Abstract
Background:
Outcomes after anterior cruciate ligament reconstruction (ACLR) are highly variable. Previous studies have failed to report the relationship between fear, objective measures of function, and reinjury rates. The purpose of this study was to determine whether fear was related to functional performance measures and risk of second ACL injury after ACLR and return to sport (RTS).
Hypothesis:
Fear will be associated with performance on functional testing and second ACL injury rate.
Study Design:
Prospective cohort study.
Level of Evidence:
Level 2.
Methods:
A total of 40 patients cleared to RTS after ACLR completed the Tampa Scale of Kinesiophobia (TSK-11), hop testing, and quadriceps strength testing, bilaterally. Patients were tracked for 12 months after RTS to identify the incidence of second ACL injury. Chi-square analyses determined whether patients with high fear (TSK-11, ≥17) were more likely to have lower levels of activity, greater asymmetry on functional testing, and higher reinjury rates.
Results:
Patients with greater fear on the TSK-11 (≥17) at RTS were 4 times (odds ratio [OR], 3.73; 95% CI, 0.98-14.23) more likely to report lower levels of activity, 7 times (OR, 7.1; 95% CI, 1.5-33.0) more likely to have a hop limb symmetry lower than 95%, and 6 times (OR, 6.0; 95% CI, 1.3-27.8) more likely to have quadriceps strength symmetry lower than 90%. Patients who went on to suffer an ipsilateral second ACL injury had a greater TSK-11 score at the time of RTS (mean, 19.8 ± 4.0) than those who did not suffer a second ACL injury (mean, 16.4 ± 3.6) (P = 0.03). Patients with a TSK-11 score of 19 or greater at the time of RTS were 13 times (relative risk, 13.0; 95% CI, 2.1-81.0) more likely to suffer a second ACL tear within 24 months after RTS.
Conclusion:
Patients with greater self-reported fear were less active, presented with lower single-leg hop performance and isometric quadriceps strength, and had an increased risk of suffering a second ACL injury in the 24 months after RTS.
Clinical Relevance:
Self-reported fear of movement/reinjury after ACLR at the time of RTS may be an important measure to incorporate into discharge criteria prior to release to return to pivoting and cutting sports after ACLR.
Keywords: ACL reconstruction, second injury, fear, functional performance
More than 200,000 anterior cruciate ligament (ACL) injuries occur annually in the United States.27 Athletes who wish to return to pivoting and cutting sports often seek ACL reconstruction (ACLR) to maximize stability and function of the knee. Recent evidence suggests less than 50% of patients who undergo ACLR return to their previous level of activity.3,5 Furthermore, up to 30% of athletes sustain a second ACL injury within 24 months of returning to sport.25 Currently, there is a lack of consensus regarding the criteria that should be used to determine whether an athlete is ready to return to sport (RTS).7,8
Current rehabilitation protocols and RTS clearance criteria after ACLR are primarily based on time from surgical reconstruction and measures of physical function.8,18 Most RTS discharge criteria include some combination of time since surgery, subjective reports of function, lower extremity strength measurements, functional tests (eg, hop testing), and/or quality of lower extremity movements.1 Ardern et al4 cited psychological readiness as the factor most strongly associated with successful RTS. Furthermore, several studies have suggested fear of reinjury as a contributing, if not primary, factor for patients not returning to sport.2,6,19,28 Despite this, minimal to no consideration of the psychological readiness of the patient to RTS has been included in RTS algorithms after ACLR, as traditional measures such as strength, hop test performance, and patient-reported outcomes on knee-specific measures continue to dominate RTS algorithms.8,15,18,20 In addition, there is limited evidence reporting the relationship between patient-reported fear, objective measures of function, and rates of second injury after ACLR and RTS.
The purpose of this study was to determine whether self-reported fear at time of RTS was related to activity level at time of RTS, objective clinical measures of function at time of RTS, and incidence of second ACL injury within the first 24 months after RTS. This study is a necessary step toward understanding the role fear plays in determining an athlete’s readiness to RTS. The first tested hypothesis was that increased patient-reported fear at the time of RTS would be associated with lower levels of activity and reduced strength and performance on single-leg hop testing at RTS. Additionally, the authors hypothesized that patient-reported fear at the time of RTS would predict patients at greater risk of a second ACL injury after ACLR and RTS.
