Abstract
In previous studies, the B-Raf proto-oncogene, serine/threonine kinase (BRAF)V600E mutation has been identified in multiple malignant tumors. BRAFV600E has been revealed to contribute to tumorigenesis by the activation of phospho-mitogen-activated protein kinases (MAPKs) and their downstream Monopolar spindle 1 (Mps1), leading to chromosome euploidy and tumor development. In the present study, the presence of phospho-MAPK and Mps1 in 161 thyroid carcinoma cases with complete clinical parameters was analyzed by immunohistochemistry, and the BRAF mutation was detected by polymerase chain reaction-direct sequencing. It was revealed that BRAFV600E was present in ~34% of thyroid cancer cases and was associated with age, clinical tumor stage and lymph node stage. However, the association of BRAFV600E with overall survival was not statistically significant. The expression of Mps1 was significantly increased in tumor tissues with BRAFV600E, however, this did not affect the expression of phospho-MAPK in thyroid carcinomas. Collectively, the results of the present study suggested that BRAFV600E may regulate the expression of Mps1 in MAP kinase independent ways in thyroid carcinoma. Therefore, Mps1 expression is associated with BRAFV600E while the upstream signaling of phospho-MAPK has no relevance. The specific mechanisms of BRAFV600E and the unknown pathway associated with Mps1 exhibit potential for further study, and provide a theoretical basis for the molecular treatment of thyroid carcinoma.
Keywords: thyroid carcinoma, B-Raf proto-oncogene serine/threonine kinaseV600E, phospho-mitogen-activated protein kinases, MpS1, immunohistochemistry
Introduction
Thyroid carcinoma is one of the major common malignant tumors of the endocrine system. Its incidence has grown to become the fifth most common cancer in females globally (1,2). In total, >50% of thyroid cancers in women and >45% of those in men were diagnosed at age 50+ (3). The increased incidence rates of thyroid cancer may be accounted for by changes in environmental risk factors, including obesity and molecular pathways (4–6). Thyroid carcinoma is classed into four main types, including papillary, follicular, medullary and anaplastic carcinomas (7). Among these four types of thyroid carcinoma, papillary thyroid carcinoma (PTC) is the predominant type, accounting for ~70% of all thyroid malignancies (8). Traditional clinical treatments for thyroid carcinoma include surgery, radioactive iodine and endocrine suppression therapy. PTC generally has an indolent course and favorable prognosis (9). However, there remain 20–30% of patients where PTC recrudesces and became resistant to radioactive iodine treatment, particularly in patients with advanced thyroid carcinoma, yielding poor prognosis and shorter survival (10,11). Therefore, there is an urgent requirement to elucidate the molecular mechanism underlying thyroid carcinoma progression and to improve the survival rate of patients with thyroid carcinoma.
Previously, there has been extensive research into the molecular alterations in thyroid carcinomas, with particular focus on the investigation of several oncogenic pathways that contribute to various cancer types (12,13). Numerous molecular markers associated with the prognosis of thyroid carcinomas have been identified, including RAS, phosphatidylinositol-4,5-bisphosphate 3-kinase, phosphatase and tensin homolog, tumour protein p53, anaplastic lymphoma kinase and B-Raf proto-oncogene serine/threonine kinase (BRAF). The most common gene alteration identified in thyroid carcinoma is BRAF mutation, which i§s associated with ~50% of these tumors (14,15). BRAF mutations are relatively specific for PTC and have not been identified in other types of thyroid carcinomas. The specific mutation that occurs in thyroid carcinomas is a threonine-to alanine nucleotide transversion at position 1799 in exon 15, which results in a valine-to-glutamate substitution at codon 600, named BRAFV600E, which has been revealed to be a potential prognostic factor in thyroid carcinoma (16,17).
BRAF belongs to the RAF protein kinase family, and is a serine/threonine kinase which serves an important function in the mitogen activated protein kinase (MAPK) signaling pathway (18). The mutation in this gene may activate the RAF/mitogen-activated protein kinase/extracellular regulated kinase (MEK)/extracellular signal regulated kinase (ERK) signaling pathway, promoting cell proliferation and inhibiting apoptosis. BRAF has been revealed to be mutated in a variety of malignant tumors. For example, BRAF mutations have been detected in ~70% of skin cancer (19), ~50% of thyroid carcinoma (20), ~20% of colorectal cancer (21), 14–30% of ovarian cancer (22), ~15% of hepatocellular carcinoma (23) and ~5% of lung cancer and breast cancer (24,25). Notably, BRAF mutation has also been identified as a lethal factor. Multiple studies have demonstrated that tumors with a BRAF mutation are resistant to traditional treatment, leading to poor prognosis (26,27). Therefore, the development of a novel therapeutic strategy for cancer with BRAF mutation is urgently required.
Previous studies have indicated that BRAFV600E mutation status may predict recurrence and prognosis in patients with thyroid carcinomas (15,28,29). BRAFV600E contributes to tumorigenesis by the continual activation of phospho-MAPK and the downstream Monopolar spindle 1 (Mps1) in thyroid carcinomas, leading to chromosome euploidy which promotes tumor development (30). Although there has been extensive research into the high frequency of BRAF mutations in thyroid carcinomas, the exact molecular mechanisms of BRAF mutation are yet to be fully understood. The present study will focus on observations of the BRAFV600E mutation in thyroid carcinomas, the associations between the BRAFV600E mutation, phospho-MAPK, Mps1 and clinical parameters of thyroid carcinomas and its prognostic significance.
Materials and methods
Ethics statement and clinical specimens
Cancer tissue samples were obtained from 161 patients with thyroid carcinomas who underwent surgical resection at the First Hospital of Shanxi Medical University, (Shanxi, China) and Shanxi Provincial People's Hospital, (Shanxi, China) between January 2009 and June 2015 (Table I). The present study was approved by the Ethics Committee of the First Hospital of Shanxi Medical University and written informed consent was obtained from the patients. All patients were enrolled at the time of surgery and did not receive treatment prior to surgery, including radiotherapy or chemotherapy. Surgically removed tissue was fixed in 10% buffered formalin for 24 h at room temperature, and embedded in paraffin. Hematoxylin and eosin-stained tumor tissues (stained for 5 min and 30 sec at room temperature, respectively) were reviewed by two pathologists. The tumor area was marked and then manually cut into 2 tissue volumes (10-µm thick) to collect tumor cells for DNA extraction. DNA was extracted using the FFPE DNA kit (Omega Bio-Tek, Inc., Norcross, GA, USA) following the manufacturer's protocol. The extracted DNA was quantified using a spectrophotometer (Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Table I.
