Abstract
Introduction:
According to the World Health Organization data repository, the average life expectancy at birth for Singapore in 2015 has risen to 83.4 years, and many octogenarians (OG) remain active socioeconomically. The aim of this study is to compare the improvement and the impact of comorbidities on functional recovery after total knee arthroplasty (TKA) between OG and their younger counterparts.
Methods:
This is a retrospective study of prospectively collected data from a single institution arthroplasty register. Between January 2006 and December 2011, 209 OG with primary knee osteoarthritis underwent TKA. Each OG (mean age 82 ± 2.1) was then carefully matched to a younger control group (YG, mean age 66 ± 4.5). Their postoperative outcomes measured include Oxford Knee Score (OKS), SF36-Physical Function (SF-PF), and knee society rating score comprising of Knee Score (KS) and Function Score (FS). Their respective degrees of improvement were compared and adjusted for their baseline comorbidities, measured using the Deyo-Charlson Comorbidity Index (D-CCI).
Results:
There were more comorbidities among the OG (P < .05). Both groups saw the largest improvement (P < .05) during the first 6 months. There was no statistical significance between their improvement for OKS, KS, and FS between baseline and 6 months and OKS, FS, and SF-PF between 6 and 24 months. Adjusted for D-CCI using linear regression, the above results remained largely unchanged.
Discussion:
In our study, both groups showed significant improvement across all functional outcomes, especially during the first 6 months. The improvement observed in OG at 6 and 24 months was comparable to that of YG, despite an overall higher baseline D-CCI.
Conclusions:
Total knee arthroplasty is a viable treatment option for the OG, offering good functional outcomes and results at 6 and 24 months when compared to their younger counterparts.
Keywords: octogenarian, arthroplasty, knee osteoarthritis, clinical outcome scores, knee replacement
Introduction
Total knee arthroplasty (TKA) has been widely regarded as an effective and safe treatment in the management of total knee osteoarthritis, offering pain relief and good functional improvement.1,2 The number of joint replacements performed over the years has risen substantially,5 leading to a projected increase in surgical load and health-care resource allocation.6,7
Besides improving quality of life, there are also potential cost benefits in offering TKA to the elderly population.8 This is especially relevant in developed countries like Singapore where the life expectancy of male and female has risen from 73.1 and 77.6 in 1990 to 80.4 and 84.9 in 2015, respectively.9 Although TKA improves functional outcomes and patient satisfaction among the octogenarian (OG; above age 80 years),10–12 it still remains unclear whether they can recover fast enough in order for them to reap the benefits. More importantly, there is insufficient data comparing the functional outcomes of the OG with that of the younger counterparts, as well as whether comorbidities play a significant role in affecting their recovery. We hypothesize that in the presence of well-controlled comorbidities and optimal patient selection, OG will reap the same level of benefits from the procedure as that of their younger counterparts. The aim of our study was (1) to compare the improvement between the OG and their younger counterparts, (2) to determine if the OG have more baseline comorbidities, and (3) to study the impact of comorbidities on the functional recovery after TKA.
Materials and Methods
We retrospectively studied prospectively collected data from a large tertiary hospital in Singapore. Out of 7532 patients who underwent TKA from January 2006 to December 2011 at our single institution arthroplasty register, 209 OG who completed their 6- and 24-month follow-up at our Orthopaedic Diagnostic Centre were identified. To establish a comparator control group, we performed a 1:1 match for each of these 209 OG with a younger patient (below age 80) based on gender, body mass index (BMI), operating surgeon, site of TKA, history of contralateral TKA, and primary diagnosis.
Deyo-Charlson Comorbidity Index
All patients were assessed for their comorbidities prior to surgery, graded using the Deyo-Charlson Comorbidity Index (D-CCI).13 Their D-CCI scores were calculated based on the 17 defined comorbid conditions, each assigned to a weighted scale from 1 to 6. All subjects were subcategorized into D-CCI of 0, 1, 2, and more than 3.