Methods
Participants
The study was approved by the institutional review board at Cincinnati Children’s Hospital (IRB No. 2008-0514), and informed consent was obtained from all participants and guardians (if applicable) before testing. A total of 40 participants were recruited as a portion of a larger, longitudinal, prospective cohort study on outcomes in patients after ACLR between March 2013 and September 2015. All patients had recently undergone primary ACLR, completed rehabilitation, and were cleared to return to their prior level of activity by their surgeon and rehabilitation team. Patients were primarily recruited through orthopaedic surgery and physical therapy practices in the region, and therefore, the authors controlled neither the rehabilitation plan of care nor RTS criteria for the study participants.
Inclusion criteria required participants to be between 10 and 25 years of age, be released by both their physician and rehabilitation team to return to all high-level athletic activity, and intend to return to cutting and pivoting (level 1 or 2)11 sports for at least 50 hours per year. The testing session occurred within 4 weeks of RTS clearance, and all testing measures were performed during the same testing session. Exclusion criteria for this study included a history of low back injury or either lower extremity injury or surgery (beyond ACLR) requiring the care of a physician in the past year or a concomitant ligament injury (beyond grade 1 medial collateral ligament injury) in the involved limb.
Patient-Reported Fear
At the time of RTS, each participant completed the shortened version of the Tampa Scale of Kinesiophobia (TSK-11). Scores on the TSK-11 range from 11 to 44, with higher scores indicating greater fear of movement/reinjury. The TSK-11 assesses pain-related fear of movement/reinjury and has been previously used to assess fear of movement/reinjury in patients who have undergone ACLR.10,13 The TSK-11 is a shortened form of the original version and has been shown to have comparable psychometric properties in patients with low back pain.34 Scores on the TSK-11 were used to divide patients into 2 groups: those reporting high fear and those reporting low fear. Patients with a score ≥17 were placed into the high-fear group, and scores ≤16 were placed into the low-fear group. The score of 17 was used as previous studies have demonstrated that scores of 17 and higher indicate patients with greater fear after ACLR.10
Activity Level
The Marx Activity Rating Scale (Marx) was used to determine the participants’ activity level at time of RTS. The Marx is a 4-item questionnaire that assesses how frequently the patient participates in running, cutting, and pivoting activities.23 Each item is scored on a 5-point ordinal scale, with 0 being the lowest (indicating the activity is done less than 1 time per month) and 4 the highest (indicating the activity is completed 4 or more times per week).23 Patients with scores of 15 or less were placed into the low activity group, whereas those with a score of 16 were placed in the high activity group. A score of 16 indicates the patient participated in running, cutting, pivoting, and decelerating activities at least 4 days per week,23 comparable to the level of activity of an athlete participating on a high school or collegiate athletic team.
Single-Leg Hop Measurement
Participants performed a series of 4 single-leg hop tests as a measure of function: single-leg hop for distance, triple hop for distance, triple-crossover hop for distance, and 6-m timed hop. These hop tests have good inter- and intrarater reliability29 and are commonly used in clinical practice. The single-leg hop for distance was the first test performed by all participants. Each participant was given a single practice trial followed by 2 measurement trials on each limb. A limb symmetry index (LSI) was calculated based on the average of the 2 trials on the involved and uninvolved limb: LSI = [involved score/uninvolved score] × 100%. The LSI is used to quantify function on hop tests, with scores less than 100% indicating deficits of the involved limb.9,12 For this study, various levels of limb symmetry were evaluated, including an LSI value of ≤95% and ≤90%, as recent reviews of limb symmetry prior to RTS suggest a minimum of 90% LSI is required prior to RTS.14,36 Furthermore, 1 study demonstrated that a 90% LSI was still inadequate to estimate knee function and may be related to second ACL injury risk.32
Strength
Isometric quadriceps femoris (QF) strength was assessed using a Biodex isokinetic dynamometer (Biodex Medical Systems Inc) during a maximum voluntary isometric contraction (MVIC). The patients were seated in a chair with hips flexed to 90° and knee flexed to 60°. The knee joint axis of rotation was aligned with the dynamometer axis, and the dynamometer resistance pad was secured to the anterior aspect of the distal leg. The pelvis and thigh were stabilized with straps. Real-time visual and verbal feedback was provided during the test to ensure maximum effort by the participant. After 1 practice trial, 3 recorded maximum-effort trials (5 seconds in duration, separated by 15 seconds of rest) were completed for each knee. The uninvolved side was always tested first. This procedure has been used previously to quantify quadriceps torque in individuals undergoing ACLR and has yielded reliable measurements.21 The peak torques of the 3 trials were averaged and then normalized to body weight (kg). The mean normalized peak torque value for each limb was used for further analysis and calculation of the quadriceps index (QI) using the equation: QI = [involved QF MVIC/uninvolved QF MVIC] × 100%. An LSI deficit in QI of ≤90% was used as a cutoff, as current literature demonstrates this level of strength deficit correlates with altered movement patterns,16,30 functional performance deficits,31 and reduced patient-reported function.35
Injury Tracking
All patients were tracked for 24 months after RTS to identify the incidence of second ACL injury. Tracking occurred with monthly communications via phone and/or email to patients inquiring whether they had sustained a second ACL injury.
