05), and improved further at 3 and 6 months following all three laser treatments (16.43 ± 4.20 and 17.46 ± 4.07, respectively). Almost all VVA symptoms were significantly improved at one month following the first treatment. A further significant improvement in VVA symptoms was noted at 3 and 6 months following the third laser treatment. Following treatments, the FSFI score increased significantly (22.36 ± 10.40 vs. baseline 13.78 ± 7.70; p < 0.05), and remained significantly higher than baseline at the 3- and 6-month follow-up visits.
Conclusion
CO2 laser therapy for post-menopausal women can be considered an effective therapeutic option providing relief of symptoms already noted after one laser treatment.
Keywords: CO2 laser, vulvovaginal atrophy, menopause, sexual function
Introduction
Vulvovaginal atrophy (VVA) is a disorder that occurs in postmenopausal women whose symptoms includes vaginal burning, dryness, itching, dyspareunia, and lower urinary dysfunction 1–3). As the result of hypoestrogenism, the vaginal wall becomes thin, dry, pale, less elastic, prone to petechiae and the vulva also may undergo shrinkage and fusion. Urinary symptoms may include dysuria, stress and urge incontinence and recurrent urinary tract infections. In several surveys of post-menopausal women, it has been shown that VVA negatively affects interpersonal relationships, quality of life, daily activities, and sexual function 4). VVA is a chronic disorder and is less likely to be resolved without intervention 5, 6). The therapeutic goals of VVA management are relief of symptoms as well as restoration of the vaginal environment to a healthy state. Treatments include topical preparations such as lubricants, moisturizers, local estrogen creams, tablets, rings and systemic hormonal replacement therapy 7–9). Vaginal lubricants and moisturizers provide temporary relief from vaginal dryness and dyspareunia, however, they have no long-term therapeutic effects 10). Estrogen, either topical or systemic, is an effective treatment for women with moderate to severe symptoms of vaginal atrophy 11, 12). However, patient adherence to treatment is low and these treatments are contraindicated for patients with a history of estrogen-dependent cancers 13).
There has been growing interest in new therapeutic options that can effectively provide long term symptomatic relief for VVA 10). CO2 lasers can be used to address this unmet need, as they have been scientifically proven to be beneficial and safe for tissue remodeling in many clinical specialties 14–18). Laser energy is absorbed by water in treated tissue, heats the microscopic treatment zones, causing ablation of the tissue that results in immediate collagen fiber contraction as well as initiation of the longer process of neocollagenesis 9). In the short term, CO2 laser utilization results in shorter and thicker collagen fibers, and during long term healing, the CO2 treatments produce neovascularization and new collagen fibers 19).
The use of fractional CO2 lasers was extended to treatment of subjects suffering from VVA-related symptoms 19). The procedure includes a treatment provided to the vaginal canal that can be followed by an option of direct irradiation to the vaginal introitus. The CO2 laser wavelength, 10,600 nm (infrared range), is highly absorbed by water. In cases of vaginal atrophy, the laser energy is absorbed by the moist layer of connective tissue underlying the epithelium 20). The CO2 energy is delivered in a fractional manner which generates thermal micro millimeter tissue damage. The fractional pattern is important, as it maintains healthy tissue surrounding each micro ablation zone enabling rapid and complete epithelial repair.
Fractional CO2 laser treatments have been shown to improve VVA symptoms 21, 22). Histological analysis of punch biopsies before and after treatments revealed an improved state of the vaginal wall, resembling a non-atrophied state 21, 22). After treatment, the epithelium was thicker with a basal layer of closely-packed cells. In addition, an increase in fibroblast activity was noted 23). The treatment usually includes 3 laser treatments, provided in monthly intervals. Improvement in symptoms was usually noted at the completion of the treatment protocol or at 4 weeks following the third laser treatment 24–26).
The aim of the current study was to assess the early effect of the fractional CO2 laser system in treating postmenopausal women with clinical symptoms of VVA.
