Abstract
Objective:
To determine pattern of health care utilization and extent of out-of-pocket healthcare expenditure in rural areas of Punjab in India.
Methods:
Using multi stage sampling procedure, 660 participants were selected from 110 villages, out of all 22 districts; 440 participants had utilized outpatient care in past 15 days, and 220 had been hospitalized in past one year. Pretested semistructured questionnaires were used to enquire about household and healthcare expenditures. Out-of-pocket (OoP) expenditure included only direct costs of healthcare. Sevety seven 77 (12%) participants could not provide expenditures, hence were excluded from analysis. More than 10% of total household expenditure on healthcare was considered catastrophic.
Results:
Majority of the participants had used public sector health facilities for outpatient (57%) and inpatient (51.5%) care. Public sector facilities were utilized more often for communicable diseases and gynaecological problems whereas private sector services were used more commonly for accidents and non-communicable diseases. Mean healthcare expenditure on outpatient and inpatient healthcare services was Indian Rupees (INR) 8501 and INR 53889 respectively. Expenditure in private sector was significantly higher compared to the public sector facilities. Catastrophic expenditure was incurred by 7% of the households while seeking outpatient care and by 53% while seeking inpatient care. To pay for outpatient and inpatient care, 23.3% and 61.5% of the participants respectively had to borrow money or sell their assets.
Conclusions:
Healthcare expenditure places households under considerable financial strain in rural areas of Punjab in India. Improvements of public hospitals may increase their utilization and decrease financial burden.
Keywords: Cost, financing, health-care service, out-of-pocket expenditures, quality
Introduction
India's health system is a mix of public and private health-care providers. Public health-care system is funded through general taxation or public sector health insurance, whereas private health care is paid for through out-of-pocket (OoP) expenditure or through private health insurance. Direct OoP expenditure accounted for 89% of the private expenditures and 60% of the country's expenditures on health in 2012.[1] With India's annual per capita gross national income at a low of 1570 USD (INR 102850),[2] OoP expenditure forms a barrier to health-care access and brings poorer sections under considerable financial strain. It is estimated that nearly 6% Indians fall below poverty line (BPL) due to expenses incurred for health care.[3,4,5] Reduction of health-care expenditure-induced poverty has been advocated as a key goal of health system financing reforms.[6]
The three-tiered public sector health-care system in India got strengthened after India became a signatory to the “Health for All” declaration of Alma Ata in 1978.[7] With rapid demographic and epidemiologic transition, the Government of India has now initiated next step of reforms under universal health care (UHC). Goal of UHC is to ensure availability of promotive, preventive, curative, rehabilitative, and palliative health-care services to all citizens without undue financial hardship with a focus on equity, increasing coverage of interventions and financial risk protection. A High-Level Expert Group on UHC constituted by Planning Commission of India in 2010 with a mandate to develop framework for achieving affordable and acceptable health care for all Indians opined that the government should be “guarantor and enabler, although not necessarily the only provider of health and related services” for achieving UHC in India.[8]
Knowledge of patterns of illness, health-care seeking, expenditures on health care, and effects of health-care expenditure on households is required for carrying out health-care financing reforms which form the basis of providing UHC.
This study was carried out to ascertain the health-care seeking patterns and expenditure incurred by households on outpatient and inpatient health care in rural Punjab, India.
Materials and Methods
Punjab is a North Indian state with area of 50,362 km2 and population of about 27.7 million. Punjab has 22 districts, 141 towns and cities, and 12673 villages. The literacy rate is 80.5% in males and 62.5% in females. About 38% of the population live in urban areas.[9] About 55% of the rural households have a pucca dwelling. Scheduled castes constitute about 37% of the households, and 17% belong to other backward classes.[10] The state had per capita income of INR.78,171 (USD 1193) as on 2011–2012.[11] In 2004, average expenditure on hospitalization in Punjab was INR 12,132 (USD 183.5) compared to the all India average of INR 5,695 (USD 86.15).[12]
Using multistage random sampling, 660 participants were included in the study. In the first stage, one community health center and one primary health center were randomly selected from the health centers in each of the 22 districts of Punjab. In the second stage, five villages were randomly selected from the catchment area of the so-selected health centers. In the third stage, a house-to-house enquiry was carried out starting from center of the each selected village till 4 persons who had illness during previous 15 days and 2 persons who were hospitalized in the past 1 year were identified. Thus, 220 hospitalization cases and 440 outpatients were recruited. The sample size was purposively decided based on experience from surveys in other states. Using the final sample size achieved, power was calculated based on mean and standard deviations for the hospitalized persons and those with acute illness, using moderate design effect and alpha error of 0.05. A power of >0.95 was achieved in both the subsamples.
