Abstract
Study Design:
Case series.
Objective:
Thoracolumbar burst fractures (TLBF) are the most frequent type of spinal fractures. Approximately half of the patients are neurologically intact and their treatment is still debatable. Gender could influence outcome after surgical procedures, but this is still unclear in patients sustaining a spinal fracture. The aim of this study was to investigate how gender influences health-related quality of life (HRQOL) and disability in patients operated on for TLBF.
Methods:
We identified 44 neurologically intact patients from a consecutive series of patients treated surgically for a single-level traumatic burst fracture (AOSpine Subaxial Classification System A3) in the thoracolumbar transition area (Th12-L2). At 1 year after surgery, they were evaluated using the SF-36v2 questionnaire to assess HRQOL and Oswestry Disability Index (ODI) questionnaire to evaluate disability.
Results:
Male patients scored higher in each item of the SF-36v2, with significant differences (P < .05) for Physical Function (PF), Bodily Pain (BP), and Social Function (SF). Male patients also had lower disability scores. Overall ODI score had a strong correlation with Physical Function, Role-Physical, Bodily Pain, Vitality, Mental Health, and overall Physical Component Summary (PCS) of the SF-36 in women, but only with Physical Function, Role-Physical, Role-Emotional, and PCS in men.
Conclusions:
In this study, male patients reported better outcomes at 1 year after surgery for TLBF than women. Disability strongly correlated with the overall HRQOL, physical and mental health in women, but not in men. We found gender-related differences favoring men after surgical interventions for spinal fractures.
Keywords: health-related quality of life, disability after spine surgery, thoraco-lumbar burst fractures, gender influence on outcome
Objective
The thoracolumbar junction represents the most frequent location for spinal fractures. This is most probably because of the particular biomechanics of the spine at this level, where the rigid thoracic region meets the more mobile lumbar one.1 Thoracolumbar burst fractures (TLBFs) account for up to 45% of the fractures in this region.1,2 They are usually caused by traumatic incidents that imply high axial compression forces, like falls, motor vehicle accidents, and high-intensity sports.2,3 About half of the patients will be neurologically intact and the opinions are still largely divided regarding their best management, as both the surgical and nonsurgical treatment have been recommended.4,5 Operative management includes spinal fixation with or without fusion through various approaches, like the posterior reduction and stabilization, combined procedures using titanium or bony mesh implants or anterior procedures. The nonoperative one involves postural reeducation, bed rest, body cast, and use of orthoses.6,7 None of the operative approaches has been proven to be more efficient than others when comparing kyphosis, the degree of fusion or complications, but the posterior approach is more effective for spinal decompression, surgery length, and blood loss.8–10 The algorithms of management were until now limited and only recently, better management guidelines have been introduced with the Thoracolumbar Injury Classification System (TLICS) and Thoracolumbar AOSpine Injury Score (TL AOSIS) being 2 examples.11,12
Defining success of any therapy in spinal pathology must assess the patient’s view of the treatment.13 It has been shown extensively that outcome of any medical procedure cannot rely only on objective measures, as patients may have different opinions from those of their physicians.14,15 Moreover, until now, no functional or radiological parameter has been linked to the quality of life and subjective outcome after spinal procedures, including those for TLBF.13,16 Evaluation of the patient’s beliefs should be done by using Health-Related Quality of Life (HRQOL) and disease-specific questionnaires after spine surgery.17 The degree of correlation between the 2 variables following spinal surgery seems influenced by the spinal pathology.18 Various studies suggest that gender could impact outcome after certain types of surgery.19 This influence of gender on self-reported outcome after spinal procedures is disputed, as studies of this issue have had controversial results.20,21
The purpose of this study was to assess HRQOL and disability in patients operated for TLBF, the correlation between the 2 and to observe whether gender could play a potential role in the outcome of patients.
Methods
After institutional board review, a series of patients was evaluated 1 year after undergoing short-segment posterior stabilization for the treatment of a single-level traumatic burst fracture (AOSpine Thoracolumbar Classification System A3) in the thoracolumbar transition area (Th11–L2). Eligible patients had to fulfil the following criteria: (a) age between 18 and 70 years; (b) patient operated for a burst-type fracture of a single vertebral body in the Th12-L2 region; (c) no neurologic deficit or bowel or bladder function abnormality after the traumatic incident; (d) no history of psychiatric disorders, no other illnesses like osteoporosis, cancer, infection, bleeding disorders that could affect outcome; (e) no previous spinal surgery or significant spinal degeneration; and (f) agreement with the proposed surgical treatment.