Methods
Study Design
This prospective study of postmenopausal women presenting with VVA-related symptoms was conducted between April 2016 and April 2017 at the Center of Women's Health and Wellness, Plainsboro, New Jersey USA. The protocol was approved by Schulman Institutional Review Board. Written informed consent was obtained from all subjects.
Study Population
Thirty-two subjects were enrolled and twenty-eight subjects completed the study. Main inclusion criteria were: sexual activity or desire for sexual activity, menopausal status, and one or more VVA-related symptoms (e.g. dryness, itching, burning, dysuria or dyspareunia). Women that had Vaginal Health Index (VHIS) scores below 5 (Gloria Bachmann's Vaginal Health Index (VHI) 27), systemic steroid or hormonal use in previous three months, active genital infection, recurrent urinary tract infections, abnormal Pap smears, or pelvic organ prolapse (POP) > II, were excluded.
Study Protocol and Procedure
Three treatment visits were scheduled four weeks apart. Subjects were asked to refrain from using vaginal lubricants seven days prior to treatment. The treatment of the vaginal canal was provided by the FemTouch™ handpiece of the Lumenis AcuPulse™ system. The Fem-Touch™ handpiece was inserted into the vagina. The fractional CO2 laser energy was transmitted through the handpiece along the vaginal canal in a retrograde manner. Treatment settings were determined by the physician, based on the degree of vaginal atrophy and varied at 7.5, 10 or 12.5 mJ.
Following treatment, subjects were instructed to avoid heat exposure in the treated area and refrain from sexual activity up to 72 hours. Subjects were asked to document the timing of resumed sexual activity after the procedure.
Data Collection
Demographic data and medical history were collected during the screening visit. At each study visit, vaginal health was assessed by the investigator and a VHIS score consisting of five vaginal parameters: Elasticity, Secretion/fluid volume, Vaginal pH, Integrity of the epithelium, and Lubrication/moisture of the vaginal wall, was recorded. VVA symptom severity was self-evaluated by study participants on a 10cm visual analogue scale (VAS).
Subjects were asked to rate treatment discomfort /pain immediately after treatment in the following categories: insertion of the probe into the vagina, movement of the probe inside the vagina and laser irradiation inside the vagina. The rating was based on a pain VAS scale where the extreme left indicates “no pain” and extreme right indicates “intolerable pain”.
The Female Sexual Function Index (FSFI), a questionnaire designed to measure sexual functioning in women with a specific focus on sexual arousal, orgasm, satisfaction, and pain was collected at each visit. In addition, “sexual downtime”, defined as the period of time following the procedure during which the subject could not have sexual intercourse, was reported by the subjects at treatment visits following procedure and at the first month follow-up visit.
The subject's overall satisfaction level with the treatment procedure and outcome were assessed at the third treatment visit and at each follow-up visit, using a 5-point Likert scale where 0 represents “very dissatisfied” and 4 represents “very satisfied”.
Statistical Analysis
All statistical analyses were performed using SAS® version 9.4 (SAS Institute, Cary NC, USA) software. Statistical tests performed were two-sided. The level of significance is 0.05. All p-values are nominal.
Descriptive statistics (frequency - count and proportion, mean, standard deviation, minimum, median and maximum) are presented for the background variables and study variables.
The changes from baseline in the VHIS, subject assessment of VVA symptoms and FSFI were evaluated using repeated measures analysis of variance models, where the changes were modeled (individually) as a function of respective baseline values and visit number (categorical).
A sample size of 28 subjects, was designed to provide an 82% power and a 5% significance level to detect a mean change in the study measurements.
Results
Demographic and Baseline Characteristics of Study Population
Thirty-two women were enrolled, three subjects withdrew consent and one was lost to follow up. A total of twenty-eight post-menopausal women completed the protocol (3 treatments and the full 6-months follow-up period). Demographic and other baseline characteristics are presented in Table 1.
