Abstract
Background:
Self-medication is a serious health problem that leads to an increased per capita consumption of medications, drug resistance, lack of optimal treatment, drug poisoning, and other unwanted complications. This study was conducted to compare self-medication in pregnant and nonpregnant women presenting to Shahid Akbar Abadi Teaching Hospital in Tehran, Iran.
Materials and Methods:
To conduct this cross-sectional study, 210 pregnant women and 210 nonpregnant women aged 15–45 years presenting to Shahid Akbar Abadi Teaching Hospital, Tehran, Iran, were selected through random sampling. Data were collected through interviews using a semi-structured questionnaire. The Chi-square test, t-test, and logistic regression model were used to analyze the data.
Results:
The prevalence of self-medication was 34.8% in the pregnant and 77.1% in the nonpregnant women. The age group in which the most frequent instances of self-medication were observed (53.4%) was the 21–30 age group in the pregnant women and the 31–40 age group (44.4%) in the nonpregnant women, suggesting a statistically significant intergroup difference in terms of age (P = 0.0001). Medicinal plants were the most common medications used by the pregnant women (19.6%) and synthetic medications were the most common used by the nonpregnant women (38.1%). The reasons for using medications without a prescription included believing in the illness being mild (22.8%), not having health insurance (9%), easy access in the pregnant women, a previous history of the illness, and easy access in the nonpregnant women.
Conclusions:
As medicinal plants are the most common medications used by pregnant women and since assessing the risk of herbal substances is difficult, pregnant women should be advised against the arbitrary use of these substances.
Keywords: Herbal medicine, medicinal plants, pregnant women, self-medication
Introduction
The World Health Organization (2000) defines self-medication as “the use of medicinal products by the consumer to treat self-recognized disorders or symptoms, or the intermittent or continued use of a medication prescribed by a physician for chronic or recurring diseases or symptoms.”[1] As a concept, self-medication dates back to the 1980s. “The self-medication concept is reminiscent of an equally popular belief about cravings for certain types of food, given credence in psychology and physiology as 'specific hungers'.”[2] Self-medication is a serious social health and economic problem all over the world, including Iran.[3] In one study, Azami-Aghdash et al. reported the overall prevalence of self-medication in Iran as 53%, which exceeds the percentage reported in other studies conducted elsewhere in the world; for example, the prevalence of self-medication was reported as 29.9% in Brazil (2010), 32.9% in China (2011), 18.9% in Portugal (2014), 13.8% in Germany (2004), 11.9% in India (2014), and 19.2% in Nigeria (2011). As shown, most other countries have a reportedly lower prevalence of self-medication than Iran.[4] There is currently a global increase in the consumption of drugs and the expenditure in them; by 2016, the annual global spending on medicines is expected to reach nearly $1.2 trillion.[5] Self-medication increases the likelihood of outlawing the use of medicines and drug abuse.[6] The risks associated with self-medication include not getting a proper clinical evaluation for the condition by a health-care provider, which could result in misdiagnosis and the incorrect choice of drugs, delays in seeking appropriate treatment, the excessive use of drugs, the use of lower dosages, and prolonged duration of use.[7] The current trends of self-medication appear to be economy driven, as persons not able to afford the costs of seeking medical care practice self-medication as a more feasible alternative.[8] The use of herbal medicines is believed to be increasing in many developing and industrialized countries. Herbal medicines are defined as plant-derived material and preparations perceived to have therapeutic effects and containing raw or processed ingredients from one or more plants; this category of medicines includes herbs, herbal material, herbal preparations, and finished herbal products that contain parts of plants or other plant materials as their actual ingredients.[9] Studies have concluded that the inclination to self-medication is more common among women, especially those who are pregnant, live alone, have chronic health issues or psychiatric conditions, and are younger.[8] The use of medicines during pregnancy calls for a particular attention because, in this case, the health and life of the unborn child is also at stake aside from the mother's.[10] Exposing pregnant women to medicines is a particular health concern due to the risk of congenital malformations and stillbirth. Abnormalities occur in approximately 2%–3% of all newborns, with an estimated 1% being the result of prescription drug use.[11] Given the importance of the issue of self-medication in pregnant women, whose high-risk health behaviors can create problems for both the mother and the fetus, and also the importance of the issue in nonpregnant women, this study was conducted to investigate the prevalence and causes of self-medication in women.
