Abstract
Study Design:
Retrospective trends analysis.
Objectives:
Cervical fusion is a common adjunctive surgical modality used in the treatment of cervical spondylotic myelopathy (CSM). The purpose of this study was to quantify national trends in patient demographics, hospital characteristics, and outcomes in the surgical management of CSM.
Methods:
This was a retrospective study that used the National Inpatient Sample. The sample included all patients over 18 years of age with a diagnosis of CSM who underwent cervical fusion from 2003 to 2013. The outcome measures were in-hospital mortality, length of stay, and hospital charges. Chi-square tests were performed to compare categorical variables. Independent t tests were performed to compare continuous variables.
Results:
We identified 62 970 patients with CSM who underwent cervical fusion from 2003 to 2013. The number of fusions performed per year in the treatment of CSM increased from 3879 to 8181. The average age of all fusion patients increased from 58.2 to 60.6 years (P < .001). Length of stay did not change significantly from a mean of 3.7 days. In-hospital mortality decreased from 0.6% to 0.3% (P < .01). Hospital charges increased from $49 445 to $92 040 (P < .001).
Conclusions:
This study showed a dramatic increase in cervical fusions to treat CSM from 2003 to 2013 concomitant with increasing age of the patient population. Despite increases in average age and number of comorbidities, length of stay remained constant and a decrease in mortality was seen across the study period. However, hospital charges increased dramatically.
Keywords: cervical spondylotic myelopathy, anterior cervical fusion, posterior cervical fusion, NIS, National Inpatient Sample, trends, mortality, hospital charges
Introduction
Cervical spondylotic myelopathy (CSM) is the most common spinal disorder among adults in the United States.1,2 Without surgical intervention, it is estimated that 20% to 60% of CSM patients with mild disease will deteriorate.3 Surgical intervention via decompression of the spinal cord is warranted for CSM when symptoms progress or when patients present with substantial neurological impairment.3–5
Prior studies have assessed epidemiological trends,6 compared the effectiveness of different surgical approaches,7–21 and estimated the cost of the surgical management of CSM.22,23 In 2005, an estimated 45 cervical fusions were performed per 100 000 Medicare beneficiaries, and CSM was the most common diagnosis made prior to these procedures.2 While Wang et al quantified the rate of cervical fusions overall, it is currently unknown how national trends in cervical fusion for CSM specifically evolved over the last decade. The most recent study of this question used data from 1993 to 2002, where Lad et al found that there was a 7-fold increase in the number of fusions performed in the treatment of CSM.6 However, the US population is aging, and the incidence of degenerative conditions of the cervical spine likely increases with age.24,25 Since 2002, both the incidence of CSM and the number of surgical modalities used to treat CSM would be expected to increase. Therefore, it is important to quantify the extent to which cervical fusion is being used to treat CSM, providing an update to the results published by Lad et al. It is similarly important to document the changing demographic and comorbidity profiles of the surgical CSM population so that patients, surgeons, and hospital systems can better anticipate surgical volume, the demographics of CSM patients undergoing cervical fusion, and associated outcomes.
The present study uses the National Inpatient Sample (NIS) to quantify trends in anterior and posterior spinal fusions for patients with CSM. We hypothesized that demographics, comorbidity burden, insurance status, and hospital charges associated with cervical fusions for CSM changed significantly from 2003 to 2013.
Methods
Data Source
This study used the NIS to collect data on CSM patients who underwent cervical fusion from 2003 to 2013. The name was changed from the Nationwide Inpatient Sample to the National Inpatient Sample in 2012, when changes were made to the sampling strategy of the database. The NIS includes analytical weights that allow for data to be used simultaneously from both before (pre-2012) and after (2012-present) the change in sampling strategy.
Data is recorded in the NIS using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes.26 Patients were identified by the ICD-9-CM diagnosis code for CSM, 721.1, and procedure codes for index anterior cervical fusion (ACF) and index posterior cervical fusion (PCF), 81.02 and 81.03, respectively. Revision procedures were excluded. Other procedures used to treat CSM were excluded because the focus of this study was on fusion specifically, there is no ICD-9-CM code for anterior-posterior fusion, and the coding for laminoplasty is not specific. Furthermore, only subaxial (C2-T1) cervical spinal fusions were included because of the heterogeneity in underlying etiology for CSM in the atlantoaxial cervical spine.27
Study Population
All hospitalized CSM patients of at least 18 years of age who underwent subaxial cervical fusion were initially included in this study. Data points included patient demographics (eg, age, gender, race, comorbidity burden, and primary insurance provider) and hospital characteristics (eg, hospital size [based on the number of beds; varies based on hospital region location, and teaching status], geographic location [Northeast, Midwest, South, West], and teaching status).
Outcome Definitions
In-hospital mortality, length of stay (LOS), and hospital charges served as our outcome variables. The NIS gathers data on in-hospital events; therefore, postdischarge mortality could not be assessed in the present study. Hospital charges were adjusted for inflation to 2013 US dollars using the Bureau of Labor Statistics CPI Inflation Calculator.28
Statistical Analysis
Absolute values, means, and frequencies for patient demographics, hospital characteristics, and outcomes were calculated for each year from 2003 to 2013. Calculations were done using the sampling weights provided by the NIS to account for the stratified sampling design of the database. The sampling weights used were from after the NIS redesign in 2012, which allowed for trends to be studied across the years before and after the redesign.
Chi-square tests were used to compare categorical variables (eg, gender, race, comorbidities, insurance status, hospital size, hospital region, academic institution, and mortality) in 2003 compared to 2013. Independent t tests using the Satterthwaite method were used to compare continuous variables (eg, age, LOS, and hospital charges) in 2003 compared to 2013. Analyses were performed using SAS version 9.4. Our α level for determining statistical significance was set at P < .01. This study did not require institutional review board approval.
Results
All Fusions
From 2003 to 2013, 62 970 patients with CSM, and who underwent cervical fusion, were identified. The number of fusions per year increased from 3879 to 8181. Patient demographics, hospital characteristics, and outcome data for all patients are shown in Table 1.
Table 1.
