Abstract
1. This article aims to provide a long-term update 2 years on from our initial paper and summarises service evaluation data collected from 21 pain management programmes, using a solution-focused approach in a community pain service.
2. An examination of the larger baseline and subsequent follow-up data suggests an improvement in participants’ function, pain self-efficacy and mental well-being following CPS PMP, and corroborates the findings of the earlier dataset.
3. Additional findings suggest that CPS PMP may help pain interfere less in participants’ lives (post-PMP and at 10-week follow-up) and that improvements in mental well-being and self-efficacy are maintained on a long-term basis (at 6- and 12-month follow-up). Limitations of the data are discussed.
4. The article also discusses the nature of community healthcare services for chronic pain, including how we view PMP treatment intensity, deliver cost effectiveness, measure outcomes and support patients post-PMP.
5. It is suggested that effective, meaningful PMPs can be facilitated successfully by multi-professional teams in the community, at arguably lower cost than secondary/tertiary settings, while enabling convenient and long-lasting integration of self-management into people’s lives.
Keywords: Pain management programme, solution focused, community pain management, pain self-efficacy, well-being, chronic pain, function, patient-centred care, cost effectiveness
Introduction
This article aims to open discussion around the nature of community healthcare services for chronic pain and includes reflection on issues that we feel are fundamental to the design and implementation of chronic pain services. This article focuses particularly on pain management programmes (PMPs), and discusses how we view PMP treatment intensity, deliver cost effectiveness, measure outcomes and support patients post-PMP.
As published longitudinal data from PMPs in multidisciplinary community settings appear scarce, this article also aims to provide a long-term update 2 years on from our initial paper.1 It summarises service evaluation data collected from 21 PMPs run by the community pain service (CPS) over 5 years.
Pain management in the community setting: overview of benefits and challenges
Community services play a major role in healthcare delivery. The NHS confederation2 reported that within the United Kingdom, community health services account for over 100 million patient contacts per year. Proportionately, this represents approximately 18% of NHS patient contacts, approximating to £9.75b, 10% of the overall NHS annual budget. The NHS confederation defines community services:
They provide a wide range of care, from supporting patients to manage long-term conditions, to treating those who are seriously ill with complex conditions … Teams of nurses and therapists coordinate care, working with professions including GPs and social care.3
The community setting has many benefits in line with current NHS principles, including timely care closer to home, convenient locations with easy access, closer third-sector links and partnership, and a demedicalised setting.4
As the Department of Health recognises chronic pain as a long-term condition, it would seem its management can fall well within the remit of community services as described above. This is consistent with the Faculty of Pain Medicine (FPM) who have published core standards for pain management services within the United Kingdom, with a specific chapter devoted to pain management services within the community5 (see Box 1).
Box 1.
Core standards for PMPs, FPM.5
| 1. There must be timely access to all forms of pain rehabilitation. 2. Standard and intensive PMPs must be available in a group format, but in some circumstances may be best provided on an individual basis. Consent must be obtained. 3. PMPs must be properly resourced with time, personnel and facilities. 4. Suitability for a PMP is based on the impact of pain, and there must be no discrimination on the basis of age, literacy, litigation or judgement of motivation. 5. A PMP must be delivered by an interdisciplinary team where some competencies are shared and some are unique to particular professions. 6. PMPs may be delivered in a primary, secondary or tertiary care settings; the required resources must be equally available in both settings. 7. The effective delivery of standard and intensive PMPs for complex participants must be undertaken by highly skilled staff, working as a team in adherence to the core principles. 8. Evaluation of outcomes must be standard practice. This should include assessing changes in function, psychological well-being, healthcare use, quality of life and work status where relevant. 9. Interventions to facilitate return to work should be viewed as an essential component of the work of PMP teams and be integrated with other treatment offered. 10. There must be co-operation between primary care, secondary care and local authorities to deliver effective, integrated services for people with chronic pain. This will include pain management and other treatments such as medicines and injections. 11. PMPs must aim for high-quality leadership and effective team working. 12. PMP staff must have adequate time for training and continued professional development in the wider aspects of pain treatment. |
The number (and nature) of UK pain services located in community and secondary/tertiary settings has been challenging to report. In 2012, the National Pain Audit identified that in England, 136 pain clinics were based in acute trusts and 31 in community trusts. Their setting was not clear in 37 cases. The same report commented upon the staff/skill mix within services, finding that within Wales, 60% of clinics were multidisciplinary, whereas less than 40% of the English clinics were reported to meet the minimum multidisciplinary standard (the presence of a psychologist, physiotherapist and physician). The audit found that community clinics were especially difficult to identify and characterise as many provided treatment in a very different way to hospital care, with a greater emphasis on support to self-care.6
The challenge often faced in the design and delivery of community services is the apparent dichotomy between essential medicalisation to ensure diagnostic safety versus necessary demedicalisation to ensure optimal patient self-management. This line can be difficult. Equally, the recommended interface between health and social care sectors and third/volunteer sectors in practice provides a number of logistical and governance challenges, and there is currently little evidence to offer guidance on either, in pain settings.