A study was approved by the Institutional Ethics Committee. Informed written consent was obtained from the participants before recruitment. Pretested, structured questionnaires were used to collect data at the household level. Data analysis was done using Epi Info software.
Total household expenditure was calculated by adding expenditures for each item consumed during the past 1 month or year for annual expenditures such as purchase of vehicle or payment of education fee. Place of seeking health care was classified as public health facility which included institutions set up by government through taxpayer funds or as private health-care facilities which included all nongovernment establishments (for-profit and not-for-profit) and also care sought at home from private qualified/unqualified practitioners.
Expenditures on health care were enquired under different expenditure heads, for example, hospital charges, medicine, doctor's/nursing staff fee, diagnostics, transportation, and boarding/lodging for relatives who accompanied the patient. However, in most instances, patient was given a consolidated bill, especially for hospitalized persons. Details were available only in cases where medications or diagnostic tests had to be procured from a different health-care establishment than where patient was being treated. However, total expenditure incurred on illness episode was vividly recalled in most cases. Seventy-seven (12%) participants who could not provide details of expenditures were excluded from analysis. Catastrophic expenditure on health care was defined as more than 10% of total household expenditures. This was preferred as residents in rural areas where agriculture is the main occupation found it difficult to list out the details of food and nonfood expenditure separately. Conventionally, health-care expenditure of 40% or more, out of the nonfood expenditure, is considered as catastrophic expenditure.[13]
Households were classified into quintiles based on monthly household consumption expenditure with 1st quintile representing households with highest and 5th quintile representing households with lowest monthly consumption expenditure. Impoverishment status of households was assessed by enquiring about enrollment in public distribution system for rations and other commodities or those categorized as BPL by government to enable access to essential commodities at subsidized rates. The current poverty line for rural India is income less than INR 32 (USD 0.49) per day per capita (INR 11680 [USD 178.35] per capita annually).[11] Chi-square test for trend was used to test statistical association.
Results
Out of 660 participants, most (70%) were in the age group of 15–60 years, 64% were females, 68% belonged to backward class, and 21% were BPL. Forty-five percent of the heads of household were daily wage laborers and 33.4% were illiterate.
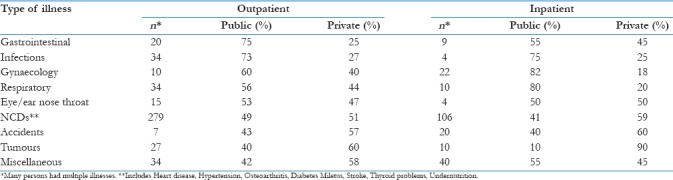
About half (53.9%) of the participants had utilized public health facilities; 56.5% for outpatient and 48.4% for inpatient care. Among the BPL group, 50.6% had sought treatment in public health facilities for outpatient and 51.3% for inpatient health care. Private facilities were utilized more often for health care related to accidents and noncommunicable diseases (NCDs) whereas public facilities were commonly used for infections, gastrointestinal obstetrics, and gynecological and respiratory problems [Table 1].
Table 1.
Place of seeking healthcare according to the type of illness
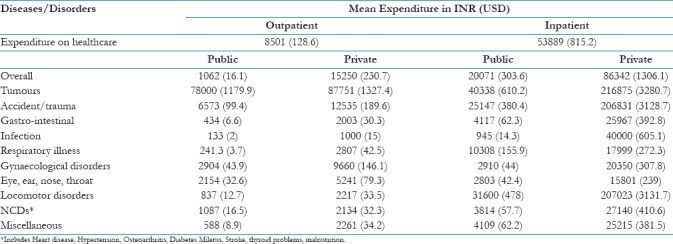
Mean OoP expenditure for inpatient and outpatient care was INR 53889 (USD 815.2) and INR 8501 (USD 128.6) per episode, respectively. The OoP expenditure for inpatient and outpatient care was 4 times to 15 times higher, in private facilities compared to the public facilities for almost all diseases [Table 2].
Table 2.