Materials and Methods
This cross-sectional, descriptive, analytical study was conducted over 3 months' period from October 22, 2016, to January 22, 2017, on 420 women presenting to Shahid Akbar Abadi Teaching Hospital in Tehran; this center was selected because of being related to government and high rate of pregnant women reference to gynecologist; additionally, it is a thoroughly academic centers to which applicants refer in case of necessity. The participants consisted of 210 pregnant and 210 nonpregnant women aged 15–45 years. To conduct the study, first, after taking a moral code number IR-IUMS. REC 1395.95-29032-208-03, a formal introduction letter from Iran University of Medical Sciences was submitted to Shahid Akbar Abadi Hospital. Data collection then began with a semi-structured questionnaire as a part of master's thesis associated with the department of Midwifery of Ahvaz University of Medical Sciences. Permission to use the questionnaire was obtained through E-mail and was evaluated by ten faculty members of Shahid Akbar Abadi Teaching Hospital and had had its reliability confirmed with a Cronbach's alpha of 0.81. The sample size was obtained by statistical advice for each group which earned 210 with 80% power to detect the effect size of 0.06 using a two-sided t-test. The goal is a significant level of 0.0500. The real significance level obtained by this test is 0.0530. Women with special diseases who required long-term medication use, those with a history of mental illness (such as depression), or those who did not consent to participate in the study for any reason were excluded. Samples from eligible pregnant women in prenatal clinic samples and nonpregnant women in the hospital gynecology clinic at the time in the morning to get their service were performed. The participants were selected based on the inclusion and exclusion criteria, and they submitted their written consent form after they were ensured of the anonymity of the questionnaires, the confidentiality of their data, and their right to withdraw at any time during the interviews. The researcher and a research assistant (BSc. in Midwifery) then held the interviews and filled out the questionnaires after briefing the participants on the objectives of the research and providing them with definitions of synthetic medications, herbal medicines, and medicinal plants. This semi-structured questionnaire consisted of open-ended questions and guided the interviews. For the nonpregnant women, the questionnaire contained 12 demographic items (on age, level of education, occupation, reproductive health, gestational age, etc.) and 23 items on self-medication (including the route of administration and the type, form and duration of medication used, instances of medication use, their causes, etc.). For the pregnant women, in addition to the items shared with the nonpregnant women, several items also discussed their current pregnancy (prenatal care, high- or low-risk nature of the pregnancy, the frequency of receiving prenatal care, etc.). The data obtained were analyzed in SPSS-19 (IBM, Armonk, NY, United States of America) using descriptive statistics such as frequency distribution, the Chi-square test, the Phi statistic, the independent t-test, and the logistic regression model. The variables of age, level of education, occupation, the number of births, the number of abortions, ethnicity, type of health insurance, etc., were entered into the univariate logistic model, and the significant variables and others that were considered important by the researcher and in previous articles were entered into the multivariate logistic model and the required analyses were then performed. The level of statistical significance was set at P < 0.05 and confidence interval at 95%.