PMPs in the community: quality and effectiveness
High-level evidence has repeatedly shown PMPs to improve physical functioning and coping, and to reduce distress and disability immediately post-PMP.7 It has also been shown in high-quality studies that structured self-management programmes can improve pain and disability.8 The British Pain Society (BPS) have commissioned the development of a directory of PMPs, the latest available version of which suggests that in 2013, there were around 97 PMPs in the United Kingdom.9 It is not possible to definitively identify from this resource how many of these programmes are community-based.
There has previously been considerable heterogeneity in PMPs; guidance from the BPS,10 and more latterly FPM,5 has aimed to define the nature of a PMP and also the core standards for delivery of quality care. This has given more clarity to how PMPs should operate, and how they should be benchmarked. However, much of the effectiveness data seem to be derived from specialist services based either in secondary or tertiary centres as there appear to be relatively few published studies evaluating multi-professional PMPs in the community,1,11 despite the more recent acknowledgement that the community is an appropriate setting for delivery of PMP.5
Providing a CPS PMP in practice: the Southport and Formby model
The NHS 5 Year Forward View4 advises action on three fronts: demand, efficiency and funding. With this in mind, the CPS has worked to try to meet the needs of the local population (some of whom would not wish to or be able to travel to tertiary services for PMP), by embedding a PMP into the service.
The PMP aims to be highly patient-centred and to empower and actively engage patients, remembering that ‘patients are arguably the greatest untapped resource within the NHS’.12 This active, community-based engagement of patients is a common thread through all the recent 10 priorities outlined by the Kings Fund in the ‘Transforming Our Health Care System’ 2015 update13 and a key part of the NHS 5 Year Forward View,4 and of sustainability and transformation planning. One way the CPS and PMP aims to be highly patient-focused is by taking a solution-focused (SF) approach14 to biopsychosocial aspects of pain management. An SF approach advocates working with the person rather than the problem, listening to and working with patient priorities, hopes and expertise to develop meaningful goals, noticing exceptions to problems and noticing smallest signs of success (as defined by the person). It also encourages clinicians and services to take a whole person perspective to the integration of physical and mental healthcare, another of the Kings Fund 10 priorities.
A full description of the delivery of the CPS PMP can be found in our original article.1
Brief overview of PMP practicalities
The community PMP comprises 5 hours of group work per week (over three sessions) for 8 weeks, that is, 40 hours, with a 2-hour follow-up group session 10 weeks later. The PMP is run as part of the wider work of the CPS. Each week there are 2, hour long PMP exercise (circuit-based) sessions run by a specialist pain physiotherapist with skills in psychological approaches, 2 of which are introductory hydrotherapy sessions. The remaining weekly PMP session is discursive, is 3 hours in duration and is divided into 3 part-sessions with breaks between. Each part-session is facilitated by a different clinician, who is timetabled to leave their outpatient clinic to facilitate, and then will return to clinic on the same site afterwards. This enables effective utilisation of clinician time.
Assessment
The community PMP offers an introductory morning to PMP, where prospective attendees learn more about the programme and meet the others they will likely work with throughout. This includes fellow attendees and clinicians, as well as ‘experts by experience’, that is, recent PMP ‘graduates’, promoting a pooling of expertise. It gives an opportunity for deeper understanding of PMP, and from the clinical perspective, a chance to ensure medical, physical and psychological safety. Providing there are no safety concerns, we do not preclude access to the PMP, and also accept people with a range of co-morbidities. Significantly, assessment/screening focuses predominantly on curiosity around the person’s ‘best hopes’ for themselves if the programme was useful to them in their life, and ensuring that these are a good fit, in general terms, with the aims of the programme. This contrasts with other assessment approaches which often focus more on the measurement of level of distress/disability.
