Abstract
Eruptive xanthomatosis is described as the sudden eruption of erythematous yellow papules in the presence of hypertriglyceridemia, often associated with serum triglyceride levels above 2000 mg/dl. Severe hypertriglyceridemia can be caused by primary genetic mutations, secondary chronic diseases, or a combination of both. Uncontrolled diabetes mellitus is a known risk factor. It is imperative for physicians to be aware of eruptive xanthomatosis as a warning sign for severe hypertriglyceridemia due to the underlying risk for the potentially fatal complication of acute pancreatitis. Herein, we discuss a case of a 52-year-old man with uncontrolled diabetes mellitus who presented with eruptive xanthomata and a triglyceride level of 7157 mg/dl, the highest recorded value in the absence of acute pancreatitis, with a remarkable response to drug therapy. A review of the literature is included to discuss the clinical relevance and appropriate treatment of this disease entity.
Keywords: Acute pancreatitis, eruptive xanthoma, fenofibrate, hyperlipoproteinemia, hypertriglyceridemia, icosapent ethyl, low-density lipoprotein receptor, molluscum contagiosum
Introduction
It is crucial for clinicians to recognize eruptive xanthomata as a clinical sign for underlying hypertriglyceridemia. Prompt workup and treatment of severe hypertriglyceridemia are necessary to reduce the immediate risk for acute pancreatitis and long-term development of cardiovascular disease. Eruptive xanthomata are described as 1–4 mm erythematous, yellow papules that localize to the elbows, posterior thighs, lumbar region, and buttocks.[1] Eruptive xanthomata develop almost exclusively in the presence of hypertriglyceridemia and have an estimated prevalence of 18 cases in 100,000 people, making it a rare finding.[1] The case herein describes a patient who presented with eruptive xanthomata who was subsequently found to have a fasting serum triglyceride level of 7157 mg/dl with no history of acute pancreatitis. This is one of the highest documented serum triglyceride levels ever recorded and the only case of this level to occur in the absence of acute pancreatitis.
Case Report
A 52-year-old male first presented to an outpatient clinic with a 3-month history of malaise, excess thirst, and calf muscle aches. He has a history of poorly controlled noninsulin dependent diabetes mellitus and esophageal reflux. He is sexually active with one female partner. Vital signs were within normal limits, and his body mass index was 29.8 kg/m2. Physical examination revealed multiple, nodular/firm pearly-yellow papules distributed bilaterally on the skin of the anterior thighs and on the right elbow [Figure 1]. During routine phlebotomy, the patient's blood appeared lipemic with a thick, milky supernatant [Figure 2].
Figure 1.

Crops of small, red-yellow dome-shaped papules of approx. 6 mm with well-defined borders located on the anterior medial thigh
Figure 2.

Appearance of venous blood following phlebotomy, exhibiting a thick, milky supernatant
Laboratory results revealed elevated levels of triglycerides (7157 mg/dl), elevated fasting glucose (300 mg/dl), and an elevated hemoglobin A1c (11.0%). A shave biopsy of the skin lesions revealed the collections of lipid-laden histiocytes and areas of extracellular lipid deposition, including cholesterol clefts, consistent with a diagnosis of eruptive xanthomatosis [Figures 3 and 4]. Additional stains and cultures for infectious organisms were all negative.
Figure 3.
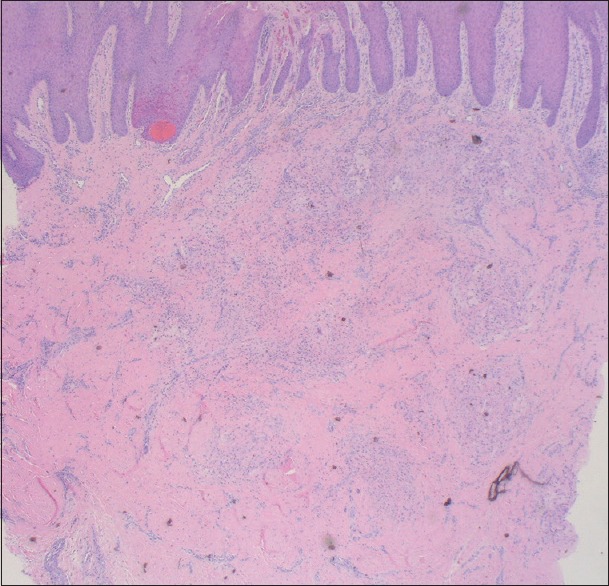
Biopsy photo showing changes of lichen simplex chronicus above collections of lipid-laden histiocytes and areas of extracellular lipid deposition, including cholesterol clefts. (H and E, ×20)
Figure 4.