Statistical Analysis
One-way analysis of variance (ANOVA) was used to determine differences in demographic data between patients who reported greater fear and those who reported lesser fear. Chi-square analysis was used to determine the association between self-reported fear as measured on the TSK-11 and all functional performance measures as well as incidence of second ACL injury. Odds ratios (ORs) and 95% confidence intervals were reported.
Results
At time of RTS, all patients (N = 40) completed the TSK-11 and the Marx activity scale; 38 patients were able to complete the single-leg hop for distance, and 39 patients were able to complete the isometric quadriceps strength assessment. At the time of RTS, patients were dichotomized into those who reported greater fear (n = 19; TSK-11 score ≥17) and those who reported lesser fear (n = 21; TSK-11 <17) on the TSK-11. There was no significant difference (P > 0.05) in age, height, weight, or time from surgery to RTS between groups (Table 1). Table 2 displays the distribution of patients within each cohort on measures of self-reported fear who presented with low activity as reported on the Marx activity scale (≤15) and low limb symmetry on the single-leg hop for distance (≤95%) and isometric QF strength (≤90%). Patients who reported greater fear on the TSK-11 were 4 times (OR, 3.73; 95% CI, 0.98-14.23) more likely to report lower levels of activity (≤15) on the Marx activity scale. With regard to functional performance, patients with greater fear were 7 times (OR, 7.1; 95% CI, 1.5-33.0) more likely to have a single-leg hop LSI less than 95%. No associations between fear and other functional hop tests were identified. Patients with greater levels of fear were 6 times more likely to have an isometric quadriceps strength limb symmetry index less than 90% (OR, 6.0; 95% CI, 1.3-27.8).
Table 1.
Patient demographics
| Total (N = 40) | High Fear (≥17) a (n = 19) | Low Fear (<17) a (n = 21) | P | |
|---|---|---|---|---|
| Age, y, mean (SD) | 16.2 (3.4) | 16.3 (3.5) | 16.1 (3.3) | 0.87 |
| Height, cm, mean (SD) | 163.7 (12.0) | 162.3 (11.7) | 165.0 (12.4) | 0.47 |
| Weight, kg, mean (SD) | 66.0 (17.4) | 62.9 (16.1) | 68.9 (18.5) | 0.29 |
| Time from surgery to RTS, mo, mean (SD) | 7.6 (2.4) | 7.8 (2.9) | 7.4 (1.8) | 0.60 |
RTS, return to sport.
As determined by the Tampa Scale of Kinesiophobia (TSK-11).
Table 2.
Distribution of patient activity and performance in patients with fear and low fear
| Low Marx Activity Score (≤15) (n = 40) a | Low Single-Leg Hop LSI (≤95) (n = 38) b | Low Isometric Quad LSI (≤90) (n = 39) c | |
|---|---|---|---|
| High TSK-11 (≥17) (n = 19) | 14/19 (73.7%) | 10/18 (55.6%) | 9/18 (50%) |
| Low TSK-11 (<17) (n = 21) | 9/21 (42.9%) | 3/20 (15%) | 3/21(14.3%) |
LSI, limb symmetry index; TSK-11, Tampa Scale of Kinesiophobia.
n = 40 patients completed Marx activity scale.
n = 38 patients completed the single-leg hop for distance.
n = 39 patients completed the isometric quadriceps strength assessment.
