Abstract
Introduction and Objective:
The majority of formerly conducted studies have focused on the prevalence of posttraumatic stress disorder merely during pregnancy period; however, pregnancy period is by itself accompanied with the stress of getting pregnant again; therefore, the present study was conducted to evaluate the prevalence of posttraumatic stress disorder (PTSD) during pregnancy and postpartum period.
Methods:
A total of 3475 articles were found by searching keywords of PTSD, pregnancy, stress, and birth, through various research databases, including PubMed, Google Scholar, and Science Direct; 37 papers turned out to be completely relevant, 18 of which had provided through examination of the prevalence of intended disorder.
Results:
The prevalence rate varied from 0% to 21% in community-related samples; this rate varied from 0% to 43% in high-risk samples.
Conclusion:
PTSD is a common phenomenon during pregnancy and postpartum period, and it might get worse and worse unless it is diagnosed and treated after delivery. Thus, it is recommended to assess pregnancy and postpartum services.
Keywords: Postpartum, postraumatic stress disorder, pregnancy
Introduction
Posttraumatic stress disorder (PTSD) involves an individual's experience of a traumatic event that is associated with a serious risk of death, injury, or a threat to his physical, or others, physical integrity; its main symptoms, which must necessarily last for more than 1 month,[1] include a wide range of responses, including reexperiencing the event in the mind of the individual (disturbing thoughts, nightmares, and reoccurrence of the incident) and avoiding the occurrence of events and motivational reactions (irritability, anger, problem with concentration and sleep, and excessive alertness). Pregnancy and childbirth can stimulate emotions and feelings which, in turn, might developmental symptoms of harm in some women.[2] PTSD is a major concern for the health of pregnant and postpartum women; the onset of this disorder can occur during pregnancy or at birth.[3] PTSD during pregnancy can be caused by traumatic events, such as accidents, interpersonal violence, or disasters.[4] However, this disorder might get worse and worse in the other after the birth of the child because they are anxious about the possibility of the child's having been damaged or hurt. If women have a history of this disorder, they might be in trouble during pregnancy and experience more severe complications.[5] Various studies have shown that this disorder can have negative effects on women, their relationships with others, and the birth of their child.[6,7,8,9] Based on DSM-IV benchmark, the majority of studies have categorized the repercussions of PTSD into three distinct groups: (a) reexperiencing a traumatic event through nightmares, intrusive thoughts, or flashback, (b) persistent avoidance of event reminder and loss of it, and (c) increased arousal, such as hypnosis, irritability, difficulty concentration, and other emotional disturbances; one must have at least one symptom of reexperience, three avoidance symptoms, and two signs of arousal to be diagnosed with this disorder. Symptoms should cause discomfort and severe impairment in the occupational or social function of the individual.[10] The prevalence of this disorder is very high during pregnancy (0%–35%)[11,12] and postpartum period (0%–21%).[13,14] Therefore, this is a common problem, differing greatly in various studies of miscellaneous countries, in the epidemiology of mental disorder.[15] Changes in the prevalence of this disorder may be due to several factors, such as differences in sampling, measurement, and cultural contexts. Measurement differences are also important, especially in studies of full-scale or single-symptom measurements. In addition, in self-reported measurements, the prevalence rate can be estimated high since full diagnosis criteria are not exactly delineated.[16] Valid data on the prevalence of birth-related PTSD are of crucial importance. It is important to note that, clinically, the actual rate of prenatal PTSD is of great importance for raising awareness and providing interventions. Our accurate estimate of prevalence rate enables us to categorize the prevention and treatment costs well both economically and politically. It is necessary to know that the prevalence rate of PTSD is considerably high. There are three overviews that provide information about the prevalence of PTSD after birth.[17,18,19] The present study provides an overview of risk factors and possible outbreaks of PTSD after childbirth; however, there are many gaps to be scrutinized. In the first place, despite huge evidence signifying the presence of PTSD in a significant proportion of women and being associated with adverse outcomes such as preterm labor, there has been no study focusing merely on pregnancy period PTSD.[8,9] In the second place, most survey studies are based on symptom-based outbreaks. In the third place, less studies have looked at the disorder immediately after birth and before birth. Finally, review studies have not taken into account the changes that have been made over time in this disorder.
Materials and Methods
The present systematic review tried to investigate the prevalence rate and causes of PTSD during both pregnancy and postpartum period; searching was done through various databases, such as google, yahoo, science direct journal, PubMed, and Scopus, using several search terms, such as PTSD-related terminology (posttraumatic, disorder, and PTSD) and birth-related terminology (birth, pregnancy, peripartum, and postpartum), from 1998 to 2017; 3475 papers were initially found, out of which 37 papers turned out to be relevant, with 18 articles providing thorough examination of intended topic.