Functional Outcomes
Clinical information was collected prospectively by our institution Orthopedic Diagnostic Center at each follow up visit, scheduled 6 and 24 months postprocedure. Pre and postoperative functional outcomes were measured using Oxford Knee Score (OKS),14 SF36-Physical Function (SF-PF), Knee Society Rating Score comprising of Knee Score (KS), and Function Score (FS).15 Oxford Knee Score is a patient-reported outcome questionnaire, grading from 12 (best) to 60 (worse), which is used to assess the patient’s perspective of the outcome after TKA. The KS takes into consideration, pain, knee stability, range of motion, and implant alignment, while FS evaluates function of daily living including walking distance, ability to climb stairs, and the requirement of walking assistance. The functional outcomes (OKS, SF-PF, KS, and FS) at each time frame were computed as mean and standard deviation. Within each group, the minimal clinically important difference (MCID) for both Knee Society Score and OKS were used to determine whether the improvement at 6 and 24 months was clinically significant when compared to their baseline.
Degree of Improvement
The degree of improvement between each follow-up was calculated based on the difference in score. For example, the degree of improvement for KS between 0 and 6 months was calculated by subtracting the KS value at 6 months from its baseline score.
Statistical Analysis
All statistical comparisons were made using the SPSS version 21 (SPSS, Inc., Chicago, Illinois, USA). The difference in functional outcomes within each group was analyzed using analysis of variance with least significance difference method. We compared the difference in improvement between both groups using independent t test. To account for the influence of baseline comorbidities, the P values of the degree of improvement compared between both groups were D-CCI adjusted using linear regression method. The threshold for significance was < .05.
A sample size of n per group is adequate to detect an effect size of (4/square root n) with an 80% power at α = .05 using a 2-tailed t test. In our study, with a sample size of 209, our effect size was computed as .28. Using Cohen d for a t test, this study is considered to have a “small” effect size. This study was approved by the Singhealth Centralised Institutional Review Board, Singapore (CIRB Ref. No: 2016/3053)
Results
A total of 209 OG were studied. The mean age was 82.1 ± 2.1 years for the OG and 66.1 ± 4.5 years for the YG. Their average BMIs were 26.4 and 26.6 respectively (P > .05). There were more baseline comorbidities among the OG, with about 49.8% yielding a D-CCI score of more than 1, as compared to 34.9% in the YG (Table 1).
Table 1.
Preoperative Characteristics and Baseline Functional Scores.
| Baseline Functional Scores and Comorbidities | |||
|---|---|---|---|
| Control (YG) | Octogenarian (OG) | P value | |
| Age | 66.1 | 82.1 | < .05 |
| BMI | 26.6 | 26.4 | .430 |
| D-CCI | |||
| 0 | 65.1% | 49.8% | < .05 |
| 1 | 26.8% | 36.4% | |
| 2 | 7.7% | 11.0% | |
| >3 | 0.5% | 2.9% | |
| Functional Scores | |||
| Oxford Knee Score (OKS) | 35.15 ± 8.325 | 38.63 ± 8.816 | < .05 |
| Knee Score Rating Score | |||
| Knee Score | 38.10 ± 18.527 | 36.77 ± 19.684 | 0.477 |
| Function Score | 52.70 ± 18.140 | 39.50 ± 20.200 | < .05 |
| SF36–Physical Function | 37.70 ± 22.970 | 25.24 ± 21.34 | < .05 |
Abbreviations: BMI, body mass index; D-CCI, Deyo-Charlson Comorbidity Index; YG, younger control group.
Bold values signify (P < 0.05).
