Abstract
Introduction
This audit focused on patients who sustained enteric injury following blunt abdominal trauma.
Methods
Our prospectively maintained electronic registry was interrogated retrospectively, and all patients who had sustained blunt abdominal trauma between December 2011 and January 2016 were identified.
Results
Overall, 2,045 patients had sustained blunt abdominal trauma during the period under review. Seventy per cent were male. The median age was 28 years.
Sixty patients (2.9%) sustained a small bowel injury (SBI). Thirty-five of these were peritonitic on presentation. All patients with a SBI had a chest x-ray and free air was present in seven. In 18 patients with a SBI, computed tomography (CT) was performed, which revealed isolated free fluid in 12 and free intraperitoneal air in 5. In five cases, the CT was normal. A total of 32 patients (1.5%) sustained blunt duodenal trauma (BDT). All patients with BDT had a chest x-ray on presentation. Free intraperitoneal air was not present in any. CT was performed on 17 patients with BDT. This revealed isolated free fluid or retroperitoneal air in 12. The median delay between injury and presentation for these enteric injures was 15.5 hours (interquartile range [IQR]: 8–25 hours) while between presentation at hospital and operation, the median delay was 6 hours (IQR: 3–13 hours).
Conclusions
Blunt trauma related enteric hollow visceral injury remains associated with delayed diagnosis and significant morbidity. It can be caused by a disparate array of mechanisms and is difficult to diagnose even with modern imaging strategies.
Keywords: Blunt abdominal trauma, Blunt enteric injury, Blunt small bowel injury, Blunt duodenal injury
Blunt abdominal trauma (BAT) may result in injuries to both solid and enteric viscera. These two groups present in broadly different manners.1–6 Usually, solid visceral injuries involve the spleen and liver, and present with signs and symptoms of internal haemorrhage. Enteric injuries, however, are more indolent in their presentation, and manifest with peritonitis and sepsis.1,3,5,6
The enteric structures at risk for injury following BAT include the small bowel and the duodenum. The management of blunt small bowel injuries (SBIs) is made challenging by the fact that they are very often occult in nature and difficult to detect. This results in both delayed diagnosis and delayed management, which in turn translates into increased morbidity.7 Blunt duodenal trauma (BDT) is another uncommon but serious blunt enteric injury. BDT is notoriously difficult to diagnose clinically as the duodenum is a retroperitoneal structure and clinical signs do not become manifest early.2 For this reason, similar to SBI, BDT is also associated with delayed diagnosis and management, and therefore increased morbidity.8 Establishing the diagnosis relies on a policy of aggressive imaging based on mechanism of injury and clinical findings. Once diagnosed, the surgical management of BDT is also controversial.
This audit reviewed all the patients who sustained BAT in our service, with a particular focus on those who sustained a blunt SBI or BDT. The aim was to better define the nature of the pathology, and to refine the diagnostic approaches and management strategies for these injuries.
Management
All trauma patients are managed according to Advanced Trauma Life Support® principles. Chest x-ray is mandatory. Unstable patients are subjected to extended focused assessment with sonography for trauma (eFAST) and if free intra-abdominal fluid is identified, they are expedited to the operating room. All patients who respond to resuscitation are reassessed and selectively investigated with abdominal computed tomography (CT). Free air or significant unexplained free intra-abdominal fluid are indications for surgery.
Surgical management
SBIs are managed on their individual merits. Duodenal injuries are graded operatively using the American Association for the Surgery of Trauma (AAST) system (Table 1). Our management principles are to perform a primary duodenal repair using interrupted suturing and to leave a paraduodenal drain. A feeding tube is passed beyond the injury and secured with a nasal halter. A pyloric exclusion and gastroenterostomy (PEG) procedure is used selectively if there is excessive delay or if there is a large duodenal wall defect and combined pancreatic injury.
Table 1.
