Abstract
Objective
In the present meta-analysis, we test the technical and relational hypotheses of Motivational Interviewing (MI) efficacy. We also propose an a priori conditional process model where heterogeneity of technical path effect sizes should be explained by interpersonal/relational (i.e., empathy, MI Spirit) and intrapersonal (i.e., client treatment seeking status) moderators.
Method
A systematic review identified k = 58 reports, describing 36 primary studies and 40 effect sizes (N = 3025 participants). Statistical methods calculated the inverse variance-weighted pooled correlation coefficient for the therapist to client and the client to outcome paths across multiple target behaviors (i.e., alcohol use, other drug use, other behavior change).
Results
Therapist MI-consistent skills were correlated with more client change talk (r = .55, p < .001) as well as more sustain talk (r = .40, p < .001). MI-inconsistent skills were correlated with more sustain talk (r = .16, p < .001), but not change talk. When these indicators were combined into proportions, as recommended in the Motivational Interviewing Skill Code, the overall technical hypothesis was supported. Specifically, proportion MI consistency was related to higher proportion change talk (r = .11, p = .004) and higher proportion change talk was related to reductions in risk behavior at follow up (r = −.16, p < .001). When tested as two independent effects, client change talk was not significant, but sustain talk was positively associated with worse outcome (r = .19, p < .001). Finally, the relational hypothesis was not supported, but heterogeneity in technical hypothesis path effect sizes was partially explained by inter- and intra-personal moderators.
Conclusions
This meta-analysis provides additional support for the technical hypothesis of MI efficacy; future research on the relational hypothesis should occur in the field rather than in the context of clinical trials.
Keywords: motivational interviewing, change talk, sustain talk, technical hypothesis, relational hypothesis, conditional process model
Introduction
Outcome research on Motivational Interviewing (MI) has demonstrated efficacy and effectiveness across a range of behavior change outcomes, most notably alcohol and other drug use (Hettema, Steele, & Miller, 2005; Lundahl & Burke, 2009; Lundahl et al., 2013). To understand how MI produces clinical benefit, there has been a significant increase in MI process research. “Therapy process research investigates what happens in therapy sessions and how these interactions influence outcomes” (McLeod, Islam, & Wheat, 2013; p.142). Early work showed that the confrontational methods of the therapist were associated with higher client resistance and lower client engagement in contrast to a client-centered approach to alcohol treatment (Miller, Benefield, & Tonigan, 1993). In 2003, Amrhein and colleagues found that client commitment statements, in the later portion of an MI session, predicted client status as a treatment responder 12 months later. Support for these two paths, from therapist technique to client mechanisms and from client mechanisms to client outcomes, laid the groundwork for over a decade of MI process research that followed. Concurrently, there was a shift in the psychological and public health literature. Specifically, the National Institutes of Health (NIH) now call for research not just on if behavioral treatment works, but also on how specific mechanisms affect behavior change (NIH Common Fund, 2016).
The primary goal of process research is to derive empirically-based guidelines for clinical delivery, therapist training and supervision, and agency implementation in already evidence based treatments (Magill & Longabaugh, 2013). Thus far, our understanding of exactly how MI works remains elusive, and this is particularly concerning given the pervasive dissemination of MI into community-based settings. Recently, Magill and colleagues (2014) conducted the first meta-analysis of a key component of the theorized causal process model of MI efficacy – the technical hypothesis (Arkowitz, Miller, Westra, & Rollnick, 2008; Miller & Rose, 2009). This initial review, based on published data from 12 primary studies, found support for five of seven hypothesized paths. Briefly, the MI consistent skills of the therapist (e.g., open questions, simple and complex reflections, affirmations) were related to client statements in favor of behavior change (i.e., change talk), and the balance of client statements for and against change (i.e., a composite variable of change and sustain talk) was related to outcomes at follow up. Inconsistent with the technical hypothesis, MI-consistent skills were related not only to more change talk, but also more sustain talk, suggesting that MI explores positive and negative aspects of ambivalence rather than focusing solely on eliciting statements in favor of change. Finally, sustain talk alone was a significant predictor of worse outcome, but change talk alone did not predict positive behavior change (Magill et al., 2014).
The prior MI process meta-analysis answered some questions, raised others, and did not test the second key component of the MI process model – the relational hypothesis (i.e., therapist empathy and MI Spirit will be associated with client behavior change; Arkowitz et al., 2008; Miller & Rose, 2009). A more recent systematic review of 37 studies included findings related to both technical and relational paths (Romano & Peters, 2016). This review, based on reported data in published and dissertation studies, showed support for two of seven proposed pathways and “mixed support” for the remaining five pathways. The review supported the link between change talk and behavior change at follow up. While a qualitative, systematic review, offers the advantage of allowing for a more complex story than a quantitative review that utilizes averages, reliance on published and available data may result in publication bias when primary studies do not report all effect sizes regardless of statistical significance. In the case of Magill and colleagues (2014), only peer reviewed publications were reviewed, and missing data requests were made to primary study authors, yet, given the small sample and the rapid growth of this literature, Magill and colleagues’ (2014) work should be considered preliminary.
In the present meta-analysis, we test the full MI theoretical model to consider which pathways have support, under what conditions, and which, if any, require theoretical revision. We build on previous research in four major ways: 1) we incorporate a larger and more recent sample of MI process studies, 2) we include an expanded set of MI process measures, 3) we use raw MI process data derived from data requests to primary study authors, and 4) we test a more comprehensive aggregate path model of the MI processes of interest. In particular, one explanation for mixed findings reported in the literature is the MI process model does not invariably fit all clinical contexts. Therefore, we not only test the technical and relational hypotheses (Miller & Rose, 2009), but also two a priori models (i.e., interpersonal and intrapersonal) of conditional process that combine technical, relational, and client-level factors. Under a conditional process model, the expectation is that mediation pathways hold under certain conditions and not others (Preacher, Rucker, & Hayes, 2007). In meta-analyses, the need for such a model is indicated by a statistically significant Q test for between study heterogeneity. For our conditional process models, we propose two non-directional hypotheses: 1) Therapist Relational Proficiency (interpersonal model, i.e., average vs good empathy or MI Spirit) will explain between study, effect size variability at the a path (i.e., therapist skills to client language) of the technical hypothesis and 2) Client Treatment-Seeking Status (intrapersonal model, i.e., seeking treatment vs not seeking treatment for behavior change) will explain between study, effect size variability at the b path (i.e., client language to outcome) of the technical hypothesis. The notion that technical path effect sizes could be moderated by interpersonal and intrapersonal factors is consistent with a personalized medicine framework (Collins & Varmus, 2015) and a recognition that mechanisms of behavior change are not ‘one size fits all’ (Tonigan, 2016).
Method
Study Inclusion
The studies meeting inclusion for this meta-analysis were MI process studies, written in English, and published/in press in peer-reviewed journals between January 2000 and June of 2016. Qualifying interventions employed MI principles and techniques, as defined by Miller and Rollnick, (1991, 2002, 2013) and as measured by MI fidelity and/or process measures (e.g., Motivational Interviewing Skill Code). Commonly included versions of MI were single-session MI, Motivational Enhancement Therapy (MET; four sessions), and other Brief Motivational Interventions (e.g., Brief Alcohol Screening and Intervention for College Students (BASICS; Dimeff, 1999), Screening, Brief Intervention, and Referral to Treatment (SBIRT), and Group Motivational Interviewing (GMI)). Interventions were delivered to voluntary research participants, individuals seeking treatment, those opportunistically recruited (e.g., emergency departments), or those mandated (e.g., college/university campus alcohol violation) to a behavior change program. To be maximally inclusive of relevant studies, the target population was individuals aged 14 and over, experiencing problems with alcohol, other drug use, or other areas of behavior change (e.g., gambling, sexual risk behavior, poor diet). Finally, all included studies applied observational coding methods (e.g., Houck, Moyers, Miller, Glynn, & Hallgren, 2010; Martin, Moyers, Houck, Christopher, & Miller, 2005; Miller, 2000; Miller, Moyers, Ernst, & Amrhein, 2003; Miller, Moyers, Ernst, & Amrhein, 2008; Miller, Moyers, Manuel, Christopher, & Amrhein, 2008) to the study of MI within-session process. While studies using the Motivational Interviewing Treatment Integrity Scale (Moyers, Martin, Manuel, Miller, & Ernst, 2003; Moyers, Martin, Manuel, Miller, & Ernst, 2007; Moyers, Martin, Manuel, Miller, & Ernst, 2010) were eligible, these studies must have used these data to examine one or more paths outlined in the MI process model as proposed by Miller and Rose (2009; see also Arkowitz et al., 2008).
