Abstract
OBJECTIVES:
The objectives of this study are to estimate the prevalence of self-medication with antibiotics in King Khalid University Hospital population and evaluate the factors affecting this behavior.
MATERIALS AND METHODS:
This was a cross-sectional study conducted at King Khalid university hospital from April to May 2016. A pretested self-administered questionnaire was handed to a random selection of 519 patients attending the primary care clinics . Data were entered into Microsoft Office Excel 2007 and sent to SPSS version 20 for analysis. Descriptive statistics and logistic regression were applied.
RESULTS:
The prevalence rate of self-medication with antibiotics was 40.8%. Older patients and males were most likely to use antibiotics without a prescription. The most common illnesses that made patients use antibiotics was upper respiratory tract infections (73.2%). Commercial pharmacies were the major source 82.8%. Only 27.8% patients consulted their physicians for the correct dosage . The previous experience with a similar illness (67.2%) and difficulty in obtaining medical help (29.3%) were the most common reasons for self-administration of antibiotics. Improved health condition (57.8%) was the main reason for stopping the use of antibiotics while lack of improvement in health status led to a shift to another antibiotic in 62.5% of the respondents.
CONCLUSION:
The prevalence of using antibiotics without a prescription is relatively high. Proper education of the public on the dangers of the misuse of antibiotics through the media might help to reduce this practice.
Keywords: Antibiotic, prescription, primary care, self-medication
Introduction
Antibiotics are used to save the lives of millions of people and are significant in the control of the spread of infectious diseases. However, the emergence of bacterial strains resistant to the available antibiotics is a major setback to achieving the required goal.[1,2] Studies have shown an increase in bacterial resistance to antibiotics for various reasons: excessive intake of antibiotics without medical advice, taking antibiotics for viral diseases, and the use of inappropriate treatment dosage.[3] Sometimes sick persons go to pharmacies directly without consulting their doctors. Pharmacists with little experience dispense inappropriate medications and often think that prescribing antibiotics might help the patient to heal faster or simply dispense the antibiotic for profit.[4]
Antibiotic misuse and the lack of its effectiveness have caused the emergence of strains of microbes' resistant to them, which is a problem for doctors and researchers.[5] Most infectious diseases are caused by two types of germs: bacteria or viruses. Antibiotics are for bacterial infections only and not for viral infections. Therefore, antibiotics do not help in treating viral infections and will not protect people from them[6] Some reasons for the increase in bacterial resistance to antibiotics are the prescription of antibiotics for viral infections, taking antibiotics without a prescription, pressure on the doctor for an antibiotic, nonadherence to the dosage, and course of the medication.[4]
Studies conducted in 19 European countries including Greece, Russia, Lithuania to estimate the prevalence of self-medication with antibiotics for the last 12 months.[7,8,9,10,11] showed that the prevalence was high in Southern and Eastern countries of Europe and low in the others. The most common reasons for self-medication with antibiotics were upper respiratory infections. The patients procured the medication from pharmacies or used previous prescriptions.[7] Trimethoprim-sulfamethoxazole was the most common medication found in the home medicine cabinet in Russia (46.3%).[10] In other studies, penicillin was at the top of medications used in self-management.[7,8,9,11] Young, educated, and patients who had chronic diseases were those that used antibiotics the most.[7] Rural folk who self-medicated with antibiotics were 1.79 times more than people in urban areas.[10]
The prevalence of self-medication was high in such developing countries as Iran, United Arab Emirates (UAE), Jordan, Sudan, Brazil, Tobago, and Trinidad.[12,13,14,15,16,17] It was the lowest in Tobago and Trinidad (34%), but highest in Sudan and Brazil (73.9%), (74%), respectively. The most common conditions for self-medication were upper respiratory diseases. The most common source was a previous prescription patients had at home followed by private pharmacies. Fifty-eight of the pharmacies in Brazil offered antibiotics to participants and this offer increased to 74% when participants insisted.[17] Penicillin groups were the most common types of antibiotics used in self-medication in the study. Participants from Tobago and Trinidad had a misconception that antibiotics would cure all infections (54%), that they had no side effects (61%). Self-medication with antibiotics was significantly different with sociodemographic variables. In Sudan and Tobago and Trinidad, a relationship was found between higher education and low socioeconomic state,[14,15] while in Jordan and UAE, the relationship was higher with high income and high education.[12,13]
Some studies conducted in Saudi Arabia on self-medication from 1988 to 2009 showed that patients tried self-medication to resolve their symptoms or to save time and money, 58%, 35.4%, respectively.[18,19] A study conducted in Riyadh showed the estimated rate of antibiotic prescriptions as approximately 44%.[20] Another study conducted in Asir region showed that 56.2% of the prescriptions issued-contained antibiotics.[21]
The focus of this study was to find out the extent to which participants living in Saudi Arabia used antibiotics without prescriptions. It was conducted to report on the rate and pattern of use of antibiotics without prescriptions, to assess subjects' knowledge of antibiotics and their attitudes toward their use without prescription and to identify the factors relating to the use of antibiotics without prescription.