Functional Outcomes Within Each Group
Both groups saw a significant improvement (P < .05) across all 4 function outcomes (OKS, KS, FS, and SF-PF) at 6 and 24 months as compared to their preoperative scores. For the YG (Table 2, Figure 1A): their functional outcomes at each follow-up (baseline-6 months-24 months) were OKS (35.15-19.98-17.92, P < .05), KS (38.10-83.06-86.21, P < .05), FS (52.70-69.43-73.44, P < .05), and SF-PF (37.70-64.98-66.77, P < .05). For the OG (Table 2, Figure 1B): their results were OKS (38.63-22.85-20.84, P < .05), KS (36.77-83.33-84.44, P < .05), FS (39.50-52.87-56.77, P < .05), and SF-PF (25.24-46.41-49.59, P < .05). For both groups, the largest and most significant improvement was observed during the first 6 months after surgery.
Table 2.
Functional Outcome Scores Across 6 and 2 Years.
| Outcome | Baseline | 6 months | Improvement From Baseline to 6 months (CI; P Value) | 24 Months | Improvement From 6 to 24 Months (CI; P Value) | Improvement From Baseline to 24 Months (CI; P Value) |
|---|---|---|---|---|---|---|
| Control group (YG) | ||||||
| OKS | 35.15 | 19.98 | 15.18 (13.99-16.37; < .05) | 17.92 | 2.05 (0.86 to 3.24; < .05) | 17.23 (16.04-18.42; < .05) |
| FS | 52.70 | 69.43 | 16.72 (13.38-20.07; < .05) | 73.44 | 4.02 (0.67 to 7.37; < .05) | 20.74 (17.40-24.09; < .05) |
| KS | 38.10 | 83.06 | 44.96 (42.32-47.60; < .05) | 86.21 | 3.14 (0.51 to 5.78; < .05) | 48.11 (45.47-50.74; < .05) |
| SF-PF | 37.70 | 64.98 | 27.27 (23.23-31.32; < .05) | 66.77 | 1.79 (−2.25 to 5.84; .384) | 29.07 (25.02-33.11; < .05) |
| Octogenarian Group (OG) | ||||||
| OKS | 38.63 | 22.85 | 15.78 (14.35-17.21; < .05) | 20.84 | 2.01 (0.59 to 3.44; < .05) | 17.79 (16.37-19.22; < .05) |
| FS | 39.50 | 52.87 | 13.37 (9.52-17.23; < .05) | 55.77 | 2.89 (−0.96 to 6.75; .141) | 16.27 (12.42-20.12; < .05) |
| KS | 36.77 | 83.33 | 46.56 (43.73-49.40; < .05) | 84.44 | 1.11 (−1.73 to 3.94; = .444) | 47.67 (44.84-50.50; < .05) |
| SF-PF | 25.24 | 46.41 | 21.17 (16.63-25.72; < .05) | 49.59 | 3.18 (−1.36 to 7.73; .170) | 24.35 (19.81-28.90; < .05) |
Abbreviations: FS, Function Score; KS, Knee Score; OKS, Oxford Knee Score; SF-PF, SF36-Physical Function; YG, younger control group.
Figure 1.
Functional Outcome Scores across 6 and 2 years (A) YG (B) OG. OKS*: A lower score indicates better outcome. OG indicates octogenarian; OKS, Oxford Knee Score.
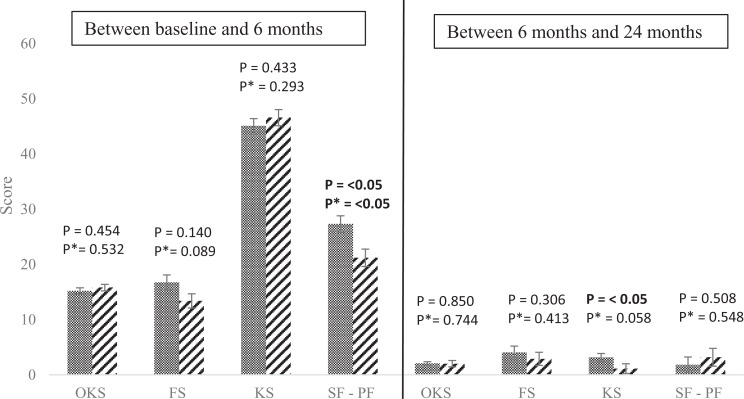
Improvement Observed Between Both Groups
Comparing the improvement between both groups (control:OG), there were no statistical significance (P > .05) between their mean difference from baseline to 6 months for OKS (15.19:15.78, P = .454), KS (44.96:46.56, P = 0.433), and FS (16.72:13.37, P = .140). Between 6 and 24 months, their difference remained statistically insignificant for OKS (2.05:2.01, P = 0.850), FS (4.02:2.89, P = .306), and SF-PF (1.79:3.18, P = .508). See Table 3 and Figure 2 for more information.