Goal setting is common to many PMPs and not a new concept. Assessment and goal setting using a SF approach, however,
allows the expertise and experience of the client to become a central tool in this process, as client and therapist collaborate on identifying a detailed picture of desired change … bringing together the client’s knowledge of their own life, with the therapists understanding <of pain management> … An added bonus is that the client may experience an immediate therapeutic benefit … positive change can occur at any time as a result of any part of a solution focused conversation.15
Participation in PMP is thus framed as something more meaningful for the participant beyond clinical goals.
Motivation to continually attend the 8-week programme is generally high, and mean drop-out rate is less than 20%. Given that PMP is embedded in the wider work of the CPS, this allows for a smooth transition from and to one-to-one work with clinicians, should this be required.
Outcome measurement
Patient-reported outcome measures (PROMs) are increasingly utilised to demonstrate treatment efficacy. Validated tools can be advantageous, especially when comparing different treatment approaches, using the same measure. They do, however, generally measure what the researcher, rather than the patient, wants to measure, and there is evidence to suggest that there can be substantial gaps between what patients value and what researchers prioritise.16 Arguably, truly individualised care would be measured by individualised measurements. For example, the most important and meaningful goals may be being able to walk the dog, and feeling like a good grandparent, the potentially random combination of which do not feature frequently in validated measures. The dichotomy of being able to robustly compare treatments or groups, but offer individualised measurements is not easily reconciled.
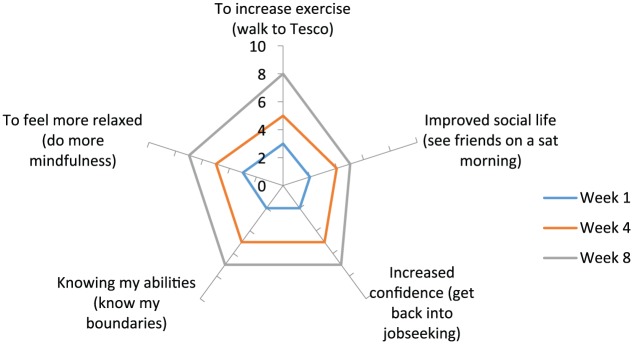
The development of an individualised measurement tool (‘iGro’, see Figure 1) came from this need to individualise measurement, and from our curiosity about working with patients’ hopes and priorities. In its evolved state, it also has become a (national innovations award winning) therapeutic tool used on our PMP, in addition to more typical standardised measures. It combines the SF principles of scaling (for a general account, see Ratner et al.;17 for more specific ideas on using SF scaling in pain settings, see Bray et al.18) with a user defined five-point star-shaped visual analogue scale (VAS). Each ‘arm’ of the star is represented by a 0–10 scale, and defined by the user (e.g. feeling like a good mother or the ability to stand and cook), and joins at the central point (zero). Rather than measure intrusive negative symptoms (e.g. poor sleep), each VAS measures positively construed goals, and success is measured at the start, mid-point and end of the PMP. Using SF scaling principles and conversation, the user is encouraged to think for each VAS how things would look differently, for example, ‘if you were at 4, ie a little higher than your 3 now – what would you notice?’, as well as notice in detail what is helping them, for example, to be a 3, and not lower down their scale. For most patients, the rated area often ‘grows’ at each time point, representing a growth in ‘living well’.
Figure 1.
Real-world example of completed ‘iGro’ (individualised measurement tool).
Such individualised tools may be difficult to cross-validate with other measures; however, large numbers of user datasets could perhaps help to explore whether a specific type of approach (e.g. SF based PMP) can help users achieve their own meaningful goals rather than the ones chosen for them from previously validated tools. We hope to explore and present this tool and dataset in a future paper.