Clinicopathological features of 161 patients with thyroid carcinomas.
| Clinicopathological feature | No. (161) |
|---|---|
| Sex | |
| Male | 34 |
| Female | 127 |
| Age, years | |
| >35 | 139 |
| ≤35 | 22 |
| Smoking status | |
| Yes | 9 |
| No | 152 |
| Drinking status | |
| Yes | 6 |
| No | 155 |
| Familial history | |
| Yes | 2 |
| No | 159 |
| Tumor grade | |
| Papillocarcinoma | 157 |
| Non-papillocarcinoma | 4 |
| Pathological T stage | |
| T1-T2 | 133 |
| T3-T4 | 28 |
| Pathological N stage | |
| N0 | 64 |
| N1 | 97 |
| Clinical M | |
| M0 | 161 |
| M1 | 0 |
| Pathological stage | |
| I–II | 106 |
| III–IV | 55 |
T, tumor; N, lymph node; M, metastasis.
BRAFV600E mutation analysis
To screen for the BRAFV600E mutation, DNA from tumor tissue was analyzed by polymerase chain reaction (PCR)-direct sequencing. Exon 15 of the BRAF gene, which contains the T1796A mutation, was amplified using the following specific primers: Forward, 5′-CTCTTCATAATGCTTGCTCTGATAGG-3′; and reverse, 5′-CTCTTCATAATGCTTGCTCTGATAGG-3′. The cycling conditions for PCR were as follows: Initial denaturation (98°C, 3 min) followed by 30 cycles of denaturation 98°C for 30 sec, annealing 58°C for 30 sec and then an extension 72°C for 30 sec. All PCR products were visualized using electrophoresis on a 2% agarose gel. Sanger sequencing was performed by the Beijing Genomics Institute (Shenzhen, China).
Immunohistochemistry (IHC)
Phospho-MAPK or Mps1 protein levels in thyroid carcinomas were determined by IHC with phospho-MAPK antibody (cat. no. 4370, Cell Signaling Technology, Inc., Danvers, MA, USA) or Mps1 antibody (cat. no. ab1118, Abcam, Cambridge, UK). IHC was performed as follows: In brief, sections were incubated with primary antibodies against phospho-MAPK (1:100) or Mps1 (1:50) overnight at 4°C, followed by detection using the PV8000 kit (Beijing Zhongshan Jinqiao Biotechnology Co., Ltd., Beijing, China) and DAB detection kit (Fuzhou Maixin Biotech Co., Ltd., Fuzhou, China), according to the manufacturer's protocol. Slides were counterstained with hematoxylin for 50 sec at room temperature. All images were captured using an Aprio automatic biopsy scanner at ×100 magnification. The percentage and intensity of positive staining of phospho-MAPK and Mps1 were analyzed using Aperio Cytoplasma 2.0 software (Leica Microsystems, Inc., Buffalo Grove, IL, USA). Statistical analyses were performed using GraphPad Prism v.6.0 software package (GraphPad Software, Inc., La Jolla, CA, USA). Using a scoring system from (−) to (+++) respectively, nucleus Phospho-MAPK expression was measured as negative for 0–25 scores (−), weak for 25–50 scores (+), median for 50–75 scores (++) or strong for >130 scores (+++). Cytoplasm Mps1 expression was measured as negative for 0–50 scores (−), weak for 50–90 scores (+), median for 90–130 scores (++) or strong for >130 scores (+++).
Statistical analysis
60 cases were selected for analysis, including 30 BRAFV600E-positive cases, which were randomly matched with 30 BRAFV600E-negative cases. The expression of phospho-MAPK and Mps1 levels between the paired samples were compared using χ2 tests or Fisher's exact tests. This was also used to assess the association between BRAF mutation status and clinical parameters. Cox regression was used to measure the association between BRAFV600E mutation and the clinical pathological information, linear regression was used to analyze the association between phospho-MAPK and Mps1 expression and survival analysis was performed using Kaplan-Meier analysis and the Log-rank test. Univariate and multivariate survival analyses were performed using a Cox proportional hazards regression model. P<0.05 was considered to indicate a statistically significant difference. All statistical tests were performed using IBM SPSS 19.0 (IBM Corp., Armonk, NY, USA).
