Abstract
Background:
Around 3 billion people use solid fuels (biomass and coal) for cooking and heating, and this number is expected to grow until at least 2030. Around 73.7% of households in rural Odisha use wood for cooking. This current study is an attempt to evaluate the impact of solid cooking fuels on health of rural women in age group of 20–40 years and to study the relationship between the duration of exposure to cooking fuels and various health problems.
Materials and Methods:
This cross-sectional study was carried out in a village which is under the field practice area of the rural health and training centre, under Department of Community Medicine, Kalinga Institute of Medical Sciences. Universal sampling technique was adopted for sample selection. Chi-square test was used to find the association between cooking fuel usage and self-reported symptoms.
Results:
Dry cough was the most common presenting symptom (15.03%), followed by eye and nose irritation present in nearly 12% each among the study participants. Headache, dry cough, and hypertension (HT) was found to associated with number of cooking years and was also found to be statistically significant (P = 0.03, 0.02 and 0.0065, respectively).
Discussion:
Our study clearly indicated that the exposure to biomass fuel smoke is significantly associated with the prevalence of symptoms of headache, dry cough, and HT. Further research is required for improving information on dose-response relationships between indoor air pollution and various health effects. Conclusion: The morbidities were increased with increase in duration of cooking . Knowledge related to health effects of cooking fuels seems to be poor among the participants.
Keywords: Health impact, rural women, solid cooking fuels
Introduction
Almost half of the world's population, who live in low-income regions, use biomass (wood, crop residues, and animal dung) as their primary fuel for cooking.[1] Many women and children are exposed to high levels of indoor air pollution emitted from biomass fuel. There is a serious impact of air pollutants on human health as they are taken by blood and circulated in the body.[2] Serious health hazards are caused by smoke from solid cooking fuels. Solid cooking fuels include coal/lignite, charcoal, wood, straw, shrubs, grass, agricultural crop wastes, and dung cakes. The World Health Organization (WHO) revealed indoor air pollution as the eighth most important risk factor responsible for 2.7% of the global burden of disease. Around 3 billion people use solid fuels (biomass and coal) for cooking and heating, and this number is expected to grow until at least 2030. In countries like India, Nepal, Pakistan, and Sri Lanka biomass fuel (72%, 88%, and 67%, respectively) is used for daily household cooking.[3] According to the National Family Health Survey-3, about 33.9% of rural households in India do not have separate room for cooking.[4] Around 73.7% of households in rural Odisha use wood for cooking.[5] Symptoms such as eye irritation, shortness of breath, cough, and dizziness were highly prevalent among biomass users. Both systolic and diastolic blood pressure showed a strong positive relationship with the number of years of exposure with biomass.[3] As of now, no studies in Odisha have assessed the adverse health impact of solid cooking fuels among rural women of Cuttack district. Keeping all the above facts in mind and due to paucity of research in similar topic in Odisha, following objective have been framed. The present study is an attempt to study the respiratory and other morbidities among rural women involved in household cooking with biomass fuels and to study the relationship between the duration of exposure and various morbidities.
In developing world, the highest air pollution exposures occur in the indoor environment. Air pollutants that are inhaled have serious impact on human health affecting, particularly the lungs and the respiratory system; as they are released in close proximity to people; they are also taken up by the blood and circulated in the body. Strong association between biofuel exposure and increased incidences of respiratory problems such as chronic obstructive pulmonary diseases (COPD) (e.g., chronic bronchitis) and bronchial asthma have been documented. The WHO has assessed the contribution of a range of risk factors to the burden of disease and revealed indoor air pollution as the eighth most important risk factor and responsible for 2.7% of the global burden of disease. It has been stated by the WHO that a pollutant released indoors is 1000 times more likely to reach the lung than that released outdoors. There is a serious impact of air pollutants on human health as they are taken by blood and circulated in the body.[2] Biofuels are at the low end of the energy ladder in terms of combustion efficiency and cleanliness.[6] Smoke from biomass combustion produces a large number of health-damaging air pollutants including respirable particulate matter, carbon monoxide (CO), nitrogen oxides, formaldehyde, benzene, 1,3 butadiene, polycyclic aromatic hydrocarbons, and many other toxic organic compounds.
In developing countries, large proportions of households rely on biofuels for cooking and space heating. The fuels are typically burned in simple, inefficient, and mostly unvented household cookstoves, which, when combined with poor ventilation, generate large volumes of smoke indoors.[7] Moreover, these cookstoves are typically used for several hours each day, at times when people are present, resulting in much higher exposure to indoor air pollutants than from outdoor sources.[8]
Exposure is usually much greater among women, who tend to do most of the cooking,[9] and among young children who tend to stay indoors and who are often carried on their mother's back or lap while she cooks.[10]
Objectives
To evaluate the impact of solid cooking fuels on health of rural women in age group of 20–40 years
To study the relationship between the duration of exposure and various health problems.