Table 3.
Comparison of Improvement Between YG and OG.
| YG | OG | Confidence Interval | P Value | P Value (CCI Adjusted) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Between baseline and 6 months | ||||||
| OKS | 15.18 | 15.78 | −0.977 | 2.183 | .454 | .532 |
| FS | 16.72 | 13.37 | −0.314 | 7.013 | .140 | .089 |
| KS | 44.96 | 46.56 | −5.617 | 2.411 | .433 | .293 |
| SF-PF | 27.27 | 21.17 | 1.775 | 10.426 | .006 | .004 |
| Between 6 months and 2 years | ||||||
| OKS | 2.05 | 2.01 | −1.019 | 1.095 | .850 | .744 |
| FS | 4.02 | 2.89 | −4.404 | 2.156 | .306 | .413 |
| KS | 3.14 | 1.11 | −4.265 | 0.188 | .019 | .058 |
| SF-PF | 1.79 | 3.18 | −2.834 | 5.609 | .508 | .548 |
Abbreviations: FS, Function Score; KS, Knee Score; OKS, Oxford Knee Score; SF-PF, SF36-Physical Function; YG, younger control group.
Bold values signify (P < 0.05).
Figure 2.
Comparison between their improvements, calculated based on the difference in scores between each time frame. P* defined as P value after CCI adjusted.
Effect of Comorbidities on Functional Recovery
In this study, we used linear regression method to adjust for the effect of their baseline differences in comorbidities on functional recovery. Taking into consideration their premorbid D-CCI, we saw no difference in the results at each of the 2 time frames for OKS, FS, and SF-PF.
Discussions
As the elderly population grows over the next decade, it is necessary for us to study and compare their functional recovery to that of a younger group (YG). As such, it is imperative that we evaluate the effects of age and comorbidities on their clinical outcomes, so as to provide better evidence in determining if an elderly patient can benefit as much as their younger counterparts. In our study, both groups showed a significant improvement across all functional outcomes, with the most substantial increase taking place during the first 6 months. At 6 and 24 months, the improvement and recovery from baseline observed in an elderly was comparable to that of a younger patient. Given their advanced age at the time of surgery and the overall outlook of life expectancy worldwide,3,4 we can highlight that an OG will still be able to reap the benefits of TKA.
Improvements in Knee Society Rating Scores
The Knee Society Clinical Rating System (KSS) is one of the most popular and commonly used questionnaire in the measurement of function recovery after TKA.16 It takes into consideration both objective measurements such as motion and implant alignments as well as subjective evaluation obtained from patients’ response. We saw, in our study, a comparable increase in KSS scores between both groups at each time frame, which was consistent with the findings presented in the current literature.11,17,18 Although the MCID for KSS has not been well established by the orthopedic community, recent studies have suggested that an MCID of more than 6.1 to 6.4 for FS and 5.3 to 5.9 for KS should be interpreted as clinically significant.19 Most studies have concurred that, within the OG, significant improvement can be seen in KS,11,17,18,20 which was also observed in our cohort. The improvement in FS seemed to be less consistent. Some authors have attributed this to the difference in information gathered and the likelihood of baseline comorbidities and other age-related factors affecting FS more than KS, thus inhibiting its improvements.18,20 However, we showed in our study that in the absence of adjudication for comorbidities, significant improvement in FS was still seen at 6 and 24 months.
