Abstract
Background
Increases in life expectancy has meant that a higher proportion of patients presenting to surgical assessment units are now elderly. Abdominal computed tomography (CT) can provide early and accurate diagnosis in the elderly, even in the presence of incomplete clinical and biological findings. The aim of this study was to investigate the use of early CT imaging in elderly patients presenting directly to the surgical assessment unit.
Materials and methods
All consecutive patients aged 65 years and over admitted directly to the surgical assessment unit between January 2017 and April 2017 were identified. Data were collected on demographics, laboratory investigations, radiological investigations and hospital admission. The primary outcome measure was overall length of stay.
Results
A total of 200 consecutive patients were identified and included over a six-month period. This comprised 110 women and 90 men with a median age of 78 years (range 64–98 years). A total of 83 patients underwent CT on admission to the surgical assessment unit. White cell count (WCC) and C-reactive protein (CRP) results were significantly higher in patients undergoing CT (P = 0.001). Median length of stay for patients undergoing CT was 5 days (range 1–19 days). This was significantly lower than those patients not receiving CT imaging, at 6 days (range 1–105 days; P = 0.034).
Discussion
CT should be considered as a first-line investigation when elderly patients with an acute abdomen are admitted to surgical assessment units. Early CT can accelerate hospital discharge and decrease overall length of hospital stay.
Keywords: Elderly, General surgery, Computed tomography
Introduction
The population of the UK is ageing.1 What defines an elderly person varies considerably in the literature; however, the most widely used reference is that of the World Health Organization, which classifies an individual aged over 65 years as elderly.2,3 As of mid-2016, 18% of the UK population falls into this category.1 This increase in life expectancy has meant that a higher proportion of patients presenting to surgical assessment units are now elderly.
For acute surgical admissions, a common shortfall in this patient group is poor preoperative assessment and delay between admission and theatre.4 Clinical diagnosis can be complex due to multiple comorbidities, polypharmacy, insufficient patient details and atypical presentations.5,6 Abdominal CT can provide early and accurate diagnosis in the elderly, even in the presence of incomplete clinical and biological findings.7
A substantial proportion of emergency admissions are via accident and emergency departments.8 For elderly patients who present via this route, the use of early CT can not only influence decision making but also significantly affect their discharge times.9 Many patients, however, are still referred to surgical assessment units directly via the GP and community.8 This route requires the presence of hospital assessment beds and junior doctors are tasked with clerking and investigating these patients with limited clinical information to hand.
The aim of this study was to investigate the use of early CT in elderly patients presenting directly to the surgical assessment unit. The authors hypothesise that CT during acute surgical admission in the elderly cohort reduces hospital length of stay through earlier diagnosis and initiation of appropriate management.
Materials and methods
In this retrospective observational cohort study, all consecutive patients aged 65 years and over admitted directly to the surgical assessment unit between January 2017 and June 2017 were identified. Data were collected from a surgical admissions unit database and verified alongside clinical records and hospital patient management systems. Data were collected on patient demographics, date and time of admission and date and time of discharge. Admission data were categorised as either weekday or weekend and day shift (8am to 7.59pm) or night shift (8pm to 7.59am). Patients who required overnight hospital admission for investigation and treatment were included; those discharged the same day were omitted from further analysis.
Initial laboratory investigations for WCC, CRP and evidence of acute kidney injury on admission were collected for all patients. The date and time of any initial x-ray investigations performed were recorded, alongside date and times of any further radiological investigations in the form of CT. For all patients undergoing CT, the main report findings were documented.
Overall length of hospital stay was calculated for all patients. In patients undergoing CT investigation, length of stay from point of CT to discharge was also documented. All inpatient deaths were recorded.
The primary outcome measure was overall length of stay. Differences in variables between groups (No CT vs CT) were calculated using the chi-squared test for categorical data and one-way analysis of variance for continuous data. A P-value of less than 0.05 was deemed to be statistically significant. All statistical analysis was performed using SPSS 23 (Version 23).
Results
Demographics
Some 163 patients (82%) were admitted during a weekday, while the remaining 37 patients were admitted during the weekend; 142 patients were admitted during day shift working hours, with 58 patients being admitted during night shift working hours. No significant differences between groups were identified for age, gender, day of admission or time of admission. Baseline characteristics of both groups are demonstrated in Table 1.
