Abstract
Background:
Outcomes after arthroscopic Bankart repair can be highly dependent on compliance and participation in physical therapy. Additionally, there are many variations in physician-recommended physical therapy protocols.
Hypothesis:
The rehabilitation protocols of academic orthopaedic surgery departments vary widely despite the presence of consensus protocols.
Study Design:
Descriptive epidemiology study.
Level of Evidence:
Level 3.
Methods:
Web-based arthroscopic Bankart rehabilitation protocols available online from Accreditation Council for Graduate Medical Education (ACGME)–accredited orthopaedic surgery programs were included for review. Individual protocols were reviewed to evaluate for the presence or absence of recommended therapies, goals for completion of ranges of motion, functional milestones, exercise start times, and recommended time to return to sport.
Results:
Thirty protocols from 27 (16.4%) total institutions were identified out of 164 eligible for review. Overall, 9 (30%) protocols recommended an initial period of strict immobilization. Variability existed between the recommended time periods for sling immobilization (mean, 4.8 ± 1.8 weeks). The types of exercises and their start dates were also inconsistent. Goals to full passive range of motion (mean, 9.2 ± 2.8 weeks) and full active range of motion (mean, 12.2 ± 2.8 weeks) were consistent with other published protocols; however, wide ranges existed within the reviewed protocols as a whole. Only 10 protocols (33.3%) included a timeline for return to sport, and only 3 (10%) gave an estimate for return to game competition. Variation also existed when compared with the American Society of Shoulder and Elbow Therapists’ (ASSET) consensus protocol.
Conclusion:
Rehabilitation protocols after arthroscopic Bankart repair were found to be highly variable. They also varied with regard to published consensus protocols. This discrepancy may lead to confusion among therapists and patients.
Clinical Relevance:
This study highlights the importance of attending surgeons being very clear and specific with regard to their physical therapy instructions to patients and therapists.
Keywords: Bankart repair, rehabilitation, shoulder, instability, physical therapy
Traumatic anterior dislocation of the shoulder is a common injury affecting young and active patients,11 with avulsion of the inferior glenohumeral ligaments from the anteroinferior labrum (Bankart lesion) frequently occurring via this mechanism.7 Arthroscopic Bankart repair is currently the most commonly performed treatment for anterior shoulder instability.9 Ultimately, however, length and quality of rehabilitation after this procedure plays an important role in the achievement of functional stability and return to activity.4,10,12
Despite the importance of postoperative rehabilitation for positive long-term outcomes, there is a lack of high-quality research investigating the effect of various rehabilitation components on functional outcome. In the only level 1 study on rehabilitation after anterior shoulder dislocation with Bankart repair, Kim et al6 showed that the recurrence rate of Bankart lesions did not differ between accelerated or conventional rehabilitation protocols, but that patients undergoing accelerated rehabilitation resumed functional range of motion faster and returned to functional activities sooner.
The American Society of Shoulder and Elbow Therapists (ASSET) offers a consensus rehabilitation guideline for anterior arthroscopic capsulolabral repair of the shoulder.5 However, it is not clear whether protocols used by individual institutions adhere to these guidelines or the degree to which they differ. After Bankart reconstruction, it may be difficult to follow a consensus rehabilitation protocol because of differences in surgeon preference, surgical technique, strength of construct, injury pattern, and patient population. Additionally, it is unclear whether therapists are aware of these guidelines. Makhni et al8 recently showed a high degree of variability between anterior cruciate ligament (ACL) reconstruction rehabilitation protocols published by academic orthopaedic programs. The authors reported that many protocols did not recommend treatment, as supported by clinical information, and that differences in protocols could result in confusion among patients and therapists.8 Bozic et al3 examined rehabilitation protocols after total joint arthroplasty and also found a high degree of correlation between standardization of orthopaedic postoperative rehabilitation protocols and clinical benefits. Similar to the findings for ACL reconstruction rehabilitation, namely discrepancy between institution-specific protocols and published guidelines, differences in protocols were found to cause confusion between providers and patients over which protocol was optimal to follow.3
Because of the importance of postoperative rehabilitation after arthroscopic Bankart repair, it is imperative to evaluate the consistency between published rehabilitation protocols and assess the degree of deviation from existing consensus guidelines, such as those provided by the ASSET. The purpose of this study was to investigate the variability across arthroscopic Bankart repair rehabilitation protocols published online by academic orthopaedic programs. We hypothesized that the consistency between recommended exercises and the timing of functional milestones and activity start dates outlined in the protocols will vary widely. We also hypothesized that protocols will vary compared with the ASSET consensus protocol.