Mean expenditure incurred on health care in various disease categories
Outpatient services were mostly paid for through current income (72.9%). However, 21% had to arrange for money from borrowings, and nearly 4.9% resorted to other measures such as sale of household items and insurance. For inpatient services, more than half the households (61.5%) had to borrow money.
In outpatient consultations, catastrophic expenditure was incurred by 28 (7%) of the households. Eighteen of these needed outpatient care for tumors (10), NCDs (7), and accidents (1). Fifteen had sought health care from private sector.
The mean expenditure on outpatient care increased from the poorest to the richest quintile, and a higher proportion of poorer households had to bear catastrophic expenditure although the increase was not statistically significant. In poorer quintiles, a higher proportion of households had to borrow money to bear health-care expenses. In richer households, significantly higher proportion of participants had sought outpatient care for NCDs. Annual household consumption expenditure did not bear a significant association with catastrophic expenditure among the different quintiles [Table 3].
Table 3.
Expenditure patterns on inpatient and outpatient healthcare according to annual household expenditure quintiles
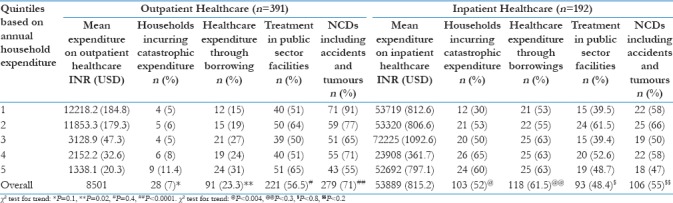
For inpatient care, catastrophic expenditure was incurred in 103 (57%) households. Accidents (17), tumors (10), NCDs (35), gynecological disorders (13), and other undiagnosed/unclassified illnesses (26) were the major causes contributing to catastrophic expenditure. Nearly 63% (65) had sought inpatient care from private sector. Significantly higher proportion of poorer households incurred catastrophic expenditure. Household consumption expenditure quintiles did not bear association with type of health facility used, the need to borrow money, or whether treatment was sought for NCDs [Table 3].
Affordability was a prominent reason for seeking inpatient (30%) and outpatient health care (21%) in public facilities. Free drug availability (20%) was another major reason for seeking health care in public health facility. Referral was a common reason cited for seeking inpatient (43.6%) and outpatient (39%) services in private facilities. Overall, referral was an important reason for seeking care in a particular type of health facility.
Discussion
Utilization of public facilities has increased for inpatient as well as for outpatient health care, compared to the findings of National Sample Survey Organization (NSSO), 2004, for rural Punjab. The OoP expenditure and percentage of families incurring catastrophic expenditure have also increased since 2004.[12] OoP expenditure in our study was much lower in public health facilities than private facilities.
Historically, public health-care services have been underutilized in India. Private sector is utilized more often for outpatient, and public sector is used more commonly for hospitalization/inpatient health care.[12] The National Council for Applied and Economic Research had reported that 60% of people in urban and 62% in rural areas of India had utilized public health facilities for hospitalization in 1987. Corresponding figures in Punjab were 67.2% and 95%, respectively. Similar pattern was seen in all other states, except in Tamil Nadu, Gujarat, Maharashtra, and Andhra Pradesh. Overall, utilization of public health facilities for hospitalization was higher in urban areas.[14]
The use of public health system for outpatient care has remained stable over the past 30 years; 21% in 1986 (NSSO 42nd round),[15] 19% in 1995 (NSSO 52nd round),[16] and 22% in 2004–2005 (NSSO 60th round).[13] However, the proportion of inpatient care provided by public sector has reduced from 60% in 1986–1987 (NSSO 42nd round) to 42% in 2004–2005 (NSSO, 60th round). A recent study in rural Odisha also showed that public health-care facilities were preferred for hospitalizations, and nearly, 50% participants accessed public facility for outpatient care also.[17] In our study, 57% of participants had sought outpatient care and 48.4% had sought inpatient care from public facilities, respectively.