Table 1.
Baseline characteristics for all patients (data expressed as whole numbers).
| Parameter | No CT imaging (n=117)n (range) | CT imaging (n=83)n (range) | P-value |
| Median age (years) | 79 (66–96) | 77 64-98 | 0.395a |
| Gender: | 0.103b | ||
| Male | 47 | 43 | |
| Female | 70 | 40 | |
| Day of admission: | 0.178b | ||
| Weekday | 99 | 64 | |
| Weekend | 18 | 19 | |
| Time of admission: | 0.982b | ||
| Day | 83 | 59 | |
| Night | 34 | 24 | |
| Median WCC (x 109 cells/l) | 10 (3–24) | 13 (3–40) | 0.001a |
| Median CRP (mg/l) | 9 (5–339) | 49 (5–323) | 0.001a |
| Acute kidney injury: | 0.002b | ||
| No | 90 | 47 | |
| Yes | 27 | 36 | |
| X-rays: | 0.513b | ||
| No | 36 | 22 | |
| Yes | 81 | 61 | |
| Inpatient mortality: | 0.611b | ||
| No | 111 | 80 | |
| Yes | 6 | 3 | |
| Median length of stay (days) | 6 (1–105) | 5 (1–19) | 0.034a |
a One-way analysis of variance.
b chi-squared test.
Laboratory Investigations
The median WCC for patients not undergoing CT was 10 x 109 cells/l (range 3–24 x 109 cells/l). This was significantly lower than those undergoing CT at 13 x 109 cells/l (range 3–40 x 109 cells/l); P = 0.001. Similarly, the median CRP for patients not undergoing CT was 9 mg/l (range 5–339 mg/l) compared with those undergoing CT imaging at 49 mg/l (range 5–323 mg/l); P = 0.001. A total of 63 patients (32%) were diagnosed as having acute kidney injury on initial laboratory investigations. In those patients who underwent CT, the proportion with acute kidney injury was significantly higher (P = 0.002).
Radiological imaging
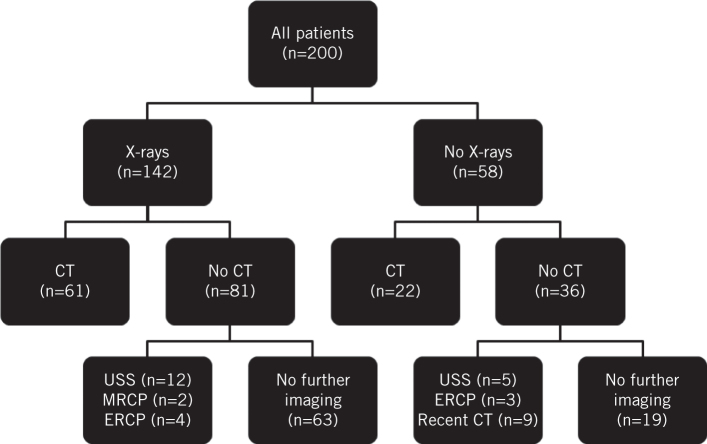
A total of 58 patients did not undergo any x-ray investigations; 22 of these patients (38%) proceeded directly to CT. The median time to CT in these 22 patients was 4.89 hours (range 0.57–16.93 hours). Of the 142 patients that underwent x-ray investigation, 61 (43%) went on to have further CT performed. The median time from x-ray to CT was 9.95 hours (range 0.35–23.85 hours). Thirty-six patients (18%) had neither x-rays nor CT imaging performed on admission. Of these 36 patients, 9 had undergone recent outpatient CT imaging, 5 had abdominal ultrasonography performed on admission and 3 patients proceeded directly to endoscopic retrograde cholangiopancreatography (Fig 1). Only three patients in total (4%) undergoing CT had scans that were reported as normal intraabdominal findings. The most common CT diagnoses are highlighted in Table 2. A total of seven patients had CT despite both normal WCC and CRP levels. Of these patients, three had evidence of diverticulosis, one was diagnosed with an abdominal aortic aneurysm, one had gallstone disease and two scans were reported as normal.
Figure 1.
Flow diagram illustrating radiological imaging on all patients
Table 2.
