Abstract
Introduction:
An “Inter-Arm Difference” (IAD) in blood pressure (BP) is defined as a variation in systolic BP of >10 mmHg. Various studies conducted in different population show that there are wide variations in the prevalence of IAD, which ranges from 5% to 46%. The aim of this study is to evaluate the prevalence of IAD in BP among adults and its association with risk factors.
Methods:
This community-based cross-sectional study was carried out among urban adults in Kancheepuram district. The study sample size of 1634 was calculated, and simple random sampling method was used. Data analysis was performed using SPSS software version 16. Prevalence of IAD in BP was calculated using percentages, and statistical significance was tested to look for an association.
Results:
This study shows that 26.2% were at moderate risk for vascular events with IAD in systolic BP of 10–15 mmHg and 17.3% were at high risk with IAD >15 mmHg. About 14.2% had diastolic BP difference of 10–15 mmHg indicative of moderate risk and 6.1% had a difference of >15 mmHg indicative of high risk for vascular events. The statistical significant association was found between IAD in systolic BP and risk factors such as hypertension, smoking, alcoholism, and between IAD in diastolic BP with overweight/obesity (P < 0.05).
Conclusion:
This study outcome shows that the prevalence of IAD in BP is on the higher side. Hence, specific guidelines should be brought in to practice for measuring BP in both arms to detect IAD in every health-care settings.
Keywords: Hypertension, risk factors, screening, two arm blood pressure difference
Introduction
Blood pressure (BP) is created by the force of blood pushing against the wall of blood vessels (arteries) as the heart pumps it. Normal adult BP is defined as systolic BP of 120 mmHg and diastolic BP of 80 mmHg. When the pressure in the blood vessel increases, the heart works harder to pump blood. Hypertension or raised BP is a condition in which there is persistent raised BP in the blood vessels. It is defined as a systolic BP ≥140 mmHg and/or diastolic BP ≥90 mmHg. Normal levels of both systolic and diastolic BP are important for the efficient function of vital organs and for overall health and well-being.[1] When left uncontrolled, hypertension can lead to complications affecting heart, brain, kidney, eyes, and blood vessels and hence, early detection is important to minimize such risk.
Under normal physiological circumstances, the BP reading is often same for both the arms. However, a BP difference between both arms is frequently encountered in various general populations.[2] This phenomenon known as “inter-arm difference” (IAD) was first recognized more than 100 years ago.[3] It is normal to have an IAD of <5 mmHg.[4] An IAD is defined as a variance in systolic BP of >10 mmHg.[5] The cause for IAD can be both physiological and pathological. In younger people, inter-arm BP difference can occur when a muscle compresses an artery supplying the arm or by a structural problem that prevents smooth blood flow through an artery. In older people, it is usually due to a blockage arising due to atherosclerosis.[6] Other causes are subclavian artery stenosis, aortic aneurysm, aortic coarctation, vasculitis, fibromuscular hyperplasia, connective tissue disorders, and thoracic outlet compression.[7] Hence, it is vital to detect an inter-arm BP difference for further vascular assessment and management of risk factors.[8]
It has become evident in many research that the measurement of BP in both arms should be practiced since a difference in inter-arm BP of >10–15 mmHg is a predictor or an indicator for various vascular diseases such as peripheral vascular diseases, cerebrovascular diseases, cardiovascular diseases, vasculitis, connective tissue disorders, and congenital anomalies.[9] It is also an independent predictor of reduced event-free survival.[6] The American Heart Association guidelines recommend that for management of hypertension, BP should be initially measured in both arms of the patients, as there may be large differences between both the arms. The arms with higher values should be used for subsequent measurements.[10]
Raised BP is one of the leading risk factors for global mortality and is estimated to have caused 9.4 million deaths and 7% of disease burden as measured in DALYs in 2010. A reduction in systolic BP of 10 mmHg is associated with a 22% reduction in coronary heart disease and 41% reduction in stroke in randomized trials and a 41%–46% reduction in mortality in epidemiological studies.[11] Among the US population, 15%–20% of them have significant IAD, with systolic BP difference of >10 mmHg.[5] Various studies conducted in different population show that there are wide variations in the prevalence of IAD. The prevalence ranges from as low as 5% to as high as 46%.[12,13]
Generally in day today practice, measurement of BP in one arm is more widely practiced. In such case, there is a possibility to miss out the variations, which is indicative of any underlying vascular diseases. Hence, this study was done to find out the prevalence of IAD among the adult population in the study area, since measuring BP is a simple yet an important determinant to identify the population at risk of developing vascular events in the future and take an appropriate intervention to prevent its development at the right time.