Methods
A single researcher reviewed publicly available physical therapy rehabilitation protocols from Accreditation Council for Graduate Medical Education (ACGME)–accredited academic orthopaedic surgery programs to ensure consistency in the analysis process. A list of academic orthopaedic surgery institutions was obtained from the ACGME website.1 From this list, a general web-based search (www.google.com) was performed to identify any rehabilitation protocols affiliated with the orthopaedic surgery department for a given academic program using the search term “[Program/hospital affiliate/medical school affiliate] Bankart repair rehabilitation protocol.” Protocols were excluded if they were specific to open Bankart repair or did not include any time points or goals for completion of specific rehabilitation phases. The websites of individual physicians were not searched; only those protocols made publicly available through a program affiliate website were included.
All rehabilitation protocols were assessed and reviewed for various components of immobilization and rehabilitation. The following broad categories were defined: postoperative adjunct therapy, early range of motion, passive range of motion start dates and goals, late range of motion exercises and goals, resistance exercises and strengthening, and sport-specific activities. Within each category, specific functional milestones, exercise recommendations, and start times were recorded. The complete list of reviewable metrics is available in Table 1. Information regarding rehabilitation protocols were recorded and analyzed in Microsoft Excel (Microsoft Corp). The primary outcome of this study was inclusion or exclusion of these metrics in each identified rehabilitation protocol, as well as start dates and completion dates of various rehabilitation activities.
Table 1.
List of analyzed categories and therapy recommendations
| Postoperative adjunct therapy | Type of immobilization, length of immobilization, brace for return to play |
| Early range of motion (ROM) | Periscapular stretching, elbow/wrist/hand, pendulum, supine forward elevation (FE), supine external rotation (ER), supine cross-chest adduction, wand, sleeper stretch, hand up spine, shoulder pinches, scapular clocks, standing internal rotation (IR) |
| Passive ROM start dates and goals | Passive forward flexion (PFF), passive ER, passive IR |
| Late ROM exercises and goals | Isometric deltoid, scapular stabilization, submaximal isometrics, isotonic resistance, serratus punches, normal scapulothoracic motion, full passive ROM, start active ROM, full active ROM |