Patient Demographics, Hospital Characteristics, and Outcomes for Cervical Fusions in the Treatment of CSMa.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of fusions | 3879 | 4096 | 4307 | 4494 | 5115 | 5562 | 5624 | 6635 | 7603 | 7474 | 8181 | |
| Age** | 58.2 | 58.0 | 58.5 | 58.3 | 59.0 | 59.1 | 59.8 | 59.6 | 60.5 | 60.1 | 60.6 | <.001 |
| Female | 1695 (43.9) | 1916 (46.8) | 2038 (47.4) | 2065 (46.0) | 2382 (46.6) | 2522 (45.4) | 2505 (44.5) | 3015 (45.5) | 3429 (45.1) | 3442 (46.1) | 3737 (45.7) | .10 |
| Race | ||||||||||||
| White** | 2265 (58.4) | 2272 (55.5) | 2615 (60.7) | 2607 (58.0) | 2874 (56.2) | 3454 (62.1) | 3669 (65.2) | 4418 (66.6) | 5201 (68.4) | 5359 (71.1) | 5849 (71.5) | <.001 |
| Black* | 389 (10.0) | 425 (10.4) | 361 (8.4) | 450 (10.0) | 437 (8.5) | 582 (10.5) | 539 (9.6) | 846 (12.8) | 1045 (13.7) | 973 (13.0) | 1091 (13.3) | .01 |
| Other* | 270 (7.0) | 209 (5.1) | 269 (6.2) | 282 (6.3) | 347 (6.8) | 413 (7.4) | 546 (9.7) | 582 (8.8) | 806 (10.6) | 777 (10.4) | 795 (9.7) | .01 |
| Comorbidity | ||||||||||||
| 0** | 1347 (34.7) | 1259 (30.7) | 1255 (29.1) | 1146 (25.5) | 1212 (23.7) | 1299 (23.4) | 1229 (21.9) | 1397 (21.1) | 1416 (18.6) | 1392 (18.6) | 1484 (18.1) | <.001 |
| 1** | 1172 (30.2) | 1263 (30.8) | 1259 (29.2) | 1307 (29.1) | 1450 (28.3) | 1461 (26.3) | 1534 (27.3) | 1718 (25.9) | 1883 (24.8) | 1909 (25.5) | 1976 (24.2) | <.001 |
| 2* | 787 (20.3) | 870 (21.2) | 920 (21.4) | 1033 (23.0) | 1197 (23.4) | 1343 (24.1) | 1217 (21.6) | 1489 (22.4) | 1732 (22.8) | 1680 (22.5) | 1913 (23.4) | <.01 |
| 3+** | 573 (14.8) | 704 (17.2) | 873 (20.3) | 1008 (22.4) | 1256 (24.6) | 1459 (26.2) | 1644 (29.2) | 2031 (30.6) | 2572 (33.8) | 2493 (33.4) | 2808 (34.3) | <.001 |
| Insurance | ||||||||||||
| Private** | 1915 (49.4) | 2019 (49.3) | 2095 (48.6) | 2265 (50.4) | 2417 (47.3) | 2515 (45.2) | 2571 (45.7) | 2808 (42.3) | 3101 (40.8) | 2967 (39.7) | 3243 (39.6) | <.001 |
| Medicare** | 1413 (36.4) | 1442 (35.2) | 1630 (37.8) | 1702 (37.9) | 1978 (38.7) | 2175 (39.1) | 2214 (39.4) | 2739 (41.3) | 3322 (43.7) | 3325 (44.5) | 3650 (44.6) | <.001 |
| Medicaid* | 197 (5.1) | 259 (6.3) | 261 (6.1) | 242 (5.4) | 281 (5.5) | 409 (7.4) | 366 (6.5) | 487 (7.3) | 515 (6.8) | 538 (7.2) | 576 (7.0) | <.01 |
| Uninsured | 55 (1.4) | 91 (2.2) | 62 (1.4) | 55 (1.2) | 102 (2.0) | 95 (1.7) | 98 (1.7) | 130 (2.0) | 128 (1.7) | 143 (1.9) | 158 (1.9) | .17 |
| Academic hospital | 2260 (58.3) | 2585 (63.1) | 2158 (50.1) | 2717 (60.5) | 3082 (60.3) | 3351 (60.2) | 3069 (54.6) | 3755 (56.6) | 4551 (59.9) | 4610 (61.7) | 5139 (62.8) | .30 |
| Hospital size | ||||||||||||
| Small** | 236 (6.1) | 371 (9.1) | 410 (9.5) | 524 (11.7) | 803 (15.7) | 436 (7.8) | 669 (11.9) | 882 (13.3) | 894 (11.8) | 968 (13.0) | 1075 (13.1) | <.001 |
| Medium | 1035 (26.7) | 830 (20.3) | 878 (20.4) | 955 (21.3) | 991 (19.4) | 1157 (20.8) | 1117 (19.9) | 1219 (18.4) | 1374 (18.1) | 1622 (21.7) | 1871 (22.9) | .41 |
| Large | 2608 (67.2) | 2895 (70.7) | 3019 (70.1) | 3015 (67.1) | 3321 (64.9) | 3969 (71.4) | 3705 (65.9) | 4469 (67.4) | 5246 (69.0) | 4884 (65.3) | 5235 (64.0) | .30 |
| Hospital region | ||||||||||||
| Northeast | 541 (13.9) | 654 (16.0) | 595 (13.8) | 701 (15.6) | 635 (12.4) | 918 (16.5) | 861 (15.3) | 908 (13.7) | 971 (12.8) | 1190 (15.9) | 1269 (15.5) | .77 |
| Midwest | 659 (17.0) | 803 (19.6) | 1014 (23.5) | 870 (19.4) | 1051 (20.5) | 1090 (19.6) | 1150 (20.4) | 1390 (20.9) | 1561 (20.5) | 1545 (20.7) | 1592 (19.5) | .64 |
| South | 2055 (53.0) | 1953 (47.7) | 1996 (46.3) | 2104 (46.8) | 2342 (45.8) | 2535 (45.6) | 2425 (43.1) | 2792 (42.1) | 3351 (44.1) | 3093 (41.4) | 3587 (43.8) | .18 |
| West | 624 (16.1) | 686 (16.7) | 702 (16.3) | 819 (18.2) | 1087 (21.3) | 1019 (18.3) | 1188 (21.1) | 1545 (23.3) | 1720 (22.6) | 1646 (22.0) | 1733 (21.2) | .28 |
| Mortality* | 24 (0.6) | 25 (0.6) | 23 (0.5) | 15 (0.3) | 23 (0.4) | 26 (0.5) | 24 (0.4) | 26 (0.4) | 32 (0.4) | 23 (0.3) | 22 (0.3) | <.01 |
| LOS | 3.6 | 4.0 | 3.5 | 3.7 | 3.6 | 3.6 | 3.7 | 3.9 | 3.9 | 3.6 | 3.6 | .87 |
| Hospital charge, $ (inflated to 2013)** | 49 445 | 54 452 | 55 865 | 61 129 | 68 087 | 77 015 | 78 305 | 85 934 | 93 628 | 87 367 | 92 040 | <.001 |
Abbreviations: CSM, cervical spondylotic myelopathy; LOS, length of stay; NIS, National Inpatient Sample.
aAll data is from the NIS and include patients over 18 years of age that underwent cervical spinal fusion in the treatment of CSM from 2003 to 2013. Data is expressed as a raw value with the percentage in parentheses. Data from 2003 was compared with 2013 for a single category to determine statistical significance.
*Denotes statistical significance at P < .01. **Denotes statistical significance at P < .001.
