Abstract
Introduction:
Increased risk of periodontal disease has been associated with diabetes mellitus (DM) and also periodontitis is considered as the sixth complication of DM. Medical physicians may have an advantageous position compared to the dentists to provide early patient counseling about oral health because patients attend medical offices more often than to dental offices and are more likely to be affiliated to medical than to dental insurance. Hence, the medical practitioners should have sufficient knowledge in this regard. The study aimed to assess the knowledge, attitudes, and practice behaviors of endocrinologists, general medicine practitioners, and diabetologists on the relationship between periodontal disease and DM.
Materials and Methods:
Data were collected from sixty participants practicing in Nellore, using a structured questionnaire survey. The obtained data were analyzed through percentages.
Results:
All the participants (100%) were aware that there existed a relation between oral health and general health. However, only 17.8% (10) of the participants refer their patients to dentists without patients asking for referral.
Conclusion:
The endocrinologists were aware of the didactic relationship, whereas general medicine practitioners and diabetologists are not much well-equipped with the knowledge on relationship between DM and periodontitis. There exists a wide gap between their practice behaviors and current scientific evidence. Therefore, more emphasis must be made by medical practitioners for the diabetic patient toward periodontal health which is most important yet neglected aspect of comprehensive health care.
Keywords: Diabetes mellitus, endocrinologists, general practitioners, knowledge, periodontal disease
Introduction
Diabetes mellitus (DM) is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both.[1] Of all the health emergencies, globally, DM constitutes one of the major emergencies in 21st century. According to the International Diabetes Federation, India ranks 2nd in its order globally with the prevalence rate of 69.2 million in the year 2015 which is expected to increase 123.5 million by the year 2040 with more prevalence in urban areas than in rural areas.[2] The various medical and dental complications associated with diabetes include cardiovascular diseases, retinopathy, nephropathy, and neuropathy, microvascular diseases, altered wound healing, periodontitis, tooth loss, gingivitis, and soft tissue pathologies. Among all the oral complications, periodontitis is most widely noted.[3,4]
Chronic periodontitis is an infectious disease resulting in inflammation within the supporting tissues of the teeth, progressive attachment, and bone loss.[5] The proven didactic relationship between diabetes and periodontitis suggests that increased susceptibility of periodontitis for the patient with uncontrolled diabetes and vice versa.[6] Hence, diabetic patients must be aware of this possible relationship for the prevention of oral and periodontal problems. However, studies have proven that the awareness on oral and periodontal problems is low among diabetic patients compared to the systemic diseases.[6,7] Reports shown that only10.8% of the diabetic patients have visited a dentist for a regular dental checkup. The main reason for not visiting a dentist for >2 years was unawareness (29.7%) and attitude of the need for a dental checkup.[7] This unawareness in large majority population can be due to failure of the information from the health-care providers.
As the patients are unaware of this possible relationship, now the role of health-care providers becomes crucial in increasing the knowledge, awareness, and its possible complications. Diabetic patients are encouraged for the more comprehensive oral health as an integral part of general health. Actually, the International Diabetes Federation and World Dental Federation have made emphasis on that the key of prevention of periodontitis for patients with DM lies in close collaboration between dentists and physicians.[2]
However, studies reported that medical practitioners have limited knowledge of this possible relationship and very few are referring their diabetic patients to the dental practitioner for the advice.[8,9] As India ranks second in its order globally for the prevalence of diabetes, an attempt was made to assess the knowledge, attitude, and practice behaviors regarding diabetes and periodontal disease among medical practitioners who deal with diabetes and their willingness to advise their patients to seek dental treatment.
Materials and Methods
This cross-sectional survey was carried out involving health-care professionals who are registered and practicing in and around Nellore city, Andhra Pradesh, India, with specialty in endocrinology, general medicine, and diabetology with the help of a self-administered, structured questionnaire. The questionnaire was designed and subsequently distributed by the principal investigator and coinvestigators. After explaining the purpose of the study, verbal informed consent has been obtained from all the participants. Twenty-three item questionnaires were developed. The first part sought information on demographic and job-related characteristics including age, gender, specialty, experience, place, and years of practice. The second part addressed doctors' perceptions of the relationships between diabetes, oral, periodontal health, and sources of information. The third part addressed the practice behaviors and advising of diabetic patients for periodontal health evaluation. The data were collected from January to March 2016.