| Resistance exercises and strengthening | Band training, light resistance, cocking weight, plyometrics, medicine ball, closed chain training, push-ups, resisted ER and IR cables, dumbbell training/free weights, light biceps curls, bench press, lat pull-downs/pull-ups |
| Sport-specific activities | Aquatic therapy (ROM), jogging, stationary bike, walk on treadmill, stairmaster, jogging, running, swimming, upper body ergometer, sport-specific activities (nonoverhead), overhead sports activities (throwing), throw from mound, return to sport, return to game |
Results
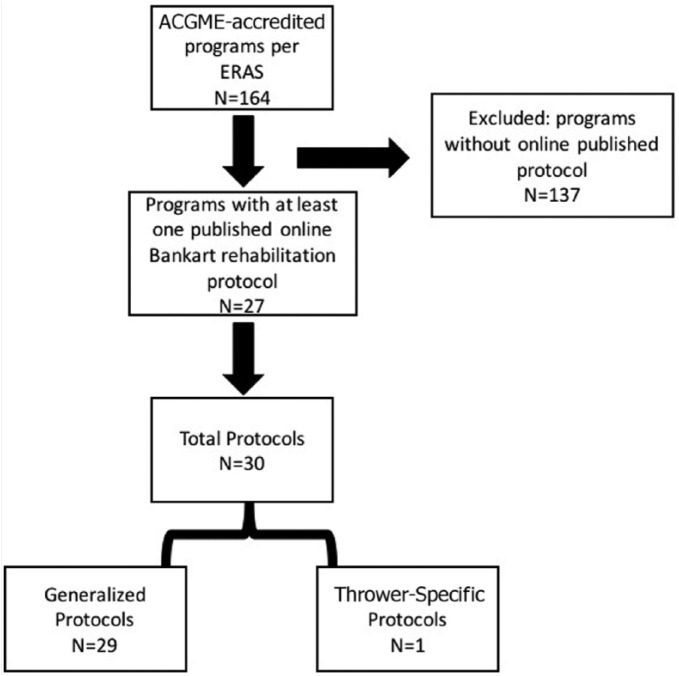
Of the 164 programs included for review, 27 institutions (16.4%) had publicly available rehabilitation protocols, with 30 total protocols included for review. Twenty-nine programs were generalized for all patients/athletes, while 1 protocol was specific to throwers (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart. ACGME, Accreditation Council for Graduate Medical Education; ERAS, Electronic Residency Application Service.
Postoperative Adjunct Therapy
Of the 30 included protocols, 28 (93.3%) recommended some type of postoperative immobilization, with 24 (80%) recommending sling immobilization and 4 (13.3%) recommending sling combined with an adjuvant swath or immobilizer (Table 2). While a majority of protocols advocated for early range of motion, 9 (30%) recommended some duration of strict shoulder immobilization (mean, 2.8 ± 1.6 weeks). The mean length of sling immobilization for all protocols was 4.8 ± 1.8 weeks. One protocol recommended the use of a brace after return to sport, although the type of brace was not specified.
Table 2.
Postoperative adjunct therapy recommendationsa
| n | % | |
|---|---|---|
| Sling | 24 | 80.0 |
| Sling + other | 4 | 13.3 |
| Not listed | 2 | 6.7 |
| Period of no movement | 9 | 30.0 |
| Brace on return to play | 1 | 3.3 |
Mean, 2.8 ± 1.6 weeks. Average time to sling discontinuation, 4.8 ± 1.8 weeks.
Early Range of Motion
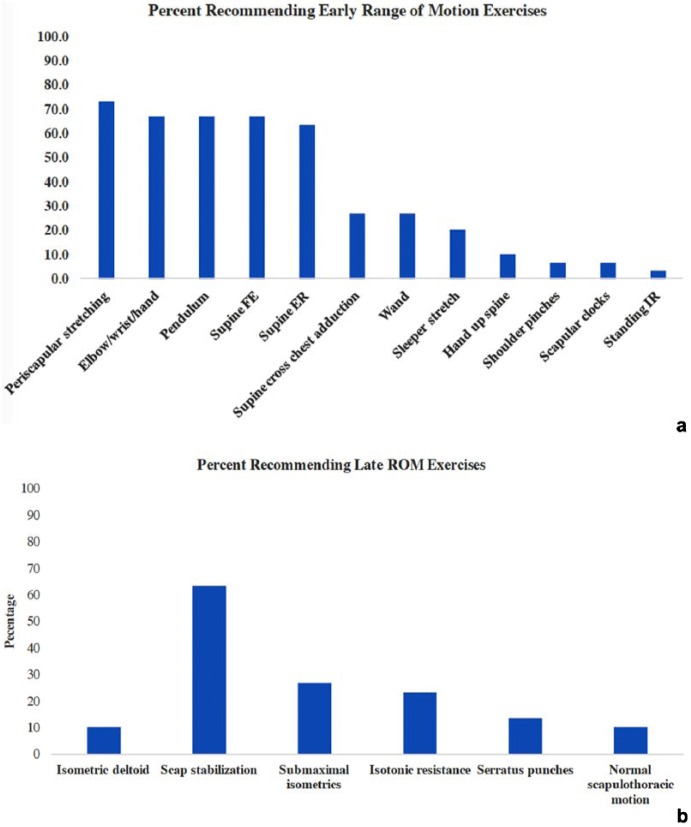
Immediate therapy recommendations varied from protocol to protocol with regard to which exercises patients should be performing in the immediate postoperative period. Nine protocols (30%) recommended a brief period of immobilization; however, generally, low-impact mobilization of the upper extremity was recommended (Figure 2a). Periscapular stretching was the most often recommended exercise (22 protocols, 73.3%). Elbow/wrist/hand motion, pendulums, and passive supine forward elevation were recommended in 20 (66.7%) protocols. Immediate postoperative passive supine external rotation was recommended by 19 (63.3%) protocols. Postoperative early abduction was more limited, only recommended by 8 (26.7%) protocols, as was internal rotation (1 protocol, 3.3%).