During the analyzed interval, 82 patients were operated for a TLBF. We identified 49 patients who fulfilled our inclusion criteria. Five patients refused to complete one or both of the questionnaires included in the study, which left 44 eligible patients available. Informed consent was obtained from all individual participants included in the study.
All patients were operated upon in the first 7 days after the traumatic incident. The surgical approach was done in all cases through a posterior midline incision centered on the fractured vertebrae. In all the 44 patients included in this study, pedicle screws were inserted after subperiosteal exposure, using an image intensifier control, one level above and one below the fractured vertebrae. Lordotization and distraction were performed using rods that locked onto the pedicle screws, allowing for the approximation of the structure of the vertebral column and ligamentotaxis, in an attempt to indirectly reduce canal encroachment. We use the load sharing classification (LSC) developed McCormack and all in order to decide if fusion is needed.22 In the patients included in this study, LSC score was ≤7 and no additional fusion was performed. A drain was placed in all cases and removed the next day after surgery, mobilization was initiated and movement allowed without braces, starting the same day.
The patients completed 2 questionnaires, the SF-36 version 2 (Quality Metric, Inc, Lincoln, RI) and the Oswestry Disability Index (ODI). The SF-36 is one of the widest used instruments for evaluating HRQOL.23 Through 36 questions it covers 8 dimensions of HRQOL and offers physical component summary (PCS) and mental component summary (MCS) scores. It has been proven as a valid instrument in measuring outcome after spinal surgery.24,25 Higher scores on the SF-36 domains reflect a better quality of life. ODI is a disease-specific questionnaire, developed for patients with back pain. It uses 10 items, each with 6 possible statements scored from 0 to 5, with higher scores indicating a higher disability.26 Analysis of the SF-36v2 data was done using the QualityMetric Health Outcomes Scoring Software 4.5 (QualityMetric Inc). Statistical analysis was carried out using the GraphPad Prism Software (GraphPad Software, Inc, La Jolla, CA, USA). Unadjusted comparison between groups was performed using analysis of variance or t test, as considered appropriate. A Spearman correlation test was conducted to evaluate the correlation between ODI and SF-36v2 items. In all cases, a P value <.05 was considered statistically significant.
Results
Out of the 44 patients, 17 were female and 27 were male. Age, the level of fracture, use of pain medicine at 1 year after surgery are detailed in Table 1. There was no significant difference between male and female patients in local kyphotic angle, canal encroachment, LSC preoperatively or after surgery.
Table 1.
Age, Sex Distribution, Fracture Location, and Use of Pain Medication for Back Pain.
| Female | Male | |
|---|---|---|
| No. of patients | 17 | 27 |
| Age, y, mean (SD) | 37.88 (13.56) | 44.04 (14.28) |
| Location of fracture | ||
| T11 | 1 | 2 |
| T12 | 1 | 5 |
| L1 | 12 | 16 |
| L2 | 3 | 4 |
| Use of pain medication | ||
| 1-3 times/wk | 5 | 4 |
No significant operative complications were recorded during surgery or in the 1 year after. Two patients were reoperated upon during this interval. One male patient underwent a second surgery 2 days after the first one for the reinsertion of a wrongly inserted screw. One female patient had a superficial wound infection that was treated with antibiotics and local debridement 8 days after the initial surgery.