The percentage of fusion patients that were white increased significantly from 58.4% in 2003 to 71.5% in 2013 (P < .001). The mean age increased significantly from 58.2 to 60.6 years (P < .001). The percentage with no comorbidities and 1 comorbidity decreased from 34.7% to 18.1% (P < .001) and 30.2% to 24.2% (P < .001), respectively, over the study period. Conversely, the percentage of patients with 2 comorbidities and 3 or more comorbidities increased from 20.3% to 23.4% (P < .01) and 14.8% to 34.3% (P < .001), respectively (Figure 1).
Figure 1.
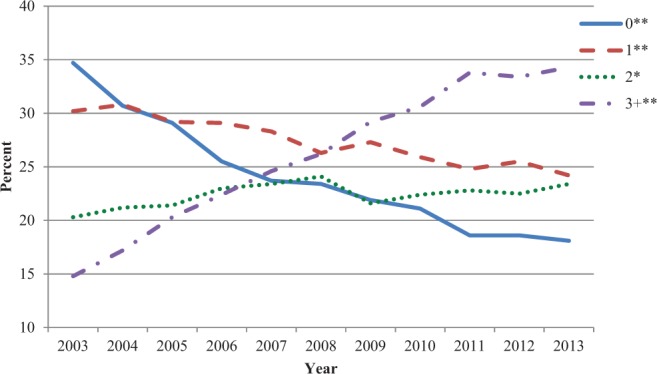
Number of comorbidities by percentage for all cervical spondylotic myelopathy (CSM) patients undergoing cervical fusion. The trends in the average number of comorbidities by percentage are shown for all CSM patients undergoing cervical fusion. Data from 2003 was compared to data from 2013 by number of comorbidities to determine statistically significant changes over time. A “*” denotes statistical significance with P < .01. A “**” represents statistical significance with P < .001.
Medicare (36.4% to 44.6%, P < .001) and Medicaid (5.1% to 7.0% P < .01) primary payers increased significantly, whereas private insurance payers (49.4% to 39.6%, P < .001) decreased significantly from 2003 to 2013 (Table 1 and Figure 2).
Figure 2.
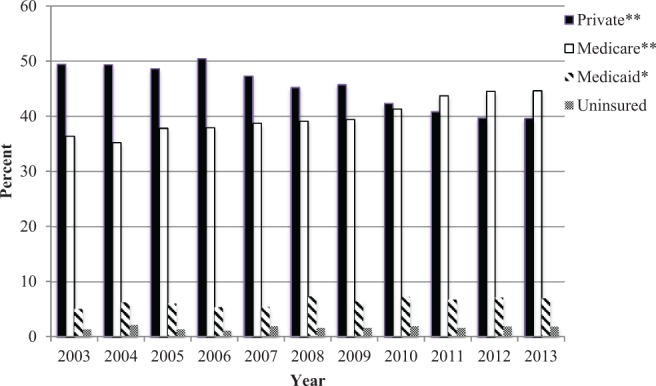
Breakdown of insurance status by percentage for all cervical spondylotic myelopathy (CSM) patients undergoing cervical fusion. The percentage of CSM patients undergoing cervical fusions are represented by insurance status. Data from 2003 was compared to data from 2013 by beneficiary to determine statistically significant changes over time. A “*” denotes statistical significance with P < .01. A “**” represents statistical significance with P < .001.
Cervical fusions were increasingly performed at smaller hospitals (6.1% to 13.1%, P < .001, as defined by the NIS). The majority of procedures were performed in the South (53.0% in 2003, 43.8% in 2013). There were no statistically significant changes in medium or large hospital centers or in geographic regions across the United States (Table 1).
Throughout the study period, LOS remained unchanged, with a mean of 3.7 days. However, in-hospital mortality rate following cervical fusion decreased from 0.6% to 0.3%, P < .01 (Table 1). Mean hospital charges increased from $49 445 (adjusted for inflation to 2013 US dollars) to $92 040, P < .001.
Anterior and Posterior Cervical Fusions
Trends in patient demographics, hospital characteristics, and outcomes were further analyzed according to surgical approach (ACF [Table 2] and PCF [Table 3]). In 2003, 3226 CSM patients underwent ACF and 830 patients underwent PCF; in 2013, 6204 patients underwent ACF and 2416 patients underwent PCF (Figure 3). Trends for ACF and PCF were broadly similar to the all fusion cohort.
Table 2.
Patient Demographics, Hospital Characteristics, and Outcomes for ACF in the Treatment of CSMa.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of ACFs | 3226 | 3228 | 3530 | 3623 | 4128 | 4214 | 4494 | 5136 | 5818 | 5721 | 6204 | |
| Age** | 57.4 | 56.7 | 57.6 | 57.3 | 58.0 | 57.8 | 58.8 | 58.6 | 59.4 | 58.9 | 59.6 | <.001 |
| Female | 1475 (46.0) | 1563 (48.5) | 1728 (49.0) | 1731 (47.8) | 1988 (48.2) | 1974 (46.9) | 2096 (46.6) | 2389 (46.5) | 2774 (47.7) | 2732 (47.8) | 2920 (47.1) | .35 |
| Race | ||||||||||||
| White** | 1885 (58.4) | 1760 (54.5) | 2154 (61.0) | 2130 (58.8) | 2329 (56.4) | 2696 (64.0) | 2974 (66.2) | 3436 (66.9) | 4029 (69.3) | 4138 (72.3) | 4511 (72.7) | <.001 |
| Black | 299 (9.3) | 330 (10.2) | 284 (8.0) | 327 (9.0) | 347 (8.4) | 413 (9.8) | 403 (9.0) | 615 (12.0) | 737 (12.7) | 708 (12.4) | 765 (12.3) | .02 |
| Other | 228 (7.1) | 159 (4.9) | 205 (5.8) | 207 (5.7) | 243 (5.9) | 304 (7.2) | 417 (9.3) | 444 (8.6) | 592 (10.2) | 591 (10.3) | 598 (9.6) | .03 |
| Comorbidity | ||||||||||||
| 0** | 1194 (37.0) | 1065 (33.0) | 1115 (31.6) | 999 (27.6) | 1059 (25.7) | 1094 (26.0) | 1082 (24.1) | 1185 (23.1) | 1191 (20.5) | 1210 (21.2) | 1253 (20.2) | <.001 |
| 1** | 963 (29.9) | 1001 (31.0) | 1056 (29.9) | 1096 (30.3) | 1206 (29.2) | 1135 (27.0) | 1255 (27.9) | 1384 (26.9) | 1486 (25.5) | 1505 (26.3) | 1581 (25.5) | <.001 |