Results
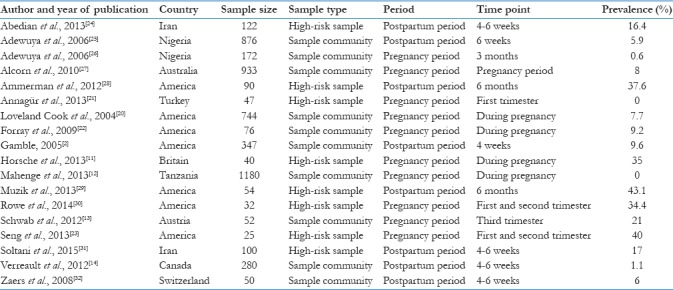
There were 18 relevant papers with desirable characteristics found in the initial overview; these studies were had been done from 1998 to 2017 and emphasized the prevalence of PTSD in pregnancy. Ten studies focused on the pregnancy, and 8 examined postpartum period; studies had been conducted in different countries. Pregnancy-oriented PTSD increases due to several factors, such as interpersonal violence,[12] history of sexual and physical abuse,[20] pregnancy-related events such as the diagnosis of embryonic anomalies,[11] or the complications of the embryonic period.[21,22,23] The results of these studies showed that the risk of PTSD varies significantly from study to study. The prevalence of PTSD varied from 0% to 40% during pregnancy; this rate turned out to be 40%[23] for women with nausea and vomiting, 35%[11] in women with anomalous embryos, and 34% in women with an adverse history of childhood education; clinical interviews showed the prevalence rate of PTSD varying from 0% to 40% and questionnaires showed this rate to be 0%–35%. This data are shown in Table 1.
Table 1.
The main features of studies on the prevalence of posttraumatic stress disorder during pregnancy and postpartum period
Discussion
The main objective of the present study was investigating the prevalence of PTSD during pregnancy and postpartum period. According to the results, the outbreak of a community sample or high-risk samples varied from 3% to 18%, with this rate being higher in the high-risk sample; this rate has been reported differently in various communities, for example, 10% in case of the USA.[33] Postpartum prevalence rate of this disorder turned out to be 4% in community and 15% in high-risk samples.[18] Although there is no significant change in the prevalence of this disorder during pregnancy and postpartum periods, the mean of the outbreak at different time points gives us an appropriate insight into the prevalence of prelabor period. According to the results of the present systematic review, postpartum prevalence mean of this disorder, sometimes, turns out to be higher than pregnancy period mean and this might be due to labor-wasting experiences that may lead to a newer state of this disorder or to aggravate it during pregnancy. Similarly, childbirth may function as a stimulus for women with a history of trauma and previous PTSD, reexperiencing the same complications again after childbirth. On the other hand, most studies did not have control over PTSD during pregnancy and could not assess the history of trauma, which may disturb the actual outbreak of PTSD after delivery. Quantitative studies of PTSD have been conducted in relation to a wide range of traumatic events; so, it is likely that the overall prevalence of PTSD outbreaks has been reduced in this review; therefore, results should be considered with caution. The analysis of the mean prevalence in the first 6 months of postpartum showed that PTSD increased in both community and high-risk samples. This pattern is also consistent with some of the longitudinal studies of PTSD before birth;[32] it is incompatible with PTSD samples other than prebirth ones, where there is a significant decrease in the first 5 months after the PTSD traumatic event.[34] This difference in postpartum PTSD in women may be due to the unique elements of the postpartum period, such as encountering a newborn and falling asleep, which might either delay or transform symptoms; this finding is supported by various evidences. Based on a huge study which was conducted in Norway, poor social support and negative events in life during the first 8 postpartum weeks are associated with the persistence of PTSD symptoms up to 2 years after childbirth.[35] In addition, birth experience trauma might reawaken previous traumatic events, thus increasing the risk in later periods of PTSD. However, analysis of PTSD course over time has been done based on a limited number of studies; so, conclusions should be made at this stage with caution. According to the findings of the present study, there were significant differences in the prevalence of PTSD based on geographical areas and the quality of the studies; the highest prevalence of PTSD has been reported in high-risk case studies. However, there are some limitations that should be considered before drawing an applicable conclusion. However, there are some limitations that should be considered before concluding. First of all, the focus on prenatal PTSD diagnosis criteria, which may cost a lot to public health, is lowered. For example, qualitative research shows that many women who do not have PTSD diagnostic criteria can still suffer from significant symptoms and can potentially benefit from treatment.[36] The second point is that it is difficult to evaluate and to compare the results and create a comprehensive picture of postpartum PTSD when examining the postpartum PTSD period. Third, there were wide variables in the prevalence rate across studies which could be due to different methodological differences, including the use of various measures for PTSD and the heterogeneity of the studied populations and geographical locations. In addition, the average prevalence of PTSD during pregnancy in high-risk individuals may be affected by special rates reported in several studies.[28,29,37]