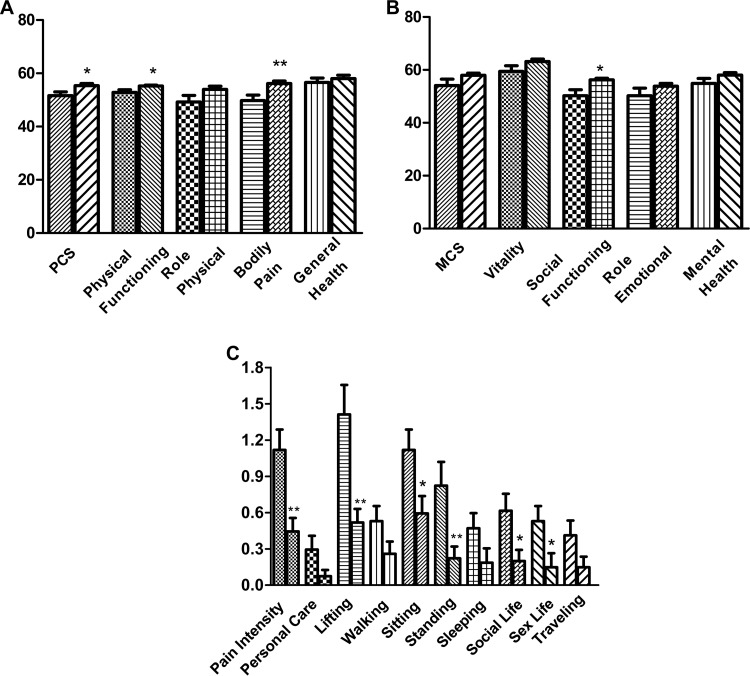
Male patients had a significantly higher score on the physical component summary (PCS) of the SF-36 as compared with female patients (P = .0143, 95% CI −6.73 to −0.78). There were no significant differences regarding the Role-Physical (RP) and General Health (GH) items, although male patients had higher scores. Males had a significantly higher Physical Functioning (PF) score (P = .0163, 95% CI −4.315 to −0.4628) and a highly significant difference was seen on the Bodily Pain (BP) item (P = .0032, 95%CI −10.56 to −2.269) (Figure 1A).
Figure 1.
(A) Physical component summary (PCS) scale and items. The first column for each item represent values for women and second for men. Values marked with “*” represent significant differences and values marked with “**” represent highly significant differences and are placed over the better scoring item. (B) Mental component summary (MCS) scale and items. The first column for each item represent values for women and second for men. Values marked with “*” represent significant differences and values marked with “**” represent highly significant differences and are placed over the better scoring item. (C) Oswestry Disability Index (ODI) items. The first column for each item represent values for women and second for men. Values marked with “*” represent significant differences and values marked with “**” represent highly significant differences and are placed over the better scoring item.
On the mental component summary (MCS), men had higher scores in all domains, although the overall difference was not statistically significant (P = .0786, 95% CI = −8.097 to 0.4578) (Figure 1B). The only significant difference between genders was on the Social Functioning (SF) scale (P = .0035, 95%CI −9.857 to −2.072).
On the ODI scale, male patients showed lower disability compared with female patients, with the overall ODI score showing a highly significant difference between the genders favoring men (P = .0028, 95% CI 3.22 to 14.48). “Personal Care.” “Walking,” “Sleeping,” and “Traveling” were the items in which no significant difference was seen between the 2 genders. The difference was significant for “Sitting” (P = .02, 95% CI 0.069 to 0.98), “Sex Life” (P = .014, 95% CI 0.08 to 0.74), and “Social Life” (P = .03, 95% CI 0.02 to 0.73), while for the rest of the items, the difference was highly significant, with men scoring much lower on the “Pain Intensity” (P = .0012, 95% CI 0.28 to 1.0), “Lifting” (P = .0005, 95% CI 0.41 to 1.37), and “Standing” (P = .0041, 95% CI 0.20 to 1.00) items (Figure 1C).
Correlation analysis between ODI and SF-36 highlighted differences between genders, with a higher degree of correlation in females (Table 2). In female patients, the overall ODI score strongly correlated with PF, RP, BP, VT, MH, PCS, and also correlated moderately with the rest of the items on the SF-36v2 questionnaire. In males, ODI strongly correlated with PF, RP, RE, PCS, and moderately with BP and GH, without showing any correlation with the rest of the items of the SF-36. The “Pain Intensity” item from ODI correlated strongly with all the items from the SF-36, except RE, where it showed moderate correlation, in females but it only strongly correlated with RP in male patients. Similarly, the PF scale of the SF-36, showed strong or moderate correlation with all the ODI items for females, while showing correlation only with the overall ODI score in males. All correlations were statistically significant.
Table 2.