Materials and Methods
A cross-sectional study was conducted in the primary health care (PHC) of King Khalid University Hospital (KKUH) in April and May 2016. The participants were faculty members, hospital staff, eligible patients, and their families, who attended the primary care clinics.
The target population of the present study was adult patients (≥18 years) attending PHC of KKUH, Riyadh, Saudi Arabia There was no exclusion criterion.
The estimate of the sample size was based on the average rate of self-medication of 45% based on the rates reported from UAE, Jordan, Sudan, and Iran, ranging from 39.5% to 53%.[12,13,14,16,22] with an acceptable degree of precision of 5% at the 95% level of confidence according to the following equation:
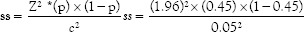
Based on the aforementioned assumption, the estimated minimum sample size was 380 participants. An additional 10% was considered to compensate for nonresponse resulting in a minimum sample size of 415 participants.
The questionnaire used in this study was based on a questionnaire used in a similar previous study.[23] The questionnaire was translated into Arabic, the native language of participants and validated by consultants in family and community medicine.
The questionnaire[23] consisted of 20 questions with open response options in three sections. First section addressed the pattern of self-medication including reasons for self-medication with an antibiotic, the health problem for which the antibiotic was sought, how the antibiotic was chosen, the source of antibiotic, duration of use, compliance with treatment, and whether the patient instruction in the pack of antibiotic was read. The second section included participant's knowledge of self-medication including the meaning of antibiotic and self-medication, indication for the use of antibiotics, associated health effects of self-medication, and the common side effects of antibiotics. The third section included a number of questions on sociodemographic data and the history of chronic health problems. A pilot study was conducted to test the questionnaire and the feasibility of data collection procedure.
The self-administered questionnaire was distributed to 519 patients selected randomly from those attending PHC of KKUH from April to May 2016. Trained medical students collected and checked the completeness of the data provided by participants and assisted illiterate participants to complete the questionnaire.
The Microsoft Office Excel 2007 was used for data entry and sent to SPSS Statistics (version 20.0) (IBM, Chicago, Illinois, USA) for data analysis. Frequency distribution and cross tabulation were done to check for outliers and data entry errors. Data were described using number, percentages. The univariate and multivariate logistic regression analyses were used to identify the predictors of the use of antibiotics without prescription. The significance of the obtained results was judged at the level of 5%.
Ethical approval was obtained from the Institutional Review Board. Participants were requested to sign an informed consent form which emphasized voluntary participation, the right to withdraw at any stage without any adverse consequences, as well as anonymity and confidentiality of the collected data.