Literature Search
A literature search to obtain all eligible studies was conducted through May of 2016. The first step was a database search in PsycINFO, PubMed, and Medline with keywords: “change talk”, “sustain talk”, “client speech”, “client language”, “change language”, “commitment language”, “motivational interviewing skills”, “motivational interviewing process”, “motivational interviewing mediators”, “motivational interviewing mechanisms”, “motivational interviewing ingredients”. The second step was a hand search of these studies’ reference lists, as well as pertinent review papers (e.g., Apodaca & Longabaugh, 2009; Arkowitz et al., 2008; Longabaugh, Magill, Morgenstern & Huebner, 2013; Magill et al., 2014; Miller & Rollnick, 2013; Miller & Rose, 2009, Romano & Peters, 2015; Romano & Peters, 2016) for: (1) additional keywords and (2) any missing studies. The final step was a call for in press papers to: (1) the first authors of derived studies, (2) identified experts in the area of MI process research, and (3) the MI International Network of Trainers. Figure 1 provides a pictorial summary of study inclusion, consistent with QUORUM guidelines (Moher et al., 1999). Study eligibility was determined by the first and fifth authors, with a consensus review of the final list of studies provide by the investigative team.
Figure 1.
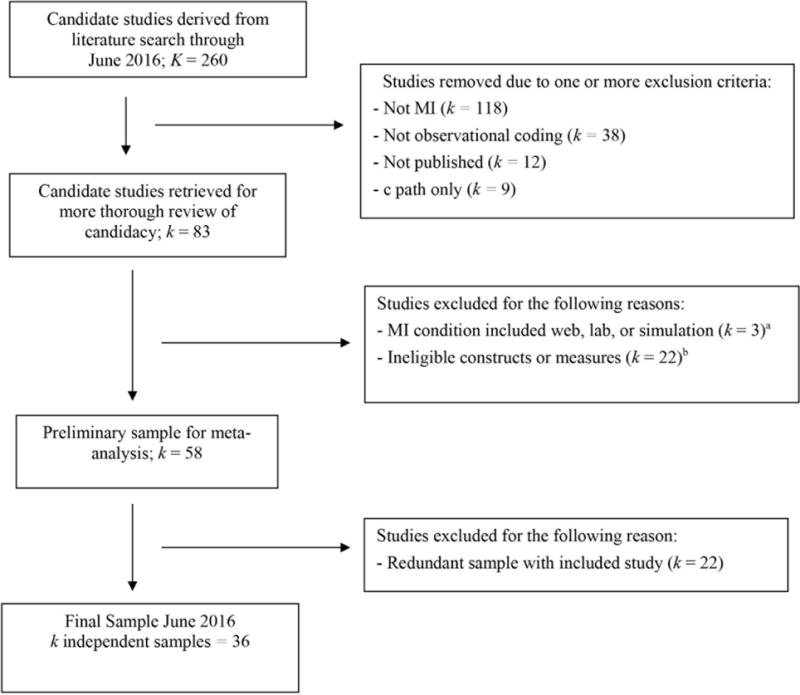
Flow of primary study inclusion.
Notes. K/k is defined as number of groups.
aFeldstein Ewing et al., 2011; Glynn & Moyers, 2010; Klonek et al., 2014.
bE.g. Laws et al., 2015 [Physicians as Counselors coding system, (PaCCS)]; Lord et al., 2015 [Language Style Synchrony (LSS)]
Data Extraction Methods
Study descriptor variables
Descriptors of primary study characteristics fell into four classes. First, Sample Demographic Factors included mean age, age group (i.e., adolescent, college/young adult, adult), percent female participants, percent Caucasian participants, percent African American participants, and percent Hispanic participants. Second, Sample Clinical Factors were treatment seeking vs. non-treatment seeking status and outcome type (i.e., alcohol, other drug or poly-drug, other behavior). Third, MI Implementation Factors were session time in minutes, MI type (i.e., MI/BMI, MET, BASICS, GMI, SBIRT), setting type (i.e., specialty mental health/substance setting, college campus, medical setting, other), manualization (i.e., flexibly delivered vs. manualized), and global relational scores (i.e., study-level proficiency cut-point for Global Empathy and MI Spirit [“average” vs. “good” or higher]). Finally, Study Methodological Factors were MI coding measure (i.e., process measure [e.g., Motivational Interviewing Skill Code] vs. fidelity measure [e.g., Motivational Interviewing Treatment Integrity Scale]), and data type (i.e., raw data directly from study author/s vs. extracted data from published report).
Data collection procedure
Each study was assigned an identification number that corresponded to descriptor codes and effect size data within study datasets. Primary study coding was conducted by trained research assistants using a combination of independent and consensus methods (i.e., first, fifth, and sixth authors). When descriptor data were missing from process study reports, the original clinical trial was consulted. For effect size data at Technical a (i.e., therapist skills to client language), Technical b (i.e., client language to client outcome), and Relational (i.e., Empathy and MI Spirit to outcome) paths, Pearson moment correlation matrices were requested from primary study authors. We elected to use raw correlation data, where possible, to reduce variability in statistical estimation (e.g., OLS regression vs. multi-level model) and covariate adjustment (i.e., bivariate vs. multivariate path effect sizes) as well as to increase the number of available effect sizes per measurement category, regardless of primary study reporting (i.e., to reduce publication bias). Each study author was provided a list of variable compute and correlation matrix syntax statements in their preferred software format (e.g., SPSS, STATA), and the response rate for these data requests was 94% (i.e., 34 of 36 independent samples). When data requests were not met, effect sizes were extracted from the published report and transformed using available formulae (e.g., t and p to r; Hunter & Schmidt, 2004; Lipsey & Wilson, 2001; Rosenthal, 1994). Research assistants performed all data entry, which was verified by a biostatistician staff member. All project methods are detailed in a study protocol available from the first author, and the Primary Study Coding Form is available as an online supplement.
Data-analysis
Overview of analyses
Descriptive analyses of primary study characteristics (i.e., means, standard deviations, medians, percentiles) were conducted. Next, we tested the unconditional MI technical and relational path models. If heterogeneity in a or b path effect sizes was observed, the proposed conditional process models were also tested. All additional diagnostics and sensitivity analyses are described below.
Technical and relational paths tested
The variables of interest to this review were those identified in established MI process coding systems (e.g., Houck et al., 2010; Miller et al., 2003; 2008a/b). These variables are typically measured as session-level frequency counts (i.e., MI consistent and inconsistent skills, change talk, sustain talk), but we have additionally included several proficiency indicators identified by the Motivational Interviewing Skill Code (i.e., proportion MI consistent [total MI consistent skills/total MI skills], proportion complex reflections [total complex reflections/total reflections], reflection to question ratio [total reflections/total questions], proportion change talk [total change talk/total change and sustain talk]). To test the technical hypothesis, path effect sizes were pooled for associations between therapist MI skills and client change language (seven a paths: MI consistent to change talk, MI consistent to sustain talk, MI inconsistent to change talk, MI inconsistent to sustain talk, proportion MI consistent to proportion change talk, proportion complex reflection to proportion change talk, reflection to question ratio to proportion change talk) and between client change language and client behavioral outcome (three b paths: change talk to outcome, sustain talk to outcome, and proportion change talk to outcome). To test the relational hypothesis, we pooled effect sizes for associations between two MI relational measures (i.e., Global Empathy and MI Spirit) and client behavioral outcome. We included outcomes (e.g., frequency, heavy frequency, other outcome) based on the primary target behavior (i.e., alcohol, other drug or poly-drug, other behavior) in the published report at the latest point within two clinically-informative timeframes (i.e., early follow up [0 to 6 months], late follow up [7 months or later]). Finally, the majority of studies reported outcomes in terms of reduction of a risk behavior (93%), and when studies reported positive outcomes (e.g., number of fruits and vegetables), these effects were reverse scored such that effect interpretation was consistent across primary studies.