Spearman Correlation Coefficients (r s) Between SF-36 and ODI.a
| PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS | |
|---|---|---|---|---|---|---|---|---|---|---|
| r s value for women | ||||||||||
| Pain intensity | −0.65 | −0.77 | −0.76 | −0.67 | −0.75 | −0.69 | −0.56 | −0.81 | −0.77 | −0.75 |
| Personal care | −0.52 | −0.42 | −0.55 | −0.45 | −0.47 | −0.15 | −0.27 | −0.35 | −0.63 | −0.21 |
| Lifting | −0.81 | −0.73 | −0.64 | −0.39 | −0.63 | −0.34 | −0.40 | −0.55 | −0.68 | −0.38 |
| Walking | −0.67 | −0.54 | −0.48 | −0.28 | −0.46 | −0.31 | −0.29 | −0.43 | −0.53 | −0.29 |
| Sitting | −0.45 | −0.53 | −0.51 | −0.33 | −0.42 | −0.45 | −0.50 | −0.48 | −0.38 | −0.53 |
| Standing | −0.64 | −0.58 | −0.58 | −0.13 | −0.65 | −0.43 | −0.66 | −0.68 | −0.43 | −0.59 |
| Sleeping | −0.76 | −0.54 | −0.46 | −0.19 | −0.62 | −0.42 | −0.36 | −0.59 | −0.51 | −0.46 |
| Sex life | −0.65 | −0.69 | −0.68 | −0.26 | −0.65 | −0.33 | −0.43 | −0.58 | −0.63 | −0.38 |
| Social life | −0.57 | −0.54 | −0.63 | −0.34 | −0.46 | −0.18 | −0.29 | −0.43 | −0.60 | −0.22 |
| Traveling | −0.68 | −0.54 | −0.45 | −0.22 | −0.62 | −0.49 | −0.16 | −0.54 | −0.51 | −0.41 |
| ODI | −0.84 | −0.78 | −0.77 | −0.46 | −0.75 | −0.52 | −0.56 | −0.74 | −0.75 | −0.59 |
| r s value for men | ||||||||||
| Pain intensity | −0.59 | −0.63 | −0.51 | −0.29 | −0.26 | −0.08 | −0.53 | −0.04 | −0.56 | −0.19 |
| Personal care | −0.25 | −0.50 | −0.42 | −0.15 | −0.33 | −0.32 | −0.57 | −0.42 | −0.38 | −0.42 |
| Lifting | −0.58 | −0.69 | −0.65 | −0.33 | −0.38 | −0.50 | −0.44 | −0.23 | −0.64 | −0.29 |
| Walking | −0.49 | −0.44 | −0.31 | −0.22 | −0.36 | −0.11 | −0.63 | −0.48 | −0.34 | −0.59 |
| Sitting | −0.33 | −0.45 | −0.29 | −0.18 | −0.27 | −0.10 | −0.55 | −0.28 | −0.29 | −0.41 |
| Standing | −0.38 | −0.39 | −0.20 | −0.34 | −0.17 | −0.14 | −0.51 | −0.27 | −0.40 | −0.33 |
| Sleeping | −0.38 | −0.63 | −0.37 | −0.30 | −0.24 | −0.25 | −0.73 | −0.27 | −0.51 | −0.41 |
| Sex life | −0.44 | −0.52 | −0.24 | −0.34 | 0.11 | 0.21 | −0.67 | 0.15 | −0.50 | 0.02 |
| Social life | −0.34 | −0.53 | −0.27 | −0.26 | −0.12 | −0.34 | −0.62 | −0.14 | −0.42 | −0.31 |
| Traveling | −0.38 | −0.63 | −0.37 | −0.30 | −0.24 | −0.25 | −0.73 | −0.27 | −0.51 | −0.41 |
| ODI | −0.70 | −0.68 | −0.59 | −0.51 | −0.43 | −0.17 | −0.64 | −0.34 | −0.67 | −0.42 |
Abbreviations: PF, Physical Functioning; RP, Role-Physical; BP, Bodily Pain; GH, General Health; VT, Vitality; SF, Social Functioning; RE, Role-Emotional; MH, Mental Health; PCS, Physical Component Summary; MCS, Mental Component Summary; ODI, Oswestry Disability Index.
aValues in boldface indicate strong correlations (0 ≥ r s ≥ 0.6).