Figure 2.
Percentage of protocols recommending specific range of motion (ROM) exercises. (a) Early ROM exercises; (b) late ROM exercises. ER, external rotation; FE, forward elevation; IR, internal rotation; Scap, scapular.
Passive Range of Motion Start Dates and Goals
Range of motion start dates and goals varied from protocol to protocol with regard to start dates and motion intervals. Goals for full range of motion in various planes varied between protocols (Figure 3). The goal of 60° passive forward flexion averaged 1.7 ± 0.6 weeks postoperatively between protocols. Full passive forward flexion goals averaged 7.2 ± 2.4 weeks postoperatively. Early external rotation began with a goal of 20° to 30°, with an average start time recommendation of 3.6 ± 1.6 weeks. The mean time recommended to achieve full passive external rotation was 9.1 ± 2.6 weeks.
Figure 3.
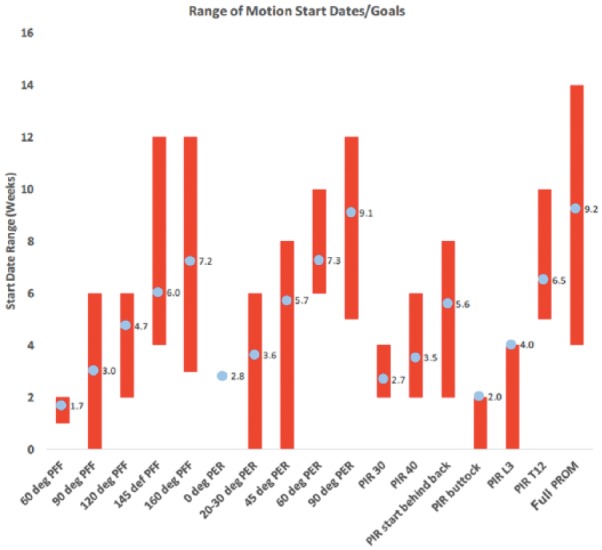
Ranges (red) and average goal (blue dots) in various planes of motion. PER, passive external rotation; PFF, passive forward flexion; PIR, passive internal rotation. PROM, passive range of motion.
Internal rotation goals were more variably defined within the protocols. Four programs graded internal rotation with regard to the number of degrees recommended, 6 made recommendations of a spinous process level that should be achieved, and 7 others simply gave a goal for “internal rotation behind the back.” The mean time expected to achieve full passive range of motion in all planes was 9.2 ± 2.8 weeks.