Results
Most of the 519 participants were Saudi nationals (93.3%) and city dwellers (93.8%). Females made up 56.6% of the participants and more than one third of them were aged between 18 and <30 (37.6%) and 30 to <40 (32.2%). Smaller percentages were aged between 40 and <50 (17.5%) and 50 years and older (12.7%). In respect of education, only 3.1% had never been to school while 66.2% had a university or postgraduate degree. The remaining proportion had basic (7.9%) or high school (22.7%) education.
The majority of participants (90.2%) were aware of what is meant by an antibiotic. However, a substantial proportion of participants reported that it was used for the treatment of viral (53.4%) and parasitic (6.2%) infections among other illnesses (4.4%). Although 46.8% of the participants reported that it was used for bacterial infections, only 39.5% (n = 205) said that it was only for bacterial infections. Almost two-thirds of participants had some knowledge of the possible side effects associated with the use of antibiotics including nausea and vomiting (48.3%), diarrhea (35.5%) and rash (30.0%) [Table 1].
Table 1.
Knowledge of antibiotics and attitudes toward self-medication (n=519)
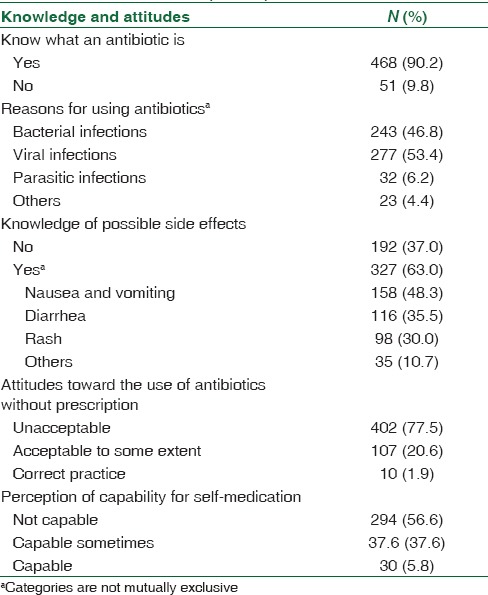
More than three-quarters of the participants (77.5%) acknowledged that the use of antibiotics without prescription was unacceptable and 56.6% did not think they were capable of self-medication [Table 1].
Of the participants, 93.4% (n = 485) said they used antibiotics and 40.8% (n = 198) reported using them without prescription. It was found that 39.9% had used antibiotics without prescription only once while 32.8% had used them three or more times (32.8%). The reported pattern of use [Table 2] shows that antibiotics were used without prescription mostly for respiratory illnesses (73.2%). The most common reason for doing this was what they knew or their previous experience (67.2%) and the difficulty of obtaining a prescription (29.3%). The choice of the antibiotic was governed by the participants' previous experience (60.1%) or the suggestion of a pharmacist (39.9%). Antibiotics used without prescription were mostly obtained from pharmacies (82.8%) and less frequently kept at home (24.2%).
Table 2.
Pattern of use of antibiotics without prescription (n=198)
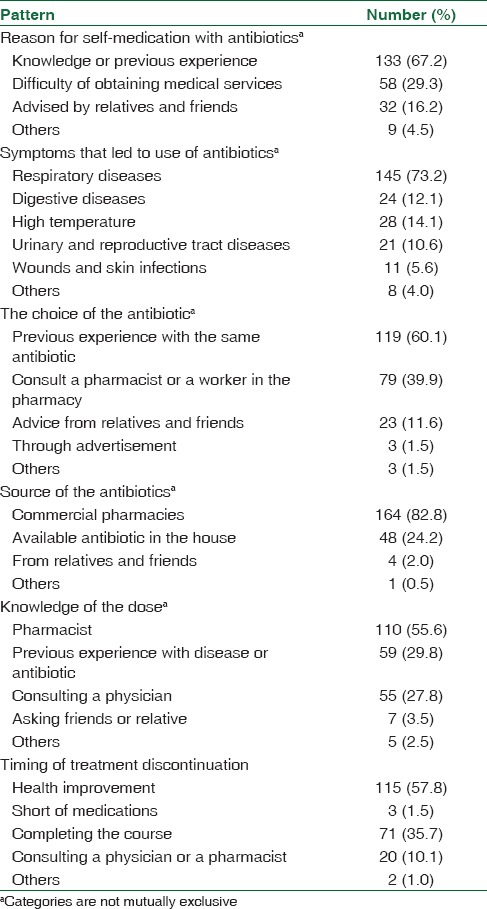
Before using the antibiotic, 83.3% (n = 165) of the participants claimed they read the patient information leaflet either always (64.8%; n = 107) or sometimes (35.2%; n = 58) and some of them, 67.2% (n = 111) said they had only a partial understanding of the drug information provided while 27.9% (n = 28) claimed that they understood the information fully. However, for 55.6% of the participants, the dosage of the antibiotics was determined by the pharmacist and for 29.8%), it was based on the user's experience with the disease or the type of the antibiotic. Less frequently, a physician was consulted (27.8%). Only 35.7% of the participants reported that they completed the full course of treatment before they discontinued its use while in 57.8% of the instances, they discontinued use when health improved [Table 2].