Table 1: Demographic Characteristics of The Study Population.
| Age (years) | 60.1 ± 5.55 |
| Body Mass Index (kg/m2) | 26.2 ± 4.41 |
| Smokers | 3.57% (1/28) |
| Previous Vaginal Deliveries | 57.14% (16/28) |
| Time Since Last Spontaneous Menstrual Bleeding (months) | 106.7 ± 72.57 |
Data are presented as mean ± standard deviation (continuous variables) or % (n/N) (categorical variables).
Adverse events (AE) reported during the study were of moderate severity and were unrelated to the procedure. One episode of vaginal bleeding was reported to occur at one month following last treatment but was deemed unrelated to the procedure. A single serious adverse event of Trigeminal Neuropathy was reported and was assessed as unrelated to the procedure. No subjects were discontinued due to an adverse event. Immediately following the procedure, women were asked to rate the discomfort they experienced during the procedure. All pain scores were low, the maximal mean score was 2.73 ± 2.80, for insertion of the probe at the second treatment.
The downtime following procedure was reported by the participants. The majority of women felt no discomfort at all, or only up to 1 week after the first procedure.
Change from Baseline in VHI Score and VVA Symptoms
The mean VHI score (± standard deviation) was significantly improved following treatment as already seen at 1 month following the first laser treatment (13.89 ± 4.25 vs. baseline 11.93 ± 3.82; p < 0.05) (Table 2). Following the completion of all treatments, the study primary endpoint, VHI score at three months post treatment, was significantly improved (16.43 ± 4.20). The improvement from baseline was also significant at the six months follow-up visit (17.46 ± 4.07).
Table 2: VHI Score and VVA Symptoms.
| Baseline | 1M After Tx1 | 1MFU | 3MFU | 6MFU | |
|---|---|---|---|---|---|
| VHIS score | 11.93 ± 3.82 | 13.89 ± 4.25* | 17.07 ± 4.24* | 16.43 ± 4.20* | 17.46 ± 4.07* |
| Vaginal itchinga | 1.22 ± 2.06 | 0.84 ± 1.65 | 0.56 ± 0.90* | 0.58 ± 1.13* | 0.36 ± 0.92* |
| Vaginal burninga | 1.68 ± 2.52 | 0.94 ± 1.55* | 0.39 ± 0.73* | 0.38 ± 0.93* | 0.12 ± 0.28* |
| Vaginal drynessa | 5.04 ± 3.16 | 2.57 ± 2.42* | 1.99 ± 1.84* | 1.53 ± 1.85* | 2.30 ± 2.78* |
| Dyspareunia (Pain during intercourse)a | 6.29 ± 3.23 | 2.84 ± 2.74* | 2.13 ± 2.49* | 2.25 ± 2.91* | 2.38 ± 3.07* |
| Dysuria (Pain/stinging during urination)a | 1.35 ± 2.31 | 1.51 ± 2.60 | 0.44 ± 0.79* | 0.32 ± 0.66* | 0.22 ± 0.51* |
Data is presented as mean ± standard deviation. aData is measured on a VAS scale (range 0–10).
Significantly different from baseline, p < 0.05. Tx1: first treatment; MFU: months of follow-up after third laser treatment.
VAS scoring of VVA symptoms by visit is presented in Table 2 and Figure 1. VVA symptoms such as vaginal burning, vaginal dryness and dyspareunia were significantly improved at 1 month following the first treatment compared to baseline. From the time point of 1 month following the completion of laser treatments, all VVA symptoms (vaginal itching, vaginal burning, vaginal dryness, dyspareunia and dysuria (pain/stinging during urination)) were significantly improved compared to baseline, and this improvement was sustained at the six months follow-up visit.