Rates of seeking health care from public sector between respondents from different quintiles of household consumption expenditure were similar. This finding varies with the earlier reports of NSSO 42nd, 52nd, and 60th rounds where the richer segments of the population were found to be using public health system more. A study in the 1990s reported that although in numbers, poorer people access public system more, it is the richer segments who get most benefit from subsidies offered through the public health-care system.[18] Recent studies have reported findings similar to our study that the poor and the rich use the public health system equally, and lately, the pro-poor utilization patterns have been seen at least in the outpatient care seeking.[19] Possibility of not seeking inpatient care due to cost factor in the poorer quintiles cannot be ruled since OoP cost of hospitalization was quite high even in public health-care facilities. Financial constraints as a reason for not seeking health care have been cited repeatedly in all the three NSSO reports on health expenditure (42nd round, 52nd round, and 60th round).
Utilization of private sector was observed more often in diseases such as cancers, accidents, heart disease, and other NCDs. People use public sector for communicable diseases, obstetrics, and gynecology-related needs. This may reflect the fact that despite epidemiologic transition, public health system has not re-oriented itself to address needs arising due to NCDs. In the absence of growth of public sector, private health sector has mushroomed rapidly, though in an unregulated manner, to meet the growing needs for NCDs.[20] Public system is poorly equipped to meet health-care needs arising out of injury and NCD epidemics.[21] Need to strengthen the public system to meet health-care needs due to NCDs has been advocated by other observers as well.[22]
Other reasons for choosing private sector in our study were availability of better infrastructure, quality care, convenient timings, and referral by health-care providers. Availability of better infrastructure and better reputation of doctors was mentioned as reasons for seeking care in the private sector in NSSO 2004 as well.[12] Public sector was perceived as technically competent but inconvenient and provider centered, with complex systems that took time and effort to negotiate.[23] Other studies in India report that patients were seen for longer durations, were more likely to have a physical examination during visit, and diagnosis explained by private sector physicians compared to public sector.[24]
Public facilities are preferred due to availability of qualified health-care personnel and availability of free drugs as shown in our study. The need to improve drug availability in the public system for increasing the utilization of health-care services has been stressed. Prinja et al. have suggested that it is possible to provide drugs at 40% less cost if generic drugs are made available.[25] Hence, shifting to generic drugs can compensate for the rising cost of government expenditure on strengthening of health system.
Consumption expenditure of households was based on recall by household members. Such methods usually underestimate the expenditure. However, these have been found useful in relative ranking of households according the consumption expenditure to examine the pro-poor/pro-rich concentration of illness, health-seeking behavior, spending capacity of households, and potential impoverishment due to expenditure on health care.[26]
In India, mean monthly household consumption expenditure reported by NSSO in 2004 was INR 6724 (USD 101.7) and mean monthly OoP expenditure on health care was INR 854 (USD 12.9), respectively. Health OoP expenditure was 13% of the total household expenditures.[13] In our study, mean monthly household expenditure was INR 8214 (USD 124.3) and mean health expenditure on outpatient and inpatient services was INR 8501 (USD 128.6) and INR 53889 (USD 815.2), respectively. The highest expenditures were for the treatment of tumors in outpatient and for accidents in the inpatient care. Most (71%) of the outpatient and 55% of inpatient consultations were for NCDs. Other studies from India have also found that NCDs are a great burden on the Indian rural people who are more likely to incur catastrophic expenditure.[27,28] In a study in 2012, NCDs accounted for 20% of all diseases in Odisha and 30% in Bihar. Digestive and musculoskeletal problems contributed most to the expenditures followed by cardiovascular and neuropsychiatric conditions. In the inpatient category, expenditure on digestive and cardiovascular diseases was highest.[29]
NSSO 2004 report states that nearly 73% of health financing is through current income.[13] Peters reported that 40% of hospitalized patients in India had to sell assets or borrow money to pay for hospital costs.[30] Duggal found that among the poorest quintile in India, the percentage of participants who had to pay from savings or borrowings was 50%.[31] In rural Odisha, about 25% of households reported hardship financing health care, and among households facing hospitalization, 40% reported hardship.[17] In our study, catastrophic expenditure was more often borne by households in poorer quintiles. About, 23.3% of outpatient and 59% of the inpatient health-care expenditures were financed through borrowings or from other sources such as sale of assets suggesting financial hardship in meeting health expenses. Need to borrow even for outpatient health care was higher in the poorer household expenditure quintiles.
There is inter-state variation in the disease pattern and related OoP expenditures. In rural Punjab, 67% of increases in poverty were estimated to be due to OoP expenditure. OoP expenditure payments vary in accordance with ability to pay and tend to increase with increase in consumption expenditure.[32]
In this study, we find that most respondents who sought health care were in the age group of 15–60 years. This is in variance with the earlier reports by NSSO 2004 where most of the illness was found in the older age groups.[13] However, since we interviewed only the households who had sought care and did not conduct a community-based morbidity survey, the rates of illness and the unmet need for health care could not be estimated.