Materials and Methods
This cross-sectional study was carried out in a village which is under the field practice area of the rural health and training centre (RHTC), under Department of Community Medicine, Kalinga Institute of Medical Sciences. The study participants were women in age group of 20–40 years apparently normal and living within the catchment area of the RHTC, that is, Kalarabanka village, for at least more than 6-month duration.
Study area was selected on the basis of the following criteria:
It is one of the service areas of the RHTC and the village is in vicinity hence was chosen for better accessibility
The location is 10 km away from the National Highway thus minimizes the effect of vehicular pollution
No air polluting industries such as thermal power plant, cement factory, and rice mill within 10 km radius so no impact of industrial pollution.
Sample size
A complete enumeration of all households of the Kalarabanka village was done by the health worker of RHTC. As per the demographic data obtained by the health worker, the total population of Kalarabanka village was 879. Eligible participants were found to be 201 women.
Universal sampling was done, that is, those women who fulfilled the inclusion criteria and gave written consent were included in this study. This study included women in the age group of 20–40 years residing in the village for at least more than 6 months, who cooked regularly with biomass at least 2 h/day, 5 days/week for ≥ 5 years. Women with known case of hypertension (HT), diabetes, COPD, body mass index (BMI) (<19 and > 30 kg/m2) and family history of tuberculosis (TB), and those using mixed fuels (biomass + liquefied petroleum gas (LPG) + kerosene) and pregnant and also not giving their consent were excluded from this study.
Baseline information was collected using a pretested, semi-structured questionnaire consisting of information related to sociodemographic profile, average family income, cooking hours/day, cooking years, type of cooking fuel used, family structure, other usage of chullah, and ventilation status of the house, location of chullah, overcrowding status, and type of house. Health related information such as blood pressure was measured using automated digital blood pressure monitor, OMRON Model HEM-7120, with appropriate cuff sizes. Hypertension was defined as mean systolic BP ≥ 140 mmHg or mean diastolic BP ≥ 90 mmHg.[3] The average of three readings of systolic BP and diastolic BP were used to describe the BP for each participant and diastolic blood pressure levels (SBP and DBP, respectively) were measured while the participants were at rest in a sitting position by automated digital blood pressure monitor. International classification for categorizing individuals into Normal, Pre -hypertension, Stage 1 and Stage 2 was used. Normal: Systolic lower than 120mm Hg, diastolic lower than 80mm Hg. Pre-Hypertension: Systolic 120-139mmHg, diastolic lower than 80-89mm Hg. Stage 1: Systolic 140-159mmHg, diastolic 90-99mm Hg. Stage 2: Systolic 160mm Hg or greater, diastolic 100mm Hg or greater. For consistent measurement of each participant, three blood pressure measurements with 5-min rest interval were made. Common self-reported symptoms such as shortness of breath, cough and dizziness, nasal irritation, body ache, and frequent headache was also taken into account.
Statistical analysis
The questionnaires were checked for completeness by the researcher. All the data were compiled and analyzed using Statistical Package software for social science for windows, release 21.0 (SPSS Inc., Chicago, IL, USA) and appropriate statistical tests were applied. Chi-square test was used to test the association between self reported symptoms and duration of usage of solid cooking fuel used by the respondents with the level of significance set at P-value less than 0.05.
Ethical considerations
Approval to carry out the study was obtained from the Ethics and Research committee of the Kalinga instiute of medical sciences, KIIT university. Informed written consent was obtained from each of the respondents. Confidentiality and privacy of the respondents was respected during the interviews.
Results
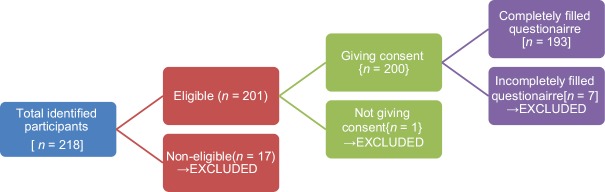
From the 218 participants, 25 participants were not included because of their missing potential confounder's data including BMI, known cases of HT, diabetes, and COPD; on medications, mixed fuel users, and family history of TB. This study included 193 (96.02% of 201) participants [Figure 1].
Figure 1.