Discussion
In this study of self-reported outcomes of patients operated for a TLBF, our findings suggest that male patients have better outcomes than females in both HRQOL and disability. A second finding is that HRQOL correlates to a much higher extent with disability in women, but not in men and back pain is associated to a high degree to all the quality of life domains in women, but not in men. A third finding is that in female patients, disability is strongly correlated with the mental component of QOL, while this association could not be identified in male patients. We see these findings as the main reason for interest in this research. Another reason is that, to our information, this study offers the first perspective on HRQOL and disability after surgery for spinal fractures coming from this region of Europe and as such it will provide comparative material for other studies investigating various topics of self-reported outcome after surgery for TLBF.
The surgical treatment for TLBF is safe and effective.27 The various surgical approaches seem to provide similar results when comparing clinical and radiological outcomes, but the posterior approach is associated with shorter surgical time, less blood loss, and better decompression.9,10,28 Multiple studies have reported that no clinical or radiological parameters are correlated with quality of life and satisfaction after surgery for TLBF.29–33 Therefore, self-reported HRQOL and disability questionnaires are until now, the only tools that can reliably measure outcome after these procedures. Furthermore, some studies suggest that SF-36 can predict the need for reintervention after spinal procedures in patients with poor results after a first procedure.34,35 This makes these questionnaires vital in comparing outcome after various types of treatment or for identifying the patients that will benefit most from a certain therapy.
Gender seems to influence the outcome after various surgical procedures, although the relation is still unclear since various studies report different results.19 Regarding postoperative complications, male patients had higher rates of mortality, hospital readmissions, revision surgery and wound infections after primary total knee arthroplasty in one study.36 But other researchers found that males reported fewer postoperative complications.20 When investigating the relation between gender and outcome after spinal surgery, results have also been mixed.20,21,37,38 Studies that indicate that gender influences outcome after spine surgery usually found better outcomes in males.20,39 This is in line with research that suggests that women report worse health outcomes than men, not only after medical procedures but also in population norm studies.40,41 Also, women report more disability compared with men when performing a task, even if the observed difficulty is similar and are more fatigued after spinal procedures.42 The reasons for this difference are to this point unclear, but several hypotheses exist.
One theory is that men and women value their health differently. Various studies found that patient’s expectations before a surgical procedure positively correlate with outcome, with the male gender being associated with higher preoperative expectations which result in a higher postoperative satisfaction.39,43 Evaluating the preoperative HRQOL in an acute setting like the one determined by the traumatic incident that leads to a TLBF may not provide accurate results. One study that investigated this phenomenon found that preoperative SF-36 values in patients operated for a TLBF were not correlated to the postoperative quality of life.13
Other researchers suggest that men and women have different temporal patterns when presenting for treatment, both medical and surgical, this timing directly influencing the outcome. In studies investigating HRQOL after cholecystectomy, the authors found that female patients went through the procedure at an earlier time after the onset of symptoms and in better health and this left a smaller room for improvement.19,44 But studies of this issue in patients with spinal pathology showed that females were operated on at more advanced stages, so the issue could be disease specific.20,21,45 Because of the acute onset of TLBF and the evolution of the disease, patients rarely decide the timing of presentation to a physician and of the treatment, so this factor does not seem to explain the difference in the outcome. In our study, all the patients were operated on in the first 7 days after the traumatic incident.
One possible explanation for the difference in outcome between genders in our study could be related to how disability and HRQOL correlated differently in male and female patients. Studies investigating the correlation between spinal disability questionnaires and HRQOL questionnaires reported little or moderate associations between the 2.18,46,47 It has been suggested that these instruments measure different aspects of quality of life, have different constructs or that the type of spinal pathology determines the degree of the correlation.18,48 We did not identify studies that showed that the degree of association between the two is different in males and females. In studies investigating ODI and SF-36, ODI Pain Intensity correlated moderately with the PCS domain of the SF-36.46 It has been argued that because of a higher sensitivity to pain, females experience it more for a given severity of a disease.20 In our study, ODI strongly correlated with 6 domains of the SF-36v2 (PF, RP, BP, VT, and MH) and moderately with the remaining 3 (GH, SF, RE) in women. Furthermore, ODI Pain Intensity in females correlated strongly with all the domains of SF-36v2, except RE, with which it correlated moderately, but it did not show any strong correlation with SF-36 domains in male patients. Also, PF of the SF-36, correlated strongly with 7 domains of ODI and moderately with the remaining 3 in females. This is important since PF reflects the overall physical functioning of a person and ODI relates to specific disability problems caused by back pain. In males, ODI correlated strongly only with PF, RP, and RE, and moderately with BP and GH. Moreover, PF did not show strong correlations with any ODI item.