| 2** | 623 (19.3) | 666 (20.6) | 705 (20.0) | 818 (22.6) | 932 (22.6) | 1013 (24.0) | 941 (20.9) | 1141 (22.2) | 1328 (22.8) | 1301 (22.7) | 1442 (23.2) | <.001 |
| 3+** | 446 (13.8) | 496 (15.4) | 654 (18.5) | 710 (19.6) | 931 (22.6) | 972 (23.1) | 1216 (27.1) | 1426 (27.8) | 1813 (31.2) | 1705 (29.8) | 1928 (31.1) | <.001 |
| Insurance | ||||||||||||
| Private** | 1693 (52.5) | 1710 (53.0) | 1806 (51.2) | 1952 (53.9) | 2068 (50.1) | 2069 (49.1) | 2192 (48.8) | 2330 (45.4) | 2540 (43.7) | 2425 (42.4) | 2624 (42.3) | <.001 |
| Medicare** | 1074 (33.3) | 998 (30.9) | 1247 (35.3) | 1249 (34.5) | 1486 (36.0) | 1485 (35.2) | 1640 (36.5) | 1960 (38.2) | 2347 (40.3) | 2358 (41.2) | 2596 (41.8) | <.001 |
| Medicaid* | 155 (4.8) | 203 (6.3) | 200 (5.7) | 185 (5.1) | 210 (5.1) | 299 (7.1) | 286 (6.4) | 380 (7.4) | 385 (6.6) | 417 (7.3) | 413 (6.7) | <.01 |
| Uninsured | 48 (1.5) | 71 (2.2) | 49 (1.4) | 43 (1.2) | 79 (1.9) | 64 (1.5) | 72 (1.6) | 94 (1.8) | 99 (1.7) | 108 (1.9) | 117 (1.9) | .33 |
| Academic hospital | 1776 (55.1) | 1919 (59.4) | 1671 (47.3) | 2045 (56.4) | 2347 (56.9) | 2335 (55.4) | 2251 (50.1) | 2744 (53.4) | 3182 (54.7) | 3323 (58.1) | 3664 (59.1) | .37 |
| Hospital size | ||||||||||||
| Small** | 194 (6.0) | 301 (9.3) | 341 (9.7) | 411 (11.3) | 680 (16.5) | 387 (9.2) | 586 (13.0) | 738 (14.4) | 742 (12.8) | 812 (14.2) | 901 (14.5) | <.001 |
| Medium | 904 (28.0) | 694 (21.5) | 738 (20.9) | 784 (21.6) | 840 (20.3) | 910 (21.6) | 858 (19.1) | 959 (18.7) | 1116 (19.2) | 1284 (22.4) | 1425 (23.0) | .29 |
| Large | 2128 (66.0) | 2233 (69.2) | 2451 (69.4) | 2428 (67.0) | 2608 (63.2) | 2917 (69.2) | 2932 (65.2) | 3390 (66.0) | 3899 (67.0) | 3625 (63.4) | 3878 (62.5) | .28 |
| Hospital region | ||||||||||||
| Northeast | 400 (12.4) | 494 (15.3) | 429 (12.2) | 504 (13.9) | 476 (11.5) | 609 (14.5) | 612 (13.6) | 588 (11.4) | 607 (10.4) | 818 (14.3) | 836 (13.5) | .86 |
| Midwest | 554 (17.2) | 619 (19.2) | 799 (22.6) | 710 (19.6) | 844 (20.4) | 783 (18.6) | 855 (19.0) | 1100 (21.4) | 1196 (20.6) | 1119 (19.5) | 1160 (18.7) | .83 |
| South | 1710 (53.0) | 1545 (47.9) | 1711 (48.5) | 1718 (47.4) | 1893 (45.9) | 2011 (47.7) | 2058 (45.8) | 2227 (43.4) | 2715 (46.7) | 2502 (43.7) | 2879 (46.4) | .41 |
| West | 562 (17.4) | 570 (17.7) | 591 (16.7) | 691 (19.1) | 915 (22.2) | 811 (19.2) | 969 (21.6) | 1221 (23.8) | 1300 (22.3) | 1282 (22.4) | 1329 (21.4) | .45 |
| Mortality* | 18 (0.6) | 15 (0.5) | 19 (0.5) | 7 (0.2) | 17 (0.4) | 16 (0.4) | 18 (0.4) | 20 (0.4) | 21 (0.4) | 15 (0.3) | 14 (0.2) | <.01 |
| LOS | 3.2 | 3.4 | 2.9 | 3.1 | 3.1 | 3.0 | 3.1 | 3.3 | 3.2 | 2.9 | 3.1 | .21 |
| Hospital charge, $ (inflated to 2013)** | 46 804 | 49 963 | 51 234 | 56 208 | 61 469 | 68 501 | 71 117 | 77 314 | 85 192 | 78 153 | 83 930 | <.001 |
aAll data is from the NIS and include patients over 18 years of age that underwent ACF in the treatment of CSM from 2003 to 2013. Data is expressed as a raw value with the percentage in parentheses. Data from 2003 was compared with 2013 for a single category to determine statistical significance.
*Denotes statistical significance at P < .01.
**Denotes statistical significance at P < .001.
Abbreviations: ACF, anterior cervical fusion; CSM, cervical spondylotic myelopathy; LOS, length of stay; NIS, National Inpatient Sample.
Table 3.
Patient Demographics, Hospital Characteristics, and Outcomes for PCF in the Treatment of CSMa.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of PCFs | 830 | 1017 | 989 | 1109 | 1182 | 1666 | 1454 | 1919 | 2228 | 2155 | 2416 | |
| Age* | 61.8 | 62.2 | 62.4 | 61.6 | 62.6 | 62.4 | 63.0 | 62.7 | 63.8 | 63.5 | 63.3 | <.01 |
| Female* | 306 (36.9) | 426 (41.9) | 407 (41.3) | 453 (40.9) | 480 (40.6) | 676 (40.6) | 542 (37.3) | 812 (42.3) | 855 (38.4) | 891 (41.3) | 1014 (42.0) | <.01 |
| Race | ||||||||||||
| White* | 474 (57.1) | 596 (58.6) | 587 (59.4) | 597 (53.8) | 640 (54.1) | 962 (57.7) | 901 (62.0) | 1256 (65.5) | 1484 (66.6) | 1507 (69.9) | 1643 (68.0) | <.01 |
| Black | 111 (13.4) | 111 (10.9) | 93 (9.4) | 142 (12.8) | 117 (9.9) | 204 (12.2) | 168 (11.6) | 284 (14.8) | 370 (16.6) | 315 (14.6) | 392 (16.2) | .17 |
| Other | 62 (7.5) | 58 (5.7) | 71 (7.2) | 90 (8.1) | 127 (10.7) | 136 (8.2) | 172 (11.8) | 172 (9.0) | 265 (11.9) | 232 (10.8) | 237 (9.8) | .16 |