American Association for the Surgery of Trauma grading of small bowel injury and duodenal trauma
| Grade | Small bowel | Duodenum |
| I | Contusion or haematoma without devascularisation; partial-thickness laceration, no perforation | Single segment haematoma; partial-thickness laceration, no perforation |
| II | Laceration <50% of circumference | Multiple segment haematoma; laceration <50% of circumference |
| III | Laceration ≥50% of circumference without transection | Laceration 50–75% of circumference of D2, or 50–100% of D1, D3 or D4 |
| IV | Complete transection of the small bowel | Laceration >75% of circumference of D2, or rupture of ampulla or distal common bile duct |
| V | Transection of the small bowel with segmental tissue loss; devascularised segment | Massive duodenopancreatic injury; devascularisation of duodenum |
Methods
This was a retrospective review of a prospectively maintained electronic registry undertaken at the Pietermaritzburg Metropolitan Trauma Service (PMTS). Ethical approval for this study and for maintenance of the registry was granted by the Biomedical Research Ethics Committee of the University of Kwa Zulu-Natal. The PMTS provides definitive trauma care to the city of Pietermaritzburg, the capital of Kwa Zulu-Natal province. The electronic registry was reviewed for a four-year period (January 2011 – December 2014) and all patients who had sustained BAT were identified.
Results
Overall, 2,045 patients sustained BAT during the period under review. Seventy per cent were male. The median age was 28 years. Table 2 summarises the mechanisms of injury in our cohort. A total of 267 patients (13%) required a laparotomy for BAT.
Table 2.
Mechanism of injury for blunt abdominal trauma (BAT)
| Mechanism | All BAT patients (n=2,045) | Small bowel injury (n=60) | Duodenal injury (n=32) |
| Motor vehicle collision | 741 (36.2%) | 27 (45.0%) | 12 (37.5%) |
| Pedestrian–vehicle collision | 546 (26.7%) | 8 (13.3%) | 6 (18.8%) |
| Assault | 465 (22.7%) | 13 (21.7%) | 10 (31.3%) |
| Accidental fall | 137 (6.5%) | 6 (10.0%) | 3 (9.4%) |
| Structural collapse | 34 (1.6%) | ||
| Agricultural accident | 31 (1.5%) | ||
| Motorcycle collision | 27 (1.3%) | ||
| Bicycle related | 14 (0.6%) | 2 (3.3%) | |
| Sport related | 12 (0.6%) | 2 (3.3%) | 1 (3.1%) |
| Animal related | 8 (0.4%) | 2 (3.3%) | |
| Unspecified | 30 (1.5%) |
Blunt small bowel injury
Sixty patients (2.9%) were identified with SBIs. On presentation, the mean heart rate was 106bpm, the mean systolic blood pressure was 117mmHg and the mean lactate was 5.2mg/dl. Thirty-five patients were peritonitic on presentation. All patients had a chest x-ray and free air was present in seven cases. In 18 patients, CT was performed. This revealed isolated free fluid in 12 and free intraperitoneal air in 5 patients. In five cases, CT was normal.
Blunt duodenal trauma
Thirty-two patients (1.5%) had BDT. On presentation, the mean heart rate was 104bpm, the mean systolic blood pressure was 111mmHg and there was a mean base deficit of -5.2mEq/l. All patients had a chest x-ray on presentation. However, free intraperitoneal air was not present in any. In two patients, eFAST was performed, with free fluid being present in only one. CT was performed in 17 cases. This revealed isolated free fluid or retroperitoneal air in 12 patients. Figure 1 shows free retroperitoneal air in a young boy who was driven over by a tractor and sustained a duodenal injury.
Figure 1.