This would suggest that the disability caused by TLBF strongly affects the overall quality of life in women, but this is true to a lesser extent in men. Back pain seems to be associated with quality of life in women, but not in men. It is also worthwhile to notice that disability links to the mental quality of life in women but not in men. This could influence the psychological well-being of women. Our hypothesis is that the higher correlation between disability and overall HRQOL, combined with the closer relation between pain and quality of life together with a supposed higher sensitivity to pain in women, can explain why women reported lower scores than men in our study. Future research should concentrate on comparing the link between disability and HRQOL and identify the patients in which the correlation between the 2 is higher.
There are several shortcomings of our study. As stated previously, we do not have any knowledge of how evaluations have been influenced by the acute onset of the fractures and the resulting emotional shock. Another possible limitation is the fact that this study did not compare clinical parameters as this was not the purpose of the research protocol.
Conclusions
In this study, male patients reported better outcomes at 1 year after surgery for TLBF than women. This was true in all domains of disability and HRQOL. Disability strongly correlated with both physical and mental components of QOL in women, but to a lesser extent in men. The pain was closely associated with quality of life in women, but not in men. We found gender-related differences favoring men after surgical interventions for spinal fractures, that should be scrutinized further. Future studies should investigate if this relation between gender and outcome is valid and emphasize the mechanism through which disability caused by spinal pathology links to HRQOL in both men and women.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17:528–540. [DOI] [PubMed] [Google Scholar]
- 2. Bensch FV, Koivikko MP, Kiuru MJ, Koskinen SK. The incidence and distribution of burst fractures. Emerg Radiol. 2006;12:124–129. doi:10.1007/s0010140-005-0457-5. [DOI] [PubMed] [Google Scholar]
- 3. Scheer JK, Bakhsheshian J, Fakurnejad S, Oh T, Dahdaleh NS, Smith ZA. Evidence-based medicine of traumatic thoracolumbar burst fractures: a systematic review of operative management across 20 years. Global Spine J. 2015;5:73–82. doi:10.1055/s-0034-1396047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aleem IS, Nassr A. Cochrane in CORR®: surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Clin Orthop Relat Res. 2016;474:619–624. doi:10.1007/s11999-015-4305-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4:351–358. doi:10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 6. Karimi M. The effects of orthosis on thoracolumbar fracture healing: a review of the literature. J Orthop. 2015;2:1–8. doi:10.1016/j.jor.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture. Asian Spine J. 2015;9:133–146. doi:10.4184/asj.2015.9.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pfeifer R, Pishnamaz M, Dombroski D, Heussen N, Pape H-C, Schmidt-Rohlfing B. Outcome after thoracoscopic ventral stabilisation of thoracic and lumbar spine fractures. J Trauma Manage Outcomes. 2012;6:10 doi:10.1186/1752-2897-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schmid R, Krappinger D, Blauth M, Kathrein A. Mid-term results of PLIF/TLIF in trauma. Eur Spine J. 2011;20:395–402. doi:10.1007/s00586-010-1615-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhu Q, Shi F, Cai W, Bai J, Fan J, Yang H. Comparison of anterior versus posterior approach in the treatment of thoracolumbar fractures: a systematic review. Int Surg. 2015;100:1124–1133. doi:10.9738/intsurg-d-14-00135.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Joaquim AF, de Almeida Bastos DC, Jorge Torres HH, Patel AA. Thoracolumbar injury classification and injury severity score system: a literature review of its safety. Global Spine J. 2016;6:80–85. doi:10.1055/s-0035-1554775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kepler CK, Vaccaro AR, Schroeder GD, et al. The Thoracolumbar AOSpine Injury Score. Global Spine J. 2016;6:329–334. doi:10.1055/s-0035-1563610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Briem D, Lehmann W, Ruecker AH, Windolf J, Rueger JM, Linhart W. Factors influencing the quality of life after burst fractures of the thoracolumbar transition. Arch Orthop Trauma Surg. 2004;124:461–468. doi:10.1007/s00402-004-0710-5. [DOI] [PubMed] [Google Scholar]