Effect size, model of inference, sensitivity analyses
The effect size for the current study was the pooled correlation coefficient, which provides an inverse-variance-weighted indicator of the significance, strength, and direction of a bivariate relationship. All effect estimates were z-transformed for analyses and returned to the r metric for reporting purposes (Raudenbush & Bryk, 2002). The MI process paths were considered random effects from a distribution of studies with both known and unknown moderators of effect magnitude. This model of inference re-weights individual effect sizes by adding a constant that represents population variability, providing a more conservative estimate of significance and allowing broader generalization to the population of studies from which the effect sizes were drawn (Hedges & Vevea, 1998). Sensitivity analyses were conducted to assess the stability and homogeneity of all path effect sizes. First to assess stability, we re-pooled effects with ‘one-study-removed’, and presented trimmed estimates without influential studies (i.e., those that, if removed, would change the substantive conclusion regarding the significance, strength, and/or direction of the pooled effect size) when needed (Baujat, Mahe, Pignon, & Hill, 2002). We additionally present trimmed estimates in Tables 2–5 to assess the stability of pooled effect sizes with studies demonstrating less than “fair” (as defined by Landis & Koch, 1977) inter-rater reliability removed. Similarly, because technical and relational process could vary significantly in GMI versus one-to-one MI delivery, these studies (D’Amico, Houck, Hunter, Miles, Osilla, & Ewing, 2015; Shorey, Martino, Lamb, LaRowe, & Santa Ana, 2015) were removed in sensitivity analyses (reported in Tables 2–4). Second, the Q statistic tested for the presence of significant between-study heterogeneity, and when the Q value was statistically significant, a priori moderators were tested and a percentile estimate of between-study variance was provided (i.e., I2; Higgins & Thompson, 2002). For moderator analysis, conditional paths were re-pooled in sub-groups (i.e., by specific interpersonal, intrapersonal, and outcome factors) and the Q statistic and I2 were re-examined for reductions in unexplained, between-study variance. Overall, the aim was to derive homogeneous path effect sizes, and thus increase confidence the population of studies testing the relationships of interest had been fully specified. Analyses were conducted in Comprehensive Meta-Analysis v 2.0.
Table 2.
a and b path studies of the MI Technical Hypothesis – Change Talk
| a Path | b Path | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| First Author (date) | n | Session min.a | MI type | Effect Size (r) | Target Behavior | Follow-up Time point | Effect Size (r) |
| Apodaca (2013) | 195 | 49.98 | MI/BMI | alcohol | 0-6 mo | .05 | |
| MICO to CT - MI | .59*** | ||||||
| MIIN to CT - MI | .23** | ||||||
| MICO to CT - MI+SO | 167 | 47.26 | MI/BMI | .54*** | alcohol | 0-6 mo | .11 |
| MIIN to CT - MI+SO | .22** | ||||||
|
| |||||||
| Apodaca (2014) | 92 | 53.40 | MI/BMI | alcohol | 0-6 mo | −.01 | |
| MICO to CT | .47*** | ||||||
| MIIN to CT | .06 | ||||||
|
| |||||||
| Baer (2008) | 51 | 33.00 | MI/BMI | — | poly-drug | 0-6 mo | −.03 |
|
| |||||||
| Barnett (2014)b, c | 74 | 20.55 | MI/BMI | other drug | 7+ mo | −.10 | |
| MICO to CT | .56*** | ||||||
| MIIN to CT | .18 | ||||||
|
| |||||||
| Boardman (2006)d | 9 | 30.00 | MI/BMI | other drug | — | — | |
| MICO to CT | −.33 | ||||||
| MIIN to CT | −.34 | ||||||
| MICO to CT | 12 | 30.00 | MI/BMI | −.05 | nutrition | — | — |
| MIIN to CT | .12 | ||||||
|
| |||||||
| Borsari Site 1 (2015) | 91 | 46.93 | BASICS | alcohol | 0-6 mo | .14 | |
| MICO to CT | .66*** | ||||||
| MIIN to CT | .27* | ||||||
|
| |||||||
| Borsari Site 2 (2015) | 160 | 52.68 | BASICS | alcohol | 0-6 mo | −.07 | |
| MICO to CT | .62*** | ||||||
| MIIN to CT | −.21* | ||||||
|
| |||||||
| Campbell (2010) | 28 | 50.00 | MI/BMI | — | alcohol | 0-6 mo | −.17 |
|
| |||||||
| Catley (2006) | 86 | 30.00 | MI/BMI | other drug | — | — | |
| MICO to CT | .69*** | ||||||
| MIIN to CT | −.02 | ||||||
|
| |||||||
| D’Amico (2015) | 43 | 55.00 | GMI | — | poly-drug | 0-6 mo | −.13 |
|
| |||||||
| Davis (2015)e | 19 | 27.94 | MI/BMI | other drug | 0-6 mo | −.19 | |
| MICO to CT - MI | .36 | ||||||
| MIIN to CT - MI | −.07 | ||||||
| MICO to CT - MIF | 21 | 24.80 | MI/BMI | .75*** | other drug | 0-6 mo | .05 |
| MIIN to CT - MIF | .04 | ||||||
|
| |||||||
| Flickinger (2013)e | 27 | 28.04 | MI/BMI | sex risk | — | — | |
| MICO to CT | .83*** | ||||||
| MIIN to CT | .23 | ||||||
|
| |||||||
| Gaume (2008 a, b & 2009)c | 97 | 15.00 | MI/BMI | alcohol | 7+ mo | −.07 | |
| MICO to CT | .52*** | ||||||
| MIIN to CT | .05 | ||||||
|
| |||||||
| Gaume (2010 & 2013) | 149 | 25.00 | MI/BMI | alcohol | 0-6 mo | −.04 | |
| MICO to CT | .45*** | ||||||
| MIIN to CT | −.05 | ||||||
|
| |||||||
| Gaume (2016) | 208 | 25.00 | MI/BMI | alcohol | 0-6 mo | .23** | |
| MICO to CT | .48*** | ||||||
| MIIN to CT | −.07 | ||||||
|
| |||||||
| Hodgins (2009) | 40 | 32.30 | MI/BMI | — | gambling | 0-6 mo | −.06 |
|
| |||||||
| Kahler (2016) | 90 | 63.00 | MI/BMI | alcohol | 0-6 mo | .07 | |
| MICO to CT | .55*** | ||||||
| MIIN to CT | .35** | ||||||
|
| |||||||
| Kaplan (2013)c, e | 33 | 25.20 | MI/BMI | medication adherence | 0-6 mo | .02 | |
| MICO to CT | .11 | ||||||
| MIIN to CT | −.20 | ||||||
|
| |||||||
| Lee (2014)f | 41 | 60.00 | BASICS | alcohol | 0-6 mo | .23 | |
| MICO to CT | .64*** | ||||||
| MIIN to CT | −.11 | ||||||
|
| |||||||
| Moyers (2009) | 118 | 60.00 | MET | alcohol | 0-6 mo | .04 | |
| MICO to CT | .23* | ||||||
| MIIN to CT | .06 | ||||||
|
| |||||||
| Neighbors (2012)f | 22 | 60.00 | BASICS | alcohol | 0-6 mo | −.17 | |
| MICO to CT | .72*** | ||||||
| MIIN to CT | .08 | ||||||
|
| |||||||
| Pirlott (2012) | 43 | 45.00 | MI/BMI | nutrition | 7+ mo | −.33* | |
| MICO to CT | .61*** | ||||||
| MIIN to CT | −.04 | ||||||
|
| |||||||
| Roy-Byrne (2014)f | 70 | 30.00 | SBIRT | poly-drug | 0-6 mo | −.10 | |
| MICO to CT | .60*** | ||||||
| MIIN to CT | .05 | ||||||
|
| |||||||
| Shorey (2015) | 30 | 75.00 | GMI | alcohol | — | — | |
| MICO to CT | .70*** | ||||||
| MIIN to CT | — | ||||||
|
| |||||||
| Vader (2010)c | 30 | 45.00 | MI/BMI | alcohol | 0-6 mo | −.42* | |
| MICO to CT - MIF | .61*** | ||||||
| MIIN to CT - MIF | .23 | ||||||
| MICO to CT – MIO | 30 | 45.00 | MI/BMI | .50** | alcohol | 0-6 mo | .21 |
| MIIN to CT - MIO | −.16 | ||||||
Notes.
p < .001;
p < .005;
p < .05;
p < .10.
mo = month; wk = week; min = minutes; CT = change talk; MI = motivational interviewing; MICO = MI consistent; MIIN = MI inconsistent; MI+SO = MI with significant-other participation; MIF =MI with feedback; MIO = MI other. Removal of GMI studies did not result in substantive changes to pooled estimates.
Session length in minutes based on published report or target session length.
Effect sizes based on Barnett marijuana subsample N=74.
Trimmed estimate with study removed due to less than fair interrater reliability is (r = .05, 95% CI [−.03, .14]; p = .214, k = 20, Q < .05).
Boardman (2006) CT measure is the Vanderbilt Psychotherapy Process Scale (O’Malley et al., 1983) client engagement subscale.
Study used a measure other than MISC to code in-session behaviors [e.g. MITI 2.0 (Moyers et al., 2005), 3.0 (Moyers et al., 2007), 3.1.1 (Moyers et al., 2010), PEPA (Mastroleo, 2009)].