Improvements in OKS
Oxford Knee Score has been widely used as an evaluation tool to assess the outcome of knee replacements since it was first described.14,21 It is a self-administered quality of life questionnaire that has been well validated in various languages,22–25 and it has also been evaluated for its suitability in the evaluation of knee function before and after knee replacement surgery.26 The MCID estimated for OKS has to be reported as an improvement of at least 4 points14,27,28 in order for it to be considered clinically relevant. In our study, both groups met the MCID at 6 and 24 months.
Comparison of Functional Outcomes Between OG and YG
The comparison of the FS scores between both groups at baseline, 6 months, and 24 months were statistically significant: baseline (52.70:39.50, P < .05); 6 months (69.43:52.87, P < .05); 24 months (73.44:56.77, P < .05). Similar observations were also seen for OKS and SF-PF. These differences could be attributed to factors such as age, activity level, and other concomitant medical problems. As such, comparing their scores at each discrete time point may not be the best method to compare the functional outcomes between both groups and their improvements. In this study, we calculated instead, their absolute improvement at 6 and 24 months in order to minimize the effect of their baseline functional difference. We found that by measuring their improvement at each follow-up, there was no difference in their FS between the 2 groups at 6 months (16.72:13.37, P = .140) and 24 months (4.02:2.89, P = .306). This shows that the potential to improve after TKA among the OG were comparable to that of the YG at each of those time period.
For OKS, there was again no statistical difference in their improvement between the 2 groups at 6 months (15.19:15.78, P = .454) and 24 months (2.05:2.01, P = .850). The result was consistent with other studies that utilize mean improvement in their functional outcome evaluation.10,29
Effects of D-CCI on Functional Outcomes
The D-CCI is a validated clinical evaluation tool,13 derived from the original Charlson comorbidities index 30,31 that was first published in 1987. It is a summative score, calculated based on a weighted scale of 17 comorbidities. It has been shown by various studies that increasing comorbidities may lead to (1) worsening functional outcomes,32–34 (2) poorer survival of implants,35 (3) increased complication rates,36 (4) higher likelihood of being transferred to a rehabilitation facility,29,37,38 and (5) may require a more intensive physical therapy regime.39 In addition, a higher D-CCI was also determined to be associated with a higher risk of poor functional outcomes at 2 years after knee replacement.40 In our study, we found that OG have more baseline comorbidities as compared to their younger counterparts. In spite of this, the comparison between their mean improvements in functional outcome scores remained largely unchanged after being adjusted for preoperative health.
Limitations
We recognize some limitations in our study. Firstly, we lost a significant number of patients to follow up with. Out of the 342 OG who underwent TKA during the 5-year period, 285 patients returned at 2-year review, out of which 209 OG with all required functional scores were analyzed in this study. This could be attributed to not only the higher possibility of anticipated death due to old age but also the difficulty in following up with these patients due to compliance issues. Our overall lost to follow-up rate of 16.7% was, however, comparable to many other studies (14%-18%).18,41,42 Secondly, as this is a retrospective review on patients who have undergone TKA, OG who were deemed unsuitable or not offered surgery for any reasons were not captured in the database. Thirdly, in order to minimize the effect of confounding factors, we carefully matched each OG to a younger control subject based on as many confounding factors as we can, except for age and comorbidities.
In addition, since TKA is still not the standard of care for treating knee osteoarthritis among the OG, the preoperative patient selection process would have already been biased toward those who are healthier. Lastly, we did not take into consideration other factors such as additional resources including rehabilitation programs, socioeconomic influence, and family involvement in the care of the OG, just to name a few.
Conclusion
Total knee arthroplasty offers excellent functional outcomes in OG. The improvement across most measures over 6 and 24 months were comparable to that of their younger counterparts despite higher overall baseline comorbidities. Age and higher D-CCI may not be limiting factors against recommending TKA to the OG. We believe that TKA is a viable treatment option for advanced knee osteoarthritis in the OG.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Skou ST, Roos EM, Laursen MB, et al. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015;373(17):1597–1606. doi:10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 2. Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271(17):1349–1357. doi:10.1001/jama.1994.03510410061034. [PubMed] [Google Scholar]
- 3. WHO | Life expectancy. WHO. http://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends_text/en/. Updated 2018. Accessed June 21, 2016.