Fifteen (37.5%) patients suffered a second, noncontact ACL injury within 24 months of RTS after ACLR, leaving 25 patients in the reference group. Eight patients (20%) suffered an ipsilateral graft retear, and 7 patients (17.5%) suffered a contralateral ACL injury. Patients who went on to suffer a second ACL injury on the ipsilateral side had significantly greater TSK-11 score at the time of RTS (19.8 ± 4.0) than those who did not (16.4 ± 3.6) (P = 0.03). Patients who suffered a contralateral second ACL injury presented with no difference in TSK-11 score at the time of RTS (16.0 ± 1.8) compared with those who did not (17.3 ± 4.2) (P = 0.43). Chi-square analysis revealed patients with a TSK-11 score of 19 or greater at the time of RTS were 13 times (relative risk [RR], 13.0; 95% CI, 2.1-81.0) more likely to suffer an ipsilateral second ACL tear within the first 24 months after RTS. This variable predicted ipsilateral second ACL injury (area under the receiver operating characteristic curve, 0.740) in this population with high sensitivity (0.75) and specificity (0.81) (Figure 1). Self-reported fear on the TSK-11 was not associated with contralateral second ACL injury in this population (P = 0.652)
Figure 1.
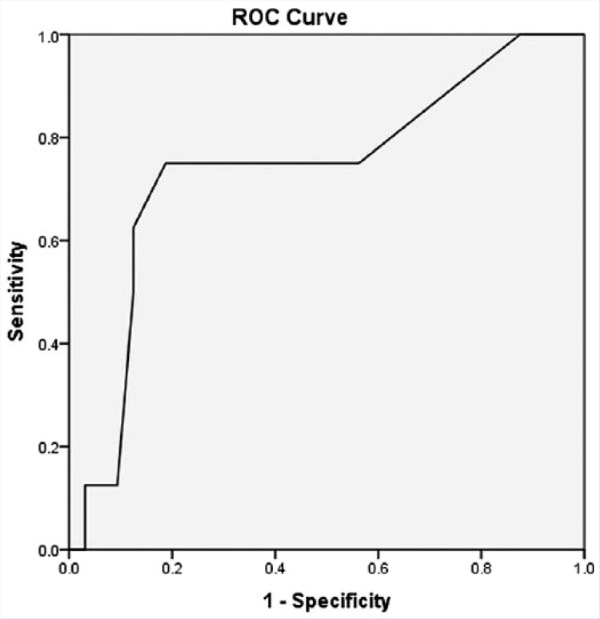
AUC highlighting ability of TSK-11 to predict second ACL injury after ACLR and RTS. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; AUC, area under the receiver operating characteristic curve; ROC, receiver operating characteristic; RTS, return to sport; TSK-11, Tampa Scale of Kinesiophobia.
Discussion
The purpose of this study was to determine the relationship between patient self-reported fear after ACLR and activity level, objective measures of function at time of RTS, and incidence of a second ACL injury within the first 24 months after RTS. Consistent with the tested hypothesis, patients with greater levels of fear at the time of RTS presented with an increased likelihood of reduced levels of activity, asymmetry on single-leg hop for distance assessment, and asymmetry on an isometric QF strength performance test at time of RTS. Furthermore, patients who returned to pivoting and cutting sports with greater self-reported fear demonstrated an increased risk of suffering a second ACL injury in the 24 months after RTS.
Fear and Activity
One prior study examined the relationship between self-reported fear on the TSK-11 and activity.22 Lentz et al22 reported on a cohort of 73 patients after ACLR and grouped them based on their ability to RTS at 1 year post-ACLR. They classified the cohort into 3 groups: those who were successful with RTS, those who were not successful because of fear to return, and those who were not successful because of other factors. They noted that patients who were able to RTS at 1 year postoperative presented with significantly lower scores on the TSK-11 at 6 months and 1 year post-ACLR when compared with patients who did not RTS due to fear. These authors22 were the first to indicate that a group who has a lower activity level, as indicated by RTS status at 1 year post-ACLR, may present with higher TSK-11 scores at 6 and 12 months postoperative. This study represents a novel contribution as it is the first to investigate the relationship between fear as reported on the TSK-11 and self-reported activity on an objective scale of activity, specifically the Marx activity scale. Despite the methodological differences in data analysis between these studies, both studies collectively suggest that patients with greater level of fear after ACLR may be less active after discharge to RTS. Assessment of patient-reported fear at the time of RTS may be an indicator of their potential level of activity and ability to RTS after ACLR.