Results
BRAFV600E mutation and its association with clinical parameters in thyroid carcinomas
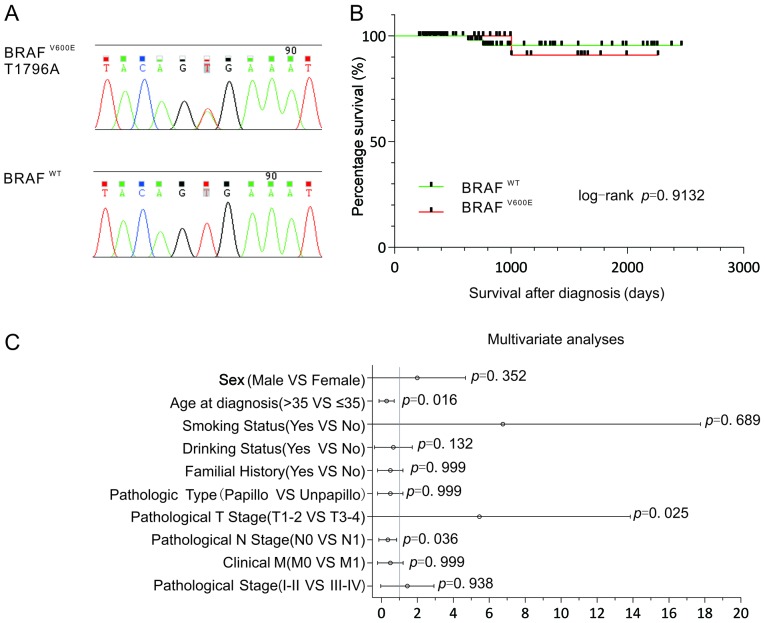
Single-base substitutions were detected by Sanger sequencing, which were presented in BRAF exon 15: T1796A, leading to a substitution of valine to glutamic acid at position 600 (V600E) in thyroid cancer (Fig. 1A). In 161 cases of thyroid carcinomas, 55 cases (34%) of BRAFV600E mutation were identified. A statistical analysis of BRAF mutations and clinical parameters revealed that BRAF mutations were significantly associated with age, tumor (T) stage and lymph node (N) stage, were more prevalent in younger patients (≤35 years), pathological T1-T2 stage patients and pathological N0 stage patients (χ2 test or Fisher's exact test, P<0.05, Table II; Cox regression analysis, P<0.05, Fig. 1C). However, there was no significant association between BRAF mutation status and other clinical parameters, including sex, smoking status, drinking status, familial history, tumor grade, clinical metastasis (M) and pathological stage (χ2 test or Fisher's exact test, P>0.05, Table II; Cox regression analysis, P>0.05, Fig. 1C). Although patients with thyroid carcinomas with BRAFV600E mutations had a higher risk of mortality, the association of BRAFV600E mutations with overall survival (OS) was not statistically significant [Log-rank (MantelCox), P=0.9132, Fig. 1B]. Furthermore, the Cox regression model revealed that age, T stage and N stage were associated with BRAFV600E mutation in thyroid cancer (Fig. 1C).
Figure 1.
BRAFV600E mutation and its association with clinical parameters in thyroid carcinomas. (A) Sanger sequencing peak figure of BRAF gene, The BRAFV600E mutation shows additional peaks compared with the wild-type, (B) Kaplan-Meier survival curves for patients with BRAFV600E mutations or wild-type in the cohort, (C) Cox regression analyses were used to assess the association of BRAFV600E mutation with clinical parameters in thyroid carcinomas. BRAF, B-Raf proto-oncogene serine/threonine kinase.
Table II.
Associations between BRAFV600E mutation/phospho-MAPK/Mps1 and clinicopathological parameters in thyroid carcinomas.
| B-RAFV600E mutation (n=161) | Phospho-MAPK in tumor (n=60) | MpS1 in tumor (n=60) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Clinicopathological feature | + | − | P-value | + | − | P-value | + | − | P-value |
| No. (%) | 54 (34%) | 107 (67%) | 2 (3%) | 58 (97%) | 47 (78%) | 13 (22%) | |||
| Sex | 0.514 | >0.999 | >0.999 | ||||||
| Male | 13 | 21 | 1 | 29 | 10 | 3 | |||
| Female | 41 | 86 | 1 | 29 | 37 | 10 | |||
| Age, years | 0.025 | 0.472 | >0.999 | ||||||
| >35 | 42 | 97 | 2 | 28 | 38 | 11 | |||
| ≤35 | 12 | 10 | 0 | 30 | 9 | 2 | |||
| Smoking status | 0.727 | 0.472 | >0.999 | ||||||
| Yes | 4 | 5 | 0 | 30 | 2 | 1 | |||
| No | 50 | 102 | 2 | 28 | 45 | 12 | |||
| Drinking status | 0.190 | 0.472 | >0.999 | ||||||
| Yes | 4 | 2 | 0 | 30 | 2 | 0 | |||
| No | 50 | 105 | 2 | 28 | 45 | 13 | |||
| Familial history | 0.211 | 0.472 | |||||||
| Yes | 2 | 0 | 0 | 30 | 0 | 0 | |||
| No | 52 | 107 | 2 | 28 | 47 | 13 | |||
| Tumor grade | 0.367 | 0.472 | |||||||
| Papillocarcinoma | 54 | 103 | 2 | 28 | 47 | 13 | |||
| Non-papillocarcinoma | 0 | 4 | 0 | 30 | 0 | 0 | |||
| Pathological T stage | 0.018 | 0.472 | 0.629 | ||||||
| T1-T2 | 50 | 83 | 2 | 28 | 41 | 10 | |||
| T3-T4 | 4 | 24 | 0 | 30 | 6 | 3 | |||
| Pathological N stage | 0.004 | 0.472 | 0.898 | ||||||
| N0 | 30 | 34 | 0 | 30 | 28 | 8 | |||
| N1 | 24 | 73 | 2 | 28 | 19 | 5 | |||
| Clinical M | 0.472 | ||||||||
| M0 | 54 | 107 | 2 | 28 | 47 | 13 | |||
| M1 | 0 | 0 | 0 | 30 | 0 | 0 | |||
| Pathological stage | 0.585 | 0.472 | >0.999 | ||||||
| I–II | 34 | 72 | 0 | 30 | 33 | 9 | |||
| III–IV | 20 | 35 | 2 | 28 | 14 | 4 | |||
BRAF, B-Raf proto-oncogene serine/threonine kinase; phospho-MAPK, phospho-mitogen-activated protein kinases; T, tumor; N, lymph node; M, metastasis.
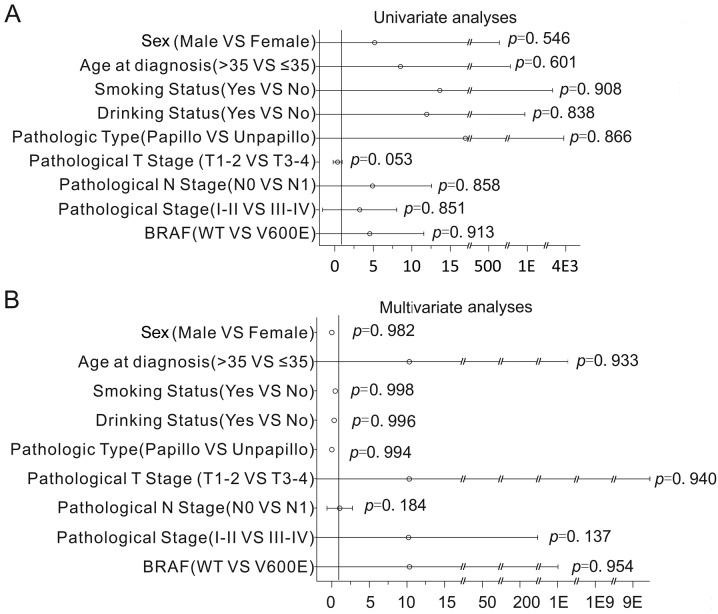
Cox regression analysis was used to assess the impact of BRAF mutations and clinical parameters on OS. Notably, the results revealed that the association of BRAF mutations with OS was not statistically significant (Cox regression univariate analyses, P=0.913, Fig. 2A; Cox regression multivariate analyses, P=0.954; Fig. 2B). Additionally, the association of clinical parameters with OS was not statistically significant (Cox regression univariate analyses, P>0.05; Fig. 2A; Cox regression multivariate analyses, P>0.05; Fig. 2B). This data indicates that there were no significantly associated prognostic factors in thyroid carcinoma.