| Comorbidity | ||||||||||||
| 0** | 196 (23.6) | 227 (22.3) | 191 (19.3) | 194 (17.5) | 186 (15.7) | 262 (15.7) | 185 (12.7) | 261 (13.6) | 264 (11.8) | 233 (10.8) | 268 (11.1) | <.001 |
| 1** | 267 (32.2) | 307 (30.2) | 250 (25.3) | 274 (24.7) | 286 (24.2) | 383 (23.0) | 355 (24.4) | 433 (22.6) | 480 (21.5) | 479 (22.2) | 488 (20.2) | <.001 |
| 2 | 201 (24.2) | 242 (23.8) | 262 (26.5) | 270 (24.3) | 308 (26.1) | 413 (24.8) | 352 (24.2) | 427 (22.3) | 513 (23.0) | 467 (21.7) | 587 (24.3) | .86 |
| 3+** | 166 (20.0) | 241 (23.7) | 286 (28.9) | 371 (33.5) | 402 (34.0) | 608 (36.5) | 562 (38.7) | 798 (41.6) | 971 (43.6) | 976 (45.3) | 1073 (44.4) | <.001 |
| Insurance | ||||||||||||
| Private | 298 (35.9) | 373 (36.7) | 384 (38.8) | 434 (39.1) | 426 (36.0) | 579 (34.8) | 514 (35.4) | 652 (34.0) | 741 (33.3) | 686 (31.8) | 793 (32.8) | .15 |
| Medicare | 417 (50.2) | 503 (49.5) | 476 (48.1) | 545 (49.1) | 583 (49.3) | 825 (49.5) | 715 (49.2) | 965 (50.3) | 1176 (52.8) | 1167 (54.2) | 1258 (52.1) | .38 |
| Medicaid | 55 (6.6) | 66 (6.5) | 71 (7.2) | 70 (6.3) | 82 (6.9) | 133 (8.0) | 106 (7.3) | 135 (7.0) | 154 (6.9) | 147 (6.8) | 190 (7.9) | .32 |
| Uninsured | 10 (1.2) | 25 (2.5) | 14 (1.4) | 12 (1.1) | 25 (2.1) | 35 (2.1) | 28 (1.9) | 45 (2.3) | 38 (1.7) | 45 (2.1) | 49 (2.0) | .14 |
| Academic hospital | 605 (72.9) | 778 (76.5) | 609 (61.6) | 832 (75.0) | 851 (72.0) | 1213 (72.8) | 1010 (69.5) | 1261 (65.7) | 1612 (72.4) | 1543 (71.6) | 1767 (73.1) | .92 |
| Hospital size | ||||||||||||
| Small | 53 (6.4) | 79 (7.8) | 79 (8.0) | 134 (12.1) | 145 (12.3) | 64 (3.8) | 113 (7.8) | 197 (10.3) | 189 (8.5) | 186 (8.6) | 217 (9.0) | .17 |
| Medium | 177 (21.3) | 164 (16.1) | 168 (17.0) | 204 (18.4) | 189 (16.0) | 306 (18.4) | 322 (22.1) | 347 (18.1) | 351 (15.8) | 424 (19.7) | 540 (22.4) | .85 |
| Large | 600 (72.3) | 774 (76.1) | 742 (75.0) | 771 (69.5) | 848 (71.7) | 1296 (77.8) | 1000 (68.8) | 1352 (70.5) | 1654 (74.2) | 1545 (71.7) | 1659 (68.7) | .41 |
| Hospital region | ||||||||||||
| Northeast | 172 (20.7) | 183 (18.0) | 198 (20.0) | 236 (21.3) | 202 (17.1) | 354 (21.2) | 298 (20.5) | 386 (20.1) | 426 (19.1) | 428 (19.9) | 499 (20.7) | .87 |
| Midwest | 139 (16.7) | 215 (21.1) | 280 (28.3) | 222 (20.0) | 242 (20.5) | 352 (21.1) | 354 (24.3) | 395 (20.6) | 448 (20.1) | 517 (24.0) | 523 (21.6) | .38 |
| South | 428 (51.6) | 460 (45.2) | 356 (36.0) | 460 (41.5) | 506 (42.8) | 677 (40.6) | 492 (33.8) | 707 (36.8) | 829 (37.2) | 726 (33.7) | 873 (36.1) | .06 |
| West | 91 (11.0) | 159 (15.6) | 155 (15.7) | 191 (17.2) | 232 (19.6) | 283 (17.0) | 310 (21.3) | 431 (22.5) | 525 (23.6) | 484 (22.5) | 521 (21.6) | .05 |
| Mortality* | 9 (1.1) | 12 (1.2) | 10 (1.0) | 9 (0.8) | 10 (0.8) | 11 (0.7) | 11 (0.8) | 13 (0.7) | 17 (0.8) | 11 (0.5) | 8 (0.3) | <.01 |
| LOS | 6.1 | 6.5 | 6.3 | 6.4 | 6.2 | 5.9 | 6.4 | 6.5 | 6.5 | 6.0 | 5.8 | .19 |
| Hospital charge, $ (inflated to 2013)** | 72 208 | 77 783 | 86 688 | 92 448 | 104 692 | 113 838 | 125 357 | 128 851 | 140 303 | 131 509 | 134 895 | <.001 |
Abbreviations: PCF, posterior cervical fusion; CSM, cervical spondylotic myelopathy; LOS, length of stay; NIS, National Inpatient Sample.
aAll data is from the NIS and include patients over 18 years of age who underwent PCF in the treatment of CSM from 2003 to 2013. Data is expressed as a raw value with the percentage in parentheses. Data from 2003 was compared with 2013 for a single category to determine statistical significance.
*Denotes statistical significance at P < .01. **Denotes statistical significance at P < .001.
Figure 3.
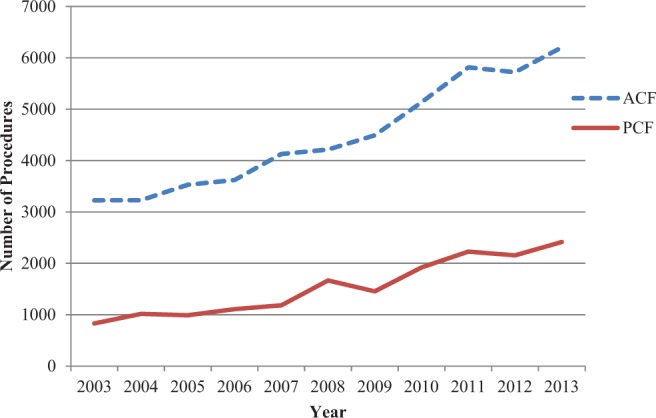
Number of cervical fusions performed per year in the treatment of cervical spondylotic myelopathy (CSM). The number of fusions performed in the treatment of CSM are stratified by procedure (anterior cervical fusion [ACF] and posterior cervical fusion [PCF]) from 2003 to 2013.
Throughout the study period, PCF patients were older than ACF patients (P < .01; Figure 4). The average age increased from 57.4 to 59.6 years (P < .001) for ACF and from 61.8 to 63.3 years (P < .01) for PCF. The trends in comorbidity burden of ACF and PCF patients mirrored the trends of the all fusions cohort (Tables 2 and 3).
Figure 4.