Fear and Functional Performance
Limited previous work has evaluated the relationship between physical function and fear. Lentz et al22 reported that patients who did not RTS at 1 year post-ACLR because of fear of reinjury or lack of confidence presented with significantly lower quadriceps strength normalized to body weight at both 6 and 12 months post-ACLR compared with those patients who did return to prior level of sport at 12 months postoperatively. This was the first work to report differences in QF strength between those who were able to return to preinjury level of activity and those who chose not to return because of fear of reinjury or lack of confidence. Limited research has sought to identify the relationship between other performance-based measures, such as single-leg hop for distance and self-reported fear at time of RTS after ACLR. Further, there are no reports in the literature of differences in functional performance at the time of RTS after ACLR between those with high and low self-reported fear. These data are the first to report the potential relationship between high self-reported fear on the TSK-11 and greater asymmetries on functional performance assessments and QF asymmetry. The findings of our study suggest that the ease and accessibility of administering the TSK-11 may allow clinicians to use TSK-11 scores as a screening tool to optimize the timing of hop testing and assessment of RTS readiness. Future work should continue to investigate the relationship between objective measures of strength and function and patients’ self-reports of fear and confidence. Furthermore, additional studies are needed to assess the potential cause-and-effect relationship between these variables, which is currently unknown, as well as determine whether improving strength and performance prior to RTS would result in a reduction in fear.
Fear and Second ACL Injury Risk
The risk of second ACL injury after ACLR and RTS in young, active individuals is high. Paterno et al24 reported 23.5% of young, active patients suffered a second ACL injury in the first 12 months after RTS following ACLR. Subsequently, this group reported that 29.5% of young, active athletes who returned to cutting and pivoting sports after ACLR suffered a second ACL injury 24 months after RTS.25 A recent systematic review by Wiggins et al33 has confirmed the belief that young, active athletes are at greater risk to suffer subsequent ACL injury after ACLR and RTS. The present study found that a similar percentage of 37.5% of patients sustained an ACL injury in the initial 24 months after RTS.
The relationship between various risk factors and second ACL injury rate has been discussed in the literature. Kaeding et al17 noted younger age and higher activity level were predictors of increased odds of both ipsilateral and contralateral ACL injury, while allograft graft type was also a predictor of ipsilateral graft failure. Paterno et al26 prospectively identified biomechanical and neuromuscular predictors of second ACL injury after ACLR, noting landing mechanics and deficits in postural stability could predict second ACL injury with high sensitivity and specificity. To date, the relationship as well as the potential mechanistic link between patient-reported fear and second injury risk after ACLR has yet to be described. These data represent important pilot data investigating the relationship between patient-reported fear and second ACL injury rates. Potential mechanisms, such as fear leading to altered high-risk movement patterns or fear due to foundational high-risk impairments need further investigation.
This important discovery suggests that patient reports of fear may be related to second injury rates. Prior determinants of readiness to RTS were focused on measures of physical impairment and time after ACLR.7,18 More recent data suggest including abnormal movements in the RTS decision algorithm.14 No reports, to date, have included patient-reported fear of movement/fear of reinjury into a discharge planning algorithm after ACLR, despite the evidence suggesting the presence of fear in subpopulations after ACLR and RTS.2,19 These data, which suggest an association between patient-reported fear and future activity, functional performance, and second injury rates, provide potential support for the importance of evaluating this factor prior to RTS. Future work should build on these preliminary findings to better understand the role of patient-reported fear and other psychological factors in RTS decision-making and the potential to positively affect these through rehabilitation.