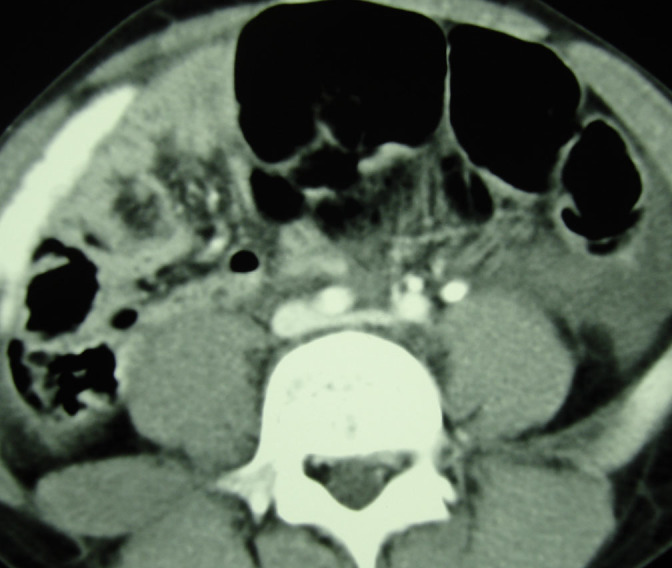
Retroperitoneal air following blunt duodenal injury in an 8-year-old boy who was driven over by a tractor
Delay
The median delay between injury and presentation for these enteric injures was 15.5 hours (interquartile range [IQR]: 8–25 hours). The median delay between presentation at hospital and operation was 6 hours (IQR: 3–13 hours).
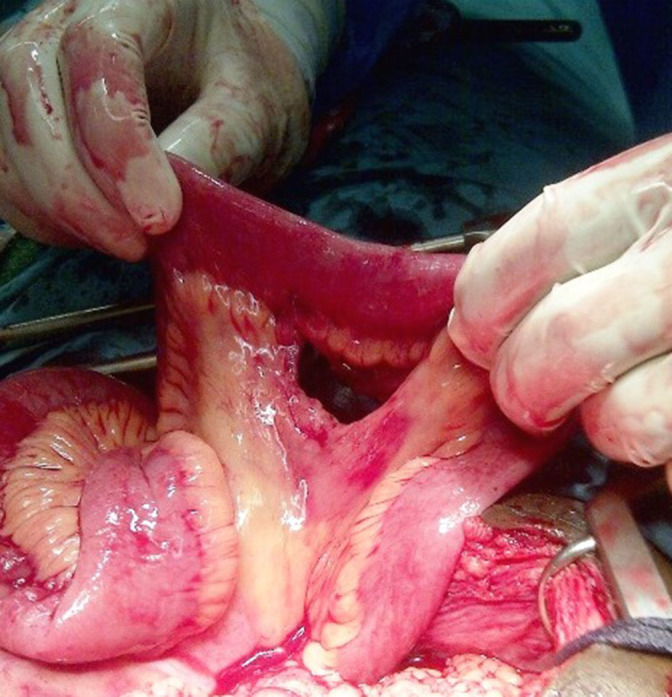
Operative management of small bowel injuries
There were 60 small bowel perforations. Figure 2 shows a single small bowel perforation. There were 19 mesenteric tears, of which 17 were associated with an ischaemic segment of small bowel. Figures 3 and 4 depict mesentery tears: one with an ischaemic segment of small bowel and the other with a well perfused segment. There were 45 jejunal and 15 ileal injuries.
Figure 2.

Small bowel perforation following blunt abdominal trauma
Figure 3.
Mesenteric defect following blunt abdominal trauma with a perfused segment of small bowel
Figure 4.

Large mesenteric defect following blunt abdominal trauma with an ischaemic segment of small bowel
The management was a primary resection in 13 cases, a stoma in 2, damage control ligation in 3 and minor mesenteric injuries were simply repaired in 2 patients. All the other perforations were repaired primarily. Extensive four quadrant sepsis was present in 18 (30%) of the 60 patients and 12 patients (20%) required at least one repeat laparotomy. Associated intra-abdominal injuries included the liver (n=9), spleen (n=8), large bowel (n=7), pancreas (n=6), bladder (n=5), duodenum (n=4), diaphragm (n=3), stomach (n=1), kidney (n=1) and urethra (n=1). There was also an intra-abdominal vascular injury. In 25% of cases, temporary abdominal closure was required. Thirty patients required intensive care unit (ICU) admission and five died (8%).