Diagnosis following computed tomography.
| Diagnosis | Patients (n) |
| Bowel obstruction | 13 |
| Cholecystitis | 13 |
| Diverticulitis | 12 |
| Perforation | 7 |
| Pancreatitis | 6 |
| Disseminated malignancy | 6 |
| Appendicitis | 4 |
| Colitis | 4 |
| Normal | 3 |
| Other | 15 |
Surgical intervention
Twenty-eight patients required surgical intervention during their acute admission, with all patients undergoing CT prior to theatre. Median time from x-ray to CT was 4.5 hours (range 0.78-20.13 hours). Median length of stay in patients requiring surgical intervention was 4 days (range 1–14 days).
Inpatient mortality
Nine patients (5%) died during their acute admission: five male and four female, with a median age of 88 years (range 67–96 years). Six patients did not undergo inpatient CT compared with three patients who had CT on admission; P = 0.611. The most common cause of death was metastatic colorectal cancer (n = 4). Other causes were ischaemic bowel (n = 3), severe acute pancreatitis (n = 1) and aspiration pneumonia (n = 1).
Length of stay
Median length of stay for patients undergoing CT was 5 days (range 1–19 days). This was significantly lower than those patients not receiving CT at 6 days (range 1–105 days); P = 0.034. Median length of stay from CT to discharge was 4 days (range 1–14 days).
Discussion
The results of this study demonstrate that early CT in elderly patients admitted to surgical assessment unit can accelerate hospital discharge and decrease overall length of hospital stay. Baseline characteristics were similar among the groups, with the only significant differences identified in WCC, CRP and the presence of acute kidney injury. Patients who underwent early CT presented with higher baseline WCC and CRP levels. Surprisingly, a higher proportion of patients with acute kidney injury also underwent CT, indicating that the need for urgent diagnosis outweighed concerns over the risk of further kidney injury. One study has shown that intravenous contrast is not associated with increased frequency of acute kidney injury, therefore rejecting the notion that CT should be delayed until adequate fluid resuscitation.10
Publicity from the work generated by Freemantle et al. highlighted the negative effects of weekend care provision on patients, indicating that mortality risk is higher when compared with those admitted during weekdays.11 A more recent multicentre study by Walker et al. has argued that these differences in mortality arise from patient differences rather than reduced hospital services and care on weekends.12 Similarly, our results demonstrated that frequency of CT was not influenced by admission day or time, thus excluding any treatment bias.
Plain chest or abdominal radiographs are conventionally seen as the recommended diagnostic modality in demonstrating signs of pneumoperitoneum or bowel obstruction. However, not only do they provide limited clinical information, they can also be misleading.13,14 Furthermore, any overt signs on a plain radiograph will likely require more detailed CT.14 Almost 25% of patients who underwent CT within our study were diagnosed with either bowel obstruction or visceral perforation. There is evidence to suggest that CT is not only the most accurate diagnostic modality for evaluating pneumoperitoneum but also has a far superior sensitivity in detecting bowel obstruction than plain radiographs.14–16 The proportion of patients undergoing x-ray was similar within both our study groups. Some patients waited almost 24 hours following x-ray before undergoing CT. We argue that these plain radiographs only served as a delay in those requiring further imaging and subsequent management; these patients should be proceeding directly to CT. Furthermore, obtaining a CT-confirmed diagnosis that requires surgical intervention earlier would allow for more appropriate CEPOD classification. Such patients could be classified accordingly (immediate, urgent or expedited) based on pathological findings, allowing for timelier intervention and earlier recovery for discharge.