Results
The prevalence of self-medication was 34.8% (n = 73) in the pregnant and 77.1% (n = 162) in the nonpregnant women [Table 1]. Of the total 210 pregnant women, 47.6% presented to health-care centers, 32.9% to physicians' offices, and 18.1% to midwives' offices for receiving prenatal care. The majority of the pregnant women who self-medicated had a high school education (49.3%) and 73 (45.1%) nonpregnant women who self-medicated also had a high school education, which does not suggest a statistically significant intergroup difference (P = 0.081). The results showed that 94.1% of the pregnant and 92% of the nonpregnant women who self-medicated had health insurance, which does not suggest a statistically significant intergroup difference (P = 0.830). The pregnant women who self-medicated even in their current pregnancy reported their main reasons to be nausea, vomiting, and heartburn (5.75%), morning sickness (4.3%), lack of appetite (3.8%), spotting (2.95%), and high blood pressure (2.4%), in respective order of prevalence. The most common medications used included medicinal plants in the pregnant women (19.6%) and synthetic medications (38.1%) in the nonpregnant women [Table 2], which suggests a significant intergroup difference in terms of the type of medication used (P = 0.0001). The most common herbal medicines used during pregnancy for self-medication included thyme, Mentha pulegium and mint water (19.6%), musk willow, and Fumaria and chicory water (7.1%); in the pregnant women, 20% used thyme, Mentha pulegium, and mint extract, 19% used the distilled water of different plants, 9% used ibuprofen, 8.6% used cough syrup, and 8.1% used antibiotics; these figures suggest a statistically significant difference between the pregnant and nonpregnant women in terms of the use of medications (P = 0.0001), while 4.8% of pregnant women used medicinal plants arbitrarily during their entire course of pregnancy. In the pregnant women, the most frequent duration of medication was 1 month for all the three categories of medications. The results showed statistically significant differences between the pregnant and nonpregnant women in the use of synthetic medications and medicinal plants (P = 0.0001), but not in the use of herbal medicines. From the total of 17 pregnant women who used synthetic medications, nine (4.3%) procured their medications from the pharmacy (which was the most common means of access to this category of medications) and seven (3.3%) used the medications they already had at home; in the nonpregnant women, 54 (25.7%) procured their medications from the pharmacy and 16 (7.6%) used the medications they already had at home for self-medication. Sixteen of the pregnant (7.6%) and 21 of the nonpregnant (10%) women procured their herbal medicines from the pharmacy while five of the pregnant (2.4%) and eight of the nonpregnant (3.8%) women used the herbal medicines they already had at home for self-medication. In addition, 1.9% of the pregnant and 2.4% of the nonpregnant women got their supply of medicinal plants from friends and acquaintances while 3.3% of the pregnant and 3.3% of the nonpregnant women used the medicinal plants they already had at home for self-medication; however, 11.4% of the pregnant and 23.35% of the nonpregnant women procured medicinal plants from medicinal plant shops (which was the most common means of access to this category of medications); these figures reveal a significant difference between the pregnant and nonpregnant women in terms of the means of procuring synthetic medications and medicinal plants (P = 0.0001), but not in the means of procuring herbal medicines. According to the results, the proximity of pharmacies and medical plant shops was the main reason for which the participants met their medical needs by visiting these shops. The most common source of information about synthetic medications was family and friends in both groups; however, most of the pregnant women obtained their information about medicinal plants from friends and family first and from books, magazines, the Internet, and medicinal plant shops' clerks next; the nonpregnant women obtained this information from friends and family first and from their own previous experience with the illness and from medicinal plant shops' clerks next; a statistically significant difference was observed between the pregnant and nonpregnant women in terms of the sources of information about synthetic medications and medicinal plants (P = 0.0001). In the pregnant women, the most common reasons for the use of synthetic medications without a prescription were having no health insurance, easy access, the availability of the medication at home, believing that plants and herbal medicines are harmless, and not taking the disease seriously [Table 3]. In the nonpregnant women, the most common reasons included easy access, a previous history of the illness, the availability of the medication at home, having witnessed good results from self-medication in the past, the illness being mild, and having no health insurance. There was a statistically significant difference between the pregnant and nonpregnant women in terms of the reasons for the use of medications without a prescription (P = 0.0001). Nearly 3.3% of the pregnant and 14.8% of the nonpregnant women used complementary medicine; massage therapy performed by a physician for relieving back ache was the most prevalent type of treatment received in the pregnant women (1.9%) and bloodletting performed by a physician for back ache and muscle pain was the most common type in the nonpregnant women (11.4%). A statistically significant intergroup difference was thus observed in terms of the use of complementary medicine (P = 0.0001).
Table 1.