During the course of treatment, almost one-third of the participants modified the suggested dose (32.8%) or changed the antibiotic (31.8%). The cited reasons for modification of the dosage during the course of treatment, in order of frequency, were perceived improvement of health (40.3%), poor health status despite use (25.4%), avoidance of possible side effects of the drug (23.9%) and shortage of the drug (17.9%). Similarly, the cited reasons for the change of the antibiotic in order of frequency were poor health or lack of improvement in spite of use (62.5%), the need to reduce the side effects experienced (20.3%), shortage of the previously used antibiotic (17.2%), and the lower price of the new antibiotic.
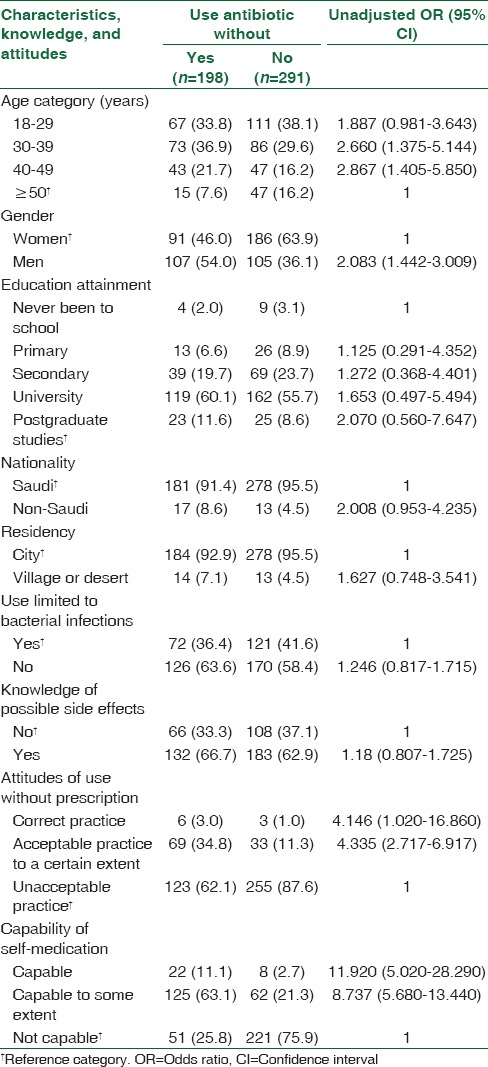
Men were twice as likely to use antibiotics without prescription than women (odds ratio [OR] = 2.083; 95% confidence interval [CI] = 1.442, 5.850) higher in those aged 30 to <40 years (OR = 2.660; 95% CI = 1.375, 5.144) in 40 to <50 years (OR = 2.867; 95% CI = 1.405, 5.850) in participants aged 50 years and older. A statistical significant risk was also observed in relation to participants' attitudes toward the use of antibiotics without prescription since it was used 4 times more by those who saw the practice as acceptable (OR = 4.146; 95% CI = 1.020, 16.860) or acceptable to a certain extent (OR = 4.335; 95% CI = 2.717, 6.917). Similarly, the risk of using antibiotics without prescription was significantly higher among participants who reported that they were capable of self-medication (OR = 11.920; 95% CI = 5.020, 28.290) or capable to a certain extent (OR = 8.737; 95% CI = 5.680, 13.440). On the other hand, no excess risk was observed in participants' nationality, area of residence, educational attainment, knowledge of the use of antibiotics for bacterial infections, and knowledge of the side effects [Table 3].