Figure 2.
Cox regression analyses according to BRAF mutation status. Cox regression analysis was used to adjust for traditional prognostic factors, (A) Cox univariate regression analyses were used to examine the associations between clinical pathological parameters and prognosis, (B) Cox multivariate regression analyses were used to examine the associations between clinical pathological parameters and prognosis. BRAF, B-Raf proto-oncogene serine/threonine kinase.
IHC and evaluation of phospho-MAPK and Mps1 in thyroid carcinomas
Aside from a number of the papillary thyroid micro carcinoma cases, which were excluded due to the tumor tissue being too thin to obtain, 30 BRAFV600E cases and 30 BRAFWT cases matched in age, sex, pathological type and tumor size were selected to undergo IHC.
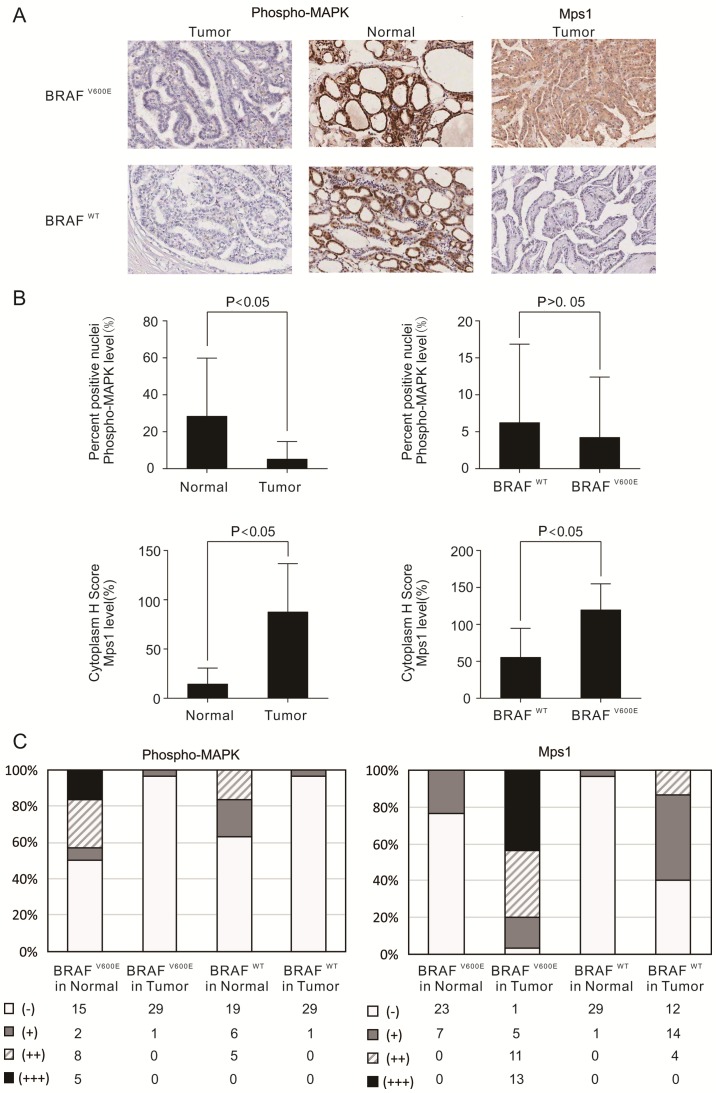
The results of IHC demonstrated that phospho-MAPK was expressed in the nucleus of normal tissues. The expression of phospho-MAPK was negative and had no difference between BRAFV600E and BRAFWT thyroid carcinomas tissues (Fig. 3A; χ2 test or Fisher's exact test, P>0.05, Table III). However, unexpectedly, phospho-MAPK levels were significantly decreased in tumor tissues compared with those in matched normal thyroid tissues, particularly in the tissues with BRAFV600E mutations (P<0.05; Fig. 3A). In the BRAFV600E samples, only 3.33% (1/30) demonstrated positive stained nuclei phospho-MAPK in tumor tissues, while 50% (15/30) demonstrated strongly stained nuclei in normal thyroid tissues (Fig. 3B and C). However, in the BRAFWT cases, only 3.33% (1/30) had nuclei that stained positive for phospho-MAPK in the tumor tissues, while 36.67% (11/30) demonstrated strongly positive nuclei staining in normal thyroid tissues (Fig. 3B and C).
Figure 3.
Immunohistochemical staining and evaluation of phospho-MAPK and Mps1 in thyroid carcinomas. (A) Representative immunohistochemistry images revealed phospho-MAPK or Mps1 staining in thyroid carcinomas and corresponding normal tissues with BRAFWT or BRAFV600E mutations, at ×100 magnification. In the BRAFWT and BRAFV600E mutation of thyroid carcinomas, the expression of phospho-MAPK was negative (first row), while in the normal tissues with BRAFWT and BRAFV600E mutation, the expression of phospho-MAPK was strongly positive in the nuclei (second row). In the thyroid carcinomas with BRAFWT, the expression of Mps1 was negative (third row left), while in the thyroid carcinomas with BRAFV600E mutation, the expression of Mps1 was strongly positive in the cytoplasm (third row right). (B) The bar graph revealed there was no significant difference in expression of Phospho-MAPK. (C) Cumulative bar chart revealing phospho-MAPK (left panel) and Mps1 (right panel) immunoreactivity in thyroid carcinomas. BRAF, B-Raf proto-oncogene serine/threonine kinase; MAPK, mitogen-associated protein kinase.