Included study as part of a larger observational measurement development project (Atkins et al., 2014).
Table 5.
Global path studies of the MI Technical Hypothesis
| First Author (date) | n | Session min.a | MI type | Target Behavior | Follow-up Time point | Effect Size (r) | |
|---|---|---|---|---|---|---|---|
| Apodaca (2013)b | 195 | 49.98 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome – MI | .04 | ||||||
| MI Spirit to Outcome – MI | −.03 | ||||||
| Empathy to Outcome - MI+SO | 167 | 47.26 | MI/BMI | alcohol | 0-6 mo | −.06 | |
| MI Spirit to Outcome - MI+SO | −.01 | ||||||
|
| |||||||
| Apodaca (2014)b | 92 | 53.40 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome | −.05 | ||||||
| MI Spirit to Outcome | −.03 | ||||||
|
| |||||||
| Bertholet (2014)/Saitz (2007) | 124 | 25.50 | MI/BMI | poly-drug | 7+ mo | ||
| Empathy to Outcome | .06 | ||||||
| MI Spirit to Outcome | .03 | ||||||
|
| |||||||
| Borsari Site 1 (2015) | 91 | 46.93 | BASICS | alcohol | 0-6 mo | ||
| Empathy to Outcome | −.28* | ||||||
| MI Spirit to Outcome | −.30* | ||||||
|
| |||||||
| Borsari Site 2 (2015) | 160 | 52.68 | BASICS | alcohol | 0-6 mo | ||
| Empathy to Outcome | −.13 | ||||||
| MI Spirit to Outcome | −.18* | ||||||
|
| |||||||
| Feldstein Ewing (2015)c | 65 | 60.00 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome | −.17 | ||||||
| MI Spirit to Outcome | −.18 | ||||||
|
| |||||||
| Gaume (2008 a, b & 2009) | 97 | 15.00 | MI/BMI | alcohol | 7+ mo | ||
| Empathy to Outcome | −.24* | ||||||
| MI Spirit to Outcome | −.16 | ||||||
|
| |||||||
| Gaume (2010 & 2013) | 149 | 25.00 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome | .06 | ||||||
| MI Spirit to Outcome | .04 | ||||||
|
| |||||||
| Gaume (2016) | 208 | 25.00 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome | .01 | ||||||
| MI Spirit to Outcome | .02 | ||||||
|
| |||||||
| Kahler (2016) | 90 | 63.00 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome | .07 | ||||||
| MI Spirit to Outcome | .09 | ||||||
|
| |||||||
| Kaplan (2013)c | 33 | 25.20 | MI/BMI | medication adherence | 0-6 mo | ||
| Empathy to Outcome | .28 | ||||||
| MI Spirit to Outcome | .31† | ||||||
|
| |||||||
| Knittle (2014) | 27 | 33.10 | MI/BMI | physical activity | 0-6 mo | ||
| Empathy to Outcome | −.09 | ||||||
| MI Spirit to Outcome | −.19 | ||||||
|
| |||||||
| Lee (2013)c, d | 47 | 60.00 | MI/BMI | other drug | 0-6 mo | ||
| Empathy to Outcome | .06 | ||||||
| MI Spirit to Outcome | .00 | ||||||
|
| |||||||
| Mastroleo (2014)c | 53 | 32.20 | BASICS | alcohol | 0-6 mo | ||
| Empathy to Outcome | .13 | ||||||
| MI Spirit to Outcome | .23 | ||||||
|
| |||||||
| McCambridge (2011)c | 73 | 27.00 | MI/BMI | other drug | 0-6 mo | ||
| Empathy to Outcome | .01 | ||||||
| MI Spirit to Outcome | −.13 | ||||||
|
| |||||||
| Pirlott (2012) | 43 | 45.00 | MI/BMI | nutrition | 7+ mo | ||
| Empathy to Outcome | −.19 | ||||||
| MI Spirit to Outcome | −.14 | ||||||
|
| |||||||
| Tollison (2008)c | 53 | 60.00 | BASICS | alcohol | 0-6 mo | ||
| Empathy to Outcome | .17 | ||||||
| MI Spirit to Outcome | −.01 | ||||||
|
| |||||||
| Tollison (2013)c | 302 | 52.50 | BASICS | alcohol | 0-6 mo | ||
| Empathy to Outcome | −.05 | ||||||
| MI Spirit to Outcome | .02 | ||||||
|
| |||||||
| Vader (2010) | 30 | 45.00 | MI/BMI | alcohol | 0-6 mo | ||
| Empathy to Outcome - MIF | −.34† | ||||||
| MI Spirit to Outcome - MIF | −.31 | ||||||
| Empathy to Outcome - MIO | 30 | 45.00 | MI/BMI | alcohol | 0-6 mo | −.05 | |
| MI Spirit to Outcome - MIO | .09 | ||||||
Notes.
p < .001;
p < .005;
p < .05;
p < .10.
mo = month; wk = week; min = minutes; CT = change talk; MI = motivational interviewing; MICO = MI consistent; MIIN = MI inconsistent; MI+SO = MI with significant-other participation; MIF =MI with feedback; MIO = MI other.
Session length in minutes based on published report or target session length.
Trimmed estimate with study removed due to less than fair interrater reliability is (r = −.04, 95% CI [−.10, .03]; p = .242, k = 18, Q > .05).
Study used a measure to code in-session behaviors other than MISC [e.g. MITI 2.0 (Moyers et al., 2005), 3.0 (Moyers et al., 2007), 3.1.1 (Moyers et al., 2010), PEPA (Mastroleo, 2009)].
Included study as part of a larger observational measurement development project (Atkins et al., 2014).
Table 4.
a and b path studies of the MI Technical Hypothesis – Proportion Change Talk Estimates
| a Path | b Path | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| First Author (date) | n | Session min.a | MI type | Effect Size (r) | Target Behavior | Follow-up Time point | Effect Size (r) |
| Amrhein (2003)b | 84 | 67.50 | MI/BMI | — | poly-drug | 7+ mo | −.16 |
|
| |||||||
| Apodaca (2013) | 195 | 49.98 | MI/BMI | alcohol | 0-6 mo | −.27*** | |
| ProMICO to ProCT – MI | .17* | ||||||
| ProREC to ProCT – MI | −.01 | ||||||
| QtoRratio to ProCT – MI | −.06 | ||||||
| ProMICO to ProCT - MI+SO | 167 | 47.26 | MI/BMI | .10 | alcohol | 0-6 mo | −.06 |
| ProREC to ProCT - MI+SO | .04 | ||||||
| QtoRratio to ProCT - MI+SO | −.03 | ||||||
|
| |||||||
| Apodaca (2014) | 92 | 53.40 | MI/BMI | alcohol | 0-6 mo | −.29* | |
| ProMICO to ProCT | −.24* | ||||||
| ProREC to ProCT | −.01 | ||||||
| QtoRratio to ProCT | −.07 | ||||||
|
| |||||||
| Barnett (2014)c | 74 | 20.55 | MI/BMI | other drug | 7+ mo | −.36*** | |
| ProMICO to ProCT | .16 | ||||||
| ProREC to ProCT | .11 | ||||||
| QtoRratio to ProCT | .04 | ||||||
|
| |||||||
| Borsari Site 1 (2015) | 91 | 46.93 | BASICS | alcohol | 0-6 mo | −.20 | |
| ProMICO to ProCT | −.28* | ||||||
| ProREC to ProCT | .01 | ||||||
| QtoRratio to ProCT | −.10 | ||||||
|
| |||||||
| Borsari Site 2 (2015) | 160 | 52.68 | BASICS | alcohol | 0-6 mo | −.14 | |
| ProMICO to ProCT | .18* | ||||||
| ProREC to ProCT | −.03 | ||||||
| QtoRratio to ProCT | .10 | ||||||
|
| |||||||
| Catley (2006) | 86 | 30.00 | MI/BMI | other drug | — | — | |
| ProMICO to ProCT | .13 | ||||||
| ProREC to ProCT | −.11 | ||||||
| QtoRratio to ProCT | .20† | ||||||
|
| |||||||
| D’Amico (2015) | 43 | 55.00 | GMI | — | poly-drug | 0-6 mo | −.13 |
|
| |||||||
| Davis (2015)b | 19 | 27.94 | MI/BMI | other drug | 0-6 mo | −.29 | |
| ProMICO to ProCT – MI | −.21 | ||||||
| ProREC to ProCT – MI | .09 | ||||||
| QtoRratio to ProCT – MI | −.48* | ||||||
| ProMICO to ProCT – MIF | 21 | 24.80 | MI/BMI | .17 | other drug | 0-6 mo | −.13 |
| ProREC to ProCT – MIF | .16 | ||||||
| QtoRratio to ProCT – MIF | −.39† | ||||||
|
| |||||||
| Flickinger (2013)b | 27 | 28.04 | MI/BMI | sex risk | — | — | |