Operative management of duodenal injuries
Of the 32 duodenal injuries, 11 were to the first part of the duodenum, 2 to the second part, 15 to the third part and 4 to the fourth part. Ten patients had AAST grade I, nineteen had grade II and three had grade III injuries. There were no grade IV or V injuries. Associated injuries included small bowel (n=9), large bowel (n=2), liver (n=10), gallbladder (n=2), bladder (n=9), kidney (n=2) and spleen (n=1). These were managed on their merits.
The management for the AAST grade I injuries was paraduodenal drainage and serosal repair. Primary repair was undertaken in the remaining cases. A six-year old boy, who had been beaten by his foster parents three days earlier and who presented with peritonitis, was found at laparotomy to have a 75% disruption of the second part of his duodenum and extensive retroperitoneal sepsis. He was managed with a PEG procedure. A 36-year-old man, who was struck in the abdomen with a brick, was found to have a large disruption of the second part of his duodenum and he also underwent a PEG procedure. Both of these patients recovered uneventfully. There were no duodenal leaks. Twenty patients required ICU admission. Complications in the BDT group included respiratory complications (n=6) and renal failure (n=3). Three patients died although none of the deaths were related to the duodenal injury.
Discussion
Blunt small bowel injury
This injury is uncommon and most of the literature on the topic consists of either individual case studies or multicentre trauma registry reviews.3–6,9 The incidence of blunt SBI in patients with BAT is low; in our series it was 2.9%. In a large multicentre study from the US, out of 227,972 blunt injury patients, only 2,632 (1.2%) sustained a hollow viscus injury.5 The authors estimated that SBI was present in less than 0.3% of blunt admissions. The slightly higher incidence in our series reflects the high incidence of motor vehicle related trauma and poor compliance with safety legislation in Southern Africa.10
As was also shown in our series, mortality and morbidity is high for blunt SBI. This is because blunt SBI is associated with long delays between injury and diagnosis. The atypical and occult nature of these injuries is demonstrated by the diverse mechanisms of injury in our series. While half of the mechanisms were vehicle related, the remainder were associated with assaults and falls, and then with sport and farming. It is important that emergency staff understand that atypical or ‘freak’ accidents can result in significant and life threatening injuries. The common feature of all these mechanisms is a sharp, sudden force applied to the abdomen.3–6
There are two distinct injury patterns seen with this pathology. The first pathophysiology occurs when a knuckle of small bowel is caught between the blunt object, striking the abdomen and a rigid structure such as the vertebral body. This sudden dramatic increase in intraluminal pressure results in a free perforation (Fig 2).
The other mechanism involves a rapid acceleration and deceleration of the small bowel along the mesentery, precipitating a tear in the mesentery. If the tear is full-thickness through the mesentery, it leads to complete disruption of the blood supply to the overlying segment of small bowel. This results in an ischaemic segment of small bowel. The initial presentation is benign as there is no spillage of enteric contents and the patient does not develop peritonitis. In addition, the luminal continuity of the bowel is maintained. The operative photographs in Figures 3 and 4 show these mesenteric tears. Only as the segment becomes ischaemic do the clinical symptoms increase in severity. The patient eventually develops features of a small bowel obstruction and ischaemic bowel. These two mechanisms were present in our study in the ratio of 1:2 (19:41).
The morbidity associated with these injuries is high. Half of the patients required ICU admission and a quarter required temporary abdominal closure. This is a direct result of the delay in recognition with concomitant four quadrant sepsis.3–7 The reason for this delayed recognition is unclear. It has been shown repeatedly that clinical examination of the abdomen is unreliable in blunt trauma and the best way to assess these patients is modern CT.1,9,11,12 However, even with aggressive imaging, establishing the diagnosis of a blunt enteric injury is difficult.