Table III.
Associations between phospho-MAPK and Msp1 expression, and BRAF mutation status.
| Phospho-MAPK | MpS1 | |||||
|---|---|---|---|---|---|---|
| PTC | + (%) | − (%) | P-value | + (%) | − (%) | P-value |
| BRAFV600E | 1 (3) | 29 (97) | 29 (97) | 1 (3) | ||
| BRAFWT | 1 (3) | 29 (97) | – | 18 (60) | 12 (40) | 0.002 |
PTC, papillary thyroid carcinoma; BRAF, B-Raf proto-oncogene serine/threonine kinase; phospho-MAPK, phospho-mitogen-activated protein kinases.
Further evaluations were made concerning the expression of Mps1 in cytoplasm. The expression of Mps1 was significantly increased in tumor tissues compared with that in matched normal tissues (P<0.05; Fig. 3A), and it was significantly increased in BRAFV600E mutation-positive tissues compared with that in BRAFWT tissues (Fig. 3A; χ2 test or Fisher's exact test, P<0.05, Table III). Furthermore, 71.67% (43/60) of the samples demonstrated cytoplasmic stained Mps1 in the tumor tissues, while 13.3% (8/60) stained positive in normal tissues (Fig. 3B). When the BRAF status was analyzed, 96.67% (29/30) of the samples were cytoplasmic-positive for Mps1 in BRAFV600E samples, while 60% (18/30) were cytoplasmic-positive in BRAFWT samples (Fig. 3B and 3C).
Association between phospho-MAPK or Msp1 expression and clinical parameters
Analysis of phospho-MAPK expression and clinical parameters revealed that the expression of phospho-MAPK in thyroid carcinomas had no significant association with clinical parameters, including sex, age, smoking status, drinking status, familial history, tumor grade, pathological N stage, clinical M and pathological stage (P>0.05, Table II). The expression of Mps1 had no significant association with clinical parameters, including sex, age, smoking status, drinking status, familial history, tumor grade, pathological T stage, pathological N stage, clinical M and pathological stage (P>0.05, Table II).
Associations between phospho-MAPK or Msp1 expression and BRAF mutation
The associations between phospho-MAPK or Msp1 expression and BRAF mutation were analyzed. No association was identified between the expression of phospho-MAPK and BRAF mutation (P>0.05, Table III). However, there was significant association between the expression of Mps1 and BRAF mutation (P<0.05, Table III). The expression of phospho-MAPK and Mps1 were not significantly associated (Linear regression correlation coefficient R2=0.032, P>0.05).
Discussion
The majority of patients with thyroid carcinoma are cured routinely and have a relatively good prognosis (31). Generally, patients with thyroid carcinomas are treated with thyroidectomy, and then radioiodine to remove residual tumor tissue and metastasis (12,32). However, in certain patients, thyroid cancer is diagnosed as a poorly differentiated carcinoma or anaplastic thyroid carcinoma rather than well-differentiated PTC. These patients also have significantly reduced survival (32). Therefore, it is important to identify novel therapeutic approaches for these types of thyroid carcinomas.
Thyroid carcinomas are associated with RAF-MEK-MAPK signaling (33). It has been revealed that BRAFV600E causes a 500-fold increase in activation of BRAF, and activates MEK-MAPK signaling constantly to regulate the expression of a variety of malignant tumor-associated genes, resulting in cell proliferation and differentiation (34–36). Thus, it serves an important function in the occurrence and progression of cancer.
BRAFV600E mutation appears to be the most frequent ontogenetic event in thyroid carcinomas. Due to its high frequency and specificity for thyroid carcinomas, the BRAFV600E mutation serves a unique and fundamental function in thyroid carcinomas (37). Therefore, it is of great importance to investigate the function and molecular mechanism of BRAFV600E in thyroid cancer, in order to identify novel treatment strategies, and to improve the survival rate. In the present study, 55 cases (34%) with BRAFV600E mutation in 161 cases of thyroid carcinomas were identified. Multiple studies have reported that the frequency of BRAFV600E mutation is 30–50% in thyroid carcinomas, and is associated with lymph node metastasis, extra thyroidal extension, tumor size, recurrence and drug tolerance (38–41). Xing (42) conducted a multicenter retrospective study, and after a mean follow-up of 33 months, they identified that the BRAFV600E mutation significantly increased cancer-associated mortality. However, other research from Japan and South Korea yielded different results, demonstrating that B-RAFV600E was not associated with poor prognosis in thyroid cancer (43,44). The results of the present study revealed that BRAF mutations were significantly more prevalent in younger patients (≤35 years), pathological T1-T2 stage patients, and pathological N0 stage patients. The association of BRAFV600E mutations with OS was not statistically significant. This may be due to the good prognosis of thyroid carcinomas, short follow-up time, difference of analysis method and the genetic difference between those of eastern Asian and Caucasian descent. The specific mechanisms of BRAFV600E still require further study.
The development of specific kinase inhibitors targeting BRAF, and the BRAFV600E allele in particular, has been achieved. One of these is inhibitor PLX4032. It is a highly selective inhibitor of BRAF kinase and has an anti-proliferative effect on the A375 melanoma cell line, which is BRAFV600E-positive. However, no differences in apoptosis and cell cycle in the thyroid carcinoma cell line NPA and ARO were observed, which also carries the BRAFV600E mutation. These results may be due to the opposite direction of regulation of p21cip1/waf1 between melanoma and thyroid cancer cells (45). Previous preclinical studies indicated that combination with BAY43-9006 or other agents to increase its efficacy was thought to be a novel strategy for effective clinical therapy (46).