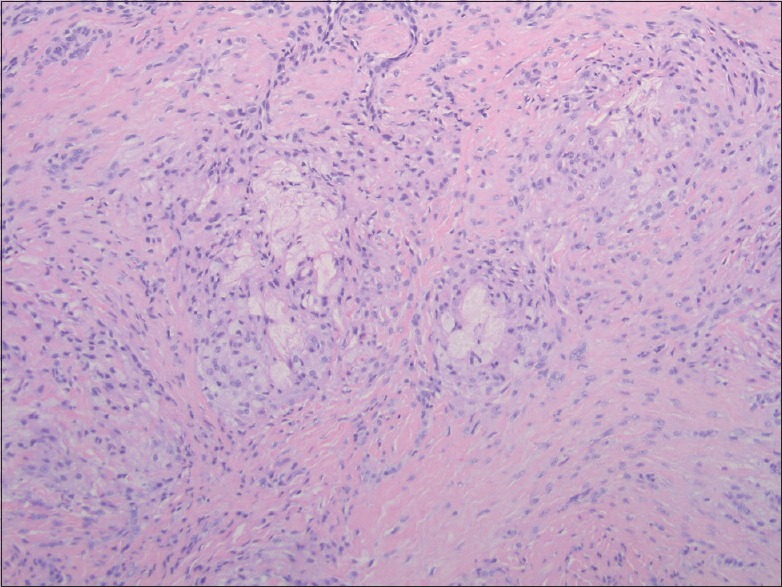
Within the dermis, there are somewhat nodular collections of lipid-laden histiocytes highlighted by a CD68 stain. Areas of extracellular lipid deposition are also seen including cholesterol clefts. (H and E, ×100)
The patient was started on a daily dose of fenofibrate 145 mg and an omega-3-fatty acid derivative, icosapent ethyl 1 g, for the treatment of severe hypertriglyceridemia. The patient was also started on metformin 1000 mg and linagliptin 5 mg daily. The patient was instructed to undergo lifestyle modifications to further control his lipid levels. He was also advised to report to the emergency department if he experiences a sudden onset of abdominal pain, concerning for acute pancreatitis.
Overall, the patient demonstrated an excellent response to therapy. The patient's triglyceride levels at 1 week, 9 weeks, and 5 months after initiating treatment were 2785, 145, and 124, respectively. His blood glucose was also better controlled 9 weeks after optimizing his diabetes medications, reducing his hemoglobin A1c to 6.7%. The eruptive xanthomata resolved completely after several months and he continues to be evaluated for routine follow-up care.
Discussion
The diagnosis and management of hypertriglyceridemia are a challenge for physicians due to its complex etiology and classification. The National Cholesterol Education Program Adult Treatment Panel III classifies serum triglyceride levels into four categories: normal, <150 mg/dl; borderline high, 150–199 mg/dl; high, 200–499 mg/dl; and very high, >500 mg/dl. These values are based on large prospective observational studies.[2]
The Fredrickson classification has been historically used to define the different phenotypes of hyperlipoproteinemia. This classification is based on the fractions of lipoproteins separated by agarose gel electrophoresis. Each phenotype was previously thought to be due to specific genetic differences. However, in the postgenomic era, evidence has shown this is typically not the case. Even though 80% of patients with familial hypercholesterolemia (Type 2A by Fredrickson classification) express a known monogenic variant in LDLR, a gene that encodes the low-density lipoprotein receptor, 95% of all patients presenting with hypertriglyceridemia have a more complex, multigenic component.[3] The combination of rare large-effect variants and common small-effect variants determines a patient's susceptibility for hypertriglyceridemia, especially in the presence of secondary causes.
Factors that increase the risk or severity of hypertriglyceridemia include obesity, uncontrolled diabetes mellitus, alcohol use, hepatosteatosis, renal disease, hypothyroidism, pregnancy, and certain types of medications.[3] Hypertriglyceridemia in the presence of one of these factors is defined as secondary hypertriglyceridemia even though a genetic susceptibility component is likely to be present. In our case, the patient presented with severe hypertriglyceridemia in the presence of uncontrolled diabetes mellitus. By applying the Fredrickson classification, the patient in this case likely has Type 5 mixed hypertriglyceridemia due to the adult presentation of severe hypertriglyceridemia in the presence of secondary causes.[3]
High levels of circulating triglycerides lead to a progression of signs and symptoms due to the abnormal deposition in various body tissues.[4] Most patients may be asymptomatic; however, classic symptoms includes recurrent abdominal pain, nausea, vomiting, irritability, and lack of concentration. Accumulation of triglycerides in the retina results in lipemia retinalis, referring to the creamy appearance of blood vessels observed during fundoscopic examination. Deposits in the skin lead to eruptive xanthomata, commonly localized to the extensor surfaces of the extremities and buttocks.[1] Accumulation of triglycerides in the liver can lead to hepatosplenomegaly as well. The appearance of blood samples in patients with severe hypertriglyceridemia is perhaps the most notable clinical finding. On initiating phlebotomy, the blood will appear lactescent. By undergoing the “refrigerator test”, blood samples kept under cool temperatures will result in the separation of chylomicrons (the lipoprotein with the highest concentration of triglycerides) as a milky supernatant.[4]
Hypertriglyceridemia is the leading cause of acute pancreatitis, behind alcohol, and gallstones, accounting for 10% of total cases. Patients with severe hypertriglyceridemia have a 15%–20% lifetime risk of acute pancreatitis. In these patients, acute pancreatitis is associated with greater severity and higher complication rates.[5] The mechanism behind the increased risk for acute pancreatitis involves lipolysis of chylomicrons in the pancreatic capillaries by pancreatic lipase, forming high local concentrations of free fatty acids causing direct cytotoxicity to acinar cells.[5] Increased blood viscosity in the pancreas may also lead to microthrombi and ischemia correlating with the high frequency of necrotic pancreatitis in these patients. The overall mortality rate of acute pancreatitis is 3.8%; however, severe acute pancreatitis has been reported to be as high as 20%.[6] In the case herein, the patient had a remarkable triglyceride level of 7157 mg/dl, placing him at an exceptionally high risk for acute pancreatitis.