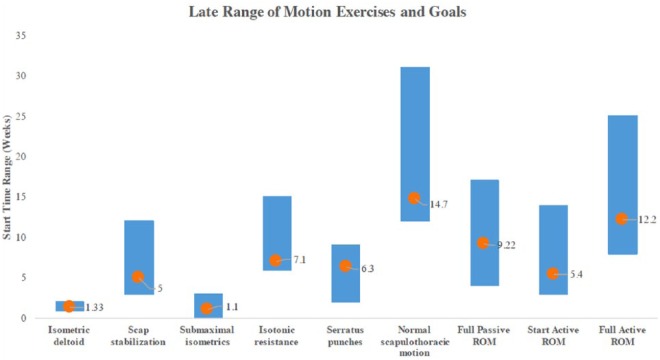
Late Range of Motion Exercises and Goals
A variety of additional range of motion exercises were recommended in later phases of the shoulder rehabilitation protocols (Figure 2b). Exercises included isometric deltoid strengthening, scapular stabilization, submaximal isometric exercises, isotonic resistance training, and serratus punches. Start dates for these exercises as well as range of motion goals for scapulothoracic motion as well as passive and active motion varied as well (Figure 4). Active range of motion began on average at 5.4 ± 1.8 weeks, with a goal of full active motion by 12.2 ± 2.8 weeks. Normal scapulothoracic motion was to be achieved by a mean of 14.7 ± 4.6 weeks.
Figure 4.
Late range of motion (ROM) exercises and goals. Scap, scapular.
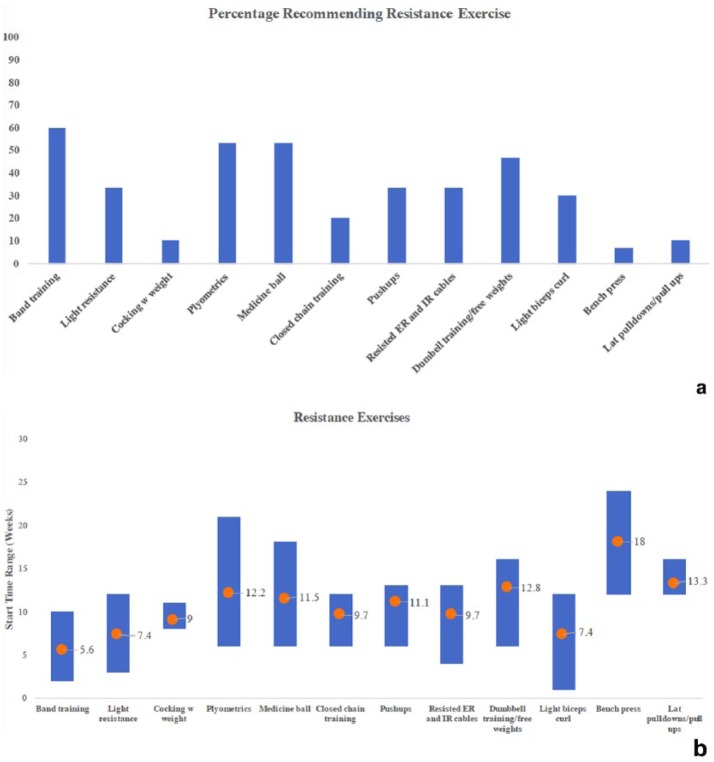
Resistance Exercises and Strengthening
There were a number of common resistance exercises recommended (Figure 5a). The most commonly recommended exercise was resistance band training in 18 (60%) protocols. Other popular exercises included plyometrics medicine ball (16 each, 53.5%); dumbbell training (14, 46.7%); and “light resistance training,” internal and external rotation cable exercises, and push-ups (10 each, 33.3%). Start dates varied by type of exercise (Figure 5b), with lower impact, open chain training such as that with resistance bands (mean, 5.6 ± 2.1 weeks) and biceps curls (mean, 7.4 ± 3.6 weeks) beginning earlier than heavier closed chain training exercises such as push-ups (mean, 11.1 ± 2.2 weeks) and bench press (mean, 18 ± 8.5 weeks).
Figure 5.
(a) Percentage of protocols recommending resistance activity. (b) Range and average start date of resistance activity. ER, external rotation; IR, internal rotation.