Conclusion
The present review was conducted to determine the prevalence of PTSD in pregnancy and postpartum periods among different samples using various measures. Based on the analysis of the results of studied articles, PTSD is relatively common in pregnancy, varying from 4% to 6% among women at different times. In addition, it seems that the prevalence of PTSD increases from 1 to 6 months after delivery; thus, increasing awareness and continuous evaluation are important in this period. Finally, PTSD measurement questionnaires offer similar rates to clinical interviews; thus, despite not being golden measuring rods, these questionnaires can function as an essential step for the diagnosis of PTSD during pregnancy and postpartum periods.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Paul TA. Prevalence of posttraumatic stress symptoms after childbirth: Does ethnicity have an impact? J Perinat Educ. 2008;17:17–26. doi: 10.1624/105812408X324534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P, et al. Effectiveness of a counseling intervention after a traumatic childbirth: A randomized controlled trial. Birth. 2005;32:11–9. doi: 10.1111/j.0730-7659.2005.00340.x. [DOI] [PubMed] [Google Scholar]
- 3.Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J, et al. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384:1775–88. doi: 10.1016/S0140-6736(14)61276-9. [DOI] [PubMed] [Google Scholar]
- 4.Malak SM, Crowley MJ, Mayes LC, Rutherford HJ. Maternal anxiety and neural responses to infant faces. J Affect Disord. 2015;172:324–30. doi: 10.1016/j.jad.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 5.Halvorsen L, Nerum H, Oian P, Sørlie T. Giving birth with rape in one's past: A qualitative study. Birth. 2013;40:182–91. doi: 10.1111/birt.12054. [DOI] [PubMed] [Google Scholar]
- 6.Nicholls K, Ayers S. Childbirth-related post-traumatic stress disorder in couples: A qualitative study. Br J Health Psychol. 2007;12:491–509. doi: 10.1348/135910706X120627. [DOI] [PubMed] [Google Scholar]
- 7.Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F, et al. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch Womens Ment Health. 2013;16:453–63. doi: 10.1007/s00737-013-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw JG, Asch SM, Kimerling R, Frayne SM, Shaw KA, Phibbs CS, et al. Posttraumatic stress disorder and risk of spontaneous preterm birth. Obstet Gynecol. 2014;124:1111–9. doi: 10.1097/AOG.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 9.Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71:897–904. doi: 10.1001/jamapsychiatry.2014.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–66. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 11.Horsch A, Brooks C, Fletcher H. Maternal coping, appraisals and adjustment following diagnosis of fetal anomaly. Prenat Diagn. 2013;33:1137–45. doi: 10.1002/pd.4207. [DOI] [PubMed] [Google Scholar]
- 12.Mahenge B, Likindikoki S, Stöckl H, Mbwambo J. Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in Tanzania: A cross-sectional study. BJOG. 2013;120:940–6. doi: 10.1111/1471-0528.12185. [DOI] [PubMed] [Google Scholar]
- 13.Schwab W, Marth C, Bergant AM. Post-traumatic stress disorder post partum: The impact of birth on the prevalence of post-traumatic stress disorder (PTSD) in multiparous women. Geburtshilfe Frauenheilkd. 2012;72:56–63. doi: 10.1055/s-0031-1280408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verreault N, Da Costa D, Marchand A, Ireland K, Banack H, Dritsa M, et al. PTSD following childbirth: A prospective study of incidence and risk factors in Canadian women. J Psychosom Res. 2012;73:257–63. doi: 10.1016/j.jpsychores.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Mov Disord. 2014;29:1583–90. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- 16.Ayers S, Wright DB, Ford E. Hyperarousal symptoms after traumatic and nontraumatic births. J Reprod Infant Psychol. 2015;33:282–93. [Google Scholar]
- 17.Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS. Risk factors for developing post-traumatic stress disorder following childbirth: A systematic review. Acta Obstet Gynecol Scand. 2012;91:1261–72. doi: 10.1111/j.1600-0412.2012.01476.x. [DOI] [PubMed] [Google Scholar]