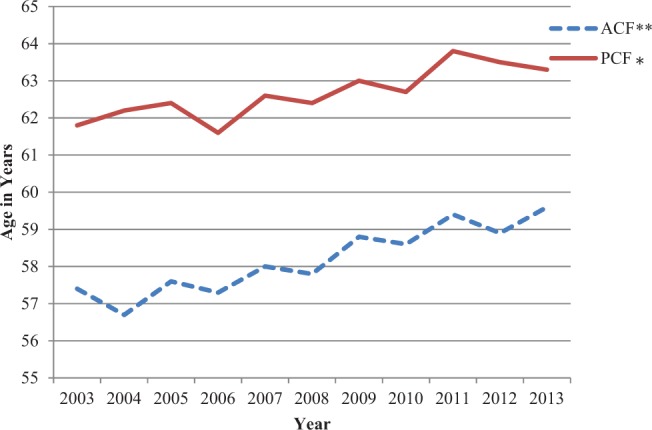
Average age of cervical spondylotic myelopathy (CSM) patients undergoing anterior cervical fusion (ACF) and posterior cervical fusion (PCF). The trends in the average age of CSM patients undergoing ACF and PCF are shown. PCF patients were significantly older than ACF patients (P < .01). Data from 2003 was compared to data from 2013 by procedure to determine statistically significant changes over time. A “*” denotes statistical significance with P < .01. A “**” represents statistical significance with P < .001.
The proportion of ACF patients with Medicare (33.3% in 2003 to 41.8% in 2013, P < .001) or Medicaid (4.8% in 2003 to 6.7% in 2013, P < .01) increased, whereas the proportion of ACF patients with private insurance decreased (52.5% to 42.3%, P < .001; Table 2). However, PCF patients with Medicare, Medicaid, or private insurance remained constant (Table 3). Finally, ACF was increasingly performed at community hospitals (6.0% in 2003 to 14.5% in 2013, P < .001); however, there was not a significant change in the PCF cohort.
LOS remained relatively unchanged following both ACF and PCF, at a mean of 3.1 days and 6.2 days, respectively. In-hospital mortality rates declined following both ACF (0.6% to 0.2%, P < .01) and PCF (1.1% to 0.3%, P < .01; Figure 5). Inflation-adjusted charges increased for both ACF ($46 804 in 2003 to $83 930 in 2013, P < .001) and PCF ($72 208 in 2003 to $134 895 in 2013, P < .001; Figure 6).
Figure 5.
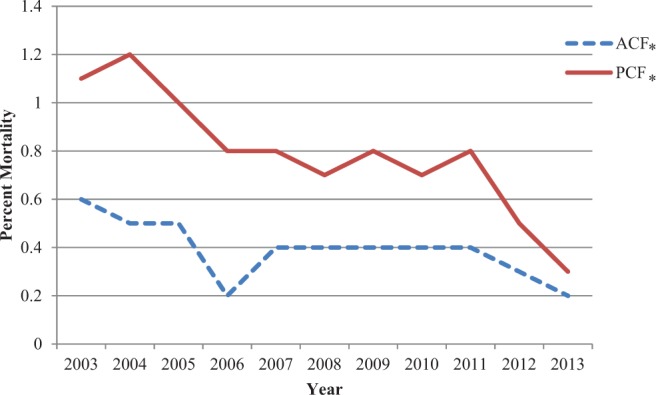
Trends in in-hospital mortality following anterior cervical fusion (ACF) and posterior cervical fusion (PCF) in the treatment of cervical spondylotic myelopathy (CSM). Declining trends in in-hospital mortality percentage are shown for ACF and PCF. Data from 2003 wascompared to data from 2013 by procedure to determine statistically significant changes over time. A “*” denotes statistical significance with P < .01.
Figure 6.
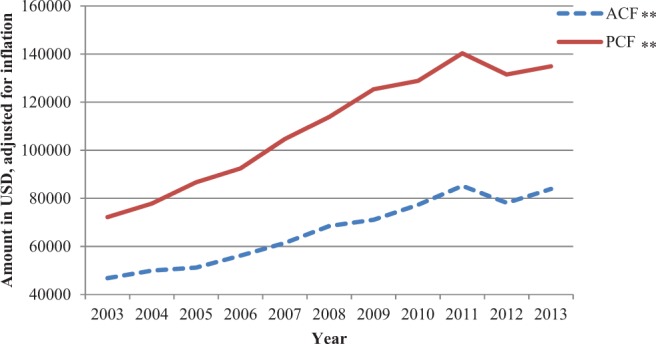
Trends in hospital charges for cervical fusions in the treatment of cervical spondylotic myelopathy (CSM). Trends in the average hospital charges for anterior cervical fusion (ACF) and posterior cervical fusion (PCF) performed in the treatment of CSM are shown. Charge data from 2003 was compared to data from 2013 by procedure to determine statistically significant changes over time. A “**” represents statistical significance with P < .001.
Discussion
The health care landscape in the United States has evolved considerably over the past decade, and the present study describes updated trends in the use of cervical spine fusion to treat CSM. The NIS is the largest all-payer, nationally representative database of hospital discharges in the United States, rendering the NIS an optimal resource for studying epidemiological trends in CSM management. In our study, we hypothesized that patient demographics would change significantly, along with comorbidity burden, and hospital charges would increase over the studied time period.6
To our knowledge, the present study is the first to describe trends in the use of any surgical modality to treat CSM over the past decade. Reporting these updated trends could provide spine surgeons with baseline knowledge of the CSM patient population treated with cervical fusion. Mirroring the increasing average age of the US population,25,29 we found the numbers of cervical fusions for CSM increased from 2003 to 2013. Moreover, average age and number of comorbidities increased, and smaller hospitals were performing more fusions. Hospital charges more than doubled over this decade, while LOS did not change.
All Fusions
The growth in the utilization of surgical procedures to treat common pathologies of the cervical spine has been well documented.2,28,30,31 For example, from 1998 to 2008, Rajaee et al reported a 114% increase in the number of primary cervical fusions for all pathologies.30 As the most common disorder of the cervical spine, the prevalence of CSM is expected to increase as the US population ages.1,2 The unique symptomatology of CSM compared to other degenerative conditions of the cervical spine suggests that trends in fusion for CSM should be studied separately from those of other conditions. Grouping CSM with other pathologies of the subaxial spine to study trends in the use of fusion would introduce substantial heterogeneity to the study sample and would therefore limit the generalizability of the results. Furthermore, prior studies have asked a similar question of data from the previous decade. Using the NIS, Lad et al analyzed data on 138 792 patients admitted with a diagnosis of CSM from 1993 to 2002 to study epidemiological trends in the surgical management of CSM. The authors found a 7-fold increase in the number of cervical fusions performed in the management of CSM when comparing the years 1998-2002 and 1993-1997.6 Similarly, we found that the number of fusions per year increased from 3879 in 2003 to 8181 in 2013, a 210.9% increase. In contrast to Lad et al, we examined each year in the study period individually.