Table 3.
The use of antibiotics without prescription in relation to participants’ characteristics, knowledge, and attitudes among ever users of antibiotics
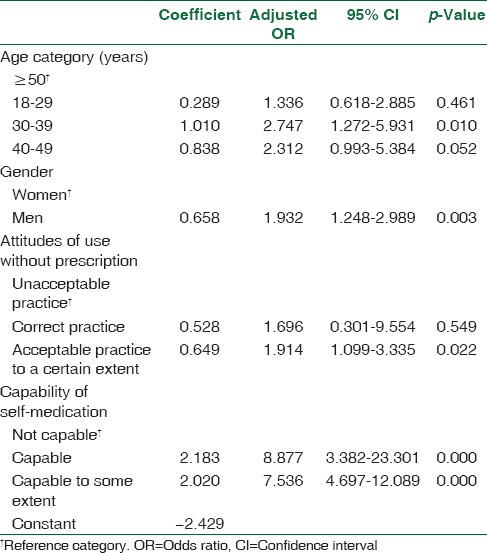
The full-model logistic regression analysis [Table 4] showed that the adjusted risk for the use of antibiotics without prescriptions was significantly higher in men than in women (ORA= 1.932, 95% CI = 1.248, 2.989); those aged 30 to <40 than those aged 50 years and older (ORA= 2.747, 95% CI = 1.272, 5.931); those who perceived the practice acceptable to a certain extent (ORA= 1.914, 95% CI = 1.099, 3.335); as well as those who said they were capable (ORA= 8.877, 95%CI = 3.382, 23.301) or capable to a certain extent (ORA= 7.536, 95% CI = 4.697, 12.089) of self-medication. These four variables correctly classify 64.6% users of 81.4% of nonusers of antibiotics without prescriptions (overall model sensitivity = 74.6%).
Table 4.
Full-model logistic regression analysis of the use of antibiotics without prescription among ever users of antibiotics
Discussion
Our study showed that the prevalence rate of self-medication with antibiotics was 40.8%, which is similar to the results of the two studies conducted in Jordan where the prevalence was 39.5% and 40.7%, respectively.[13,22] This is attributed to the fact that more than two-thirds of the participants were highly educated and had easy access to a university hospital. Our study, however, showed a low prevalence rate compared with other studies conducted in UAE and Sudan, at 56.3% and 73.9%, respectively.[12,14] Lower prevalence of self-medication with antibiotics was reported from Lithuania at 22% and from Turkey at 19.1%.[11,24]
In Sudan, women tended to use antibiotics without prescription more than men 53.0%[14] whereas in our study, it was men (54.1%) more than women (54. 9%). There was no association between gender and self-administration of antibiotics in the UAE.[12]
Age significantly affected the misuse of antibiotics. Participants aged 50 years and above-used antibiotics without prescription. The results UAE and Sudan are in support of this conclusion.[12,14]
The study showed a significant association between educational level and the use of antibiotics without prescription, the respondents with Bachelor's, Master's and PhD had more knowledge of what is meant by antibiotic, side effects and what they were used for. There was no statistical significance with the level of education as regards people who self-medicated, compared with other studies such as in the UAE and Sudan which showed significant difference[12,14]
The way to obtain antibiotics was significantly affected by nationality. Non-Saudis knew what antibiotic was and what they were used for more than Saudis. This is supported by the UAE study.[12]
The most common reason given for using antibiotics was upper respiratory tract infections followed by gastrointestinal diseases. This is supported by other studies conducted in Russia, Greece, and Tehran.[16] In addition, the same illnesses were the major cause of self-medication of antibiotics in the UAE, Sudan, and Jordan.[12,14,22]
The main sources of antibiotics as indicated by respondents in several studies also supported by our study were commercial pharmacies, antibiotics at home (mainly left-overs from previous illness), and on the advice of relative and friends.[12,13,22]
The majority were told of the dose by pharmacists, knew from previous experiences and were advised by relatives and friends. Nearly, a quarter of the study population, which was less than that of other studies as in Sudan and Jordan.[14,22] agreed that the best time to stop the use of antibiotics, was when the course was completed.