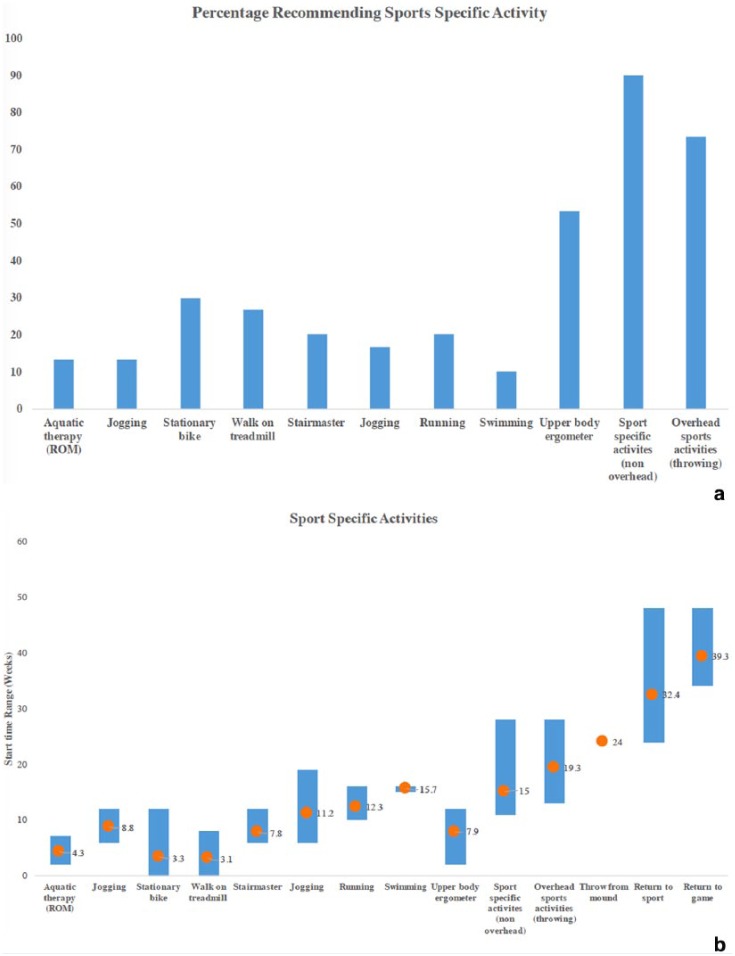
Sport-Specific Activities
Sport-specific activity was the last thing to be addressed by the various rehabilitation protocols. Most protocols (27, 90%) made specific recommendations regarding nonoverhead sport-specific activity, while 20 (66.7%) gave guidelines on return to throwing (Figure 6a). Only 10 (33.3%) addressed a timeline for return to sport, and only 3 (10%) gave an estimate on return to game competition. Various physical activities were included in the protocols, including upper body ergometer (16, 53.3%), stationary bike (9, 30%), treadmill walking (8, 26.7%), and running (6, 20%). Start dates for these sport-specific training activities varied based on the protocol (Figure 6b). The mean time to sport-specific activity was 15 ± 4.2 weeks, with throwing of any type not recommended until a mean of 19.3 weeks. Mean return to sport was 32.4 ± 9.3 weeks, with return to game allowed at a mean of 39.3 ± 7.6 weeks postoperatively.
Figure 6.
(a) Percentage of protocols recommending various sport-specific activities. (b). Ranges and average start date of sport-specific activities. ROM, range of motion.
Comparison to ASSET Guidelines
Additionally, the findings in this study were compared with the consensus recommendations made by the ASSET (Table 3). The milestones that most closely reflected the ASSET recommendations based on z-score were passive forward flexion to 90° and passive forward flexion to 135° (z = 0). Recommended time to full active range of motion was also relatively similar (z = −0.071). The recommendations that varied most were full passive forward flexion and full external rotation (z = 1.0).
Table 3.
