Case presentation
A 65-year old man experienced 6 months of gradually worsening fatigue, weight loss, and dyspnea prompting evaluation with a chest x-ray demonstrating pulmonary nodules in the right lung and a “white out” of his left lung. Thoracentesis was performed and drained 3.2L of bloody fluid. A computed tomography (CT) scan of his abdomen and pelvis demonstrated a large (8.6cm), partially exophytic, heterogeneously enhancing mass arising from the anterior aspect of the left kidney with apparent invasion into the renal vein and extensive metastatic disease in his chest (Fig. 1A and B). He underwent a CT-guided biopsy of a pulmonary nodule. Histopathologic evaluation of the biopsy specimen confirmed suspected clear cell renal cell carcinoma (RCC), Fuhrman grade 3 (Fig. 2A). Immunohistochemical analysis did not demonstrate expression of programmed death-1 (PD-1) or programmed death ligand-1 (PD-L1) on the tumor or tumor infiltrating lymphocytes (Fig. 3A and B). Due to poor pulmonary function and performance status, the patient was initially started on systemic therapy. He was initially treated with the tyrosine kinase inhibitor sunitinib. Unfortunately this did not result in any radiographic response and he was transitioned to second-line nivolumab therapy – a PD-1 inhibitor. Subsequently, his respiratory symptoms and performance status rapidly improved back to his baseline. Repeated CT imaging demonstrated complete resolution of pulmonary metastases as well dramatic change in the primary tumor, now 3.8cm in size and lacking enhancement after contrast administration (Fig. 1C and D). Due to concern for persistent malignancy in the kidney despite the favorable radiographic findings, he underwent an uncomplicated radical nephrectomy. Histopathologic evaluation of the nephrectomy specimen demonstrated no evidence of viable malignancy (Fig. 2B); the site of the former tumor was extensively infiltrated with inflammatory cells with high expression of PD-1 and PD-L1 (Fig. 3C and D). Following nephrectomy the patient recovered well and continued on nivolumab treatment. He is now one year after nephrectomy and has no evidence of disease on surveillance imaging.
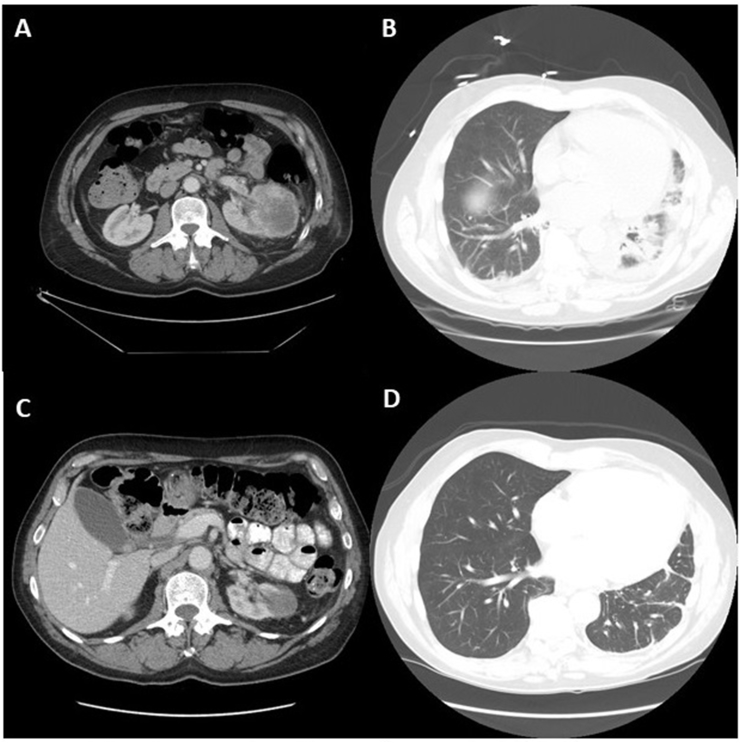
Fig. 1.
(A) Initial contrast-enhanced computed tomography (CT) scan demonstrating 8.6 cm heterogeneously enhancing left renal mass and (B) extensive metastatic disease in the chest at the time of diagnosis. Post-nivolumab therapy contrast-enhanced CT scan demonstrating 3.5cm non-enhancing left renal lesion (C) and resolution of pulmonary metastases. (D).
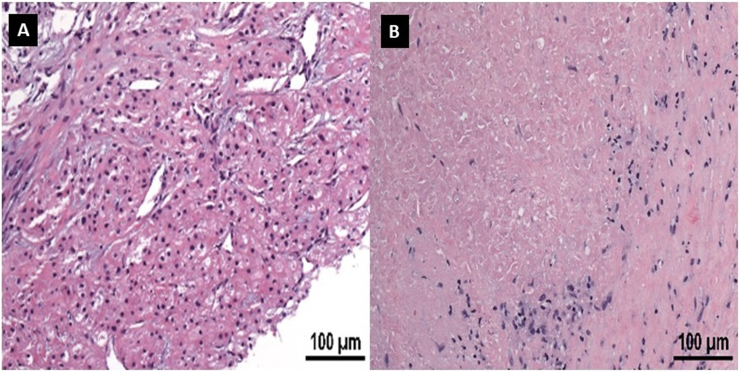
Fig. 2.