The drivers of the growth in the number of cervical fusions to treat CSM are likely multifactorial. First, as the US population continues to age,25,29 more patients are presenting with signs and symptoms of CSM, as degenerative changes associated with CSM are age-related.24 Second, with growing numbers of fellowship-trained spine surgeons,32 it is possible to increase the volume of cervical fusion in a given year. Finally, advances in surgical instrumentation in recent decades have made preforming fusions easier and safer and have allowed for a great number of patients to undergo cervical fusions in the treatment of CSM earlier in the course of their disease.33
Prior studies have reported increasing age and comorbidity burden of surgical spine patients without worse outcomes.28,30,32,34–37 Similarly, Lad et al found the majority of CSM patients receiving surgery were 45 to 64 years old (49% from 1993 to 1997 and 53% from 1998 to 2002) and the number of patients with 3 comorbidities increased from 5.7% to 17.9%.6 Lad et al also found a statistically significant decrease in the average LOS from 4.88 to 3.68 days, while mortality remained stable.6 We found similar demographic trends of increasing age and increasing average comorbidity burden. In contrast to Lad et al, we found LOS remained stable at a mean of 3.7 days and mortality decreased from 0.6% to 0.3%. The discrepancy in mortality rates might be due to improvements in surgical and anesthetic techniques in the last decade.
The trend of increasing hospital charges can likely be attributed to the CSM population growing older and presenting with greater comorbidity burdens. Charges are trending upward throughout the health care system. For example, Alosh et al found that yearly charges for cervical spine procedures increased from $1.62 billion in 2000 to $5.63 billion in 2009.38 However, hospital charges are not costs, and increases may reflect changes in reimbursement structures.39 The increasing age and comorbidity burden may also explain, in part, the significant increases we observed in the share of patients with Medicare (36.4% to 44.6%, P < .001) and Medicaid (5.1% to 7.0% P < .01) as primary payers, which broadly reflect national trends in Medicare and Medicaid enrollment.40 Further studies are warranted to determine whether specific patient and hospital characteristics are associated with the increase in hospital charges demonstrated by the present study and to determine why charges are trending upward given unchanging LOS.
ACF and PCF
In the present study, more patients underwent ACF than PCF. However, there were increases in both procedures in the treatment of CSM. Prior studies have observed similar trends in surgical approaches.2,22,28 Broadly, we found the trends seen in all cervical fusions held true for ACF and PCF. The ACF and PCF cohorts grew older and presented with a greater comorbidity burden over time, while outcomes improved and charges increased.
Prior studies have argued which procedure, ACF or PCF, is more efficacious.7,8,41 Historically, younger, healthier patients with single-level disease are more likely to undergo ACF, while older patients with more comorbidities and multilevel disease are more likely to undergo PCF.42 The present study found that PCF patients had higher rates of in-hospital mortality and longer LOS compared to ACF patients. However, PCF patients were older and had a great comorbidity burden, on average.
Our data suggests worse outcomes associated with PCF may be related to patient demographics. This explanation is consistent with the findings of Jalai et al, who used NIS data from 2001 to 2010 to compare outcomes of 35 319 CSM patients who underwent cervical fusions by age. The authors found older patients had greater comorbidity risk, higher rates of complications, longer LOS, and greater odds of mortality, while charges for their procedures were greater.43 Similarly, Fehlings et al prospectively studied 278 CSM fusion patients from 12 sites in North America and concluded there was no significant difference in the efficacy of ACF or PCF after controlling for patient characteristics and disease severity.10 In the context of prior studies, our results suggest that updated studies comparing ACF to PCF in the management of CSM are warranted, as drawing direct comparisons between the two is out of the scope of this study.
Limitations
There are several limitations to be considered when interpreting the results of this study. First, due to the nature of the NIS, all of the collected data come from inpatients. There is no follow-up after discharge and only in-hospital outcomes can be included. Therefore, we were unable to measure several important outcomes following cervical fusion for CSM including long-term clinical outcomes. We were also unable to capture trends among patients undergoing outpatient surgery for CSM, which may underrepresent the anterior fusion data specifically. Finally, we were unable to report on trends in the diagnosis of CSM over the study period.
Next, the NIS uses ICD-9-CM codes that are assigned for all diagnoses and procedures. As such, information can be miscoded in or excluded from the NIS database. Quantity and quality of information in patient charts, communication between physician and patient, physician and coder experience, and coding errors can all lead to improper records or missing information.44 Finally, trends in population-based data cannot be attributed or applied to individual patients.
Despite these limitations, the NIS has frequently been used in studies of trends in spinal surgery.6,30,32,34,36–38,45 The database is well suited to the study of epidemiological health care trends, due to the diverse sampling of hospitals.32 Despite the redesign of the NIS in 2012, using the sampling weights included in the NIS allowed us to study trends from both before and after 2012. The NIS data allowed us to conduct a study in which trends in patient demographics, hospital characteristics, and outcomes in the surgical management of CSM could be examined in a comprehensive manner.
Conclusions
From 2003 to 2013, an increasing number of anterior and posterior cervical fusions were performed to treat CSM. Although patients undergoing these procedures were older and presented with a greater comorbidity burden over time, length of hospital stay remained constant and in-hospital mortality decreased. In contrast, hospital charges increased dramatically. These results can inform spine surgeons about the broad trends of the CSM patient population undergoing cervical fusion, as well as the associated hospital characteristics and surgical outcomes. Further studies are warranted to explain the observed trends and draw causative relationships in the surgical management of CSM.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by the following grants: T32 GM007250, TL1 RR024991, TL1 TR000441, 1F30HL132433-01A1.