Methods
Study design
This study is a community-based cross-sectional study carried out in Anakaputhur, an urban area in Kancheepuram district of Tamil Nadu. The study was carried out during January to June 2016.
Study area and study population
The study area is the field practice area of the Urban Health Training Center attached to the Medical College and Hospital. The total population of this area is 45,562 with an adult population of 34,657. The study population was identified as any adult male or female in the age group of 20 years and above.
Sample size and sampling technique
The sampling method used was simple random sampling. The study area comprises of a total adult population of 34,657 spreads over 15 wards. From among the 15 wards, 1 ward with population of 2911 (adult population – 1747) was selected randomly. Based on the inclusion and exclusion criteria, 1634 adults participated in the study. The data collection started from the first house on the street and subsequently visiting all the households on the way until the total adult population was covered.
Inclusion and exclusion criteria
The inclusion criteria for the study were any adult male or female, who is apparently healthy looking and willing to participate in the study. The exclusion criteria for not including in the study were any adult who is suffering from any form of severe illness and pregnant women and those not willing to participate.
Data collection
The data collection and measurements were carried out by 15 interns who were posted at the Urban Health Training Center as part of their primary health care training. The interns were briefed thoroughly, and the correct techniques of all the relevant measurements were demonstrated. The interns were made to perform the measurements on normal subjects, and the investigator validated their technique. The data for this study were collected by house-to-house visits using a standardized pretested structured interview schedule, consisting of the sociodemographic particulars and risk factors of hypertension. Anthropometric measurements such as height, weight, and clinical measurement of BP on both right and left arm were recorded. All the relevant data collected were entered into the structured questionnaire and had been counter checked by the investigator for any data error.
Blood pressure measurement
The BP was measured using mercury sphygmomanometer. The BP between the right and left arm were measured sequentially. As BP values fluctuates within minutes, most accurate results were obtained by checking the BP twice, 5 min after first measurement and the average value was calculated.
The new clinical guidelines for hypertension from the National Institute for Health and Clinical Excellence considers an IAD of <10 mm Hg to be normal and attributes a difference of >20 mm Hg to underlying vascular disease.[14] The characteristic of inter-arm BP difference was classified as follows: <5 mmHg as normal, 5–10 mmHg as low risk, 10–15 mmHg as moderate risk, and >15 mm Hg as high risk for any vascular event.[15] The same has been used for classifying the inter-arm BP difference in this study.
Data analysis
The data analysis was carried out using SPSS for Windows, Version 16.0 (Manufactured by SPSS Inc. Chicago, USA). The prevalence of inter-arm BP difference was calculated using percentages. Statistical significance (Chi-square test and P value) was tested to look for an association between inter-arm BP difference and risk factors.
Ethical clearance, informed consents and support
The study was carried out after obtaining approval from the Institutional Ethical Committee. The participants were briefed about the study, and informed consent was obtained before the data collection. The institution as part of the logistics support provided all materials, workforce and other resources needed for conducting the study.
Results
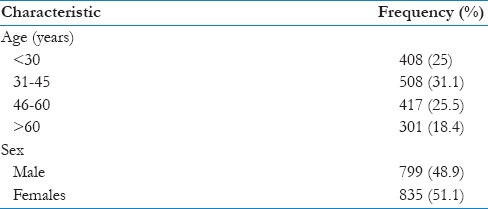
This study was carried out to estimate the prevalence of inter-arm BP difference among the adult population and its association with risk factors among 1634 study subjects. Regarding the age- and sex-wise distribution of the study population, the mean age of the participants was 44.2 ± 15.9 years. Males constituted 48.9% and females were 51.1% [Table 1].
Table 1.
Age and sex.wise distribution of the study population (n=1634)
In this study, regarding associated risk factors of vascular diseases, 32.6% were overweight, and 22.8% were obese based on their body mass index (BMI), 19.4% were known hypertensive, 18.9% were known diabetics, 10.9% were smokers, 10.8% of participants consumed alcohol, and 2.9% had a history of cardiovascular diseases [Figure 1].