Limitations
This study does have limitations. First, a small sample size of 40 participants was included, making it only a pilot work. Second, the study sample consisted of young, active athletes who plan to return to pivoting and cutting sports. While this is an ideal sample to study a high-risk population that suffers a high incidence of second ACL injury,26 it may not be representative of all patients who undergo ACLR. As a result, this population may have low generalizability to other demographics, including older patients and those not returning to cutting and pivoting sports. Third, several tools have been used in the assessment of fear after ACLR, including the TSK-11, the ACL–Return to Sport after Injury, and others. Because of the wide variation in tools used to assess fear after ACLR, it is difficult to compare these studies. Finally, the LSI cut-off scores of 90% for isometric quadriceps strength and 95% for single-leg hop for distance were chosen based on clinically reported values necessary to be discharged to RTS after ACLR. These values have been debated and may not be universally accepted at this time.
Conclusion
At time of RTS, patients who report lower levels of fear present with less asymmetries in strength and functional performance, while patients with greater self-reported fear present with a decreased likelihood to participate in higher levels of activity. Similarly, patients who report greater levels of fear may present with greater risk of future ACL injury. These findings suggest patient fear of movement/reinjury may be an important measure to incorporate into discharge criteria prior to release to return to pivoting and cutting sports after ACLR.
Acknowledgments
The authors would like to acknowledge the outstanding clinicians and scientists within the Division of Occupational Therapy and Physical Therapy and the Division of Sports Medicine at Cincinnati Children’s Hospital who supported this work.
Footnotes
The following author declared potential conflicts of interest: This work was funded by support from the National Institutes of Health grant F32-AR055844 and the National Football League Charities Medical Research Grants 2007, 2008, 2009, 2011.
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction: a systematic review. Orthop J Sports Med. 2014;2:2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ardern CL, Osterberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613-1619. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40:41-48. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Webster KE. Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J Sci Med Sport. 2012;15:488-495. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 6. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596-606. [DOI] [PubMed] [Google Scholar]
- 7. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705. [DOI] [PubMed] [Google Scholar]
- 8. Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39:100-110. [DOI] [PubMed] [Google Scholar]
- 9. Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W. Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res. 1990;255:204-214. [PubMed] [Google Scholar]
- 10. Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38:746-753. [DOI] [PubMed] [Google Scholar]
- 11. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632-644. [DOI] [PubMed] [Google Scholar]
- 12. Fitzgerald GK, Lephart SM, Hwang JH, Wainner RS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31:588-597. [DOI] [PubMed] [Google Scholar]
- 13. George SZ, Lentz TA, Zeppieri G, Lee D, Chmielewski TL. Analysis of shortened versions of the Tampa Scale for Kinesiophobia and Pain Catastrophizing Scale for patients after anterior cruciate ligament reconstruction. Clin J Pain. 2012;28:73-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:192-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43:2727-2737. [DOI] [PubMed] [Google Scholar]
- 17. Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583-1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34:269-280. [DOI] [PubMed] [Google Scholar]
- 19. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393-397. [DOI] [PubMed] [Google Scholar]
- 20. Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946-951. [DOI] [PubMed] [Google Scholar]
- 21. Larsen JB, Farup J, Lind M, Dalgas U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum Mov Sci. 2015;39:73-87. [DOI] [PubMed] [Google Scholar]
- 22. Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345-353. [DOI] [PubMed] [Google Scholar]
- 23. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213-218. [DOI] [PubMed] [Google Scholar]
- 24. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320-1325.e6. [DOI] [PubMed] [Google Scholar]
- 28. Ross MD. The relationship between functional levels and fear-avoidance beliefs following anterior cruciate ligament reconstruction. J Orthop Traumatol. 2010;11:237-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ross MD, Langford B, Whelan PJ. Test-retest reliability of 4 single-leg horizontal hop tests. J Strength Cond Res. 2002;16:617-622. [PubMed] [Google Scholar]
- 30. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47:1426-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:750-759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47:334-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117:137-144. [DOI] [PubMed] [Google Scholar]
- 35. Zwolski C, Schmitt LC, Quatman-Yates C, Thomas S, Hewett TE, Paterno MV. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:2242-2249. [DOI] [PubMed] [Google Scholar]
- 36. Zwolski C, Schmitt LC, Thomas S, Hewett TE, Paterno MV. The utility of limb symmetry indices in return-to-sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2030-2038. [DOI] [PubMed] [Google Scholar]