Figure 1:
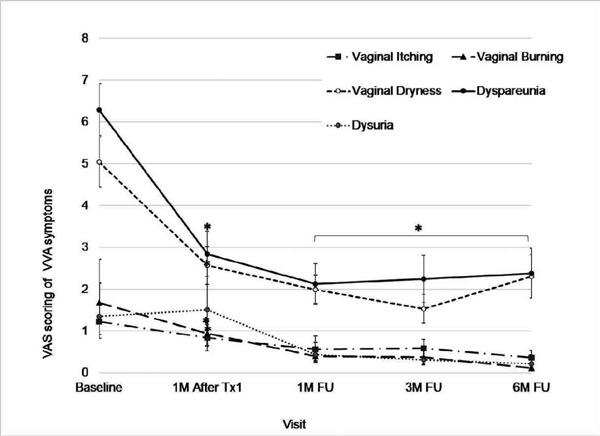
VVA Symptoms -Attached As a Separate File-
Figure 1 legend: Data, measured on a VAS scale (range 0–10), is presented as mean ± standard error. *Significantly different from baseline, p < 0.05.
Sexual Function (FSFI) and Sexual Downtime
The efficacy of CO2 laser treatment on VVA symptoms was also measured, using the FSFI. At baseline, 23 women (82%) were sexually active, while all the other patients were not sexually active due to symptoms of VVA, but had expressed an interest in regaining a normal sexual life. The mean baseline score of FSFI (± SD) was 13.78 ± 7.70 (Table 3). Following 3 treatments, by the 1-month follow-up, the total FSFI score increased significantly (22.36 ± 10.40; P < 0.05), and at the 3- and 6-month follow-up visits, the total FSFI remained significantly higher than at baseline (20.48 ± 11.44, 20.10 ± 11.26). Each FSFI domain (desire, arousal, lubrication orgasm etc.), was significantly improved at the one month follow up and this improvement was sustained until the 6 months follow up. Following the third treatment, 89% of women were able to resume sexual intercourse.
Table 3: FSFI Total and Domain Scores.
| Baseline | 1MFU | 3MFU | 6MFU | |
|---|---|---|---|---|
| Total Score | 13.78 ± 7.70 | 22.36 ± 10.40* | 20.48 ± 11.44* | 20.10 ± 11.26* |
| Desire | 2.64 ± 1.11 | 3.34 ± 1.09* | 3.26 ± 1.22* | 3.13 ± 1.18* |
| Arousal | 2.37 ± 1.56 | 3.90 ± 1.81* | 3.32 ± 2.27* | 3.35 ± 2.12* |
| Lubrication | 1.99 ± 1.57 | 3.77 ± 2.10* | 3.33 ± 2.21* | 3.42 ± 2.07* |
| Orgasm | 2.40 ± 1.91 | 3.84 ± 2.19* | 3.66 ± 2.45* | 3.54 ± 2.29* |
| Satisfaction | 2.61 ± 1.68 | 3.99 ± 2.06* | 3.86 ± 2.06* | 3.61 ± 2.08* |
| Pain | 1.77 ± 1.54 | 3.51 ± 2.21* | 3.06 ± 2.25* | 3.04 ± 2.10* |
Data is presented as mean ± standard deviation.
Significantly different from baseline, p < 0.05.
At the 3-month follow-up, 85% of patients (23 patients) were satisfied with the procedure, and that proportion increased to 89% (25 patients) satisfied patients by the 6-month follow-up.
Discussion
The present study was a relatively small study, with no control group. However, results were consistent across study participants and in accordance with published literature, lending them credibility and allowing extrapolation to the general patient population. In addition, the study was based on Physician and participant assessments; and while it can be claimed that objective measurable endpoints may have rendered it more scientifically robust, the treatment is aimed at relieving symptoms that are experienced subjectively by individual patients and thus, patient self-assessment in the study was deemed a good representation of the effectiveness of the treatment.