(A) Hematoxylin eosin (H&E) stain of diagnostic pleural biopsy demonstrating Fuhrman grade 2 clear cell renal cell carcinoma. (B) H&E stain of nephrectomy specimen following nivolumab treatment demonstrating no evidence of viable malignancy and extensive inflammatory cells infiltrating the former tumor site.
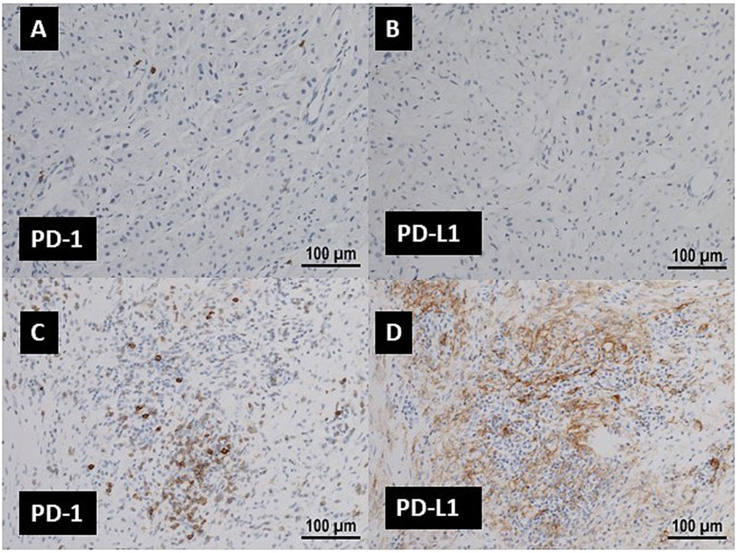
Fig. 3.
(A) and (B) Immunohistochemical (IHC) staining demonstrating lack of PD-1 and PD-L1 expression of the pleural biopsy. (C) and (D) IHC demonstrating significant expression of PD-1 and PD-L1 in inflammatory cells of nephrectomy specimen.
Discussion
The pivotal CheckMate 025 trial comparing nivolumab vs. everolimus in the second-line setting for metastatic clear cell RCC reported an objective response in 25% of cases and 1% complete response rate.1 This trial led to the regulatory approval of nivolumab and ushered in a new era of hope for patients with metastatic RCC. This paradigm shift in treatment has significant implications on other aspects of treatment – including the role of surgery.
Although level 1 evidence has established the role of cytoreductive nephrectomy (CNx) with interferon-alfa,2 and CNx is commonly performed in patients treated with tyrosine kinase inhibitors based on retrospective evidence that its use confers a survival advantage, the utility of cytoreductive nephrectomy has not been established in this most recent era of immune checkpoint inhibition.3 Approximately 90% of patients in the pivotal nivolumab trial had a prior nephrectomy before systemic therapy,1 but guidance from literature is lacking on the role of CNx following a complete radiographic response to immune checkpoint inhibitors. Additionally, the degree to which radiographic tumor resolution after immune checkpoint inhibition correlates with absence of viable malignancy pathologically is unknown. An ongoing pilot study at MD Anderson Cancer Center in which patients with metastatic RCC are treated with different combinations of immune checkpoint inhibition followed by CNx may answer some of these questions, though it will be underpowered to assess the role of CNx following complete radiographic response.4 As the use of immune checkpoint inhibition continues to increase, including in the first-line setting,5 the accumulation of similar cases should prompt further evaluation of role of CNx in this latest phase of systemic therapy.
Funding
This work was supported by the National Institute of Health (T32 CA136515 Ruth L. Kirschstein Institutional National Research Award to S.L.W.)
Conflicts of interest
None.
Acknowledgements
None.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eucr.2018.02.016.
Contributor Information
Solomon L. Woldu, Email: Solomon.Woldu@utsouthwestern.edu.
James Brugarolas, Email: James.Brugarolas@utsouthwestern.edu.
Payal Kapur, Email: Payal.Kapur@utsouthwestern.edu.
Vitaly Margulis, Email: Vitaly.Margulis@utsouthwestern.edu.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Motzer R.J., Escudier B., McDermott D.F. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Eng. J. Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flanigan R.C., Mickisch G., Sylvester R., Tangen C., Van Poppel H., Crawford E.D. Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis. J. Urol. 2004;171:1071–1076. doi: 10.1097/01.ju.0000110610.61545.ae. [DOI] [PubMed] [Google Scholar]
- 3.Petrelli F., Coinu A., Vavassori I. Cytoreductive nephrectomy in metastatic renal cell carcinoma treated with targeted therapies: a systematic review with a meta-analysis. Clin. Genitourin. Canc. 2016;14:465–472. doi: 10.1016/j.clgc.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 4.ClinicalTrials.gov . Health USNIo. 2017. Nivolumab vs Nivolumab + Bevacizumab vs Nivolumab + Ipilimumab in Metastatic Renal Cell Carcinoma (mRCC) [Google Scholar]
- 5.ClinicalTrials.gov . Health USNIo. 2017. Nivolumab Combined With Ipilimumab Versus Sunitinib in Previously Untreated Advanced or Metastatic Renal Cell Carcinoma (CheckMate 214) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.