Previous studies have identified Mps1 to be a downstream target of B-RAFV600E, and demonstrated that is significantly associated with phospho-MAPK in melanoma (30). Based on the high mutation rate of BRAFV600E in thyroid carcinoma, the present study detected the expression of phospho-MAPK and Mps1 in thyroid carcinoma by IHC. Compared with normal thyroid tissues, phospho-MAPK was significantly decreased in patients with thyroid carcinomas with the BRAFV600E mutation, which was consistent with previous studies (47,48). Furthermore, the expression of phospho-MAPK was not associated with tumor size or clinical stage. The expression of Mps1 in patients with the BRAFV600E mutation was significantly higher than that in patients with BRAFWT, it was significantly higher in tumor tissues than in paired normal tissue, and was not associated with clinical factors. The present study revealed that the expression of phospho-MAPK and Mps1 were not associated in patients with BRAFV600E. The classical theory of BRAFV600E, which is that it serves an important function in thyroid carcinomas through the continuous activation of the RAF-MEK-ERK signaling pathway, has been demonstrated in numerous studies in vivo and in vitro (49,50). However, the results of these studies contradict one another. Potential reasons include the high tumor metabolic rate of thyroid carcinomas. This suggests that the tumor specimens lost their blood supply following operation, and thus the phosphorylation process would be forced to stop due to the lack of ATP, which may lead to the low-level of phospho-MAPK (47). Therefore, the level of phospho-MAPK observed in specimens may not represent the actual level of phospho-MAPK in vivo. In addition, MAPK pathway signaling may be important in a context-dependent manner (30). As ERK phosphorylation was not associated with the presence of activating BRAF mutations, the way in which activated BRAF contributes to oncogenesis may be more complex than previously studied. This has important implications for therapeutic approaches targeting the MAP kinase pathway.
In conclusion, the results of the present study suggested that Mps1 expression is associated with BRAFV600E mutation while its upstream signal phospho-MAPK has no relevance. However, as a downstream gene of BRAF, the expression of Mps1 is affected not only by BRAFV600E but also by BRAFWT. These results revealed that BRAFV600E may regulate the expression of Mps1 in MAP kinase independent ways in thyroid carcinoma. In addition, these results demonstrated that the expression of Mps1 was not directly associated with prognosis of thyroid cancer, which may be due to the overall positive prognosis of thyroid cancer and limited number of samples. In future studies, sample size should be expanded to further research and explore the unknown pathways associated with Mps1, in order to provide a theoretical basis for molecular treatment of thyroid cancer.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant no. 81201956).
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 3.O'Grady TJ, Gates MA, Boscoe FP. Thyroid cancer incidence attributable to overdiagnosis in the United States 1981–2011. Int J Cancer. 2015;137:2664–2673. doi: 10.1002/ijc.29634. [DOI] [PubMed] [Google Scholar]
- 4.Aschebrook-Kilfoy B, Grogan RH, Ward MH, Kaplan E, Devesa SS. Follicular thyroid cancer incidence patterns in the United States, 1980–2009. Thyroid. 2013;23:1015–1021. doi: 10.1089/thy.2012.0356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen AY, Jemal A, Ward EM. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer. 2009;115:3801–3807. doi: 10.1002/cncr.24416. [DOI] [PubMed] [Google Scholar]
- 6.Schmid D, Ricci C, Behrens G, Leitzmann MF. Adiposity and risk of thyroid cancer: A systematic review and meta-analysis. Obes Rev. 2015;16:1042–1054. doi: 10.1111/obr.12321. [DOI] [PubMed] [Google Scholar]
- 7.Faam B, Ghaffari MA, Ghadiri A, Azizi F. Epigenetic modifications in human thyroid cancer. Biomed Rep. 2015;3:3–8. doi: 10.3892/br.2014.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ulisse S, Baldini E, Sorrenti S, Barollo S, Prinzi N, Catania A, Nesca A, Gnessi L, Pelizzo MR, Mian C, et al. In papillary thyroid carcinoma BRAFV600E is associated with increased expression of the urokinase plasminogen activator and its cognate receptor, but not with disease-free interval. Clin Endocrinol (Oxf) 2012;77:780–786. doi: 10.1111/j.1365-2265.2012.04465.x. [DOI] [PubMed] [Google Scholar]
- 9.Kim SH, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, Kim SY. Differences in the recurrence and survival of patients with symptomatic and asymptomatic papillary thyroid carcinoma: An observational study of 11,265 person-years of follow-up. Thyroid. 2016;26:1472–1479. doi: 10.1089/thy.2016.0238. [DOI] [PubMed] [Google Scholar]
- 10.Wobker SE, Kim LT, Hackman TG, Dodd LG. Use of BRAF v600e immunocytochemistry on FNA direct smears of papillary thyroid carcinoma. Cancer Cytopathol. 2015;123:531–539. doi: 10.1002/cncy.21575. [DOI] [PubMed] [Google Scholar]
- 11.Benvenga S, Koch CA. Molecular pathways associated with aggressiveness of papillary thyroid cancer. Curr Genomics. 2014;15:162–170. doi: 10.2174/1389202915999140404100958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xing M. BRAF mutation in papillary thyroid cancer: Pathogenic role, molecular bases, and clinical implications. Endocr Rev. 2007;28:742–762. doi: 10.1210/er.2007-0007. [DOI] [PubMed] [Google Scholar]