The present prospective study evaluated the efficacy of fractional CO2 laser therapy in postmenopausal women with symptoms of VVA. Physician assessments were based on the VHIS and the VVA symptoms were evaluated by the subjects. The results showed statistically-significant improvement in the VHIS that was significantly increased following treatment; this was in accordance with previous studies 9, 20, 28). Notably, in our study, improvement was already observed after the first laser treatment. In addition, the percentage of women that could be considered as non-atrophic by the VHIS had doubled at the 3 months follow up compared to baseline. The VVA symptoms were significantly improved following the CO2 treatment and this was apparent after the first treatment. Vaginal dryness and dyspareunia, that were the most bothersome complaints at baseline, were dramatically improved following treatment.
The women's sexual function, as assessed by the FSFI questionnaire, improved significantly. Improvement in all components of the FSFI was observed at the one month follow up and was sustained throughout the six months of follow up. Improvement in the FSFI was presented in several studies with a shorter follow up of up to 12 weeks following CO2 treatment 24, 29). This observation can be explained by the improvement in vaginal dryness resulting in less painful intercourse 30).
Of note, in the current study, a significant improvement in vaginal health and symptoms, assessed by physician and subjects, was already apparent after one treatment and was sustained for six months following treatments. Vaginal health improvement was accompanied by improved sexual function as reported by study participants. At six months follow up, the vast majority of women (89%) were satisfied with the treatment. There were no AE attributed to the laser treatments.
Previous studies evaluating the efficacy of CO2 lasers in postmenopausal women were conducted 9, 20, 23, 24, 28, 31). The treatment sessions included 2–3 laser treatment provided once a month. The effect on tissue as seen in histology was noted after one or two months following treatment 20, 9), the effect on vaginal health score and VVA symptoms was noted at least one month following all treatment sessions 24, 26).
Observations in the current study suggest that our fractional CO2 laser is a safe and effective therapeutic option for the treatment of subjects who suffer from VVA. Our results are consistent with previous studies that have shown improving of VVA-related symptoms with the use of CO2 lasers 19, 32).
The clinical effect can be supported by previous histological studies, showing regeneration of the vaginal mucosa and submucosa, increased collagen and elastin, increased micro-vessel circulation, thickening of the submucosa and mucosa, and restoration of glycogen 33, 34).
In its 2013 position paper, the North American Menopause Society has defined recommendations for treatment of symptomatic VVA. The treatment paradigm is tiered, based on symptom severity and effect on overall well-being. The first line is non-hormonal local vaginal treatment, either lubricants during intercourse, or regular use of vaginal moisturizers. For moderate- to- severe, or mild-unresponsive VVA, the treatment is based on either systemic estrogen, or local low-dose estrogen, which is the preferred option. In the position paper, a few potential contraindications for local estrogen are noted: while local estrogen treatment offers sufficient estrogen to relieve symptoms with minimal systemic absorption, it still carries a class effect risk of venous thromboembolic events and for women with a history of breast or endometrial cancer, management should be done in coordination with the oncologist and may warrant close monitoring 35). Fractional CO2 laser therapy is a new technology that is highly effective in relief of VVA symptoms, most notably vaginal dryness, which causes great discomfort and adversely affects quality of life and sexual performance 36). Fractional CO2 laser treatments have been shown to be effective in VVA symptom relief in breast cancer survivors as well 37). Available clinical trial data with laser therapy for VVA, suggest that it is safe, with no significant side effects. Thus, it is a viable treatment option for women who cannot or do not want to be treated with hormone-based therapies 36). Large, long term, controlled clinical studies in a diverse population of post-menopausal women with VVA symptoms are still needed.
The strength of the current study is its prospective design. In addition, the effects of treatment were observed rapidly after the initial treatment and were sustained up to the completion of the study six months later. Conclusion: CO2 laser therapy can be considered a therapeutic option for post-menopausal women suffering from VVA symptoms. Further clinical trials with a longer follow up period are needed to explore the long-term effects of fractional CO2 laser treatment.