| ProMICO to ProCT | .33* | ||||||
| ProREC to ProCT | .24 | ||||||
| QtoRratio to ProCT | .22 | ||||||
|
| |||||||
| Gaume (2008 a, b & 2009) | 97 | 15.00 | MI/BMI | alcohol | 7+ mo | −.01 | |
| ProMICO to ProCT | .24* | ||||||
| ProREC to ProCT | .06 | ||||||
| QtoRratio to ProCT | .05 | ||||||
|
| |||||||
| Gaume (2010 & 2013) | 149 | 25.00 | MI/BMI | alcohol | 0-6 mo | −.10 | |
| ProMICO to ProCT | .24** | ||||||
| ProREC to ProCT | .05 | ||||||
| QtoRratio to ProCT | −.02 | ||||||
|
| |||||||
| Gaume (2016) | 208 | 25.00 | MI/BMI | alcohol | 0-6 mo | .03 | |
| ProMICO to ProCT | .19* | ||||||
| ProREC to ProCT | .18* | ||||||
| QtoRratio to ProCT | .14* | ||||||
|
| |||||||
| Hodgins (2009) | 40 | 32.30 | MI/BMI | — | gambling | 0-6 mo | −.28† |
| Lee (2014)d | 41 | 60.00 | BASICS | alcohol | 0-6 mo | .04 | |
| ProMICO to ProCT | .28 | ||||||
| ProREC to ProCT | .25 | ||||||
| QtoRratio to ProCT | .02 | ||||||
|
| |||||||
| Kahler (2016) | 90 | 63.00 | MI/BMI | alcohol | 0-6 mo | −.03 | |
| ProMICO to ProCT | .02 | ||||||
| ProREC to ProCT | −.02 | ||||||
| QtoRratio to ProCT | .01 | ||||||
|
| |||||||
| Kaplan (2013)b | 33 | 25.20 | MI/BMI | medication adherence | 0-6 mo | .11 | |
| ProMICO to ProCT | −.01 | ||||||
| ProREC to ProCT | .22 | ||||||
| QtoRratio to ProCT | −.09 | ||||||
|
| |||||||
| Morgenstern (2012)b | 59 | 52.50 | MET | — | alcohol | 0-6 mo | −.20† |
|
| |||||||
| Moyers (2005) | 103 | 20.00 | MET | alcohol | — | — | |
| ProMICO to ProCT | .34** | ||||||
| ProREC to ProCT | .06 | ||||||
| QtoRratio to ProCT | .03 | ||||||
|
| |||||||
| Moyers (2009) | 118 | 60.00 | MET | alcohol | 0-6 mo | −.09 | |
| ProMICO to ProCT | .22* | ||||||
| ProREC to ProCT | — | ||||||
| QtoRratio to ProCT | .16† | ||||||
|
| |||||||
| Neighbors (2012)d | 22 | 60.00 | BASICS | alcohol | 0-6 mo | −.24 | |
| ProMICO to ProCT | .10 | ||||||
| ProREC to ProCT | .21 | ||||||
| QtoRratio to ProCT | .10 | ||||||
|
| |||||||
| Roy-Byrne (2014)d | 70 | 30.00 | SBIRT | poly-drug | 0-6 mo | −.14 | |
| ProMICO to ProCT | −.06 | ||||||
| ProREC to ProCT | .10 | ||||||
| QtoRratio to ProCT | .00 | ||||||
|
| |||||||
| Vader (2010) | 30 | 45.00 | MI/BMI | alcohol | 0-6 mo | −.70*** | |
| ProMICO to ProCT – MIF | .13 | ||||||
| ProREC to ProCT – MIF | .13 | ||||||
| QtoRratio to ProCT – MIF | .09 | ||||||
| ProMICO to ProCT – MIO | 30 | 45.00 | MI/BMI | −.11 | alcohol | 0-6 mo | −.11 |
| ProREC to ProCT – MIO | −.10 | ||||||
| QtoRratio to ProCT – MIO | .02 | ||||||
Notes.
p < .001;
p < .005;
p < .05;
p < .10.
mo = month; wk = week; min = minutes; ProCT = proportion of change talk; MI = motivational interviewing; ProMICO = proportion of MI consistent; ProREC = proportion of complex reflections; QtoRratio = question to reflection ratio; MI+SO = MI with significant-other participation; MIF =MI with feedback; MIO = MI other. Removal of GMI studies did not result in substantive changes to pooled estimates.
Session length in minutes based on published report or target session length.
Study used a measure other than MISC to code in-session behaviors [e.g. MITI 2.0 (Moyers et al., 2005), 3.0 (Moyers et al., 2007), 3.1.1 (Moyers et al., 2010), PEPA (Mastroleo, 2009)].
Effect sizes based on Barnett marijuana subsample N=74.
Included study as part of a larger observational measurement development project (Atkins et al., 2014).
Results
Sample of Primary Studies
A total of 58 reports described 36 primary studies that contributed 40 effect sizes and treated N = 3025 individuals. On average, study samples had 75 participants (SD = 61; median = 53). Study sample descriptor data are provided in Table 1. The majority of studies included adults and the mean age across samples was 30 (SD = 13; median = 25). Studies had primarily Caucasian samples, and racial or ethnic representation was 29% African American and 20% Hispanic/Latino, on average. These studies targeted mostly non-treatment seeking, alcohol or other drug users. The MI, MET, BASICS, GMI or SBIRT sessions ranged from 15 to 120 minutes in length (M = 42[SD = 15] minutes). Four studies examined MET (Campbell, Adamson, & Carter, 2010; Moyers, Miller, & Hendrickson, 2005; Moyers, Martin, Christopher, & Tonigan, 2009; Morgenstern et al., 2012) and therefore involved four therapy sessions. However, all effect estimates were derived from first or second session data since the large majority of studies (i.e., 95%) only measured process in these sessions. The MI interventions were primarily manualized, and there was a fairly equal distribution across setting types. Finally, across this sample of studies, global empathy and MI Spirit were “good” on average (M = 4.3[SD = .8] and M = 4.2[SD=.8], respectively)1.
Table 1.
Summary and reliability data on primary study descriptors
| Variable | Mean(SD) | Percent(k) |
|---|---|---|
| Demographic factors | ||
| Age | 30.3(13.4) | |
| Adult sample | 50.0(20) | |
| College/young adult sample | 33.3(13) | |
| Adolescent sample | 17.9(7) | |
| Percent female in sample | 41.4(20.1) | |
| Percent Caucasian | 56.2(29.0) | |
| Percent African American | 29.2(29.6) | |
| Percent Hispanic/Latino | 20.0(21.0) | |
| Clinical factors | ||
| Treatment seeking sample | 25.0(10) | |
| Non-treatment seeking sample | 75.0(30) | |
| Alcohol study | 52.5(21) | |
| Other drug study | 32.5(13) | |
| Other behavior study | 15.0(6) | |
| Implementation factors | ||
| Session time in minutes | 42.0(15.6) | |
| Motivational Interviewing (MI) | 62.5(25) | |
| Motivational Enhancement Therapy (MET) | 10.0(4) | |
| Brief Alcohol Screening Intervention for College Students (BASICS) | 17.5(7) | |
| Group Motivational Interviewing (GMI) | 5.5(2) | |
| Screening and Brief Intervention (SBIRT) | 5.5(2) | |
| Specialty mental health/substance use setting | 25.0(10) | |
| College setting | 30.0(12) | |
| Medical setting | 22.5(9) | |
| Other setting | 22.5(9) | |
| Flexibly delivered | 15.0(6) | |
| Manualized | 72.5(29) | |
| No report | 12.5 (5) |
Notes. k = number of groups. Total k is 36 primary studies contributing 40 effect sizes (Apodaca et al., 2013; Boardman et al. 2006; Davis et al., 2015; Vader et al., 2010 contributed two effect sizes). MI interventions were proficient, on average, with respect to MI Spirit and Empathy (M = 4.2(.8), M = 4.3(.7), respectively).
Tables 2 through 5 contain individual effect sizes, along with a selection of key primary study characteristics (i.e., sample size, session length in minutes, MI treatment type, target behavioral outcome, follow up time point).