Flow diagram showing inclusion and exclusion of study participants
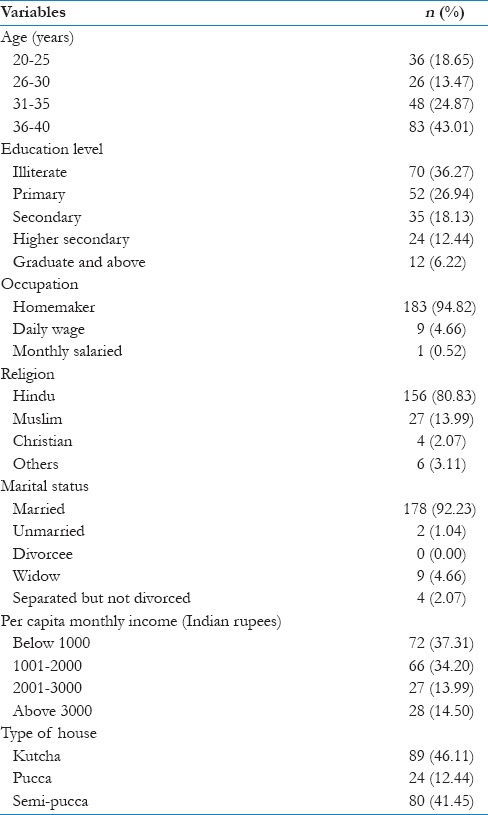
The mean age of the study participants was 33.32 ± 6.65 years, range being 20–40 years. Around 37% were illiterate; more than 95% were homemakers. About 80.83% were Hindus [Table 1].
Table 1.
General characteristics of the study population (n=193)
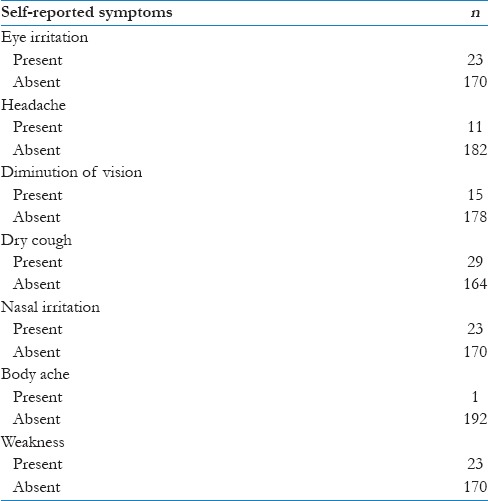
The participants were asked about common presenting self-reported symptoms in the last 6 months. Dry cough was the most common presenting symptom (15.03%), followed by eye and nose irritation present in nearly 12% each among the study participants [Table 2].
Table 2.
Distribution of participants according to the presence or absence of symptoms (n=193)
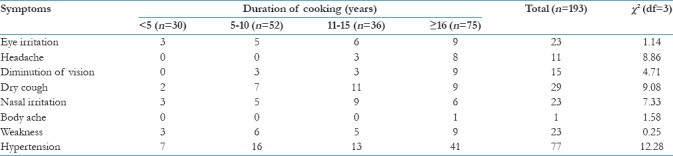
We further analyzed the symptoms with duration of cooking in years to find any associations [Table 3]. Headache, dry cough, and HT were found to associated with number of cooking years and was also found to be statistically significant.(P = 0.03, 0.02, and 0.0065, respectively)
Table 3.
Symptoms/morbid conditions with duration of cooking (years)
Discussion
Household use of unprocessed biomass fuels for cooking and heating exposes many women in developing countries to high levels of toxic air pollutants indoors. This study evaluated the role of domestic smoke on health of 193 nonsmoking rural women exposed to biomass cooking fuels. Women presenting with various symptoms/morbid conditions had greater duration of cooking. Our analysis showed that exposure to biomass fuel smoke is significantly associated with the prevalence of symptoms of headache, dry cough, and HT.
The study carried out at the National Institute of Occupational Health, Ahmedabad,[11] reported higher incidence of cough, cough with expectoration, dyspnea, and lung function abnormalities among homemakers cooking with smoky fuels who also complained of pain and watering in the eyes while cooking. Ellegård[12] proposed eye irritation in the form of tears or smarting eyes during cooking time (tears while cooking [TWC] to be a useful determinant of indoor air pollution from cooking-related sources and also reported that persons with TWC had more respiratory symptoms. It may also lead to cataract. The mechanism is thought to involve absorption and accumulation of toxins that lead to oxidation.