- 14. Ostelo RWJG, de Vet HCW. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19:593–607. doi:10.1016/j.berh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 15. Saban KL, Penckofer SM, Androwich I, Bryant FB. Health-related quality of life of patients following selected types of lumbar spinal surgery: a pilot study. Health Qual Life Outcomes. 2007;5:71 doi:10.1186/1477-7525-5-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yamashita K, Hayashi J, Ohzono K, Hiroshima K. Correlation of patient satisfaction with symptom severity and walking ability after surgical treatment for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976). 2003;28:2477–2481. doi:10.1097/01.BRS.0000090888.63860.4F. [DOI] [PubMed] [Google Scholar]
- 17. Ghogawala Z, Resnick DK, Watters WC, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 2: assessment of functional outcome following lumbar fusion. J Neurosurg Spine. 2014;21:7–13. doi:10.3171/2014.4.SPINE14258. [DOI] [PubMed] [Google Scholar]
- 18. Djurasovic M, Glassman SD, Dimar JR, Crawford CH, Bratcher KR, Carreon LY. Changes in the Oswestry Disability Index that predict improvement after lumbar fusion. J Neurosurg Spine. 2012;17:486–490. doi:10.3171/2012.8.SPINE12614. [DOI] [PubMed] [Google Scholar]
- 19. Quintana JM, Arostegui I, Oribe V, López de Tejada I, Barrios B, Garay I. Influence of age and gender on quality-of-life outcomes after cholecystectomy. Qual Life Res. 2005;14:815–825. [DOI] [PubMed] [Google Scholar]
- 20. Pochon L, Kleinstück FS, Porchet F, Mannion AF. Influence of gender on patient-oriented outcomes in spine surgery. Eur Spine J. 2016;25:235–246. doi:10.1007/s00586-015-4062-3. [DOI] [PubMed] [Google Scholar]
- 21. Strömqvist F, Ahmad M, Hildingsson C, Jönsson B, Strömqvist B. Gender differences in lumbar disc herniation surgery. Acta Orthop. 2008;79:643–649. doi:10.1080/17453670810016669. [DOI] [PubMed] [Google Scholar]
- 22. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741–1744. [DOI] [PubMed] [Google Scholar]
- 23. Fryback DG. Measuring health-related quality of life. In : Workshop on Advancing Social Science Theory: The Importance of Common Metrics; February 2010; The National Academies, Division of Behavioral and Social Sciences and Education, Washington, DC. [Google Scholar]
- 24. Brazier E, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome. BMJ. 1992;305:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Németh G. Health related quality of life outcome instruments. Eur Spine J. 2006;15(suppl 1):S44–S51. doi:10.1007/s00586-005-1046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–2952. [DOI] [PubMed] [Google Scholar]
- 27. Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976). 2004;29:803–814. [DOI] [PubMed] [Google Scholar]
- 28. Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL. Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J. 2013;22:2176–2183. doi:10.1007/s00586-013-2987-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chou P-H, Ma H-L, Wang S-T, Liu C-L, Chang M-C, Yu W-K. Fusion may not be a necessary procedure for surgically treated burst fractures of the thoracolumbar and lumbar spines. J Bone Joint Surg Am. 2014;96:1724–1731. doi:10.2106/JBJS.M.01486. [DOI] [PubMed] [Google Scholar]
- 30. Dai L-Y, Jiang L-S, Jiang S-D. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. a five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009;91:1033–1041. doi:10.2106/JBJS.H.00510. [DOI] [PubMed] [Google Scholar]