Acknowledgement
The author thank Shiri Diskin, PhD. for providing medical writing support, which was funded by Lumenis, Ltd. Yokneam Industrial Park, P.O.B 240 Yokneam 20692, Israel in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Disclosure statement
The study was sponsored by Lumenis Ltd. the manufacturer of the AcuPulse laser system evaluated in the study.
References
- 1: Heiman JR, Rupp H, Janssen E, Newhouse SK, Brauer M, Laan E. Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire. Horm. Behav. 2011;59:772-779. [DOI] [PubMed] [Google Scholar]
- 2: Hillard T. The postmenopausal bladder. Menopause Int. 2010;16:74-80. [DOI] [PubMed] [Google Scholar]
- 3: Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, et al. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am. J . Obstet. Gynecol. 2016;215:704-711. [DOI] [PubMed] [Google Scholar]
- 4: Kim H-K, Kang S-Y, Chung Y-J, Kim J-H, Kim M-R. The Recent Review of the Genitourinary Syndrome of Menopause. J. Menopausal Med. 2015;21:65-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5: Reimer A, Johnson L. Atrophic vaginitis signs, symptoms, and better outcomes. Nurse Pract. 2011;36:22-28. [DOI] [PubMed] [Google Scholar]
- 6: Nappi RE, Palacios S. Impact of vulvovaginal atrophy on sexual health and quality of life at postmenopause. Climacteric. 2014;17:3-9. [DOI] [PubMed] [Google Scholar]
- 7: Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am. J. Obstet. Gynecol. 2002;1:116-126. [DOI] [PubMed] [Google Scholar]
- 8: Omi T, Numano K. The role of the CO2 laser and fractional CO2 laser in dermatology. Laser Ther. 2014;23:49-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9: Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17:363-369. [DOI] [PubMed] [Google Scholar]
- 10: Mac Bride MB, Rhodes DJ, Shuster LT. Vulvovaginal atrophy. Mayo Clin. Proc. [Internet]. Elsevier; 2010. p. 87-94. Available from: http://www.sciencedirect.com/science/article/pii/S0025619611603145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11: Lee MS. Treatment of vaginal relaxation syndrome with an erbium: YAG laser using 90 and 360 scanning scopes: a pilot study & short-term results. Laser Ther. 2014;23:129-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12: Fistonić I, Guštek ŠF, Fistonić N. Minimally invasive laser procedure for early stages of stress urinary incontinence. J. Laser Health Acad. 2012;1:67-74. [Google Scholar]
- 13: Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, et al. Cancer and sexual problems. J. Sex. Med. 2010;7:349-373. [DOI] [PubMed] [Google Scholar]
- 14: Berlin AL, Hussain M, Phelps R, Goldberg DJ. A prospective study of fractional scanned nonsequential carbon dioxide laser resurfacing: a clinical and histopathologic evaluation. Dermatol. Surg. 2009;35:222-228. [DOI] [PubMed] [Google Scholar]
- 15: Sasaki GH, Travis HM, Tucker B. Fractional CO2 laser resurfacing of photoaged facial and non-facial skin: histologic and clinical results and side effects. J. Cosmet. Laser Ther. 2009;11:190-201. [DOI] [PubMed] [Google Scholar]
- 16: Weiss ET, Chapas A, Brightman L, Hunzeker C, Hale EK, Karen JK, et al. Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: quantitative volumetric scar improvement. Arch. Dermatol. 2010;146:133-140. [DOI] [PubMed] [Google Scholar]
- 17: Tierney EP, Hanke CW. Ablative fractionated CO2, laser resurfacing for the neck: prospective study and review of the literature. J. Drugs Dermatol. JDD. 2009;8:723-731. [PubMed] [Google Scholar]