Many UK institutions are increasingly adopting the use of Everlight Radiology (previously Radiology Reporting Online) – an off-site radiology requesting service that provides round the clock emergency CT reporting.17 It is important to appreciate that not all presentations require CT; cases of suspected cholecystitis can be easily diagnosed by ultrasonography. Unfortunately, ultrasonography is not readily available out of hours in most institutions and CT should be adopted as an alternative for these cases. CT provides an advantage over ultrasonography in obese patients or where gaseous distention limits the view.18 It also allows for better assessment of the complications of acute cholecystitis.19
Exclusion of same-day discharge patients was necessary as some admissions to the surgical assessment unit were either inappropriate (incorrect department) or equivocal and requiring no investigation or treatment. The greater problem with the elderly cohort arises through discharge planning,20 and the length of stay in some of our patients would have been influenced by social circumstances. Many are either living alone, resident in care homes or requiring packages of care that need reinstating. Relocation to such destinations often requires thorough planning and appropriate reassessment prior to discharge. Many elderly patients may even require rehabilitation placement for an interim period prior to returning home. Prolonged hospital stays and delayed discharges can affect patient mobility and independence, as well having broader financial implications for the trust.20
This study is limited by both its retrospective nature and small sample size. The inclusion of social circumstances and American Society of Anesthesiology grades would have provided a more comprehensive analysis of our patient cohort. Further work should aim to be prospectively gathered over a longer timeframe to eliminate these confounding factors. Despite these limitations, the authors feel that the frequency and use of radiological modalities within this study reflects contemporary surgical practice within a district general hospital and this study has emphasised the benefit of early CT in acutely unwell elderly patients. CT should be considered as a first-line investigation when elderly patients with an acute abdomen are admitted to surgical assessment units.
References
- 1.Office for National Statistics Statistical Bulletin: Population Estimates for UK, England and Wales, Scotland and Northern Ireland: Mid-2016. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/annualmidyearpopulationestimates/latest#uk-population-continues-to-age (cited December 2017).
- 2.World Health Organization Definition of an older or elderly person. http://www.who.int/ageing/en (cited December 2017).
- 3.National Cancer Intelligence Network . London: Public Health England; 2014. [Google Scholar]
- 4.National Confidential Enquiry into Patient Outcome and Death . London: NCEPOD; 2010. [Google Scholar]
- 5.Martinez JP, Mattu A. Abdominal pain in the elderly. 2006; : 371–388. [DOI] [PubMed] [Google Scholar]
- 6.Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. 2010; (3): 261–269.. [DOI] [PubMed] [Google Scholar]
- 7.Millet I, Alili C, Bouic-Pages E et al. . Acute abdominal pain in elderly patients: effect of radiologist awareness of clinicobiologic information on CT accuracy. 2013; (6): 1,171–1,179.. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health Emergency Admission to Hospital: Managing the Demand. HC 739 Session 2013–14. London: The Stationery Office; 2013. [Google Scholar]
- 9.Gardner CS, Jaffe TA, Nelson RC. Impact of CT in elderly patients presenting to the emergency department with acute abdominal pain. 2015; (7): 2,877–2,882. [DOI] [PubMed] [Google Scholar]
- 10.Hinson JS, Ehmann MR, Fine DM et al. . Risk of acute kidney injury after intravenous contrast media administration. 2017; (5): 577–586.e4. [DOI] [PubMed] [Google Scholar]
- 11.Freemantle N, Richardson M, Wood J et al. . Weekend hospitalization and additional risk of death: an analysis of inpatient data. 2012; (2): 74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker AS, Mason A, Quan TP et al. . Mortality risks associated with emergency admissions during weekends and public holidays: an analysis of electronic health records. 2017; (10089): 62–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maglinte DT, Reyes BL, Harmon BH et al. . Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. 1996; (6): 1,451–1,455. [DOI] [PubMed] [Google Scholar]
- 14.Gans SL, Stoker J, Boermeester MA. Plain abdominal radiography in acute abdominal pain; past, present, and future. 2012; : 525–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stapakis JC, Thickman D. Diagnosis of pneumoperitoneum: abdominal CT vs upright chest film. 1992; (5): 713–716. [PubMed] [Google Scholar]
- 16.Frager D, Medwid SW, Baer JW et al. . CT of small-bowel obstruction: value in establishing the diagnosis and determining the degree and cause. 1994; (1): 37–41. [DOI] [PubMed] [Google Scholar]
- 17.Everlight Radiology. https://www.everlightradiology.com/uk (cited December 2017).
- 18.Pinto A, Reginelli A, Cagini L et al. . Accuracy of ultrasonography in the diagnosis of acute calculous cholecystitis: review of the literature. 2013; (Suppl 1): S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reginelli A, Mandato Y, Solazzo A et al. . Errors in the radiological evaluation of the alimentary tract: part II. 2012; (4): 308–317. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health Discharging Older Patients from Hospital. HC 18 Session 2016–17. London: The Stationery Office; 2016. [Google Scholar]