Therapist MI Skills in Relation to Client Change Language – “a” path
Change talk frequency
The MI technical hypothesis proposes therapist use of MI consistent skills (e.g., open questions, simple and complex reflections, affirmations) will be associated with increased change talk and therapist use of MI inconsistent skills (e.g., confrontations, warnings, unsolicited advice) will be associated with decreased change talk. As can be seen in Table 2/left panel, the positive MI consistent skills to change talk path was supported across 21 primary studies that contributed 25 effect sizes (Apodaca, Magill, Longabaugh, Jackson, & Monti 2013; Boardman et al., 2006; Davis, Houck, Rowell, Benson, & Smith, 2015; Vader, Walters, Prabhu, Houck, & Field, 2010 examined two eligible MI conditions). Specifically, the inverse-variance weighted, pooled correlation coefficient was r = .55 (95% CI [.49, .60]; p < .001, Q < .05, I2 = 63%). For MI inconsistent therapist skills, the association with change talk was not significant (r = −.06, 95% CI [−.02, .13]; p = .118, k = 24, Q < .05, I2= 52%; Table 2/left panel).
Sustain talk frequency
The MI technical hypothesis proposes that MI consistent skills should be associated with decreased sustain talk, but we found a positive and significant random effects pooled correlation coefficient (r = .40, 95% CI [.32, .48]; p < .001, k = 23, Q < .05, I2= 75%; Table 3/left panel). When the path from MI inconsistent skills to increased sustain talk was examined, the effect estimate was consistent with theoretical expectations (r = .16, 95% CI [.08, .24]; p < .001, k = 23, Q < .05, I2= 65%; Table 3/left panel). In summary, a path frequency count measures showed MI consistent skills were associated with increased change and sustain talk, and MI inconsistent skills were associated with increased sustain talk, but not decreased change talk. A path pooled effect sizes for frequency count indicators showed between-study heterogeneity that was significant and “moderate” (52 to 75%; Higgins, Steele, & Miller, 2003).
Table 3.
a and b path studies of the MI Technical Hypothesis – Sustain Talk
| a Path | b Path | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| First Author (date) | n | Session min.a | MI type | Effect Size (r) | Target Behavior | Follow-up Time point | Effect Size (r) |
| Apodaca (2013) | 195 | 49.98 | MI/BMI | alcohol | 0-6 mo | .30*** | |
| MICO to ST - MI | .48*** | ||||||
| MIIN to ST - MI | .23** | ||||||
| MICO to ST – MI+SO | 167 | 47.26 | MI/BMI | .45*** | alcohol | 0-6 mo | .23** |
| MIIN to ST – MI+SO | .33*** | ||||||
|
| |||||||
| Apodaca (2014) | 92 | 53.40 | MI/BMI | alcohol | 0-6 mo | .28* | |
| MICO to ST | .36*** | ||||||
| MIIN to ST | −.15 | ||||||
|
| |||||||
| Baer (2008) | 51 | 33.00 | MI/BMI | — | poly-drug | 0-6mo | .19 |
|
| |||||||
| Barnett (2014)b, c | 74 | 20.55 | MI/BMI | other drug | 7+ mo | .33*** | |
| MICO to ST | .39** | ||||||
| MIIN to ST | .19 | ||||||
|
| |||||||
| Borsari Site 1 (2015) | 91 | 46.93 | BASICS | alcohol | 0-6 mo | .29* | |
| MICO to ST | .53*** | ||||||
| MIIN to ST | .23* | ||||||
|
| |||||||
| Borsari Site 2 (2015) | 160 | 52.68 | BASICS | alcohol | 0-6 mo | .13 | |
| MICO to ST | .52*** | ||||||
| MIIN to ST | −.18* | ||||||
|
| |||||||
| Campbell (2010) | 28 | 50.00 | MI/BMI | — | alcohol | 0-6 mo | .41* |
|
| |||||||
| Catley (2006) | 86 | 30.00 | MI/BMI | other drug | — | — | |
| MICO to ST | .43*** | ||||||
| MIIN to ST | .05 | ||||||
|
| |||||||
| D’Amico (2015) | 43 | 55.00 | GMI | — | poly-drug | 0-6 mo | .06 |
|
| |||||||
| Davis (2015)d | 19 | 26.80 | MI/BMI | other drug | 0-6 mo | .04 | |
| MICO to ST - MI | .29 | ||||||
| MIIN to ST - MI | .23 | ||||||
| MICO to ST - MIF | 21 | 26.80 | MI/BMI | .31 | other drug | 0-6 mo | .12 |
| MIIN to ST - MIF | .52* | ||||||
|
| |||||||
| Flickinger (2013)d | 27 | 28.04 | MI/BMI | sex risk | — | — | |
| MICO to ST | .63*** | ||||||
| MIIN to ST | .45* | ||||||
|
| |||||||
| Gaume (2008 a, b & 2009)c | 97 | 15.00 | MI/BMI | alcohol | 7+ mo | .15 | |
| MICO to ST | .28* | ||||||
| MIIN to ST | .18 | ||||||
|
| |||||||
| Gaume (2010 & 2013) | 149 | 25.00 | MI/BMI | alcohol | 0-6 mo | .11 | |
| MICO to ST | .11 | ||||||
| MIIN to ST | .27** | ||||||
|
| |||||||
| Gaume (2016) | 208 | 25.00 | MI/BMI | alcohol | 0-6 mo | .29*** | |
| MICO to ST | .20** | ||||||
| MIIN to ST | .05 | ||||||
|
| |||||||
| Hodgins (2009) | 40 | 32.30 | MI/BMI | — | gambling | 0-6 mo | .19 |
| Kahler (2016) | 90 | 63.00 | MI/BMI | alcohol | 0-6 mo | .11 | |
| MICO to ST | .48*** | ||||||
| MIIN to ST | .38*** | ||||||
|
| |||||||
| Kaplan (2013)c, d | 33 | 25.20 | MI/BMI | medication adherence | 0-6 mo | .13 | |
| MICO to ST | −.04 | ||||||
| MIIN to ST | .04 | ||||||
|
| |||||||
| Lee (2014)e | 41 | 60.00 | BASICS | alcohol | 0-6 mo | .13 | |
| MICO to ST | .64*** | ||||||
| MIIN to ST | −.13 | ||||||
|
| |||||||
| Moyers (2005) | 100 | 20.00 | MET | alcohol | — | — | |
| MICO to ST | .05 | ||||||
| MIIN to ST | .31** | ||||||
|
| |||||||
| Moyers (2009) | 118 | 60.00 | MET | alcohol | 0-6 mo | .10 | |
| MICO to ST | .16† | ||||||
| MIIN to ST | .32*** | ||||||
|
| |||||||
| Neighbors (2012)e | 22 | 60.00 | BASICS | alcohol | 0-6 mo | −.08 | |
| MICO to ST | .87*** | ||||||
| MIIN to ST | .04 | ||||||
|
| |||||||
| Pirlott (2012) | 43 | 45.00 | MI/BMI | nutrition | 7+ mo | .10 | |
| MICO to ST | .23 | ||||||
| MIIN to ST | .03 | ||||||
|
| |||||||
| Roy-Byrne (2014)e | 70 | 30.00 | SBIRT | poly-drug | 0-6 mo | .00 | |
| MICO to ST | .67*** | ||||||
| MIIN to ST | .04 | ||||||
|
| |||||||
| Vader (2010)c | 30 | 45.00 | MI/BMI | alcohol | 0-6 mo | .21 | |
| MICO to ST - MIF | .42* | ||||||
| MIIN to ST - MIF | .29 | ||||||
| MICO to ST – MIO | 30 | 45.00 | MI/BMI | .53** | alcohol | 0-6 mo | .34† |
| MIIN to ST - MIO | .11 | ||||||
Notes.
p < .001;
p < .005;
p < .05;
p < .10.
mo = month; wk = week; min = minutes; ST = sustain talk; MI = motivational interviewing; MICO = MI consistent; MIIN = MI inconsistent; MI+SO = MI with significant-other participation; MIF =MI with feedback; MIO = MI other. Removal of GMI studies did not result in substantive changes to pooled estimates.
Session length in minutes based on published report or target session length.
Effect sizes based on Barnett marijuana subsample N=74.
Trimmed estimate with study removed due to less than fair interrater reliability is (r = .16, 95% CI [.06, .25]; p = .001, k = 19, Q < .05).
Study used a measure other than MISC to code in-session behaviors [e.g. MITI 2.0 (Moyers et al., 2005), 3.0 (Moyers et al., 2007), 3.1.1 (Moyers et al., 2010), PEPA (Mastroleo, 2009)].