A comparison of the frequency and demographic characteristics of the self-medicating women in the pregnant and nonpregnant groups
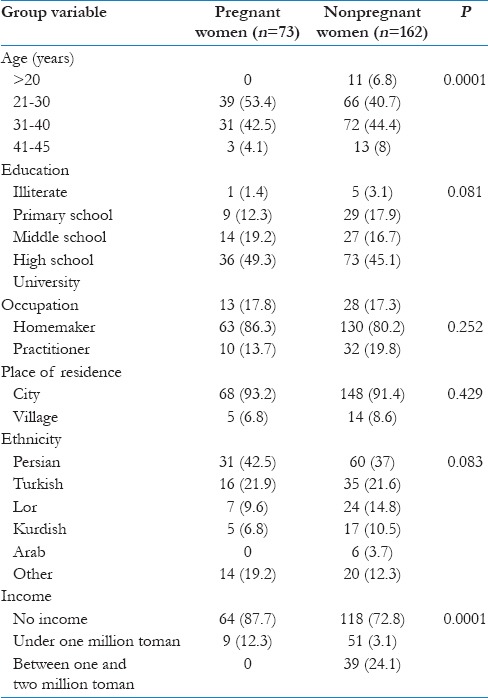
Table 2.
Type of self-medication in pregnant and nonpregnant women
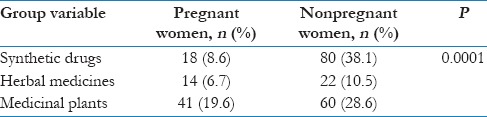
Table 3.
The reasons for the use of medications without a physician's prescription in the pregnant and nonpregnant groups

Most of the pregnant (23.9%) and nonpregnant (51%) women who had self-medicated reported that they did not know that the use of medications without a prescription could put themselves or their fetus at risk. In addition, 62.3% of the pregnant and 71% of the nonpregnant women preferred to use herbal medicines to treat their disease and 60.5% of them believed that herbal medicines and medicinal plants should be used under a physician's supervision. Moreover, 18.1% of the pregnant and 21.4% of the nonpregnant women believed that the simultaneous use of herbal medicines and synthetic medications could cause complications, while 72.4% of the pregnant and 71% of the nonpregnant women did not know that such complications could develop.
Discussion
The prevalence of self-medication was 34.8% (n = 73) in the pregnant and 77.1% (n = 162) in the nonpregnant women the results of Ayalew study (2017), which were almost consistent with what the present study showed, indicate that 36% of pregnant women use self-medication.[12] The most common age group in which the women self-medicated was the 21–30 age group (n = 39, 53.4%) for the pregnant women and the 31–40 age group (n = 72, 44.4%) for the nonpregnant women. Although self-medication was not linked to the women having health insurance or not, it was associated with their income (P = 0.0001). According to the logistic regression model, in the pregnant women [Table 4], being of Kurd and Arab ethnicities was associated with self-medication (confidence interval [CI]: 0.354–0.152, 177 odds ratio [OR] =0.7, P = 0.0002), while in the nonpregnant women [Table 5], having middle school and secondary school education was associated with this phenomenon (CI = 70.869–0.971;OR = 0.151, P = 0.043 and CI = 367.722–5.630; OR = 1.514, P = 0.0001, respectively). Dreyer et al. reported that 59.56% of the women they studied had taken at least one prescription drug and may also have used over-the-counter (OTC) medications.[20] Afshari et al. reported the rate of self-medication in nonpregnant women as 70.1% in Ahvaz.[13] These rates are consistent with the figures reported in the present study. The reasons for the use of medications without a physician's prescription included believing in the illness being mild (22.8%), not having health insurance (9%), easy access and the availability of the medication at home in the pregnant women, and easy access (16.2%) and a previous history of the illness (12.4%) in the nonpregnant women. In a study by Befekadu et al., the majority of the pregnant women claimed that they self-medicated because drugs were easily available everywhere (45.9) and because they wasted less time this way (32.8%).[14] According to Afshari et al., the most important reasons for self-medication in pregnant women included heavy medical expenses and the easy access to medications.[13] According to a study by Garofalo et al., the participants self-medicated because they believed that the disease was too mild and they did not need a physician's services (84.1%); their other reason was that they were merely re-taking a medication prescribed for them in the past (32.9%).