As long as there are no restrictions or regulations on the prescription of antibiotics, especially in developing countries, self-medication with antibiotics will continue, and thus impact on the development of antibiotic resistance.
The limitation of our study was that owing to restricted resources it was carried out in one center only. The PHC in KKUH is one of the major clinics in KKUH. The PHC services are the first level in the health-care system in KKUH and the Kingdom of Saudi Arabia. Most of the patients attending the hospitals have access to primary care besides the possibility of follow- up in other specialties or referral to specialty clinics. In addition, the characteristics of the participants who attend PHC in KKUH are similar to those who attend PHC affiliated to Ministry of Health. Consequently, the prevalence in a study conducted in specialty services or other centers might not be significantly different as factors such as education and social issues have a lot more impact on prescription.
Conclusion and Recommendations
The prevalence of using antibiotics without a prescription is relatively high. We believe that running education sessions for the public on the proper use and misuse of antibiotics with the help of the media might bring about a change in attitude.
The Ministry of Health and the General Directorate of Health Affairs could also play major roles in regulating the sale of antibiotics by pharmacies to reduce this phenomenon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kohanski MA, Dwyer DJ, Collins JJ. How antibiotics kill bacteria: From targets to networks. Nat Rev Microbiol. 2010;8:423–35. doi: 10.1038/nrmicro2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saengcharoen W, Lerkiatbundit S, Kaewmang K. Knowledge, attitudes, and behaviors regarding antibiotic use for upper respiratory tract infections: A survey of thai students. Southeast Asian J Trop Med Public Health. 2012;43:1233–44. [PubMed] [Google Scholar]
- 3.Levin BR. Minimizing potential resistance: A population dynamics view. Clin Infect Dis. 2001;33(Suppl 3):S161–9. doi: 10.1086/321843. [DOI] [PubMed] [Google Scholar]
- 4.Kotwani A, Wattal C, Katewa S, Joshi PC, Holloway K. Factors influencing primary care physicians to prescribe antibiotics in Delhi India. Fam Pract. 2010;27:684–90. doi: 10.1093/fampra/cmq059. [DOI] [PubMed] [Google Scholar]
- 5.Lindbaek M, Berild D, Straand J, Hjortdahl P. Influence of prescription patterns in general practice on anti-microbial resistance in Norway. Br J Gen Pract. 1999;49:436–40. [PMC free article] [PubMed] [Google Scholar]
- 6.Brown RB, Levin J, Morris A. Adverse effects of antibiotics. J Am Podiatr Med Assoc. 1989;79:500–4. doi: 10.7547/87507315-79-10-500. [DOI] [PubMed] [Google Scholar]
- 7.Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JG, Mechtler R, Deschepper R, Tambic-Andrasevic A, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12:452–9. doi: 10.3201/eid1203.050992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skliros E, Merkouris P, Papazafiropoulou A, Gikas A, Matzouranis G, Papafragos C, et al. Self-medication with antibiotics in rural population in Greece: A cross-sectional multicenter study. BMC Fam Pract. 2010;11:58. doi: 10.1186/1471-2296-11-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitsi G, Jelastopulu E, Basiaris H, Skoutelis A, Gogos C. Patterns of antibiotic use among adults and parents in the community: A questionnaire-based survey in a Greek urban population. Int J Antimicrob Agents. 2005;25:439–43. doi: 10.1016/j.ijantimicag.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 10.Stratchounski LS, Andreeva IV, Ratchina SA, Galkin DV, Petrotchenkova NA, Demin AA, et al. The inventory of antibiotics in Russian home medicine cabinets. Clin Infect Dis. 2003;37:498–505. doi: 10.1086/376905. [DOI] [PubMed] [Google Scholar]