- 31. Post RB, Leferink VJM. Sagittal range of motion after a spinal fracture: does ROM correlate with functional outcome? Eur Spine J. 2004;13:489–494. doi:10.1007/s00586-003-0669-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Singh R, Rohilla RK, Kamboj K, Magu NK, Kaur K. Outcome of pedicle screw fixation and monosegmental fusion in patients with fresh thoracolumbar fractures. Asian Spine J. 2014;8:298–308. doi:10.4184/asj.2014.8.3.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wang S-T, Ma H-L, Liu C-L, Yu W-K, Chang M-C, Chen T-H. Is fusion necessary for surgically treated burst fractures of the thoracolumbar and lumbar spine? Spine (Phila Pa 1976). 2006;31:2646–2652. doi:10.1097/01.brs.0000244555.28310.40. [DOI] [PubMed] [Google Scholar]
- 34. Glassman SD, Dimar JR, Johnson JR, Minkow R. Preoperative SF-36 responses as a predictor of reoperation following lumbar fusion. Orthopedics. 1998;21:1201–1203. [DOI] [PubMed] [Google Scholar]
- 35. Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15(suppl 1):S93–S108. doi:10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Singh JA, Kwoh CK, Richardson D, Chen W, Ibrahim SA. Sex and surgical outcomes and mortality after primary total knee arthroplasty: a risk-adjusted analysis. Arthritis Care Res. 2013;65:1095–1102. doi:10.1002/acr.21953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cook CE, Arnold PM, Passias PG, Frempong-Boadu AK, Radcliff K, Isaacs R. Predictors of pain and disability outcomes in one thousand, one hundred and eight patients who underwent lumbar discectomy surgery. Int Orthop. 2015;39:2143–2151. doi:10.1007/s00264-015-2748-0. [DOI] [PubMed] [Google Scholar]
- 38. Häkkinen A, Kautiainen H, Järvenpää S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16:347–352. doi:10.1007/s00586-006-0187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord. 2006;44:427–431. doi:10.1038/sj.sc.3101857. [DOI] [PubMed] [Google Scholar]
- 40. Alonso J, Regidor E, Barrio G, Prieto L, Rodríguez C, de la Fuente L. Population reference values of the Spanish version of the Health Questionnaire SF-36 [in Spanish]. Med Clin (Barc). 1998;111:410–416. [PubMed] [Google Scholar]
- 41. Holtzman J, Saleh K, Kane R. Gender differences in functional status and pain in a Medicare population undergoing elective total hip arthroplasty. Med Care. 2002;40:461–470. [DOI] [PubMed] [Google Scholar]
- 42. Fishbain DA, Cutler RB, Cole B, et al. Are patients with chronic low back pain or chronic neck pain fatigued? Pain Med. 2004;5:187–195. [DOI] [PubMed] [Google Scholar]
- 43. Ellis DJ, Mallozzi SS, Mathews JE, et al. The relationship between preoperative expectations and the short-term postoperative satisfaction and functional outcome in lumbar spine surgery: a systematic review. Global Spine J. 2015;5:436–452. doi:10.1055/s-0035-1551650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Johanning JM, Gruenberg JC. The changing face of cholecystectomy. Am Surg. 1998;64:643–647. [PubMed] [Google Scholar]
- 45. Katz JN, Wright EA, Guadagnoli E, Liang MH, Karlson EW, Cleary PD. Differences between men and women undergoing major orthopedic surgery for degenerative arthritis. Arthritis Rheum. 1994;37:687–694. [DOI] [PubMed] [Google Scholar]
- 46. DeVine J, Norvell DC, Ecker E, et al. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery. Spine (Phila Pa 1976). 2011;36(21 suppl):S69–S74. doi:10.1097/BRS.0b013e31822ef6de. [DOI] [PubMed] [Google Scholar]
- 47. Ko S, Chae S. Correlations between the SF-36, the Oswestry-Disability Index and Rolland-Morris Disability Questionnaire in patients undergoing lumbar decompression according to types of spine origin pain [published online September 21, 2016]. Clin Spine Surg. doi:10.1097/BSD.0000000000000438. [DOI] [PubMed] [Google Scholar]
- 48. Veresciagina K, Ambrozaitis KV, Spakauskas B. The measurements of health-related quality-of-life and pain assessment in the preoperative patients with low back pain. Medicina (Kaunas, Lithuania). 2009;45:111–122. [PubMed] [Google Scholar]