- 13.Caronia LM, Phay JE, Shah MH. Role of BRAF in thyroid oncogenesis. Clin Cancer Res. 2011;17:7511–7517. doi: 10.1158/1078-0432.CCR-11-1155. [DOI] [PubMed] [Google Scholar]
- 14.Soares P, Trovisco V, Rocha AS, Lima J, Castro P, Preto A, Máximo V, Botelho T, Seruca R, Sobrinho-Simões M. BRAF mutations and RET/PTC rearrangements are alternative events in the etiopathogenesis of PTC. Oncogene. 2003;22:4578–4580. doi: 10.1038/sj.onc.1206706. [DOI] [PubMed] [Google Scholar]
- 15.Xing M, Alzahrani AS, Carson KA, Shong YK, Kim TY, Viola D, Elisei R, Bendlová B, Yip L, Mian C, et al. Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol. 2015;33:42–50. doi: 10.1200/JCO.2014.56.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xing M, Haugen BR, Schlumberger M. Progress in molecular-based management of differentiated thyroid cancer. Lancet. 2013;381:1058–1069. doi: 10.1016/S0140-6736(13)60109-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xing M. Molecular pathogenesis and mechanisms of thyroid cancer. Nat Rev Cancer. 2013;13:184–199. doi: 10.1038/nrc3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazzaferri EL, Kloos RT. Clinical review 128: Current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001;86:1447–1463. doi: 10.1210/jcem.86.4.7407. [DOI] [PubMed] [Google Scholar]
- 19.Anderson S, Bloom KJ, Vallera DU, Rueschoff J, Meldrum C, Schilling R, Kovach B, Lee JR, Ochoa P, Langland R, et al. Multisite analytic performance studies of a real-time polymerase chain reaction assay for the detection of BRAF V600E mutations in formalin-fixed, paraffin-embedded tissue specimens of malignant melanoma. Arch Pathol Lab Med. 2012;136:1385–1391. doi: 10.5858/arpa.2011-0505-OA. [DOI] [PubMed] [Google Scholar]
- 20.Kim SJ, Lee KE, Myong JP, Park JH, Jeon YK, Min HS, Park SY, Jung KC, Koo do H, Youn YK. BRAF V600E mutation is associated with tumor aggressiveness in papillary thyroid cancer. World J Surg. 2012;36:310–317. doi: 10.1007/s00268-011-1383-1. [DOI] [PubMed] [Google Scholar]
- 21.Kalady MF, Dejulius KL, Sanchez JA, et al. BRAF mutations in colorectal cancer are associated with distinct clinical characteristics and worse prognosis. Dis Colon Rectum. 2012;55:128–133. doi: 10.1097/DCR.0b013e31823c08b3. [DOI] [PubMed] [Google Scholar]
- 22.Wong KK, Tsang YT, Deavers MT, Mok SC, Zu Z, Sun C, Malpica A, Wolf JK, Lu KH, Gershenson DM. BRAF mutation is rare in advanced-stage low-grade ovarian serous carcinomas. Am J Pathol. 2010;177:1611–1617. doi: 10.2353/ajpath.2010.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colombino M, Sperlongano P, Izzo F, Tatangelo F, Botti G, Lombardi A, Accardo M, Tarantino L, Sordelli I, Agresti M, et al. BRAF and PIK3CA genes are somatically mutated in hepatocellular carcinoma among patients from South Italy. Cell Death Dis. 2012;3:e259. doi: 10.1038/cddis.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kobayashi M, Sonobe M, Takahashi T, Yoshizawa A, Ishikawa M, Kikuchi R, Okubo K, Huang CL, Date H. Clinical significance of BRAF gene mutations in patients with non-small cell lung cancer. Anticancer Res. 2011;31:4619–4623. [PubMed] [Google Scholar]
- 25.Greenman C, Stephens P, Smith R, Dalgliesh GL, Hunter C, Bignell G, Davies H, Teague J, Butler A, Stevens C, et al. Patterns of somatic mutation in human cancer genomes. Nature. 2007;446:153–158. doi: 10.1038/nature05610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weeraratna AT. RAF around the edges-the paradox of BRAF inhibitors. N Engl J Med. 2012;366:271–273. doi: 10.1056/NEJMe1111636. [DOI] [PubMed] [Google Scholar]
- 27.Su F, Viros A, Milagre C, Trunzer K, Bollag G, Spleiss O, Reis-Filho JS, Kong X, Koya RC, Flaherty KT, et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. N Engl J Med. 2012;366:207–215. doi: 10.1056/NEJMoa1105358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yarchoan M, LiVolsi VA, Brose MS. BRAF mutation and thyroid cancer recurrence. J Clin Oncol. 2015;33:7–8. doi: 10.1200/JCO.2014.59.3657. [DOI] [PubMed] [Google Scholar]
- 29.Rossi M, Buratto M, Tagliati F, Rossi R, Lupo S, Trasforini G, Lanza G, Franceschetti P, Bruni S, Uberti Degli E, Zatelli MC. Relevance of BRAF(V600E) mutation testing versus RAS point mutations and RET/PTC rearrangements evaluation in the diagnosis of thyroid cancer. Thyroid. 2015;25:221–228. doi: 10.1089/thy.2014.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu J, Cheng X, Zhang Y, Li S, Cui H, Zhang L, Shi R, Zhao Z, He C, Wang C, et al. Phosphorylation of Mps1 by BRAFV600E prevents Mps1 degradation and contributes to chromosome instability in melanoma. Oncogene. 2013;32:713–723. doi: 10.1038/onc.2012.94. [DOI] [PubMed] [Google Scholar]
- 31.Samaan NA, Schultz PN, Hickey RC, Goepfert H, Haynie TP, Johnston DA, Ordonez NG. The results of various modalities of treatment of well differentiated thyroid carcinomas: A retrospective review of 1599 patients. J Clin Endocrinol Metab. 1992;75:714–720. doi: 10.1210/jcem.75.3.1517360. [DOI] [PubMed] [Google Scholar]
- 32.Chiloeches A, Marais R. Is BRAF the Achilles' Heel of thyroid cancer? Clin Cancer Res. 2006;12:1661–1664. doi: 10.1158/1078-0432.CCR-06-0051. [DOI] [PubMed] [Google Scholar]
- 33.Roberts PJ, Der CJ. Targeting the Raf-MEK-ERK mitogen-activated protein kinase cascade for the treatment of cancer. Oncogene. 2007;26:3291–3310. doi: 10.1038/sj.onc.1210422. [DOI] [PubMed] [Google Scholar]