- 18: Tierney EP, Hanke CW. Fractionated carbon dioxide laser treatment of photoaging: prospective study in 45 patients and review of the literature. Dermatol. Surg. 2011;37:1279-1290. [DOI] [PubMed] [Google Scholar]
- 19: Karcher C, Sadick N. Vaginal rejuvenation using energy-based devices. Int. J. Womens Dermatol. 2016;2:85-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20: Salvatore S, Maggiore ULR, Athanasiou S, Origoni M, Candiani M, Calligaro A, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845-849. [DOI] [PubMed] [Google Scholar]
- 21: ACOG Committee on Practice Bulletins--Gynecology. ACOG Practice Bulletin No. 85: Pelvic organ prolapse. Obstet. Gynecol. 2007;110:717-29. [DOI] [PubMed] [Google Scholar]
- 22: Bai SW, Lee JW, Shin JS, Park JH, Kim SK, Park KH. The predictive values of various parameters in the diagnosis of stress urinary incontinence. Yonsei Med J. 2004;45:287-292. [DOI] [PubMed] [Google Scholar]
- 23: Gaspar A, Addamo G, Brandi H. Vaginal fractional CO2 laser: a minimally invasive option for vaginal rejuvenation. Am. J. Cosmet. Surg. 2011;28:156-162. [Google Scholar]
- 24: Pitsouni E, Grigoriadis T, Tsiveleka A, Zacharakis D, Salvatore S, Athanasiou S. Microablative fractional CO2-laser therapy and the genitourinary syndrome of menopause: An observational study. Maturitas. 2016;94:131-136. [DOI] [PubMed] [Google Scholar]
- 25: Athanasiou S, Pitsouni E, Antonopoulou S, Zacharakis D, Salvatore S, Falagas ME, et al. The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric. 2016;19:512-518. [DOI] [PubMed] [Google Scholar]
- 26: Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch. Gynecol. Obstet. 2016;294:841-846. [DOI] [PubMed] [Google Scholar]
- 27: Bachmann GA, Notelovitz M, Kelly SJ, Thompson C, Owens A. Long-term non-hormonal treatment of vaginal dryness. Clin Pr. Sex. 1992;8:3-8. [Google Scholar]
- 28: Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80:296-301. [DOI] [PubMed] [Google Scholar]
- 29: Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zerbinati N, et al. Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climacteric. 2015;18:219-225. [DOI] [PubMed] [Google Scholar]
- 30: Sutton KS, Boyer SC, Goldfinger C, Ezer P, Pukall CF. To lube or not to lube: experiences and perceptions of lubricant use in women with and without dyspareunia. J. Sex. Med. 2012;9:240-250. [DOI] [PubMed] [Google Scholar]
- 31: Pitsouni E, Grigoriadis T, Falagas M, Tsiveleka A, Salvatore S, Athanasiou S. Microablative fractional CO2 laser for the genitourinary syndrome of menopause: power of 30 or 40 W? Lasers Med. Sci. 2017;1-8. [DOI] [PubMed] [Google Scholar]
- 32: Menachem A, Alexander B, Martinec KS, Gutman G. THE EFFECT OF VAGINAL CO2 LASER TREATMENT ON STRESS URINARY INCONTINENCE SYMPTOMS. 2016; Available from: http://www.femilift.com.ar/files/papers/SUI_Retrospective_F_HR.pdf [Google Scholar]
- 33: Salvatore S. Menopausal Vaginal Atrophy Treatment with Microablative Fractional CO2 Laser. A New Approach Deka White Paper. [Google Scholar]
- 34: Zerbinati N, Serati M, Origoni M, Candiani M, Iannitti T, Salvatore S, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med. Sci. 2015;30:429-436. [DOI] [PubMed] [Google Scholar]
- 35: Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause N. Y. N. 2013;20:888-902; quiz 903–904. [DOI] [PubMed] [Google Scholar]
- 36: Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10-5. [DOI] [PubMed] [Google Scholar]
- 37: Siliquini GP, Tuninetti V, Bounous VE, Bert F, Biglia N. Fractional CO2 laser therapy: a new challenge for vulvovaginal atrophy in postmenopausal women. Climacteric J. Int. Menopause Soc. 2017;20:379-84. [DOI] [PubMed] [Google Scholar]