- 11.Berzanskyte A, Valinteliene R, Haaijer-Ruskamp FM, Gurevicius R, Grigoryan L. Self-medication with antibiotics in Lithuania. Int J Occup Med Environ Health. 2006;19:246–53. doi: 10.2478/v10001-006-0030-9. [DOI] [PubMed] [Google Scholar]
- 12.Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3:491–7. doi: 10.3855/jidc.466. [DOI] [PubMed] [Google Scholar]
- 13.Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MA. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20:373–80. doi: 10.2478/v10001-007-0038-9. [DOI] [PubMed] [Google Scholar]
- 14.Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8:326–31. [PubMed] [Google Scholar]
- 15.Parimi N, Pinto Pereira LM, Prabhakar P. Caregivers' practices, knowledge and beliefs of antibiotics in paediatric upper respiratory tract infections in Trinidad and Tobago: A cross-sectional study. BMC Fam Pract. 2004;5:28. doi: 10.1186/1471-2296-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarahroodi S, Arzi A. Self medication with antibiotics, is it a problem among Iranian college students in Tehran? J Biol Sci. 2009;9:829–32. [Google Scholar]
- 17.Volpato DE, de Souza BV, Dalla Rosa LG, Melo LH, Daudt CA, Deboni L, et al. Use of antibiotics without medical prescription. Braz J Infect Dis. 2005;9:288–91. doi: 10.1590/s1413-86702005000400004. [DOI] [PubMed] [Google Scholar]
- 18.Alghanim SA. Self-medication practice among patients in a public health care system. East Mediterr Health J. 2011;17:409–16. [PubMed] [Google Scholar]
- 19.Saeed AA. Self-medication among primary care patients in farazdak clinic in Riyadh. Soc Sci Med. 1988;27:287–9. doi: 10.1016/0277-9536(88)90133-5. [DOI] [PubMed] [Google Scholar]
- 20.Neyaz Y, Khoja T, Qureshi NA, Magzoub MA, Haycox A, Walley T, et al. Medication prescribing pattern in primary care in Riyadh city, Saudi Arabia East Mediterr Health J. 2011;17:149–55. [PubMed] [Google Scholar]
- 21.Mahfouz AA, Shehata AI, Mandil AM, Al-Erian RA, Al-Khuzayem AA, Kisha A, et al. Prescribing patterns at primary health care level in the Asir Region, Saudi Arabia: An epidemiologic study. Pharmacoepidemiol Drug Saf. 1997;6:197–201. doi: 10.1002/(SICI)1099-1557(199705)6:3<197::AID-PDS267>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 22.Sawair FA, Baqain ZH, Abu Karaky A, Abu Eid R. Assessment of self-medication of antibiotics in a Jordanian population. Med Princ Pract. 2009;18:21–5. doi: 10.1159/000163041. [DOI] [PubMed] [Google Scholar]
- 23.Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8:e84177. doi: 10.1371/journal.pone.0084177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ilhan MN, Durukan E, Ilhan SO, Aksakal FN, Ozkan S, Bumin MA, et al. Self-medication with antibiotics: Questionnaire survey among primary care center attendants. Pharmacoepidemiol Drug Saf. 2009;18:1150–7. doi: 10.1002/pds.1829. [DOI] [PubMed] [Google Scholar]