- 4. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi:10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kremers HM, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–1397. doi:10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim S. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997-2004. Arthritis Rheum. 2008;59(4):481–488. doi:10.1002/art.23525. [DOI] [PubMed] [Google Scholar]
- 7. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94(3):201–207. doi:10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Karuppiah SV, Banaszkiewicz PA, Ledingham WM. The mortality, morbidity and cost benefits of elective total knee arthroplasty in the nonagenarian population. Int Orthop. 2008;32(3):339–343. doi:10.1007/s00264-007-0324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Population And Vital Statistics | Ministry of Health. https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Population_And_Vital_Statistics.html. Published 2016. Updated August 16, 2017. Accessed June 21, 2016.
- 10. Clement ND, MacDonald D, Howie CR, Biant LC. The outcome of primary total hip and knee arthroplasty in patients aged 80 years or more. J Btwo Joint Surg Br. 2011;93-B(9):1265–1270. doi:10.1302/0301-620X.93B9.25962. [DOI] [PubMed] [Google Scholar]
- 11. Kuo FC, Hsu CH, Chen WS, Wang JW. Total knee arthroplasty in carefully selected patients aged 80 years or older. J Orthop Surg. 2014;9:61 doi:10.1186/s13018-014-0061-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shah AK, Celestin J, Parks ML, Levy RN. Long-term results of total joint arthroplasty in elderly patients who are frail. Clin Orthop Relat Res. 2004;(425):106–109. [DOI] [PubMed] [Google Scholar]
- 13. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 14. Murray DW, Fitzpatrick R, Rogers K, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89(8):1010–1014. doi:10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 15. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop. 1989;(248):13–14. [PubMed] [Google Scholar]
- 16. Dowsey MM, Choong PFM, Dowsey MM, Choong PFM. The utility of outcome measures in total knee replacement surgery, the utility of outcome measures in total knee replacement surgery. Int J Rheumatol. 2013;2013:e506518 doi:10.1155/2013/506518, 10.1155/2013/506518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Joshi AB, Markovic L, Gill G. Knee arthroplasty in octogenarians: results at 10 years. J Arthroplasty. 2003;18(3):295–298. doi:10.1054/arth.2003.50063. [DOI] [PubMed] [Google Scholar]
- 18. Kennedy JW, Johnston L, Cochrane L, Boscainos PJ. Total knee arthroplasty in the elderly: does age affect pain, function or complications? Clin Orthop. 2013;471(6):1964–1969. doi:10.1007/s11999-013-2803-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;25(11):1–6. doi:10.1007/s00167-016-4208-9. [DOI] [PubMed] [Google Scholar]
- 20. Seo JG, Moon YW, Cho BC, et al. Is total knee arthroplasty a viable treatment option in octogenarians with advanced osteoarthritis? Knee Surg Relat Res. 2015;27(4):221–227. doi:10.5792/ksrr.2015.27.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80(1):63–69. [DOI] [PubMed] [Google Scholar]
- 22. Gonçalves RS, Tomás AM, Martins DI. Cross-cultural adaptation and validation of the Portuguese version of the Oxford Knee Score (OKS). Knee. 2012;19(4):344–347. doi:10.1016/j.knee.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 23. Ornetti P, Parratte S, Gossec L, et al. Cross-cultural adaptation and validation of the French version of the Knee injury and Osteoarthritis Outcome Score (KOOS) in knee osteoarthritis patients. Osteoarthritis Cartilage. 2008;16(4):423–428. doi:10.1016/j.joca.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 24. Xie F, Li SC, Lo NN, et al. Cross-cultural adaptation and validation of Singapore English and Chinese Versions of the Oxford Knee Score (OKS) in knee osteoarthritis patients undergoing total knee replacement. Osteoarthritis Cartilage. 