Results
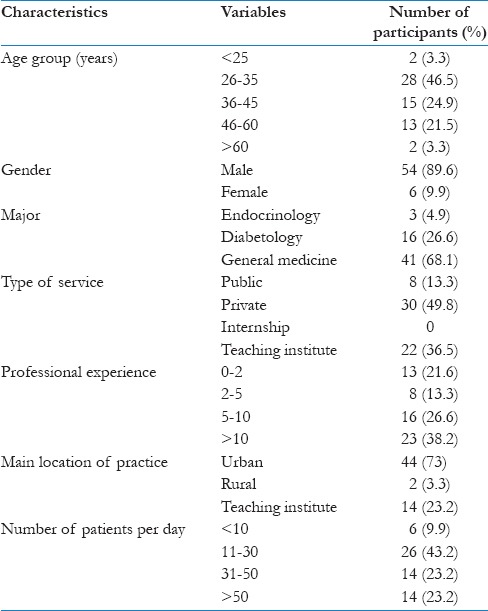
A total of 66 participants who are registered and practicing in Nellore district were included in the study. Among the 66 participants, 3 are endocrinologists, 45 are general medicine practitioners, and 18 are diabetologists. Of all the participants, two of them hesitated to participate and four did not complete the survey fully and were excluded from the study. Thus, the effective analytical data from sixty respondents were analyzed. Demographic and job-related information is summarized in Table 1.
Table 1.
Demographic and job-related characteristics of the respondents by number and percentage of total respondents
The entire participants (60, 100%) were aware of few signs and symptoms of general dental disease, among which only 66.4% knew about the gingival and periodontal problems and its consequences. Majority (80%) of them reported the symptoms as gingival bleeding, swelling of gums, gingival/periodontal abscess, halitosis, and loose teeth. Among them, 60% thought that the reason may be due to local factors and food entrapment. Only remaining 20% have mentioned that systemic conditions may be the cause.
All the participants (100%) agreed that there exists some sort of relationship between diabetes and periodontal health, of which only 43.2% were aware of the bidirectional relationship and the remaining 56.4% reported diabetes as a risk factor of periodontitis. The report regarding periodontitis as a risk factor of diabetes is nil (0%).
Participants who send their diabetic patients for dental referral are 93.3% (56), of which only after patients' concerns are 82% (46) and by themselves are just 17.8% (10) and who do not refer are 6.6% (4). Among the 93.3% (56) who refer to dentist, 71.4% (40) refer to general dentist and 28.5% (16) to specialist. The participants who enquire the patients about the dental treatment in their next visit are 23.2% (13) and the remaining 76.8% (43) does not [Table 2].
Table 2.
Referral to dentist
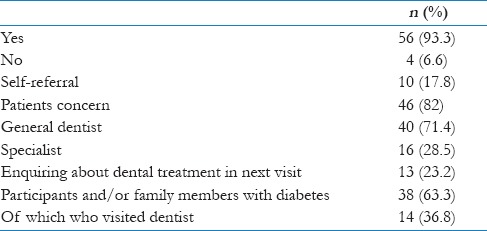
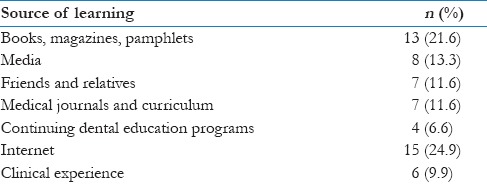
For 86.3% (52) participants, the dental clinic is situated at <1 km from their practice area. Almost 63.3% (38) of the participants and/or the family members have diabetes, of which only 36.8% (14) visited the dentist. Table 3 gives the source of information regarding dentistry. Almost 90% (54) of the practitioners showed willingness for enriching their knowledge for the better patient general well-being and preventive care.
Table 3.
Sources of information about the connection between oral health and diabetes
Discussion
In support of evidence-based care, the dental and medical professions must treat the body as a whole, realizing that interdisciplinary referrals are necessary. The World Health Organization has identified that oral health is integral to general health and is essential for general well-being. At the 101st FDI Annual World Dental Congress in 2013, a declaration was officially issued, “Oral health and general health: A call for collaborative approach.”[8] It states that, all health care providers must be aware of relationship between oral diseases and general health and they should play an important role in diagnosis and referral to dentist.
Although numerous studies have proven the bidirectional relationship between diabetes and periodontitis, it is clear from the present study that there is a lack of knowledge on this association and ill-matched situation between the scientific evidence and practice behaviors. The present study demonstrates that only 17.8% referred their patients for dental and periodontal assessment without patients' concern. This finding directs attention to an apparent need for the organized course of action to achieve a goal and interventional programs for the doctors who deal with diabetic patients. Similarly, Lin et al. 2014 noticed that only 40.4% of the diabetic patients are advised for dental referral.[8]
In the present study, all the endocrinologists (100%) were aware of the relationship and refer their diabetic patients for regular dental visits compared to general medicine practitioner and diabetologists. This finding may be because much emphasis is not given on oral health during medical education in postgraduate and undergraduate level. In support of this, Mouradian et al. 2005 observed that medical students have little knowledge on oral-systemic interactions and oral health disparities in all the training years.[10] Similarly, Lin et al. 2014 observed that endocrinologists with longer practicing years have more positive attitude toward periodontal health and DM which is possibly credited to the clinical experience which adds significance to the periodontitis and its impact on systemic health.[8] Accordingly, Al-Habashneh et al. 2010 observed that specialists are reported to advise their diabetic patients to dentists more than general practitioners.[9]
These findings put forward that more appropriate knowledge and perception of fact play a crucial role in understanding the advantage of observing dental needs for diabetic patients. Health-care providers should indulge questions on oral health along with general health, and an extra mile of effort must be put if any signs of bad breath and infection have been noticed in their mouth. The present study shows that only 23.2% (13) have enquired their patients about the dental treatment in the consequent visit which is attributed to the lack of knowledge and its importance.