The Eastern Association for the Surgery of Trauma used pooled data from 95 trauma centres over a 2-year period to match patients with a blunt SBI by age and injury severity score with equivalent blunt trauma patients who did not have a SBI.9 Logistic regression models were then employed to attempt to differentiate blunt trauma victims with SBI from those without such an injury. A significant percentage (13%) of patients with a blunt SBI had normal CT. This is similar to our experience, in which 28% of CT scans in patients with proven SBI were reported as negative.
Blunt duodenal trauma
The diagnosis of BDT is challenging as the retroperitoneal position of the duodenum means that enteric leakage does not precipitate peritonitis.2,8 Raised serum amylase is suggestive of a pancreatic or duodenal injury but is non-specific. Imaging techniques that assess the peritoneal cavity (eg sonar or plain radiology) are of limited use. The mainstay of imaging in these patients remains contrast enhanced CT.11,12 Free air or extravasation of contrast in the retroperitoneum is suggestive of duodenal injury. Nevertheless, even contrast CT has been reported to have a significant rate of false negative results and only 70% of the CT scans performed in our series confirmed the diagnosis of BDT. Figure 1 shows retroperitoneal air visualised on CT. This patient was an eight-year-old boy who fell asleep under a tractor that subsequently drove over his abdomen. He had a duodenal perforation, which was repaired primarily at laparotomy, and recovered uneventfully.
BDT is different to penetrating duodenal trauma and the grade of injury is usually less severe. There were no AAST grade IV or V injuries in our series. Combined pancreatic duodenal injuries are a distinct entity and require a more aggressive strategy. These methods involve damage control and wide drainage of the injury followed by formal pancreaticoduodenectomy once the patient has been stabilised.13,14 BDT generally results in a grade II or III injury and does not therefore usually require such complex surgery. The most serious complication of BDT is a breakdown of the repair with duodenal leak and retroperitoneal sepsis.
A number of strategies have evolved to try and prevent this, and the common theme is that they all attempted to divert the flow of physiological secretions from the repair. In the 1070s, Stone and Fabian described the ‘triple tube ostomy’, which consisted of a tube duodenostomy, a tube gastrostomy and a feeding jejunostomy.15 This is a technically simple procedure, and diverts all gastric and pancreatic secretions. In 1974 Berne et al advocated ‘diverticulisation’ of the duodenum to divert the stream of secretions.16 The complexity of this technique has made it anachronistic in modern trauma care. In 1977 Vaughan et al described the use of the pyloric exclusion and gastrojejunostomy, which achieved the same objective as Berne et al’s diverticulisation with a less complex operation.17 However, the trend in the contemporary literature has consistently been away from complexity towards a more simple technique.14,18–21
Our findings are very much in keeping with these trends. This minimalistic approach is especially relevant to AAST grade I injuries. If diagnosed on CT, they can be managed successfully without surgery. At operation, there is no need to open the serosa and evacuate the haematoma provided there is no biliary staining of the retroperitoneum. This is the approach we adopted and there were no duodenal leaks in our cohort.
Almost all other BDT related injuries can be managed safely by primary repair and paraduodenal drainage. PEG procedures may still be appropriate in more severe injuries with delay and associated retroperitoneal sepsis. Nevertheless, its role is increasingly restricted in the modern literature. Major surgical resections should be reserved for severe combined pancreatic and duodenal injuries, which are more common in penetrating trauma. These should never be undertaken in the acute setting but as part of the definitive surgical phase of a damage control strategy.
Conclusions
Blunt enteric trauma is an insidious entity that remains associated with delayed diagnosis and significant morbidity. It can be caused by a disparate array of mechanisms and is difficult to diagnose even with modern imaging strategies. Aggressive imaging of patients with BAT, and a low threshold for operation remain the key to reducing delays in diagnosis and surgery. The surgical approach to these injuries should be a minimalistic one and complex operative strategies should be eschewed.