Post-PMP patient support
The Kings Fund13 highlights 10 priorities for commissioners, recommending that ‘at the heart of the chronic disease management model … is the informed, empowered patient with access to continuous self-management support’. A community-based PMP and pain service can offer some advantages in this respect; a local knowledge of therapeutic support and volunteer and third-sector networks, affiliated groups and employment or volunteering facilitation; and is well situated ‘to reach out into communities more effectively … and harness the power of the wider community’.19
The community PMP has experience in ‘growing’ local volunteers, who have graduated PMP, or attended the community clinic. An SF framework has helped with identifying and recognising people’s skills, and in many cases noticing their hope to ‘give something back’ (a common theme for people we have worked with, which can be therapeutically utilised to help people develop their sense of purpose and meaning in their lives). In our experience, nuturing and supporting volunteers, liasing with the trust to develop an appropriate training package relevant to the role, providing a governance framework and ultimately supporting volunteers to develop self-sustaining therapeutic groups have been a worthwhile investment of our time. As well as a thriving patient support group (Pain Clinic Plus),20 examples associated with the CPS and PMP also include a chair-based exercise class, an arts and crafts group, a fortnightly ‘graduate’ PMP group and a pain service choir21 (NB service evaluation data from the choir has suggested clinically and statistically significant improvements in mental well-being22).Clinicians are able to signpost patients to these activities (when in line with the person’s ‘best hopes’), and they provide long-standing resource networks at minimal NHS cost.
Costs per 8-week community-based PMP
A breakdown of the PMP clinicians and their time dedicated to PMP are outlined in Table 1, giving an overview of the multidisciplinary input. Costs are outlined in Table 2 and are based on the 8-week programme (3 sessions per week, 5 hour treatment time per week). The programme is run from a community NHS location (health and well-being centre) utilised by the NHS trust for delivery of clinical services. The CPS is based within this centre where, in addition to PMP, it delivers outpatient and volunteer-led services. There is an arrangement where PMP patients are able to utilise the hospital hydrotherapy pool for two physio-led taster sessions, as (at the time of writing) the service is currently part of a hospital trust. Patients can then use the pool on a pay-as-you-go, ongoing basis during public sessions. As a point of reference, attending a 16- or 5-day PMP privately in a tertiary setting in 2015 costs per person £14,963 and £6905, respectively.23
Table 1.
Total clinician time devoted to 8-week community PMP (including clinician admin time).
| Clinician | Hours |
|---|---|
| Physician | 10 |
| Clinical psychologist (band 8aa) | 15 |
| Occupational therapist (band 6a) | 25 |
| Physiotherapist (band 7a) | 42 |
| Assistant psychologist (band 5a) | 35 |
| Total hours | 127 |
PMP: pain management programme.
Refers to UK Agenda for Change pay banding structure.
Table 2.
Estimated costs of 8-week community PMP.
| Estimated clinician cost (based on staffing, mid-point scale, no on-costs, see Table 1) | £2370 |
| Room cost £15 × 50 hours | £750 |
| Estimated administrative costs (5 hours per week) = 40 hours Band 3 | £450 |
| Sundries | £50 |
| Total | £3620 |
| Cost per patient (if 10 participants) | £362 |
PMP: pain management programme.
Community PMP service evaluation data summary
In 2014, we reported service evaluation data collected over 3 years (n = 85) from an NHS CPS PMP in Ainsdale, Southport.1 As published longitudinal data from PMPs in community multi-disciplinary settings appear scarce, we wanted to provide an update 2 years on from our initial paper, exploring and summarising extended service evaluation data collected from 21 PMPs, spanning over 5 years (n = 143).
Data gathered from 104 females and 39 males who had attended at least 75% of the 3 × 8 PMP sessions were included in the present analysis. These components are considered as core aspects of the PMP. Patients were diagnosed with a variety of chronic pain conditions (NB multi-morbidities were not excluded) and ages ranged from 25 to 83 years (mean = 52 years).
Methodology (data collection and analysis) relating to the extended PMP data was repeated as per our initial paper,1 which the reader is referred to if a full description is required. Data were collected from the following outcome measures (Table 3): Pain Self-Efficacy Questionnaire (PSEQ),24 Warwick–Edinburgh Mental Well-being Scale (WEMWBS),25 Brief Pain Inventory (BPI)26 and sit-to-stand test (STST).27Properties of the measures and scoring interpretations (including clinical significance indicators) are described in our initial evaluation paper. The dataset comprised data from our first PMPs (May 2010 onwards, documented in Simm, Iddon and Barker, 20141), plus additional data collected from subsequent programmes (21 programmes in total). The ongoing service evaluation was registered with Southport and Ormskirk Hospital NHS Trust Audit and Effectiveness Department (Ref: 12-314).