[15] In the present study, 62.3% of the pregnant and 71% of the nonpregnant women preferred to use herbal medicines for their treatment. In a study conducted by Negarad et al. on the use of medicinal plants in pregnant women, 79.9% reported that they had been using one or several of the listed medicinal plants.[16] A study of 1420 Italian women also revealed an increased willingness to use herbal medicines over synthetic medications.[17] The most frequently used medications were medicinal plants (19.6%) in the pregnant women and synthetic medications (38.1%) in the nonpregnant women. According to Al-Ghamdi et al. in 2016, the prevalence of herbal medication use during pregnancy was 25.3%, while 33.7% of the participants used herbs during labor and 48.9% used them after delivery.[18] In a study by Asseray et al. on 3848 women, analgesics were the most frequently used medications, and the 2184 women (75%) who self-medicated had mostly used OTC drugs.[19] Assessing the risks associated with the use of herbal substances is difficult, and women who are concerned about the use of conventional drugs in pregnancy may turn to alternative therapies such as homeopathy or herbal medicines during this period, which they perceive as being “natural” and somehow safer. Many of these alternative drugs are not regulated, and information is often lacking about their safety for use in pregnancy.[20] A solution could be to inquire pregnant women about their self-medication habits, whether with herbal or synthetic drugs, in pregnancy care centers or at the time of registering with hospitals for childbirth. Given that the most common form of self-medication in pregnant women concerns herbal medicines and since some of the women did not know that self-medication put themselves and their fetus at risk, health practitioners and university education experts should seek to raise public awareness about the potential risks and complications of using herbal medicines and should focus on pregnant women as the main target of these efforts. Health practitioners are also recommended to inquire of pregnant women about their self-medication with herbal medicines and synthetic medications in their prepregnancy as well as prenatal care visits when taking their medical history. Medicinal plant shop clerks as well as pharmacy salespeople should also be requested to train their pregnant and nonpregnant customers before supplying them with their requested medicinal plants and synthetic medications. Akbar Abadi hospital was chosen due to the large number of references, and 420 samples were selected. It is proposed that multicenter studies with larger sample sizes should be done.
Table 4.
The logistic regression model for examining the relationship between certain variables in the pregnant women who self-medicated and those who did not
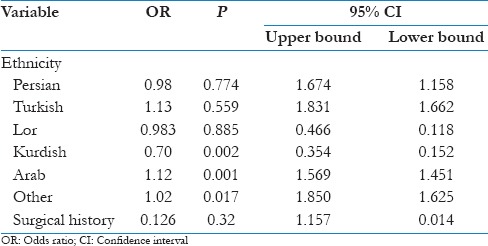
Table 5.
The logistic regression model for examining the relationship between certain variables in the nonpregnant women who self-medicated and those who did not

Conclusions
As medicinal plants are the most common medications used by pregnant women and since assessing the risk of herbal substances is difficult, pregnant women should be advised against the arbitrary use of these substances.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Hereby, the authors would like to express their gratitude to the Research Deputy of Iran University of Medical Sciences, the Director of Shahid Akbar Abadi Teaching Hospital, all the researcher assistants who helped in collecting the data and communicating with pregnant and nonpregnant women to complete the questionnaires, and all the pregnant and nonpregnant women who participated in the study and patiently responded to the researcher's questions.