Figure 1.
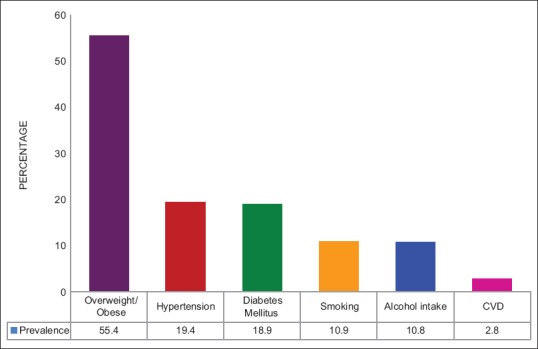
History of associated risk factors among the study subjects
Regarding the prevalence of inter-arm BP differences, it was found that 26.2% (n = 428) had a difference of 10–15 mmHg (systolic BP) and therefore were moderately at risk for vascular events. About 17.3% (n = 283) were at high risk for vascular events (difference >15 mmHg). Regarding the difference in diastolic BP for both the arms, it was observed that 14.2% (n = 232) had a difference of 10–15 mmHg and therefore were moderately at risk, whereas 6.1% (n = 100) had a difference of >15 mmHg and were at high risk for vascular events [Figure 2].
Figure 2.
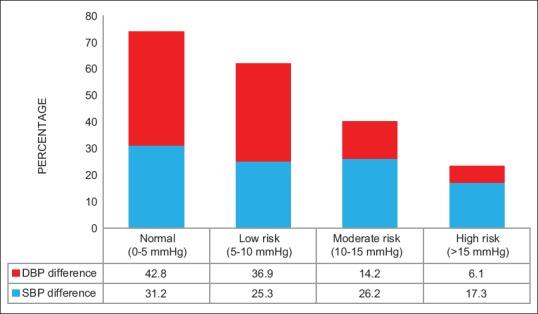
Prevalence of inter-arm blood pressure difference among study subjects
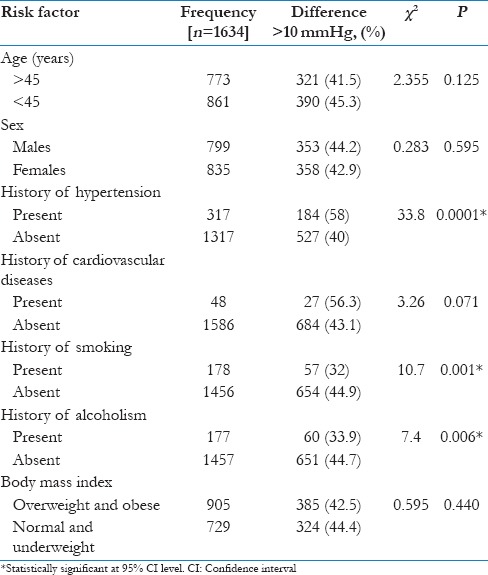
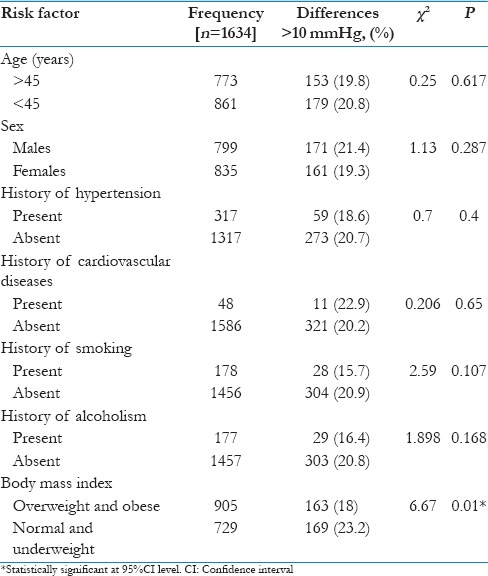
In this study, it is observed that there was an association between the inter-arm BP difference and associated risk factors. It is observed that known hypertensive individuals have a significant risk of difference in BP compared to nonhypertensives (P < 0.05). Furthermore, smokers are at increased risk of inter-arm BP difference compared to nonsmokers (P < 0.05). Similar findings are observed with alcoholism (P < 0.05) [Table 2].
Table 2.