Limitations
Many studies have reported that expenditure on outpatient treatment was significantly more as it was accessed more often compared to the hospitalizations. In our study, the expenditure on outpatient and inpatient services were calculated per episode; hence, epidemiological data on number of outpatient and inpatient consultations in a given population will be needed to compute total cost of health care. Details of the expenditure could not be reported by all study participants due to which components of direct expenditure could not be computed accurately in the study. Furthermore, indirect cost measures have not been accounted for while analyzing for the health expenditure.
Conclusions
Utilization of public health facilities has shown an increase in recent times. However, rising health-care costs continue to cause a significant burden on households. In spite of having higher GDP, proportion of households having catastrophic expenditure remains almost at the same levels in Punjab as reported in other parts of the country. OoP expenditure on health care may possibly be brought down by strengthening public health facilities.
Financial support and sponsorship
National Health Mission, Punjab.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organisation. World Health Statistics 2015. Geneva, Switzerland: World Health Organisation; 2015. [Last accessed on 2016 Nov 11]. Available from: http://www.apps.who.int/iris/bitstream/10665/170250/1/9789240694439_eng.pdf?ua=1 . [Google Scholar]
- 2.World Bank. World Bank group. 2015. [Last accessed on 2015 Nov 10]. Available from: http://www.data.worldbank.org/indicator/NY.GDP.PCAP.CD .
- 3.Thakur J, Prinja S, Garg CC, Mendis S, Menabde N. Social and economic implications of noncommunicable diseases in India. Indian J Community Med. 2011;36:S13–22. doi: 10.4103/0970-0218.94704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Health Accounts Cell: National Health Accounts India 2004-05. New Delhi: Ministry of Health and Family Welfare, Government of India; 2009. [Last accessed on 2015 Mar 26]. Available from: http://www.planningcommission.nic.in/reports/genrep/health/National_Health_Account_04_05.pdf . [Google Scholar]
- 5.Berman P, Ahuja R, Bhandari L. The impoverishing effect of healthcare payments in India: New methodology and findings. Econ Polit Wkly. 2010;45:65–71. [Google Scholar]
- 6.Everybody's Business – Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: World Health Organization Press; 2007. [Last accessed on 2016 Nov 11]. Available from: http://www.who.int/healthsystems/strategy/everybodys_business.pdf . [Google Scholar]
- 7.Declaration of Alma-Alta: International Conference on Primary Health Care, Alma-Alta, USSR, World Health Organization. 1978. Sep 6-12, [Last accessed on 2015 May 24]. Available from: http://www.who.int/publications/almaata_declaration_en.pdf .
- 8.High Level Expert Group Report on Universal Health Coverage for India. India: Planning Commission of India; 2011. [Last accessed on 2015 Mar 26]. Available from: http://www.planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf . [Google Scholar]
- 9.Census of India. 2011. [Last accessed on 2015 May 15]. Available from: http://www.censusindia.gov.in/pca/default.aspx .
- 10.District Level Household and Facility Survey 2007-08, Punjab. International Institute of Population Sciences. 2010. [Last accessed on 2015 May 15]. Available from: http://www.rchiips.org/pdf/rch3/report/pj.pdf .
- 11.State Wise Population, GDSP, Per Capita Income and Growth Rate. [Last accessed on 2015 Nov 01]. Available from: http://www.pbplanning.gov.in/pdf/Statewise%20GSDP%20PCI%20and%20G.R.pdf.
- 12.National Sample Survey Organisation (NSSO). Morbidity, Health Care and Condition of the Aged. New Delhi: Ministry of Statistics and Program Implementation, Government of India; 2006. [Google Scholar]
- 13.Xu K, Klavus J, Kawabata K, Evans DB, Hanvoravongchai P, Ortiz de Iturbide JP, et al. Household health system contributions and capacity to pay: Definitional, empirical and technical challenges. In: Murray CJL, Evans DB, editors. Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva: World Health Organization; 2003. [Google Scholar]
- 14.National Council for Applied Economic Research. Household Survey of Healthcare Utilization and Expenditure. Working Paper No. 53. New Delhi. 1995. [Last accessed on 2015 Nov 11]. Available from: http://www.file:///C:/Users/User/Downloads/1382095761WP53.pdf .