Table 3.
May 2010–August 2015: mean changes in self-efficacy, mental well-being, function and worst and average pain and pain interference from baseline (pre-PMP) to consecutive follow-ups.
| N | Pre-PMP Mean (SD) |
Post-PMP Mean (SD) |
p-value | |
|---|---|---|---|---|
| PSEQ (0–60) | ||||
| Post | 143 | 20.6 (10.7) | 29.8 (11.6)*** | <.001** |
| 10 weeks | 96 | 20.6 (10.3) | 28.6 (11.7) | <.001** |
| 6 months | 71 | 22.6 (10.8) | 25.8 (12.9) | .010* |
| 12 months | 49 | 22.2 (10.0) | 27.7 (13.7) | .002* |
| WEMWBS (14–70) | ||||
| Post | 121 | 35.2 (9.7) | 44.0 (10.1)*** | <.001** |
| 10 weeks | 78 | 35.5 (10.4) | 43.5 (10.5)*** | <.001** |
| 6 months | 62 | 36.8 (9.9) | 40.7 (11.4)*** | .001** |
| 12 months | 39 | 36.9 (11.7) | 41.8 (12.5)*** | <.001** |
| BPI worst pain (0–10) | ||||
| Post | 90 | 7.6 (1.8) | 7.6 (1.6) | .735 |
| 10 weeks | 59 | 7.5 (1.8) | 7.3 (1.7) | .469 |
| 6 months | 43 | 7.4 (2.0) | 7.6 (1.6) | .643 |
| 12 months | 21 | 6.6 (2.3) | 7.8 (1.2) | .055 |
| BPI average pain (0–10) | ||||
| Post | 90 | 6.6 (1.5) | 6.5 (1.5) | .342 |
| 10 weeks | 59 | 6.5 (1.6) | 6.5 (1.6) | .826 |
| 6 months | 43 | 6.3 (1.7) | 6.3 (1.4) | .832 |
| 12 months | 21 | 5.9 (2.1) | 6.3 (1.2) | .242 |
| BPI interference (0–10) | ||||
| Post | 89 | 7.2 (1.9) | 6.7 (1.9) | .027* |
| 10 weeks | 57 | 7.3 (1.8) | 6.6 (2.0) | .004* |
| 6 months | 40 | 6.7 (2.1) | 7.1 (1.9) | .380 |
| 12 months | 19 | 7.0 (1.9) | 7.5 (1.6) | .389 |
| STST | ||||
| Post | 98 | 9.2 (6.6) | 12.5 (5.6) | <.001** |
PMP: pain management programme; PSEQ: Pain Self-Efficacy Questionnaire; WEMWBS: Warwick–Edinburgh Mental Well-being Scale; BPI: Brief Pain Inventory; STST: sit-to-stand test; MCID: minimal important clinical difference.
Significant at .05; **significant at .001; ***MCID met.
As in our original service evaluation, statistically significant differences were found for self-efficacy immediately post-PMP (as well as clinically significant meaningful change at this time point) and 10-week follow-up. In addition, the larger dataset suggests that the improvement in self-efficacy is now statistically significant at the later time points of 6 and 12 months.
Again, as per the initial evaluation, statistically and clinically significant differences were found for mental well-being at all follow-up points post-PMP. In terms of mental well-being, with the larger dataset, these changes are now significant at the p < .001 level (previously p < .05).
As per the initial evaluation, statistically significant change was found for function at post-PMP (later time points not measured due to time constraints at follow-up group and postal return methods used at 6 and 12 months).
The initial evaluation did not show any statistically significant change on the BPI. The larger dataset, however, now shows a statistically significant difference (p < .05) on the Interference subscale post-PMP and at 10-week follow-up.
N values vary between the measures for several reasons. The WEMWBS, BPI and STST were introduced at later time points than the PSEQ, which was part of the evaluation process for the very first PMPs delivered. Also, despite best efforts, in clinical practice, not all items on the questionnaires are completed fully by every patient. There was also attrition in terms of response rates over time. Only patients who provided complete pre- and post-PMP datasets (and subsequent 10-week, 6- and 12-month follow-up data, where available) were included in the analysis.