Association between risk factors and inter arm differences in systolic blood pressure
Regarding the association between associated risk factors and the IAD in diastolic BP, it was found that people who were obese/overweight were significantly at risk of having IAD in diastolic BP compared to people who had normal BMI (P < 0.05) [Table 3].
Table 3.
Association between risk factors and inter arm differences in diastolic blood pressure
Discussion
Hypertension is a well-recognized noncommunicable disease which is under public health focus for the past few years. Screening for hypertension using a BP apparatus is one of the simplest and easiest methods to identify individuals with high BP. However, the concept of measuring BP in both the arms to identify the difference in BP has still not gained attention in our public health scenario. It is vital to identify individuals with significant IAD in BP which not only serves as a precursor of any vascular diseases in the future but also prevents from missing diagnosis. This study was carried out among 1634 adult population in the urban area of Kancheepuram district which shows a high prevalence of inter-arm BP difference, and it shows statistically significant association with risk factors.
In this study regarding the distribution of diseases among the study participants, 55.4% were overweight/obese, 19.4% were hypertensive, 18.9% were diabetic, and 2.9% had cardiovascular diseases. Similar such distribution of diseases was found among the study population in a similar study done by Sharma et al.[12]
In this study, the prevalence of IAD in systolic BP of ≥10 mmHg is 43.5%. Among the study subjects, 57.2% of them had an IAD in diastolic BP of ≥5 mmHg. The prevalence of IAD is high and this has to be taken into consideration to implement the practice of measuring BP in both arms to detect the difference at an early stage itself. These individuals are at risk of vascular events in the future and hence require regular follow-up. In a study conducted by Seethalakshmi et al., 46% of participants had IAD in systolic BP of >10 mmHg and 35% of study participants had diastolic inter-arm BP difference of >5 mmHg.[13] In another study conducted by Clark et al., the prevalence of IAD in systolic BP was ≥10 mmHg in 38% of study population.[16]
With regard to the association between inter-arm BP difference and associated factors, individuals with a history of hypertension had significant inter-arm BP difference compared to nonhypertensive. This association was statistically significant (P < 0.01). In a study done by Su et al., it was found that hypertension was associated with an IAD in systolic BP of 10 mmHg or more.[17] In this study, the difference in inter arm BP was more among smokers compared to nonsmokers (P < 0.01). Similar findings are observed with alcoholism also with statistical significance (P < 0.01). In a study conducted by White et al., there is a significant association between inter-arm BP difference of >10 mmHg and factors associated with lifestyle such as smoking, alcohol intake and obesity.[18]
In this study, it was found that people who are obese/overweight had statistical significant IAD in diastolic BP compared to people who had normal BMI (P < 0.05). In a study conducted by Song et al., the larger IAD in diastolic pressure was independently associated with BMI.[19]
Hence, it is important to remember that the modifiable risk factors such as smoking, alcohol, obesity are not only risk factors of hypertension but also could be associated with the inter-arm BP difference which when detected at an early stage and managed appropriately will prevent the occurrence of any vascular events in the future.
Conclusion
Measurement of BP in both arms to detect the difference, albeit recommended in many guidelines, is still not brought into practice in any health-care setting including primary care. It is crucial to make it a core component during initial BP measurement itself. Although national and state programs have been implemented to combat the burden of hypertension, which is one of the preventable noncommunicable disease posing a burden, awareness among medical personnel is not sufficient to detect the inter-arm BP difference at an initial stage. Screening for inter-arm BP difference at an initial level will help in detecting the vascular events likely to occur in the future. It will also help in identifying patients with the possible significant arterial disease who can be made to undergo further appropriate imaging test to identify any vascular lesion.
Considering the demographic pattern of our population in India, specific guidelines should be explicitly brought in for detecting the inter-arm BP difference so that it can be widely followed for doing more community and hospital-based studies. This will help in identifying the actual prevalence and will guide the policy makers to plan more comprehensive measures to address strategies for early diagnosis and prevention of developing vascular diseases in the long run. However, the practice to measure BP in both arms should be brought into regular practice in every health-care setting including primary health care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We acknowledge all the interns posted in the Department who were involved in data collection and the field staff who helped in organizing and carrying out this study in the field practice area of the urban health training center.
References
- 1.WHO. Global Brief on Hypertension: World Health Day. Section 2. Hypertension: The Basic Facts. 2013. [Last accessed on 2017 Jan 23]. p. 11. Available from: http://www.apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf?ua=1 .