Included study as part of a larger observational measurement development project (Atkins et al., 2014).
Proportion measures of MI skills and client language
The Motivational Interviewing Skill Code (Houck et al., 2010; Miller et al., 2003; 2008a/b) identifies proportion measures that can be interpreted in relation to MI proficiency benchmarks. Analyses of these measures showed proportion MI consistent skills was positively associated with proportion change talk (r = .11, 95% CI [.03, .18]; p = .004, k = 22, Q < .05, I2= 55%), as was proportion complex reflections (r = .05, 95% CI [.01, .10]; p = .029, k = 21) and this latter effect was homogeneous (Q > .05; Table 4/left panel). However, the ratio of therapist reflections to questions was not significantly associated with proportion change talk (r = .03, 95% CI [−.02, .07]; p = .281, k = 22, Q > .05; Table 4/left panel). Therefore, with the exception of reflection to question ratio, the hypothesized relationships between proportion measures of therapist skill and client change talk were supported. All a path sensitivity analyses found no influential studies.
Client Change Language in Relation to Client Follow-up Outcomes – “b” path
Change and sustain talk frequency
The technical hypothesis of MI proposes that client statements for and against changing the targeted behavior will predict behavior change at follow up. Across primary studies the b path pooled correlation coefficient for change talk was r = −.01, 95% CI [−.06, .06]; p = .976, k = 24, Q > .05 and for sustain talk, was r = .19, 95% CI [.15, .24]; p < .001, k = 24, Q > .05; see Tables 2 and 3/right panel, respectively). These effects were homogeneous and showed no influential studies. Therefore, when examined as two independent frequency count indicators, client change talk was not associated with reductions in the problematic behavior at follow-up, but client sustain talk was associated with worse outcome.
Proportion change talk
When client change and sustain talk were examined as proportion change talk, the pooled correlation coefficient was negative, significant, and moderately heterogeneous (r = −.16, 95% CI [−.22, −.10]; p < .001, k = 23, Q < .05, I2= 37%; see Table 4/right panel). Due to this variability, the proportion change talk to reduced risk behavior path was also examined by primary outcome (i.e., alcohol, other drug or poly-drug, and other behavior [Hodgins, Ching, & McEwen, 2009; Kaplan, Keeley, Engel, Emsermann, & Brody, 2013; Pirlott, Kisbu-Sakarya, DeFrancesco, Elliot, & MacKinnon, 2012]). These sub-group analyses did not result in a substantively different pattern of findings.
Therapist Relational Skills in Relation to Client Follow-up Outcomes – “global” path
The relational hypothesis of MI proposes that global, or session-level, indicators of therapist relational skills (i.e., empathy, MI Spirit) will predict client behavior change at follow-up. The empathy path effect size was negative, non-significant, and homogeneous (r = −.04, 95% CI [−.08, .18]; p = .198, k = 21, Q > .05). For MI Spirit, the pooled correlation coefficient showed a similar pattern of findings (r = −.04, 95% CI [−.09, .17]; p = .184, k = 21, Q > .05; see Table 5). Therefore, relational path estimates for empathy and MI Spirit were not supported, and these homogeneous random effect estimates likely represent the average effect within the overall population of relational hypothesis process studies.
Interpersonal and Intrapersonal Factors as Moderators of Between-Study Variability in MI Path Effect Sizes
The clinical process model of a given behavioral intervention may not invariably fit all contextual circumstances. This study proposes that interpersonal and intrapersonal factors could explain observed variability in effect sizes within the a and b paths of the MI technical hypothesis. First, heterogeneous therapist skills to client language paths were re-pooled by MI proficiency cut-points in global empathy and MI Spirit (Interpersonal conditional process model). These analyses resulted in 20 sub group effects, of which 12 were homogeneous (see Table 6). In other words, 60% of between-study variance in a path effect sizes could be explained by “average” vs. “good” relational proficiency. However, as can be seen in Table 6, effect size magnitude was similar between these interpersonal sub-groups, regardless of whether homogeneity was achieved. Second, the heterogeneous client language to outcome path for proportion change talk were re-pooled by client treatment seeking status (Intrapersonal conditional process model). Here, the large majority of studies involved non-treatment seeking individuals and yielded a small and heterogeneous pooled effect size (r = −.17; p < .001, k = 19, Q < .05, I2= 44%). When two high effect, influential studies were removed (Barnett et al., 2014; Vader et al., 2010), the effect size for non-treatment seeking participants remained significant, small, but became homogeneous (r = −.13; p < .001, k = 17, Q > .05). In summary, while both a and b path conditional process models resulted in noteworthy variance explained, a clinically-informative pattern of magnitude differences, by sub-group, was not observed.
Table 6.
a path Studies by Interpersonal Moderators
| MICO to CT | MICO to ST | MIIN to CT | MIIN to ST | ProMICO to ProCT | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
|
Empathy Low |
Empathy High |
Empathy Low |
Empathy High |
Empathy Low |
Empathy High |
Empathy Low |
Empathy High |
Empathy Low |
Empathy High |
|
|
|
||||||||||
| Random Effects | .57 | .57 | .34 | .45 | .01 | .07 | .24 | .14 | .16 | .09 |
| 95% CI | −.39, .93 | .53, .60 | −.40,.81 | .36, .53 | −.39, 40 | −.02, .15 | −.19, .60 | .03, .21 | −.18, .46 | .00, .17 |
| Q | < .05 | > .05 | < .05 | < .05 | > .05 | < .05 | > .05 | < .05 | > .05 | > .05 |
| k | 2 | 18 | 2 | 17 | 2 | 17 | 2 | 17 | 2 | 16 |
|
| ||||||||||
| MICO to CT | MICO to ST | MIIN to CT | MIIN to ST | ProMICO to ProCT | ||||||
|
|
||||||||||
|
MI Spirit Low |
MI Spirit High |
MI Spirit Low |
MI Spirit High |
MI Spirit Low |
MI Spirit High |
MI Spirit Low |
MI Spirit High |
MI Spirit Low |
MI Spirit High |
|
|
|
||||||||||
| Random Effects | .59 | .56 | .41 | .43 | −.11 | .09 | .08 | .19 | .17 | .07 |
| 95% CI | .18, .82 | .51, .60 | .03, .69 | .34, .52 | −.34, .14 | −.01, .16 | −.30, .43 | .09, .24 | −.04, .30 | −.01, .16 |
| Q | < .05 | > .05 | < .05 | < .05 | > .05 | > .05 | > .05 | > .05 | > .05 | > .05 |
| k | 3 | 21 | 3 | 18 | 3 | 20 | 3 | 18 | 3 | 17 |
Notes. Significant Effect sizes (p < .05) indicted in Bold. MI = motivational interviewing; MICO = MI consistent; MIIN = MI inconsistent; CT = change talk; ST = sustain talk; ProMICO = proportion of MI consistent; ProCT = proportion of change talk; CI = confidence interval.
Discussion
In this study, we followed up our previous meta-analysis of 12 MI process studies examining the technical hypothesis of MI efficacy for substance use and other behavior change. This literature has advanced rapidly, with the current sample of primary studies tripling that of the previous review. Growth in MI process research, and behavioral treatment more broadly, represents an increasing interest in identifying a core set of mechanisms underlying risk behavior change. The current meta-analysis includes brief motivational interventions targeting a range of behavioral outcomes, such as alcohol use, other drug use, gambling, sexual risk behavior, diet and exercise, and medication adherence. Evidence-based knowledge on what makes existing treatments work has the potential to enhance their efficacy and efficiency (Huebner & Tonigan, 2007; Longabaugh & Magill, 2011; Magill, 2006; Magill & Longabaugh, 2013; Morgenstern & McKay, 2007). In fact, MI process research has already impacted implementation and delivery, with revisions to the MI clinical textbook (Miller & Rollnick, 2013) and to the fidelity rating manual (Moyers, Rowell, Manuel, Ernst, & Houck, 2016). In the current meta-analysis, we intend to further inform: a) MI clinical care, b) MI process theory, and c) measurement guidelines for future MI process research. Figure 2 offers an overview of the aggregate support for the technical and relational hypotheses, as well as the proposed conditional process models.
Figure 2.