Discussion
PMP service evaluation data
With reference to the current analysis of the extended dataset (from 21 PMPs over 5 years), an examination of baseline and subsequent follow-up data suggests that the PMP continues to improve function, pain self-efficacy and mental well-being. Findings also now suggest that the PMP helps pain interfere less in patients’ lives both immediately post-PMP and at 10-week follow-up after that (which is perhaps particularly important given the Cochrane Review7 of psychological therapies for the management of chronic pain found no effect on pain). Patients rated less interference from pain, despite showing no statistically significant difference in average and worst pain ratings.
The extended dataset suggests that improvements in mental well-being and now self-efficacy have been found to be maintained on a long-term basis, and the statistically significant findings above are supplemented by clinical significance. The findings remain in line with the primary aims of the CPS PMP, that is, to improve well-being and coping despite the presence of pain, and suggest that a locally delivered SF community approach to PMP has had a positive, sustained impact on patients with chronic pain. In line with the CPS PMP approach, recent research28 has found that greater levels of positive goal engagement (comprising factors based on goal-focused hope and principles underpinning the SF approach) predict higher levels of psychological well-being, and partially mediate the relationships between both pain severity and its impact on function and psychological well-being. This suggests that there may be a protective ‘buffering’ effect of the presence of positive goal engagement in enabling individuals with chronic pain to maintain a sense of psychological well-being, while accounting for effects of the intensity and impact of the pain itself.
There are, however, some significant limitations to the CPS community PMP dataset and analysis which impact the strength of the conclusions that can be drawn, and the comparisons that can be made. However, given the general paucity of data and information regarding the delivery of PMPs in the community, combined with the growth of such commissioned services, it was felt the findings were relevant to the public domain.
The data are gathered in a ‘real-world’ clinical service, as part of a service evaluation, with no control group. It shows attrition in terms of number of participants at the follow-up time points. This is because not all patients choose to attend the 10-week follow-up group, where questionnaire data are usually collected. The 6- and 12-month data are collected by return postal questionnaire rather than in person, and it is well understood that this more distant approach can often unfavourably affect response rates. Arguably, therefore, the long-term data are skewed as it reflects only those patients who chose to respond (non-response bias). Intent-to-treat analyses of missing data were not conducted and data were analysed from small numbers of participants at some data points. The evaluation also did not control for social desirability bias, as the clinicians who delivered the programme also collected and analysed the data. These factors may reduce internal and external validity.
Relevance of findings to treatment intensity and patient need
This service evaluation data tentatively suggest that a relatively low cost, accessible, 40 hour, community-based PMP has made a significant, meaningful difference to the lives of people who live with chronic pain. In terms of the recommended guidance and evidence around commissioning PMPs, a previous Cochrane Review29 for the treatment of chronic low back pain has recommended utilising only multi-professional rehabilitation treatment of longer duration (>100 hours), although the review has now been updated with no such recommendation regarding duration or intensity. More recently, the BPS and FPM advise that for commissioning purposes, a standard PMP should be a minimum of 12, three-hour sessions (i.e. 36 hours), with more intensive programmes (e.g. 15–20 full days) offered to some very disabled and distressed patients. There is, however, no recognised standard in how to optimally agree both treatment intensity and type of psychological approach. Furthermore, our understanding is that there currently are few standardised tools (if any) that can accurately predict ‘good’ PMP outcome. Pre-PMP assessment clinics can be seen as a way to better understand an individual’s therapeutic need and wishes prior to participating on a PMP. The FPM core standards for PMPs5 state that ‘suitability for a PMP is based on the impact of pain, and there must be no discrimination on the basis of age, literacy, litigation or judgement of motivation’. It is arguable that a true needs-based assessment should also not be dependent on psychometric cut-off points, or isolated clinical opinion, but on an individualised, shared understanding of need, ‘best hopes’ and meaningful goals between individual and clinician. This would also help define what a ‘good’ outcome would look like for the individual.
This collaborative needs-based assessment is perhaps one of the greater challenges. Our anecdotal experience has found individuals with severe distress and/or disability can make meaningful change in living well with their pain if we measure meaningful outcomes for the individual. This generates uncertainty around the concept of those with severe distress and disability requiring high-intensity treatment, and may be a reflection of trying to advance and measure clinician-focused goals.