2007;15(9):1019–1024. doi:10.1016/j.joca.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 25. Naal FD, Impellizzeri FM, Sieverding M, et al. The 12-item Oxford Knee Score: cross-cultural adaptation into German and assessment of its psychometric properties in patients with osteoarthritis of the knee. Osteoarthritis Cartilage. 2009;17(1):49–52. doi:10.1016/j.joca.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 26. Jenny JY, Diesinger Y. The Oxford Knee Score: compared performance before and after knee replacement. Orthop Traumatol Surg Res. 2012;98(4):409–412. doi:10.1016/j.otsr.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 27. Clement ND, MacDonald D, Simpson AHRW. The minimal clinically important difference in the Oxford Knee Score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1933–1939. doi:10.1007/s00167-013-2776-5. [DOI] [PubMed] [Google Scholar]
- 28. Beard DJ, Harris K, Dawson J, et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol. 2015;68(1):73–79. doi:10.1016/j.jclinepi.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Williams DP, Price AJ, Beard DJ, et al. The effects of age on patient-reported outcome measures in total knee replacements. Bone Joint J. 2013;95-B(1):38–44. doi:10.1302/0301-620X.95B1.28061. [DOI] [PubMed] [Google Scholar]
- 30. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 31. Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG. Morbidity during hospitalization: can we predict it? J Chronic Dis. 1987;40(7):705–712. [DOI] [PubMed] [Google Scholar]
- 32. Elmallah R, Cherian J, Robinson K, Harwin S, Mont M. The Effect of Comorbidities on Outcomes following Total Knee Arthroplasty. J Knee Surg. 2015;28(05):411–416. doi:10.1055/s-0035-1549023. [DOI] [PubMed] [Google Scholar]
- 33. Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722–1728. doi:10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 34. Fitzgerald JD, Orav EJ, Lee TH, et al. Patient quality of life during the 12 months following joint replacement surgery. Arthritis Care Res. 2004;51(1):100–109. doi:10.1002/art.20090. [DOI] [PubMed] [Google Scholar]
- 35. Jämsen E, Peltola M, Eskelinen A, Lehto MUK. Comorbid diseases as predictors of survival of primary total hip and knee replacements: a nationwide register-based study of 96 754 operations on patients with primary osteoarthritis. Ann Rheum Dis. December 2012:annrheumdis - 2012-202064. doi:10.1136/annrheumdis-2012-202064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jain NB, Guller U, Pietrobon R, Bond TK, Higgins LD. Comorbidities increase complications in patients having arthroplasty. Clin Orthop. 2005;(435):232–238. [DOI] [PubMed] [Google Scholar]
- 37. Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86(10):2179–2186. [DOI] [PubMed] [Google Scholar]
- 38. Munin MC, Kwoh CK, Glynn N, Crossett L, Rubash HE. Predicting discharge outcome after elective hip and knee arthroplasty. Am J Phys Med Rehabil. 1995;74(4):294–301. [DOI] [PubMed] [Google Scholar]
- 39. Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003;83(8):696–706. [PubMed] [Google Scholar]
- 40. Singh JA, O’Byrne M, Harmsen S, Lewallen D. Predictors of moderate-severe functional limitation after Primary Total Knee Arthroplasty (TKA): 4,701 TKAs at 2-years and 2,935 TKAs at 5-years. Osteoarthr Cartil OARS Osteoarthr Res Soc. 2010;18(4). doi:10.1016/j.joca.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Alfonso DT, Howell RD, Strauss EJ, Di Cesare PE. Total hip and knee arthroplasty in nonagenarians. J Arthroplasty. 2007;22(6):807–811. doi:10.1016/j.arth.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 42. Pavone V, Boettner F, Fickert S, Sculco TP. Total condylar knee arthroplasty: a long-term followup. Clin Orthop. 2001;(388):18–25. [DOI] [PubMed] [Google Scholar]