References
- 1.Howes N, Walker T, Allorto NL et al. . Laparotomy for blunt abdominal trauma in a civilian trauma service. 2012; : 30–32. [PubMed] [Google Scholar]
- 2.Sriussadaporn S, Pak-art R, Sriussadaporn S, Kritayakirana K. Management of blunt duodenal injuries. 2004; : 1,336–1,342. [PubMed] [Google Scholar]
- 3.Watts DD, Fakhry SM. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the EAST multi-institutional trial. 2003; : 289–294. [DOI] [PubMed] [Google Scholar]
- 4.Kemmeter PR, Hoedema RE, Foote JA, Scholten DJ. Concomitant blunt enteric injuries with injuries of the liver and spleen: a dilemma for trauma surgeons. 2001; : 221–225. [PubMed] [Google Scholar]
- 5.Bloom AI, Rivkind A, Zamir G et al. . Blunt injury of the small intestine and mesentery –the trauma surgeon’s Achilles heel? 1996; : 85–91. [DOI] [PubMed] [Google Scholar]
- 6.Nolan BW, Gabram SG, Schwartz RJ, Jacobs LM. Mesenteric injury from blunt abdominal trauma. 1995; : 501–506. [PubMed] [Google Scholar]
- 7.Fakhry SM, Brownstein M, Watts DD et al. . Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. 2000; : 408–414. [DOI] [PubMed] [Google Scholar]
- 8.Allen GS, Moore FA, Cox CS et al. . Delayed diagnosis of blunt duodenal injury: an avoidable complication. 1998; : 393–399. [DOI] [PubMed] [Google Scholar]
- 9.Fakhry SM, Watts DD, Luchette FA. Current diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trial. 2003; : 295–306. [DOI] [PubMed] [Google Scholar]
- 10.Parkinson F, Kent S, Aldous C et al. . Road traffic crashes in South Africa: the burden of injury to a regional trauma centre. 2013; : 850–852. [DOI] [PubMed] [Google Scholar]
- 11.Oosthuizen GV, Bruce JL, Bekker W et al. . Pan computed tomography for blunt polytrauma: are we doing too many? 2016; : 801–803. [DOI] [PubMed] [Google Scholar]
- 12.Kong VY, Jeetoo D, Naidoo LC et al. . Isolated free intra-abdominal fluid on CT in blunt trauma: the continued diagnostic dilemma. 2015; : 357–359. [DOI] [PubMed] [Google Scholar]
- 13.Blocksom JM, Tyburski JG, Sohn RL et al. . Prognostic determinants in duodenal injuries. 2004; : 248–255. [PubMed] [Google Scholar]
- 14.Degiannis E, Boffard K. Duodenal injuries. 2000; : 1,473–1,479. [DOI] [PubMed] [Google Scholar]
- 15.Stone HH, Fabian TC. Management of duodenal wounds. 1979; : 334–339. [DOI] [PubMed] [Google Scholar]
- 16.Berne CJ, Donovan AJ, White EJ, Yellin AE. Duodenal ‘diverticulization’ for duodenal and pancreatic injury. 1974; : 503–507. [DOI] [PubMed] [Google Scholar]
- 17.Vaughan GD, Frazier OH, Graham DY. The use of pyloric exclusion in the management of severe duodenal injuries. 1977; : 785–790. [DOI] [PubMed] [Google Scholar]
- 18.DuBose JJ, Inaba K, Teixeira PG et al. . Pyloric exclusion in the treatment of severe duodenal injuries: results from the National Trauma Data Bank. 2008; : 925–929. [DOI] [PubMed] [Google Scholar]
- 19.Seamon MJ, Pieri PG, Fisher CA et al. . A ten-year retrospective review: does pyloric exclusion improve clinical outcome after penetrating duodenal and combined pancreaticoduodenal injuries? 2007; : 829–833. [DOI] [PubMed] [Google Scholar]
- 20.Kashuk JL, Moore EE. Should pyloric exclusion for duodenal and pancreatico-duodenal injuries be abandoned? 2007; : 452–453. [DOI] [PubMed] [Google Scholar]
- 21.Degiannis E, Krawczykowski D, Velmahos GC et al. . Pyloric exclusion in severe penetrating injuries of the duodenum. 1993; : 751–754. [DOI] [PubMed] [Google Scholar]