Comparison between our study findings and the ASSET consensus protocol for arthroscopic Bankart repair
| ASSET | Study Mean | Study SD | z-score | |
|---|---|---|---|---|
| Sling | 4 | 4.8 | 1.8 | −0.444 |
| PFF 90 | 3 | 3 | 1.3 | 0.000 |
| PFF 135 | 6 | 6 | 2.3 | 0.000 |
| PFF 155 | 9 | 7.2 | 2.4 | 0.750 |
| PFF full | 12 | 9.2 | 2.8 | 1.000 |
| PER 30 | 3 | 3.6 | 1.6 | −0.375 |
| PER 50 | 6 | 5.7 | 1.8 | 0.167 |
| PER 65 | 9 | 7.3 | 1.9 | 0.895 |
| PER full | 12 | 9.2 | 2.8 | 1.000 |
| AFE 115 | 6 | 5.4 | 1.8 | 0.333 |
| AFE full | 12 | 12.2 | 2.8 | −0.071 |
| Push-ups | 12 | 11.1 | 2.2 | 0.409 |
| Sport-specific therapy | 16 | 15 | 4.2 | 0.238 |
AFE, active forward elevation; ASSET, American Society of Shoulder and Elbow Therapists; PER, passive external rotation; PFF, passive forward flexion; SD, standard deviation.
Discussion
There exists significant variability with regard to exercises recommended, timing of range of motion milestones, and timing of specific exercises and rehabilitation milestones. Most important was the variation in the inclusion or exclusion of range of motion and sport-specific activities as well as variation in their start dates. The high degree of availability and variation indicates that while generalized components of the rehabilitation protocol are similar, there is no widely accepted standard of care with regard to rehabilitation after arthroscopic Bankart repair, despite attempts at formulating a consensus protocol.
Shoulder rehabilitation after Bankart repair offers unique challenges, such as balancing protection of the repair with the desire to initiate early range of motion to prevent long-term stiffness and pain. Current rehabilitation protocols, including 9 in this study, recommend an early period of absolute immobilization. Despite these recommendations, clinical studies recommending early range of motion have shown greater postoperative range of motion during recovery, with no increase in instability.2 Kim et al6 performed a prospective randomized controlled trail of 62 patients who underwent arthroscopic Bankart repair comparing a standard rehabilitation protocol with 3 weeks of abduction sling immobilization versus a group who began an accelerated range of motion protocol the day of surgery. Patients had no difference in recurrence rate after 31 months, with a quicker return to functional range of motion and functional activity in the early range of motion group. Postoperative pain and patient satisfaction were greater in the early motion group; however, there was no difference in functional outcome scores, return to activity scores, or pain level at final follow-up.6 This study found the mean recommendation for immobilization in a sling of some form to be 4.8 ± 1.8 weeks, which is longer than both groups in the aforementioned study. This finding may suggest that a majority of current Bankart rehabilitation protocols recommend a longer period of sling immobilization than may be necessary to achieve a successful outcome.
The ASSET developed a consensus guideline for arthroscopic Bankart repair in 2010 with collaboration from the American Society of Shoulder and Elbow Surgeons.5 The goal of this protocol was to provide a standardized guideline for the clinician, therapist, and patient alike. The protocol included 3 phases: postoperative weeks 0 through 6, postoperative weeks 6 through 12, and postoperative weeks 12 through 24. Phase 1 focuses on protecting the surgical repair while not exceeding limitations in range of motion, with a goal of 135° passive forward elevation, 35° to 50° passive external rotation, and 145° of active forward elevation at the end of this phase. The findings in the present study matched these recommendations relatively well. Phase 2 is a gradual increase in range of motion, with a goal of full range of motion at 12 weeks. This was similar to the goal for full active range of motion in the analyzed ACGME protocols (mean, 12.2 ± 2.8 weeks; range, 8-18 weeks). When z-scores were calculated comparing our findings with the ASSET consensus, the largest differences existed with regard to achieving full passive range of motion. Phase 3 emphasizes an increase in resistance training and sport-specific activity, with a goal of return to activity on completion of this phase.5 The recommendations during this phase were relatively consistent with our findings, with only slight variance based on z-score.