Understanding these issues is especially relevant to how we commission effective, cost efficient, patient-centred treatments. It may be that some of those patients traditionally thought of as ‘complex’, may be managed effectively with ‘lower’ intensity PMP (e.g. 3 MDT sessions per week for 8 weeks) and supported self-management, in a resource-hungry NHS.
Living well post-PMP: utilisation of the community setting to promote long-lasting change
After complex interventions such as coronary artery bypass grafting, the NHS rightly invests in secondary prevention. It is arguable that PMP is similarly a scarce (and often life-changing) treatment and should therefore attract similar ‘post-treatment’ (and preventative) investment. Many clinicians who work within PMP will be familiar with the trepidation that often accompanies PMP graduation. This may particularly be a feature of ‘immersion’ type courses, especially those where long distances between PMP and home are present, and with little knowledge from the clinician’s perspective of what the person will be going home to. It is our experience that a locally based, low intensity (3 sessions per week), longer duration (8 weeks) programme enables participants to progressively interweave PMP principles into their day-to-day life. Additionally, the camaraderie and sense of group identity often results in long-term peer support; both of which seem to help minimise post-PMP graduation concern and sustain long-term change.
Despite challenges, our experience is that an extended volunteer support system, although requiring some supervision and management, reduces the load on clinical services. It also provides an ‘experts by experience’ resource that some returning patients can be redirected to when they perhaps need ‘clinician-light’ support to reignite good habits around pain management and well-being. Participants in many of our groups frequently reference the power and support of being part of a peer group as a protective and helpful factor in their lives.21,30 Evidence suggests that a strong sense of social identity can positively influence mood in community and clinical settings.31 Exploring resource minimal ways that this can keep happening would appear to be another useful strategy a community-based pain service can employ to support people to live well in the long term with pain.
We stand on the cusp of a revolution in the role that patients – and also communities – will play in their own health and care. Harnessing what I’ve called this renewable energy is potentially the make it or break-it difference between the NHS being sustainable or not. 32
Simon Stevens, Chief Executive, NHS England
Our vision is to build on this success and further develop the CPS and PMP. We hope to
Further utilise the benefits of community and expert patient networks;
Develop patient-centred pathways with other healthcare providers;
Deliver early intervention and awareness projects;
Explore newer return to work initiatives;
Build more meaningful links with social care and return to work services
Acknowledgments
With thanks to the CPS PMP team for all the hard work, and to our patients and expert patients, from whom we learn so much. Thanks also to Dr Suzi Curtis and Dr Joanne Iddon.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Simm R, Iddon J, Barker C. A community pain service solution-focused pain management programme: delivery and preliminary outcome data. Br J Pain 2014; 8: 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NHS Confederation. What are community health services? http://www.nhsconfed.org/~/media/Confederation/Files/public%20access/guide_community_services.pdf (2016, accessed October 2016).
- 3. NHS Confederation. What are community health services? http://www.nhsconfed.org/resources/2015/07/what-are-community-health-services (2015, accessed October 2016).
- 4. National Health Service (NHS). NHS 5 year forward view, https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (2014, accessed October 2016).
- 5. Faculty of Pain Medicine (FPM). Core standards for pain management services in the UK, http://www.rcoa.ac.uk/system/files/CSPMS-UK-2015-v2-white.pdf (2015, accessed October 2016).
- 6. British Pain Society. National pain audit 2010–2012: final report. British Pain Society, https://www.britishpainsociety.org/static/uploads/resources/files/members_articles_npa_2012_1.pdf (2012, accessed 29 September 2017). [Google Scholar]
- 7. Williams ACDC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev 2012; 15: CD007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Du S, Yuan C, Xiao X, et al. Self-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Patient Educ Couns 2011; 85(3): e299–e310. [DOI] [PubMed] [Google Scholar]
- 9. British Pain Society. National directory of services for PMPs 2013. British Pain Society, Pain Management Programmes Special Interest Group, https://www.britishpainsociety.org/static/uploads/resources/files/pmp_sig_directory.pdf (2013, accessed 29 September 2017). [Google Scholar]
- 10. British Pain Society. Guidelines for pain management programmes for adults. London: The British Pain Society, 2013. [Google Scholar]
- 11. Wong M, Rietzschel J, Mulherin D, et al. Evaluation of a multidisciplinary outpatient pain management programme based at a community hospital. Musculoskeletal Care 2009; 7(2): 106–120. [DOI] [PubMed] [Google Scholar]
- 12. Corrigan P. DIY doctors: patients boost NHS’s value. Health Serv J 2009; 119(6154): 12–13. [PubMed] [Google Scholar]
- 13. Kings Fund. Transforming our health care system, https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/10PrioritiesFinal2.pdf (2015, accessed October 2016).