Another study conducted in North India on 3701 women using different types of cooking fuels found that women using mixed fuel experienced more respiratory symptoms (16.7%), followed by biomass (12.6%), stove (11.4%), and LPG (9.9%) users.[13]
In another study done in Central India (Nagpur) reported an overall high prevalence of chronic bronchitis of 12.5% and when analyzed for different cooking devices, it was 16.7% for biomass users.[2] This could be attributed to smoke emissions from biomass fuels (wood, agricultural waste, and animal dung) containing important pollutants that adversely affect health such as suspended particulate matter, polyaromatic hydrocarbons, and polycyclic organic matter which includes a number of known carcinogens called benzo(a) pyrene, as well as gaseous pollutants such as CO and formaldehyde. These pollutants cause irritant or inflammatory action on the conjunctiva and the mucous linings of the respiratory tract from the nose to the bronchi.
This study has few limitations like being a cross-sectional study design, we get the results by chance because of cross-sectional with inherent temporal problems. Second, we used self-reported symptoms to look for the morbidities, which introduce self-reporting bias. Third, the association between exposure to household solid fuels and HT may be linked to the other factors, such as the income level, nutritional status, and person's lifestyle, and so, we should explain these associations with caution.
Conclusion
This present study showed that the women using biomass fuel for cooking suffered from respiratory and other morbidities. Furthermore, the morbidities were found to be increased with increase in duration of cooking.
There are number of health problems, for which the available evidence is very limited or inconsistent. Further research is required for improving information on dose-response relationships between indoor air pollution and various health effects (e.g., increased mortality and morbidity risks).
Limitation
As this was a cross sectional study we could not evaluate various other important health indicators due to time constraints.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Thanks to Mr. Swaroop ray chowdhry, Ms. Pratibha, Mr. Satya, and Ms. Shradha (Social worker) for their contributions to this work.
References
- 1.Mishra V, Retherford RD. Does biofuel smoke contribute to anaemia and stunting in early childhood? Int J Epidemiol. 2007;36:117–29. doi: 10.1093/ije/dyl234. [DOI] [PubMed] [Google Scholar]
- 2.Sukhsohale ND, Narlawar UW, Phatak MS. Indoor air pollution from biomass combustion and its adverse health effects in central India: An exposure-response study. Indian J Community Med. 2013;38:162–7. doi: 10.4103/0970-0218.116353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chakraborty D, Mondal N, JK Datta. Indoor air pollution from solid biomass fuel and rural health damage: A micro-environmental study in rural area of Burdwan, West Bengal. Int J Sustain Built Environ. 2014;3:262–71. [Google Scholar]
- 4.International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-3) 2005-06. India. Mumbai: International Institute for Population Sciences; 2007. [Google Scholar]
- 5.International Institute for Population Sciences (IIPS) and ORC Macro. District Level Household and Facility Survey (DLHFS-3), 2007-08. India. Mumbai: International Institute for Population Sciences; 2010. [Google Scholar]
- 6.Smith KR, Liu Y. Indoor air pollution in developing countries. In: Samet JM, editor. Epidemiology of Lung Cancer. New York, NY: Marcel Dekker, Inc; 1994. pp. 154–63. [Google Scholar]
- 7.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull World Health Organ. 2000;78:1078–92. [PMC free article] [PubMed] [Google Scholar]
- 8.Smith KR. Indoor air pollution in developing countries: Recommendations for research. Indoor Air. 2002;12:198–207. doi: 10.1034/j.1600-0668.2002.01137.x. [DOI] [PubMed] [Google Scholar]
- 9.Behera D, Dash S, Malik SK. Blood carboxyhaemoglobin levels following acute exposure to smoke of biomass fuel. Indian J Med Res. 1988;88:522–4. [PubMed] [Google Scholar]
- 10.Albalak R, Frisancho AR, Keeler GJ. Domestic biomass fuel combustion and chronic bronchitis in two rural Bolivian villages. Thorax. 1999;54:1004–8. doi: 10.1136/thx.54.11.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute of Occupational Health, Ahmedabad. Annual Report. Domestic Source of Air Pollution and its Effects on the Respiratory Systems of Housewives in Ahmedabad. 1982:2–4. [Google Scholar]
- 12.Ellegård A. Tears while cooking: An indicator of indoor air pollution and related health effects in developing countries. Environ Res. 1997;75:12–22. doi: 10.1006/enrs.1997.3771. [DOI] [PubMed] [Google Scholar]
- 13.Behera D, Jindal SK. Respiratory symptoms in Indian women using domestic cooking fuels. Chest. 1991;100:385–8. doi: 10.1378/chest.100.2.385. [DOI] [PubMed] [Google Scholar]