- 34.Jinushi M, Chiba S, Baghdadi M, Kinoshita I, Dosaka-Akita H, Ito K, Yoshiyama H, Yagita H, Uede T, Takaoka A. ATM-mediated DNA damage signals mediate immune escape through integrin-αvβ3-dependent mechanisms. Cancer Res. 2012;72:56–65. doi: 10.1158/0008-5472.CAN-11-2028. [DOI] [PubMed] [Google Scholar]
- 35.Dhomen N, Reis-Filho JS, da Rocha Dias S, Hayward R, Savage K, Delmas V, Larue L, Pritchard C, Marais R. Oncogenic Braf induces melanocyte senescence and melanoma in mice. Cancer Cell. 2009;15:294–303. doi: 10.1016/j.ccr.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 36.Perera PM, Wypasek E, Madhavan S, Rath-Deschner B, Liu J, Nam J, Rath B, Huang Y, Deschner J, Piesco N, et al. Mechanical signals control SOX-9, VEGF, and c-Myc expression and cell proliferation during inflammation via integrin-linked kinase, B-Raf, and ERK1/2-dependent signaling in articular chondrocytes. Arthritis Res Ther. 2010;12:R106. doi: 10.1186/ar3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jeong D, Jeong Y, Park JH, Han SW, Kim SY, Kim YJ, Kim SJ, Hwangbo Y, Park S, Cho HD, et al. BRAF (V600E) mutation analysis in papillary thyroid carcinomas by peptide nucleic acid clamp real-time PCR. Ann Surg Oncol. 2013;20:759–766. doi: 10.1245/s10434-012-2494-0. [DOI] [PubMed] [Google Scholar]
- 38.Kim TH, Park YJ, Lim JA, Ahn HY, Lee EK, Lee YJ, Kim KW, Hahn SK, Youn YK, Kim KH, et al. The association of the BRAF(V600E) mutation with prognostic factors and poor clinical outcome in papillary thyroid cancer: A meta-analysis. Cancer. 2012;118:1764–1773. doi: 10.1002/cncr.26500. [DOI] [PubMed] [Google Scholar]
- 39.Elisei R, Viola D, Torregrossa L, Giannini R, Romei C, Ugolini C, Molinaro E, Agate L, Biagini A, Lupi C, et al. The BRAF(V600E) mutation is an independent, poor prognostic factor for the outcome of patients with low-risk intrathyroid papillary thyroid carcinoma: Single-institution results from a large cohort study. J Clin Endocrinol Metab. 2012;97:4390–4398. doi: 10.1210/jc.2012-1775. [DOI] [PubMed] [Google Scholar]
- 40.Barollo S, Pennelli G, Vianello F, Fernando Watutantrige S, Negro I, Boschin Merante I, Pelizzo MR, Rugge M, Mantero F, Nacamulli D, et al. BRAF in primary and recurrent papillary thyroid cancers: The relationship with (131)I and 2-[(18)F]fluoro-2-deoxy-D-glucose uptake ability. Eur J Endocrinol. 2010;163:659–663. doi: 10.1530/EJE-10-0290. [DOI] [PubMed] [Google Scholar]
- 41.Pelizzo MR, Boschin IM, Barollo S, Pennelli G, Toniato A, Zambonin L, Vianello F, Piotto A, Ide EC, Pagetta C, et al. BRAF analysis by fine needle aspiration biopsy of thyroid nodules improves preoperative identification of papillary thyroid carcinoma and represents a prognostic factor. A mono-institutional experience. Clin Chem Lab Med. 2011;49:325–329. doi: 10.1515/CCLM.2011.031. [DOI] [PubMed] [Google Scholar]
- 42.Xing M. Prognostic utility of BRAF mutation in papillary thyroid cancer. Mol Cell Endocrinol. 2010;321:86–93. doi: 10.1016/j.mce.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kebebew E, Weng J, Bauer J, Ranvier G, Clark OH, Duh QY, Shibru D, Bastian B, Griffin A. The prevalence and prognostic value of BRAF mutation in thyroid cancer. Ann Surg. 2007;246:466–471. doi: 10.1097/SLA.0b013e318148563d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nam JK, Jung CK, Song BJ, Lim DJ, Chae BJ, Lee NS, Park WC, Kim JS, Jung SS, Bae JS. Is the BRAF(V600E) mutation useful as a predictor of preoperative risk in papillary thyroid cancer? Am J Surg. 2012;203:436–441. doi: 10.1016/j.amjsurg.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 45.Sala E, Mologni L, Truffa S, Gaetano C, Bollag GE, Gambacorti-Passerini C. BRAF silencing by short hairpin RNA or chemical blockade by PLX4032 leads to different responses in melanoma and thyroid carcinoma cells. Mol Cancer Res. 2008;6:751–759. doi: 10.1158/1541-7786.MCR-07-2001. [DOI] [PubMed] [Google Scholar]
- 46.Madhunapantula SV, Robertson GP. Is B-Raf a good therapeutic target for melanoma and other malignancies? Cancer Res. 2008;68:5–8. doi: 10.1158/0008-5472.CAN-07-2038. [DOI] [PubMed] [Google Scholar]
- 47.Kim SW, Kim HK, Lee JI, Jang HW, Choe JH, Kim JH, Kim JS, Hur KY, Kim JH, Chung JH. ERK phosphorylation is not increased in papillary thyroid carcinomas with BRAF(V600E) mutation compared to that of corresponding normal thyroid tissues. Endocr Res. 2013;38:89–97. doi: 10.3109/07435800.2012.723292. [DOI] [PubMed] [Google Scholar]
- 48.Zuo H, Nakamura Y, Yasuoka H, Zhang P, Nakamura M, Mori I, Miyauchi A, Kakudo K. Lack of association between BRAF V600E mutation and mitogen-activated protein kinase activation in papillary thyroid carcinoma. Pathol Int. 2007;57:12–20. doi: 10.1111/j.1440-1827.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- 49.Kimura ET, Nikiforova MN, Zhu Z, Knauf JA, Nikiforov YE, Fagin JA. High prevalence of BRAF mutations in thyroid cancer: Genetic evidence for constitutive activation of the RET/PTC-RAS-BRAF signaling pathway in papillary thyroid carcinoma. Cancer Res. 2003;63:1454–1457. [PubMed] [Google Scholar]
- 50.Melillo RM, Castellone MD, Guarino V, De Falco V, Cirafici AM, Salvatore G, Caiazzo F, Basolo F, Giannini R, Kruhoffer M, et al. The RET/PTC-RAS-BRAF linear signaling cascade mediates the motile and mitogenic phenotype of thyroid cancer cells. J Clin Invest. 2005;115:1068–1081. doi: 10.1172/JCI200522758. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]