- 15.National Sample Survey Organisation. Utilization of Medical Services. Department of Statistics. New Delhi: Government of India; 1986-1987. [Google Scholar]
- 16.National Sample Survey Organisation. Morbidity and Treatment of Ailments. Department of Statistics. New Delhi: Government of India; 1995. [Google Scholar]
- 17.Binnendijk E, Koren R, Dror DM. Hardship financing of healthcare among rural poor in Orissa, India. BMC Health Serv Res. 2012;12:23. doi: 10.1186/1472-6963-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahal A, Yazbeck AS, Peters DH, Ramana GN. The Poor and health service use in India. Washington, DC: The World Bank; 2001. [Last accessed on 2016 Nov 17]. Available from: http://www.siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627.1095698140167/Mahal.ThePoorAnd.whole.pdf . [Google Scholar]
- 19.Prinja S, Kanavos P, Kumar R. Health care inequities in north india: Role of public sector in universalizing health care. Indian J Med Res. 2012;136:421–31. [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar C, Prakash R. Public-private dichotomy in utilization of health care services in India. J Sustain Dev. 2011;5:25–52. [Google Scholar]
- 21.Bhat R. Characteristics of private medical practice in india: A provider perspective. Health Policy Plan. 1999;14:26–37. doi: 10.1093/heapol/14.1.26. [DOI] [PubMed] [Google Scholar]
- 22.Kalpana S. Burden of non-communicable diseases in India: Setting priority for action. Int J Med Sci Public Health. 2013;2:7–11. [Google Scholar]
- 23.Berendes S, Heywood P, Oliver S, Garner P. Quality of private and public ambulatory health care in low and middle income countries: Systematic review of comparative studies. PLoS Med. 2011;8:e1000433. doi: 10.1371/journal.pmed.1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhatia J, Cleland J. Health care of female outpatients in South-central India: Comparing public and private sector provision. Health Policy Plan. 2004;19:402–9. doi: 10.1093/heapol/czh055. [DOI] [PubMed] [Google Scholar]
- 25.Prinja S, Bahuguna P, Pinto AD, Sharma A, Bharaj G, Kumar V, et al. The cost of universal health care in India: A model based estimate. PLoS One. 2012;7:e30362. doi: 10.1371/journal.pone.0030362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu C, Chin B, Li G, Murray CJ. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87:238. doi: 10.2471/BLT.08.054379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahal A, Karan A, Engelgau M. The Economic Implications of Non-Communicable Disease for India, World Bank. 2010. [Last accessed on 2016 Nov 17]. Available from: http://www.siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/281627.1095698140167/EconomicImplicationsofNCDforIndia.pdf .
- 28.Mondal S, Knajilal B, Peters DH, Lucas H. Catastrophic Out-of-pocket Payment for Health Care and its Impact on Households: Experience from West Bengal, India. 2010. [Last accessed on 2015 Jun 15]. Available from: http://www.chronicpoverty.org/uploads/publication_files/mondal_et_al_health.pdf .
- 29.Binnendijk E, Koren R, Dror DM. Can the rural poor in india afford to treat non-communicable diseases. Trop Med Int Health. 2012;17:1376–85. doi: 10.1111/j.1365-3156.2012.03070.x. [DOI] [PubMed] [Google Scholar]
- 30.Peters DH, Yazbeck AS, Sharma RR, Ramana GN, Pritchett LH, Wagstaff A. Better Health Systems for India's Poor: Findings, Analysis, and Options. Washington, DC: World Bank; 2002. [Last accessed on 2015 Jun 15]. Available from: https://www.openknowledge.worldbank.org/handle/10986/14080 . [Google Scholar]
- 31.Duggal R. Financing Healthcare in India-Prospects for Health Insurance. Express Healthcare Management. 2004. [Last accessed on 2015 Jun 05]. Available from: http://www.cehat.org/go/HealthServicesandFinancing .
- 32.Garg CC, Karan AK. Reducing out-of-pocket expenditures to reduce poverty: A disaggregated analysis at rural-urban and state level in India. Health Policy Plan. 2009;24:116–28. doi: 10.1093/heapol/czn046. [DOI] [PubMed] [Google Scholar]