The management of severe hypertriglyceridemia is based on both pharmacologic treatment and lifestyle modifications. Because hypertriglyceridemia increases the risk for acute pancreatitis, aggressive therapy should be started immediately. Fibrates are the first-line therapy due to their ability to reduce serum triglyceride levels by up to 40%. Nicotinic acid, bile acid sequestrants, and omega-3 fatty acids have also shown to be effective.[3] If acute pancreatitis is suspected in the presence of severe hypertriglyceridemia, plasmapheresis can provide rapid correction of triglyceride levels.[5] Possible secondary causes of hypertriglyceridemia should be screened and managed appropriately. Several reported cases of undiagnosed diabetes mellitus first presented as hypertriglyceridemia.[7,8,9] Once the triglyceride levels have been controlled, lifestyle modifications can be implemented to reduce premature atherosclerosis. Modifications include weight reduction, aerobic exercise, strict low-fat diet with avoidance of simple carbohydrates, and alcohol.[3] The clinical features of hypertriglyceridemia, including eruptive xanthomata, typically resolve after the correction of triglyceride levels.
In summary, timely diagnosis of eruptive xanthomata is crucial because it is often a cutaneous manifestation of underlying severe hypertriglyceridemia, which is associated with an increased risk for acute pancreatitis. The case herein provides an example of severe hypertriglyceridemia exacerbated by uncontrolled diabetes mellitus presenting as eruptive xanthomata, with a subsequent excellent response to pharmacologic therapy and complete resolution of symptoms.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We wish to acknowledge A. Caresse Gamret for the critical review of the manuscript and Dr. Sudeep Gaudi for providing histopathology imagery and analysis.
References
- 1.Zak A, Zeman M, Slaby A, Vecka M. Xanthomas: Clinical and pathophysiological relations. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158:181–8. doi: 10.5507/bp.2014.016. [DOI] [PubMed] [Google Scholar]
- 2.Berglund L, Brunzell JD, Goldberg AC, Goldberg IJ, Stalenhoef A. Treatment options for hypertriglyceridemia: From risk reduction to pancreatitis. Best Pract Res Clin Endocrinol Metab. 2014;28:423–37. doi: 10.1016/j.beem.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hegele RA, Ginsberg HN, Chapman MJ, Nordestgaard BG, Kuivenhoven JA, Averna M, et al. The polygenic nature of hypertriglyceridaemia: Implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2:655–66. doi: 10.1016/S2213-8587(13)70191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stroes E, Moulin P, Parhofer KG, Rebours V, Löhr JM, Averna M, et al. Diagnostic algorithm for familial chylomicronemia syndrome. Atheroscler Suppl. 2017;23:1–7. doi: 10.1016/j.atherosclerosissup.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Valdivielso P, Ramírez-Bueno A, Ewald N. Current knowledge of hypertriglyceridemic pancreatitis. Eur J Intern Med. 2014;25:689–94. doi: 10.1016/j.ejim.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Fu CY, Yeh CN, Hsu JT, Jan YY, Hwang TL. Timing of mortality in severe acute pancreatitis: Experience from 643 patients. World J Gastroenterol. 2007;13:1966–9. doi: 10.3748/wjg.v13.i13.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ladizinski B, Lee KC. Eruptive xanthomas in a patient with severe hypertriglyceridemia and type 2 diabetes. CMAJ. 2013;185:1600. doi: 10.1503/cmaj.130148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singla AA, Ting F, Singla A. Acute pancreatitis secondary to diabetic ketoacidosis induced hypertriglyceridemia in a young adult with undiagnosed type 2 diabetes. JOP. 2015;16:201–4. doi: 10.6092/1590-8577/2961. [DOI] [PubMed] [Google Scholar]
- 9.Solak B, Kara RO, Acikgoz SB, Kosem M. First and only symptom of undiagnosed diabetes mellitus: Eruptive xanthoma. BMJ Case Rep. 2015;2015:bcr2015212160. doi: 10.1136/bcr-2015-212160. [DOI] [PMC free article] [PubMed] [Google Scholar]