References
- 1.Karamata VV, Gandhi AM, Patel PP, Desai MK. Self-medication for acne among undergraduate medical students. Indian J Dermatol. 2017;62:178–83. doi: 10.4103/ijd.IJD_243_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manzella F, Maloney SE, Taylor GT. Smoking in schizophrenic patients: A critique of the self-medication hypothesis. World J Psychiatry. 2015;5:35–46. doi: 10.5498/wjp.v5.i1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jafari F, Khatony A, Rahmani E. Prevalence of self-medication among the elderly in Kermanshah-Iran. Glob J Health Sci. 2015;7:360–5. doi: 10.5539/gjhs.v7n2p360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azami-Aghdash S, Mohseni M, Etemadi M, Royani S, Moosavi A, Nakhaee M, et al. Prevalence and cause of self-medication in Iran: A Systematic review and meta-analysis article. Iran J Public Health. 2015;44:1580–93. [PMC free article] [PubMed] [Google Scholar]
- 5.Asmelashe Gelayee D, Binega G. Assessment of medication use among university students in Ethiopia. Sci World J. 2017:4530183.5. doi: 10.1155/2017/4530183. [Doi: 10.1155/2017/4530183] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmadi SM, Jamshidi K, Sadeghi K, Abdi A, Vahid MP. The prevalence and affecting factors on self-medication among students of Kermanshah university of medical science in 2014. J Clin Diagn Res. 2016;10:IC01–4. doi: 10.7860/JCDR/2016/18018.7847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chipwaza B, Mugasa JP, Mayumana I, Amuri M, Makungu C, Gwakisa PS, et al. Self-medication with anti-malarials is a common practice in rural communities of Kilosa district in Tanzania despite the reported decline of malaria. Malar J. 2014;13:252. doi: 10.1186/1475-2875-13-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haseeb A, Bilal M. Prevalence of using non prescribed medications in economically deprived rural population of Pakistan. Arch Public Health. 2016;74:1. doi: 10.1186/s13690-015-0113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyeko R, Tumwesigye NM, Halage AA. Prevalence and factors associated with use of herbal medicines during pregnancy among women attending postnatal clinics in Gulu district, Northern Uganda. BMC Pregnancy Childbirth. 2016;16:296. doi: 10.1186/s12884-016-1095-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohra DK, Das N, Azam SI, Solangi NA, Memon Z, Shaikh AM, et al. Drug-prescribing patterns during pregnancy in the tertiary care hospitals of Pakistan: A cross sectional study. BMC Pregnancy Childbirth. 2008;8:24. doi: 10.1186/1471-2393-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Hamimi JZ, Al Balushi KA. Patterns of prescription drugs use among pregnant women at Sultan Qaboos university hospital and Sultan Qaboos university hospital family and community medicine clinic, Oman. J Pharm Bioallied Sci. 2016;8:309–13. doi: 10.4103/0975-7406.199347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayalew MB. Self-medication practice in Ethiopia: A systematic review. Patient Prefer Adherence. 2017;11:401–13. doi: 10.2147/PPA.S131496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afshari P, Mohammadi S, Pagohedeh Z, Tabesh H. Prevalence and causes of self-medication in women referred to health centers in Ahvaz City in year 2013. Biomed Res Center Persian Gulf. 2013;18:1034–44. [Google Scholar]
- 14.Befekadu A, Dekama NH, Adem M. Self-medication and contributing factors among pregnant women attending antenatal care in Ethiopia: The case of Jimma university specialized hospital. Med Sci. 2014;3:969–81. [Google Scholar]
- 15.Garofalo L, Di Giuseppe G, Angelillo IF. Self-medication practices among parents in Italy. Biomed Res Int. 2015;2015:580650. doi: 10.1155/2015/580650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nergard CS, Ho TP, Diallo D, Ballo N, Paulsen BS, Nordeng H, et al. Attitudes and use of medicinal plants during pregnancy among women at health care centers in three regions of Mali, West-Africa. J Ethnobiol Ethnomed. 2015;11:73. doi: 10.1186/s13002-015-0057-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bacchini M, Cuzzolin L, Camerlengo T, Velo G, Benoni G. Phytotherapic compounds: The consumer-pharmacist relationship. Drug Saf. 2008;31:424–7. doi: 10.2165/00002018-200831050-00008. [DOI] [PubMed] [Google Scholar]
- 18.Al-Ghamdi S, Aldossari K, Al-Zahrani J, Al-Shaalan F, Al-Sharif S, Al-Khurayji H, et al. Prevalence, knowledge and attitudes toward herbal medication use by Saudi women in the central region during pregnancy, during labor and after delivery. BMC Complement Altern Med. 2017;17:196. doi: 10.1186/s12906-017-1714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asseray N, Ballereau F, Trombert-Paviot B, Bouget J, Foucher N, Renaud B, et al. Frequency and severity of adverse drug reactions due to self-medication: A cross-sectional multicentre survey in emergency departments. Drug Saf. 2013;36:1159–68. doi: 10.1007/s40264-013-0114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dreyer NA, Blackburn SC, Mt-Isa S, Richardson JL, Thomas S, Laursen M, et al. Direct-to-patient research: Piloting a new approach to understanding drug safety during pregnancy. JMIR Public Health Surveill. 2015;1:e22. doi: 10.2196/publichealth.4939. [DOI] [PMC free article] [PubMed] [Google Scholar]