The present study clearly shows the truth that only 6.6% (4) got the information regarding dentistry from continuing dental education programs and 11.6% (7) from medical journals and curriculums. Fortunately, the majority 90% (54) agreed that they should be taught about oral health, which is consistent with the previous study conducted by Owens et al. 2011[11] and Lin et al. 2014.[8] Based on these results, there is a need to develop the appropriate educational materials and workshops to enhance the knowledge of health-care providers about the association and its clinical implications. To increase the awareness about significance of dental services for diabetic patients, we propose that dental health education must be integrated into diabetes health-care programs. Ultimately, the resulting improved understanding of oral health for medical practitioners should be included as part of the diabetic patients health care.
Conclusion
Knowledge regarding the relationship between DM and periodontitis is less in diabetologists and general medicine doctors when compared to the endocrinologists. Ultimately, the enhanced knowledge on scientific evidence and its implication in practice benefits the patients for the better oral and general well-being. The findings of the present study focused on promoting the mutual collaboration and interprofessional education which is the utmost important yet neglected aspect of dental care.
Limitations
These results might not reflect the actual opinions of all the endocrinologists, general medicine practitioners, and diabetologists doctors due to small sample size. Moreover, the study was restricted to only one place and not representative of pan India. Sample size should be large enough to divide into groups and to detect significant differences for some of the outcomes between the groups and this survey should be conducted in other parts of India and the world. Another limitation being a cross-sectional study, the future change of practice behavior or persistence is not captured here.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I would like to acknowledge the participants of the study for their kind cooperation.
References
- 1.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. IDF Diabetes. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Last accessed on 2016 Dec 23]. Available from: http://www.diabetesatlas.org . [Google Scholar]
- 3.Orchard TJ, Dorman JS, Maser RE, Becker DJ, Drash AL, Ellis D, et al. Prevalence of complications in IDDM by sex and duration. Pittsburgh epidemiology of diabetes complications study II. Diabetes. 1990;39:1116–24. doi: 10.2337/diab.39.9.1116. [DOI] [PubMed] [Google Scholar]
- 4.Moore PA, Orchard T, Guggenheimer J, Weyant RJ. Diabetes and oral health promotion: A survey of disease prevention behaviors. J Am Dent Assoc. 2000;131:1333–41. doi: 10.14219/jada.archive.2000.0388. [DOI] [PubMed] [Google Scholar]
- 5.Jindal A, Parihar AS, Sood M, Singh P, Singh N. Relationship between severity of periodontal disease and control of diabetes (Glycated Hemoglobin) in patients with type 1 diabetes mellitus. J Int Oral Health. 2015;7(Suppl 2):17–20. [PMC free article] [PubMed] [Google Scholar]
- 6.Eldarrat AH. Awareness and attitude of diabetic patients about their increased risk for oral diseases. Oral Health Prev Dent. 2011;9:235–41. [PubMed] [Google Scholar]
- 7.Aggarwal A, Panat SR. Oral health behavior and HbA1c in Indian adults with type 2 diabetes. J Oral Sci. 2012;54:293–301. doi: 10.2334/josnusd.54.293. [DOI] [PubMed] [Google Scholar]
- 8.Lin H, Zhang H, Yan Y, Liu D, Zhang R, Liu Y, et al. Knowledge, awareness, and behaviors of endocrinologists and dentists for the relationship between diabetes and periodontitis. Diabetes Res Clin Pract. 2014;106:428–34. doi: 10.1016/j.diabres.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Al-Habashneh R, Barghout N, Humbert L, Khader Y, Alwaeli H. Diabetes and oral health: Doctors' knowledge, perception and practices. J Eval Clin Pract. 2010;16:976–80. doi: 10.1111/j.1365-2753.2009.01245.x. [DOI] [PubMed] [Google Scholar]
- 10.Mouradian WE, Reeves A, Kim S, Evans R, Schaad D, Marshall SG, et al. An oral health curriculum for medical students at the University of Washington. Acad Med. 2005;80:434–42. doi: 10.1097/00001888-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Owens JB, Wilder RS, Southerland JH, Buse JB, Malone RM. North Carolina internists' and endocrinologists' knowledge, opinions, and behaviors regarding periodontal disease and diabetes: Need and opportunity for interprofessional education. J Dent Educ. 2011;75:329–38. [PubMed] [Google Scholar]