- 18.Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: A meta-analysis. Clin Psychol Rev. 2014;34:389–401. doi: 10.1016/j.cpr.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Olde E, van der Hart O, Kleber R, van Son M. Posttraumatic stress following childbirth: A review. Clin Psychol Rev. 2006;26:1–6. doi: 10.1016/j.cpr.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Loveland Cook CA, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME, et al. Posttraumatic stress disorder in pregnancy: Prevalence, risk factors, and treatment. Obstet Gynecol. 2004;103:710–7. doi: 10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- 21.Annagür BB, Tazegül A, Gündüz S. Do psychiatric disorders continue during pregnancy in women with hyperemesis gravidarum: A prospective study. Gen Hosp Psychiatry. 2013;35:492–6. doi: 10.1016/j.genhosppsych.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 22.Forray A, Mayes LC, Magriples U, Epperson CN. Prevalence of post-traumatic stress disorder in pregnant women with prior pregnancy complications. J Matern Fetal Neonatal Med. 2009;22:522–7. doi: 10.1080/14767050902801686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seng J, Miller J, Sperlich M, van de Ven CJ, Brown S, Carter CS, et al. Exploring dissociation and oxytocin as pathways between trauma exposure and trauma-related hyperemesis gravidarum: A test-of-concept pilot. J Trauma Dissociation. 2013;14:40–55. doi: 10.1080/15299732.2012.694594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abedian Z, Soltani N, Mokhber N, Esmaeily H. Comparing post-traumatic stress disorder (PTSD) in primiparous and multiparous women with preeclampsia. J Midwifery Reprod Health. 2013;1:13–8. [Google Scholar]
- 25.Adewuya AO, Ola BA, Aloba OO, Mapayi BM. Anxiety disorders among Nigerian women in late pregnancy: A controlled study. Arch Womens Ment Health. 2006;9:325–8. doi: 10.1007/s00737-006-0157-5. [DOI] [PubMed] [Google Scholar]
- 26.Adewuya AO, Ologun YA, Ibigbami OS. Post-traumatic stress disorder after childbirth in Nigerian women: Prevalence and risk factors. BJOG. 2006;113:284–8. doi: 10.1111/j.1471-0528.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 27.Alcorn KL, O'Donovan A, Patrick JC, Creedy D, Devilly GJ. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol Med. 2010;40:1849–59. doi: 10.1017/S0033291709992224. [DOI] [PubMed] [Google Scholar]
- 28.Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB. PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:186–95. doi: 10.1037/a0023062. http://dx.doi.org/10.1037/a0023062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muzik M, Bocknek EL, Broderick A, Richardson P, Rosenblum KL, Thelen K, et al. Mother-infant bonding impairment across the first 6 months postpartum: The primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health. 2013;16:29–38. doi: 10.1007/s00737-012-0312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rowe H, Sperlich M, Cameron H, Seng J. A quasi-experimental outcomes analysis of a psychoeducation intervention for pregnant women with abuse-related posttraumatic stress. J Obstet Gynecol Neonatal Nurs. 2014;43:282–93. doi: 10.1111/1552-6909.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soltani N, Abedian Z, Mokhber N, Esmaily H. The association of family support after childbirth with posttraumatic stress disorder in women with preeclampsia. Iran Red Crescent Med J. 2015;17:e17865. doi: 10.5812/ircmj.17865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zaers S, Waschke M, Ehlert U. Depressive symptoms and symptoms of post-traumatic stress disorder in women after childbirth. J Psychosom Obstet Gynaecol. 2008;29:61–71. doi: 10.1080/01674820701804324. [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. 2007;3:137–58. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- 34.Morina N, Wicherts JM, Lobbrecht J, Priebe S. Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clin Psychol Rev. 2014;34:249–55. doi: 10.1016/j.cpr.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 35.Garthus-Niegel S, Ayers S, von Soest T, Torgersen L, Eberhard-Gran M. Maintaining factors of posttraumatic stress symptoms following childbirth: A population-based, two-year follow-up study. J Affect Disord. 2015;172:146–52. doi: 10.1016/j.jad.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 36.Ayers S, Ford E. Post-traumatic stress during pregnancy and the postpartum period. In: Wenzel A, editor. Oxford Handbook of Perinatal Psychology. Oxford University Press; 2014. [Google Scholar]
- 37.Horsch A, Jacobs I, McKenzie-McHarg K. Cognitive predictors and risk factors of PTSD following stillbirth: A short-term longitudinal study. J Trauma Stress. 2015;28:110–7. doi: 10.1002/jts.21997. [DOI] [PubMed] [Google Scholar]