- 14. Burns K. Focus on solutions: a health professional’s guide. Revised 2nd edn London: Solutions Books, 2016. [Google Scholar]
- 15. Duncan L, Mousley S, Ghul R. The solution focused measure of occupational function. In: Duncan L, Ghul R, Mousley S. (eds) Creating positive futures: solution focused recovery from mental distress. London: BT Press, 2007, pp.43–85. [Google Scholar]
- 16. Cowan K. The James Lind alliance: tackling treatment uncertainties together. J Ambul Care Manage 2010; 33(3): 241–248. [DOI] [PubMed] [Google Scholar]
- 17. Ratner H, George E, Iveson C. Solution focused brief therapy: 100 key points and techniques. London: Routledge, 2012. [Google Scholar]
- 18. Bray D, Groves K, Lathom J, et al. ‘First, do no harm’: a solution focused approach to pain measurement and management. Eur J Palliat Care 2015; 22(4): 190–193. [Google Scholar]
- 19. Kings Fund. Community services: how they can transform care, https://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/community-services-nigel-edwards-feb14.pdf (2014, accessed October 2016).
- 20. Pain Clinic Plus. http://painclinicplus.org.uk (accessed 23 November 2017).
- 21. Hopper M, Curtis S, Hodge S, et al. A qualitative study exploring the effects of attending a community pain service choir on wellbeing in people who experience chronic pain. Br J Pain 2016; 10(3): 124–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Simm R. Community pain service: ‘Good Vibrations’ choir evaluation (April-July 2013). NHS service evaluation report, 2013, pp.1–6. [Google Scholar]
- 23. The Walton Centre NHS Foundation Trust. Private patient tariff. The Walton Centre NHS Foundation Trust, https://www.thewaltoncentre.nhs.uk/uploadedfiles/FOI/Private%20Patient%20tariff%20for%20201415.pdf (2015, accessed 20 September 2017). [Google Scholar]
- 24. Nicholas MK. Self-efficacy and chronic pain. In: Annual conference of the British Psychological Society, St. Andrews, 4 April 1989. [Google Scholar]
- 25. Tennant R, Hiller L, Fishwick R, et al. The Warwick–Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007; 5: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994; 23(2): 129–138. [PubMed] [Google Scholar]
- 27. Bohannon RW. Sit-to-stand test for measuring performance of lower-extremity muscles. Percept Mot Skills 1995; 80(1): 163–166. [DOI] [PubMed] [Google Scholar]
- 28. Iddon J. The role of positive goal engagement in increased psychological well-being amongst individuals with chronic non-cancer pain. DClinPsy Thesis, University of Liverpool, 2016, https://livrepository.liverpool.ac.uk/3003728/ [Google Scholar]
- 29. Guzmán J, Esmail R, Karjalainen K, et al. Multidisciplinary bio-psycho-social rehabilitation for chronic low back pain. Cochrane Database Syst Rev 2002; 1: CD000963. [DOI] [PubMed] [Google Scholar]
- 30. Dargan P, Simm R, Murray C. New approaches towards chronic pain: patient experiences of a solution-focused pain management programme. Brit J of Pain 2013; 8(1); 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cruwys T, Haslam S, Dingle G, et al. Feeling connected again: Interventions that increase social identification reduce depression symptoms in community and clinical settings. J Affect Dis 2014; 20(159): 139–146. [DOI] [PubMed] [Google Scholar]
- 32. NHS England. Personalised care and support planning handbook: the journey to person-centred care. NHS England, Coalition for Collaborative Care, https://www.nhs.uk/NHSEngland/keogh-review/Documents/pers-care-guid-core-guids.pdf (2015, accessed 20 January 2016). [Google Scholar]