- 2.Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: A systematic review. J Hum Hypertens. 2006;20:923–31. doi: 10.1038/sj.jhh.1002093. [DOI] [PubMed] [Google Scholar]
- 3.Cyriax EF. Unilateral alterations in blood-pressure caused by unilateral pathological conditions: The differential blood-pressure sign. QJM. 1920;13:148–164. [Google Scholar]
- 4.Hypertension in Adults: Diagnosis and Management. NICE Guidelines. Guidance: Measuring Blood Pressure. 2011. [Last accessed on 2017 Jan 23]. p. 10. Available from: https://www.nice.org.uk/guidance/cg127/resources/hypertension-in-adults-diagnosisand-management-35109454941637 .
- 5.Lowry AC, Awick JL, Slayman MK, Christine Colella DN. Inter-arm Blood Pressure Differences; 2015. Blood Pressure Differences. 2015. [Last accessed on 2017 Jan 23]. Available from: http://www.nurse-practitioners-and-physician-assistants-advanceweb.com/Features/Articles/Inter-arm-Blood-Pressure-Differences.aspx .
- 6.Patrick JS. Different Blood Pressure in Right and Left Arm Could Signal Trouble. 2012. [Last accessed on 2017 Jan 23]. Available from: http://www.health.harvard.edu/blog/differentblood-pressure-in-right-and-left-arms-could-signaltrouble-201202014174 .
- 7.Mehlsen J, Wiinberg N. Interarm difference in blood pressure: Reproducibility and association with peripheral vascular disease. Int J Vasc Med. 2014;2014:841542. doi: 10.1155/2014/841542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: Primary care cohort study. BMJ. 2012;344:e1327. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark CE, Campbell JL, Powell RJ. The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: Cohort study. J Hum Hypertens. 2007;21:633–8. doi: 10.1038/sj.jhh.1002209. [DOI] [PubMed] [Google Scholar]
- 10.Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, et al. Guidelines for management of hypertension: Report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens. 2004;18:139–85. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 11.Global Status Report on Non Communicable Diseases. WHO. Chapter 6: Global target 6. 2014. [Last accessed on 2017 Jan 23]. p. 67. Available from: http://www.apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1 .
- 12.Sharma B, Ramawat P. Prevalence of inter-arm blood pressure difference among clinical out-patients. Int J Health Sci (Qassim) 2016;10:229–37. [PMC free article] [PubMed] [Google Scholar]
- 13.Seethalakshmi K, Bahuleyan B. Inter arm blood pressure difference: An indicator of cardiovascular risk. Int J Res Med Sci. 2015;3:3782–5. [Google Scholar]
- 14.Hypertension: The Clinical Management of Primary Hypertension in Adults. NICE Clinical Guidelines 127. Diagnosing Hypertension. 2011. [Last accessed on 2017 Jan 23]. p. 11. Available from: https://www.workspace.imperial.ac.uk/ref/Public/UoA%2002%20.%20Public%20Health,%20Health%20Services%20and%20Primary%20Care/NICE%20hypertension%20guidelines.pdf .
- 15.Weinberg I, Gona P, O'Donnell CJ, Jaff MR, Murabito JM. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127:209–15. doi: 10.1016/j.amjmed.2013.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark CE, Taylor RS, Butcher I, Stewart MC, Price J, Fowkes FG, et al. Inter-arm blood pressure difference and mortality: A cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. 2016;66:e297–308. doi: 10.3399/bjgp16X684949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su HM, Lin TH, Hsu PC, Chu CY, Lee WH, Chen SC, et al. Association of interarm systolic blood pressure difference with atherosclerosis and left ventricular hypertrophy. PLoS One. 2012;7:e41173. doi: 10.1371/journal.pone.0041173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White J, Mortensen LH, Kivimäki M, Gale CR, Batty GD. Interarm differences in systolic blood pressure and mortality among US army veterans: Aetiological associations and risk prediction in the Vietnam experience study. Eur J Prev Cardiol. 2014;21:1394–400. doi: 10.1177/2047487313496193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song BM, Kim HC, Shim JS, Lee MH, Choi DP. Inter-arm difference in brachial blood pressure in the general population of Koreans. Korean Circ J. 2016;46:374–83. doi: 10.4070/kcj.2016.46.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]