References
- 1. Iyer A, Azad TD, Tharin S. Cervical spondylotic myelopathy. Clin Spine Surg. 2016;29:408–414. [DOI] [PubMed] [Google Scholar]
- 2. Wang MC, Kreuter W, Wolfla CE, Maiman DJ, Deyo RA. Trends and variations in cervical spine surgery in the United States: Medicare beneficiaries, 1992 to 2005. Spine (Phila Pa 1976). 2009;34:955–961. [DOI] [PubMed] [Google Scholar]
- 3. Lebl DR, Bono CM. Update on the diagnosis and management of cervical spondylotic myelopathy. J Am Acad Orthop Surg. 2015;23:648–660. [DOI] [PubMed] [Google Scholar]
- 4. Sheikh Taha AM, Shue J, Lebl D, Girardi F. Considerations for prophylactic surgery in asymptomatic severe cervical stenosis: review article. HSS J. 2015;11:31–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rao RD, Gourab K, David KS. Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am. 2006;88:1619–1640. [DOI] [PubMed] [Google Scholar]
- 6. Lad SP, Patil CG, Berta S, Santarelli JG, Ho C, Boakye M. National trends in spinal fusion for cervical spondylotic myelopathy. Surg Neurol. 2009;71:66–69. [DOI] [PubMed] [Google Scholar]
- 7. Alvin MD, Lubelski D, Benzel EC, Mroz TE. Ventral fusion versus dorsal fusion: determining the optimal treatment for cervical spondylotic myelopathy. Neurosurg Focus. 2013;35:E5. [DOI] [PubMed] [Google Scholar]
- 8. Ghogawala Z, Martin B, Benzel EC, et al. Comparative effectiveness of ventral vs dorsal surgery for cervical spondylotic myelopathy. Neurosurgery. 2011;68:622–630. [DOI] [PubMed] [Google Scholar]
- 9. Memtsoudis SG, Hughes A, Ma Y, Chiu YL, Sama AA, Girardi FP. Increased in-hospital complications after primary posterior versus primary anterior cervical fusion. Clin Orthop Relat Res. 2011;469:649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fehlings MG, Barry S, Kopjar B, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976). 2013;38:2247–2252. [DOI] [PubMed] [Google Scholar]
- 11. Cunningham MRA, Hershman S, Bendo J. Systematic review of cohort studies comparing surgical treatments for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2010;35:537–543. [DOI] [PubMed] [Google Scholar]
- 12. Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38(22 suppl 1):S173–S182. [DOI] [PubMed] [Google Scholar]
- 13. Sun Y, Li L, Zhao J, Gu R. Comparison between anterior approaches and posterior approaches for the treatment of multilevel cervical spondylotic myelopathy: a meta-analysis. Clin Neurol Neurosurg. 2015;134:28–36. [DOI] [PubMed] [Google Scholar]
- 14. Tannous O, Jazini E, Ludwig SC. Anterior surgical treatment for cervical spondylotic myelopathy. Semin Spine Surg. 2014;26:73–80. [Google Scholar]
- 15. Woods BI, Hohl J, Lee J, Donaldson W, Kang J. Laminoplasty versus laminectomy and fusion for multilevel cervical spondylotic myelopathy. Clin Orthop Relat Res. 2011;469:688–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu Y, Hou Y, Yang L, et al. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2012;37:E1450–E1458. [DOI] [PubMed] [Google Scholar]
- 17. Hirai T, Okawa A, Arai Y, et al. Middle-term results of a prospective comparative study of anterior decompression with fusion and posterior decompression with laminoplasty for the treatment of cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2011;36:1940–1947. [DOI] [PubMed] [Google Scholar]
- 18. Luo J, Cao K, Huang S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J. 2015;24:1621–1630. [DOI] [PubMed] [Google Scholar]
- 19. Mummaneni PV, Kaiser MG, Matz PG, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:130–41. [DOI] [PubMed] [Google Scholar]
- 20. Liu JM, Peng HW, Liu ZL, Long XH, Yu YQ, Huang SH. Hybrid decompression technique versus anterior cervical corpectomy and fusion for treating multilevel cervical spondylotic myelopathy: which one is better? World Neurosurg. 2015;84:2022–2029. [DOI] [PubMed] [Google Scholar]
- 21. Shamji MF, Massicotte EM, Traynelis VC, Norvell DC, Hermsmeyer JT, Fehlings MG. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38(22 suppl 1):S195–S209. [DOI] [PubMed] [Google Scholar]
- 22. Veeravagu A, Connolly ID, Lamsam L, et al. Surgical outcomes of cervical spondylotic myelopathy: an analysis of a national, administrative, longitudinal database. Neurosurg Focus. 2016;40:E11. [DOI] [PubMed] [Google Scholar]
- 23. Whitmore RG, Schwartz JS, Simmons S, Stein SC, Ghogawala Z. Performing a cost analysis in spine outcomes research. Neurosurgery. 2012;70:860–867. [DOI] [PubMed] [Google Scholar]
- 24. Lebl DR, Hughes A, Cammisa FP, Jr, O’Leary PF. Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J. 2011;7:170–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States (Current Population Reports) Washington, DC: US Census Bureau; 2014. [Google Scholar]
- 26. Mehrotra A, Forrest CB, Lin CY. Dropping the Baton: specialty referrals in the United States. Milbank Q. 2011;89:39–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tanenbaum JE, Lubelski D, Rosenbaum BP, Thompson NR, Benzel EC, Mroz TE. Predictors of outcomes and hospital charges following atlantoaxial fusion. Spine J. 2016;16:608–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Current trends in demographics, practice, and in-hospital outcomes in cervical spine surgery: a national database analysis between 2002 and 2011. Spine (Phila Pa 1976). 2014;39:476–481. [DOI] [PubMed] [Google Scholar]
- 29. US Bureau of the Census. Aging in the United States: Past, Present, and Future. Washington, DC: US Bureau of the Census; https://www.census.gov/population/international/files/97agewc.pdf. Accessed July 7, 2017. [Google Scholar]
- 30. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012;37:67–76. [DOI] [PubMed] [Google Scholar]
- 31. Davis H. Increasing rates of cervical and lumbar spine surgery in the United States, 1979-1990. Spine (Phila Pa 1976). 1994;19:1117–1123. [DOI] [PubMed] [Google Scholar]
- 32. Oglesby M, Fineberg SJ, Patel AA, Pelton MA, Singh K. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976). 2013;38:1226–1232. [DOI] [PubMed] [Google Scholar]
- 33. Omeis I, Demattia JA, Hillard VH, Murali R, Das K. History of instrumentation for stabilization of the subaxial cervical spine. Neurosurg Focus. 2004;16:E10. [DOI] [PubMed] [Google Scholar]
- 34. Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 2013;38:916–926. [DOI] [PubMed] [Google Scholar]
- 35. Alosh H, Riley LH, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality an examination of United States trends from 1992 to 2005. Spine (Phila Pa 1976). 2009;34:1956–1962. [DOI] [PubMed] [Google Scholar]
- 36. Marawar S, Girardi FP, Sama AA, et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976). 2010;35:1454–1459. [DOI] [PubMed] [Google Scholar]
- 37. Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–758. [PubMed] [Google Scholar]
- 38. Alosh H, Li D, Riley LH, Skolasky RL. Health care burden of anterior cervical spine surgery: national trends in hospital charges and length of stay, 2000-2009. J Spinal Disord Tech. 2015;28:5–11. [DOI] [PubMed] [Google Scholar]
- 39. Skolasky RL, Riley LH., 3rd Medicare charges and payments for cervical spine surgery: association with hospital characteristics. Spine (Phila Pa 1976). 2015;40:E936–E942. [DOI] [PubMed] [Google Scholar]
- 40. CMS.gov, Centers for Medicare & Medicaid Services. Medicare & Medicaid Statistical Supplement. 2013. Edition https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Archives/MMSS/2013.html. Published 2014. Accessed July 11, 2017.
- 41. Tanenbaum JE, Lubelski D, Rosenbaum BP, Benzel EC, Mroz TE. Propensity-matched analysis of outcomes and hospital charges for anterior versus posterior cervical fusion for cervical spondylotic myelopathy [published online June 27, 2016]. Clin Spine Surg. doi:10.1097/BSD.0000000000000402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009;9:31–38. [DOI] [PubMed] [Google Scholar]
- 43. Jalai CM, Worley N, Marascalchi BJ, et al. The impact of advanced age on peri-operative outcomes in the surgical treatment of cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2016;41:E139–E147. [DOI] [PubMed] [Google Scholar]
- 44. O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40:1620–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976). 2005;30:1441–1445. [DOI] [PubMed] [Google Scholar]