It is important to note the limitations of our study. Even though we considered all academic orthopaedic institutions, only 30 rehabilitation protocols were publicly available, which represents a small percentage of institutions. It is likely that practitioners have private websites with their published protocols; however, these were not readily available through the institutions’ websites, and our methodology was designed to exclude these protocols to minimize selection bias. A second limitation is that some protocols may have been geared specifically toward throwing athletes. One rehabilitation protocol specified this directly, while several made reference to various throwing milestones (light toss, from a mound, throwing in game, etc). Several protocols did not specifically define the exercises they wished to have patients complete, simply recommending “light resistance” or “medicine ball training,” potentially leaving the exercises open to interpretation. Also, because rehabilitation protocols were not standardized in the exercises they recommended, it made it difficult to compare the start times and goals of exercises that were not as frequently recommended. Another limitation is that surgeons may vary their rehabilitation protocol based on patient factors as well as the quality of their repair; unfortunately, this was a variable we were unable to consider in this study. Additionally, with regard to injury, severity of the Bankart lesion and the type of surgical repair (other than arthroscopic) were not considered.
Conclusion
The major findings of this study were the wide variation in recommended exercises and start times/functional goals between those protocols that were available and variability when compared with the ASSET consensus protocol. While ultimately rehabilitation should be patient specific, it is also important to properly educate the patient and therapist to adequately set goals and expectations for a successful outcome and return to functional activity.
Footnotes
The following author declared potential conflicts of interest: Brett D. Owens, MD, is a paid consultant for Mitek and MTF/CONMED.
References
- 1. Accreditation Council for Graduate Medical Education. Accreditation Data System (ADS). https://apps.acgme.org/ads/public/reports/report/1. Accessed September 22, 2017.
- 2. Bacilla P, Field LD, Savoie FH. Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13:51-60. [DOI] [PubMed] [Google Scholar]
- 3. Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643-2652. [DOI] [PubMed] [Google Scholar]
- 4. Damkjær L, Petersen T, Juul-Kristensen B. Is the American Society of Shoulder and Elbow Therapists’ rehabilitation guideline better than standard care when applied to Bankart-operated patients? A controlled study. Clin Rehabil. 2015;29:154-164. [DOI] [PubMed] [Google Scholar]
- 5. Gaunt BW, Shaffer MA, Sauers EL, et al. The American Society of Shoulder and Elbow Therapists’ consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther. 2010;40:155-168. [DOI] [PubMed] [Google Scholar]
- 6. Kim S-H, Ha K-I, Jung M-W, Lim M-S, Kim Y-M, Park J-H. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: a prospective randomized clinical study. Arthroscopy. 2003;19:722-731. [DOI] [PubMed] [Google Scholar]
- 7. Liavaag S, Stiris MG, Svenningsen S, Enger M, Pripp AH, Brox JI. Capsular lesions with glenohumeral ligament injuries in patients with primary shoulder dislocation: magnetic resonance imaging and magnetic resonance arthrography evaluation. Scand J Med Sci Sports. 2011;21:e291-e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Makhni EC, Crump EK, Steinhaus ME, et al. Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy. 2016;32:1612-1621. [DOI] [PubMed] [Google Scholar]
- 9. Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical trends in Bankart repair: an analysis of data from the American Board of Orthopaedic Surgery certification examination. Am J Sports Med. 2011;39:1865-1869. [DOI] [PubMed] [Google Scholar]
- 10. Robinson CM, Jenkins PJ, White TO, Ker A, Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder. A randomized, double-blind trial. J Bone Joint Surg Am. 2008;90:708-721. [DOI] [PubMed] [Google Scholar]
- 11. Sedeek SM, Bin Abd Razak HR, Ee GW, Tan AHC. First-time anterior shoulder dislocations: should they be arthroscopically stabilised? Singapore Med J. 2014;55:511-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wilk K, Reinold M, Andrews JR. Postoperative treatment principles in the throwing athlete. Sports Med Arthrosc Rev. 2001;9:66-95. [Google Scholar]