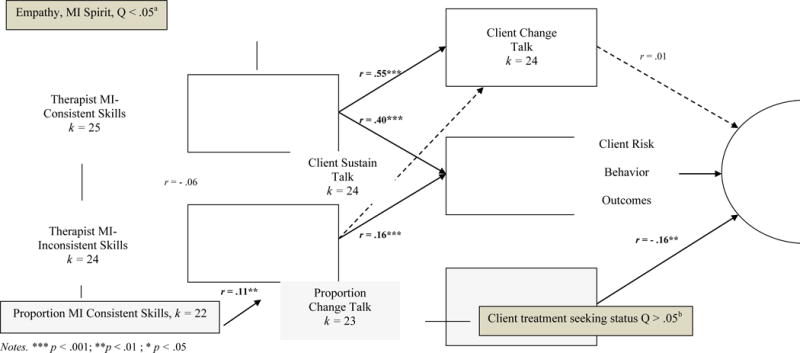
Meta-analytic results on the technical, relational, and conditional process model of MI efficacy. Notes. aHeterogeneous a path effects showed 60% of between study variance could be explained by therapist empathy and MI Spirit. bFor proportion CT to reduced risk behavior (b path), client treatment vs. non-treatment seeking status sub-groups were homogeneous with two influential studies removed (Barnett et al., 2014; Vader et al., 2010).
Summary of Results
In this meta-analysis, pooled correlation effect sizes supported seven of 10 technical hypothesis paths, while the direct paths from therapist empathy and MI Spirit to outcome (i.e., the relational hypothesis) were not supported. Of note, proportion estimates that incorporate multiple technical indicators into a single model, showed an overall pattern of findings that was consistent with theoretical expectations. Specifically, greater proportion MI consistent skills was associated with greater proportion of change talk and greater proportion of change talk was associated with risk behavior reduction. Additionally, the proposed interpersonal conditional process model explained more than half of the between study variance at the technical a path and the intrapersonal conditional process model explained the between-study variance at the technical, proportion change talk, b path. We now consider these findings in further detail.
Therapist MI Skills in Relation to Client Within-Session Change Language
MI developers and other scholars have placed a clear and consistent emphasis on operationalizing pre- and pro-scribed clinical behaviors to be enacted by the therapist within a motivational interview. In this study, frequency counts of MI consistent skills (e.g., reflective listening, open questions, and affirmations) were moderately and positively associated with client statements for, and to a slightly lesser extent, against behavior change. The latter association, found in previous MI process reviews (Magill et al., 2014; Romano & Peters, 2016), stands in contrast to the notion that therapist MI skillfulness will reduce client resistance, as indicated by the occurrence of sustain talk. The magnitude of the relationship could be partially explained by correlating frequency count measures in therapy sessions that vary in length, but the relationship itself is not merely statistical artifact. MI should facilitate an atmosphere where both positive and negative aspects of behavior change can be safely examined. The directive element of MI should also move the conversation toward ambivalence resolution. For a conservative estimate of a therapist’s effect on client change talk, studies testing temporally-lagged associations can be consulted. In these studies, the odds of change talk following MI consistent skills are higher than the odds of sustain talk (Gaume et al., 2008a; Moyers et al., 2007; 2009), which is broadly in line with MI technical theory. Similarly here, proportion MI consistency was positively related to proportion change talk, albeit with a smaller effect size than that found for frequency measures. Therefore, we can conclude that the MI consistent skills of the therapist elicit both positive and negative aspects of ambivalence, but on average, more MI consistent skills rather than inconsistent skills or non-specific skills are associated with more change rather than sustain talk. Further, the proportion of reflections that were complex, rather than simple, was positively related to proportion change talk, which underscores the unique and important contribution of this higher-level technical skill.
Process analysis of randomized clinical trial data is limited when contraindicated clinical behaviors are of interest. The therapists in these studies follow an intervention protocol and are highly trained and monitored. As such, MI inconsistent skills such as confrontations, warnings, or unsolicited advising are rarely observed in MI process research. Despite their rare occurrence, these therapeutic behaviors are harmful in the context of MI due to their positive relationship to client sustain talk, and a subsequent relationship between client sustain talk and poor outcome at follow up. This path effect was supported in this as well as in previous reviews (Apodaca & Longabaugh, 2009; Magill et al., 2014; Romano & Peters, 2016). Therefore, in MI implementation, training and supervision, it is particularly important to identify, intervene upon, and eliminate therapist behaviors that are inconsistent with MI principles.
Client Change Language in Relation to Behavior Change at Follow up
When examined as two independent frequency count indicators, change talk was not associated with reduced problem behaviors, but sustain talk did associate positively with worse outcomes. In addition, the proportion of client change statements that were in favor of change, rather than against change, was related to risk reduction. This is a replication of the previous meta-analysis with a larger, more recent, and more diverse sample of primary studies. Given these results, client language about change could be conceptualized and analyzed as a balance of pro- and anti-change statements instead of the more common emphasis on the effects of change versus sustain talk independently. Clinically, the demarcation line of success in a motivational interview would be - is ambivalence only explored or explored and resolved? The task for MI process research is to determine how to best study resolved ambivalence, or what Arkowitz and colleagues (2008) termed, the conflict resolution hypothesis. In the seminal MI process study, high commitment strength in the latter portion of an MI session predicted success status one year following drug use treatment (Amrhein, Miller, Yahne, Palmer, & Fulcher, 2003). Similarly, Miller and Rose (2009) have suggested the marker of success is a positive slope in total change talk, proportion of change talk, or mean strength in change talk over time, within an MI session. For MI clinicians, ambivalence should be worked with, and when the positive outweighs the negative, this should be prognostic of positive behavioral intention. This ‘tipping point’ can cue a therapist to move to the goal setting phase, and introduce the client to the Change Plan. Two key process questions that remain are 1) when should ambivalence be explored in MI? And 2) when is ambivalence most detrimental to MI outcome? This information would inform MI clinicians about how to best manage time within an MI session, that is, when to favor motivational enhancement (i.e., eliciting and amplifying change talk and softening sustain talk) over ambivalence exploration (i.e., exploring change and sustain talk), as well as when additional sessions or other follow up contact are indicated.
While change talk shows the most predictive validity in the context of sustain talk, sustain talk alone has demonstrated a clear and consistent deleterious effect on MI process in this as well as in previous reviews (Apodaca & Longabaugh, 2009; Magill et al., 2014). As noted above, sustain talk is one product of ambivalence exploration and therefore, we do not suggest it should be avoided. To do so, would return the field to the very situations that gave rise to MI in the first place. Rather, the task for MI theory and future research is to consider the population-based factors that might drive the relative roles of change talk versus sustain talk versus the balance of change and sustain talk (i.e., proportion change talk) within MI process. Likely, there are certain client- or outcome-based factors that predict where each indicator takes precedence as a mechanism of behavior change (Moyers, Houck, Glynn, Hallgren, & Manual, 2017). For example, is sustain talk more relevant to younger clients and change talk more relevant to older clients who have accrued more use-related consequences? Is sustain talk a key mechanism in MI for risk reduction and change talk a key mechanism in MI for health promotion? These speculations are important directions for future study in the context of both primary research and meta-analyses. Currently, this study confirms that sustain talk, on average, has greater predictive validity than change talk and may hold greater centrality in MI process than previously theorized. The task for future theory and research is to consider whether certain clinical conditions result in the unique predictive validity of one language mechanism over the other. What follows, is our effort to consider two such conditional process models.
Moderator Results and Relational Hypothesis Results: Do Interpersonal or Intrapersonal Factors Specify the Technical Hypothesis?
This study did not find support for a direct path from therapist empathy and MI Spirit to risk behavior change (i.e., relational hypothesis), but the proposed conditional process models for explaining variability in MI technical process were partially supported. First, the relationships between therapist MI skills and client change language were expected to vary by the relational proficiency of the therapist (i.e., average versus good empathy and MI Spirit; interpersonal a path model). Second, the relationship between client change language and outcome was expected to vary by whether or not study participants were seeking treatment for behavior change (intrapersonal b path model). To examine moderation in meta-analysis, the data must first suggest that a single population effect size cannot be estimated. Of 10 technical hypothesis paths tested, six were heterogeneous (i.e., five a path and one b path) and therefore warranted further testing in moderated, conditional process analysis.
Our sub-group analyses explained some, but not all of the variance in technical path effect sizes. The a path relational proficiency models yielded homogeneity in 12 out of 20 sub-groups. However, no systematic, between-group differences in effect size magnitude were identified. For example, we might expect the relationship between MI consistency and change talk to be stronger when empathy or MI Spirit are good or higher in contrast to average, but this was not observed in this sample of studies. Average relational proficiency was also rare, and variability in a path effect sizes was “moderate” (Higgins & Thompson, 2002). These statistical conditions likely hindered our ability to detect moderator effects. Alternative therapist moderators, such as provider type, might have explained additional variability in a path effects, but we consider relational proficiency the more actionable (i.e., trainable) marker of the processes of interest. The task for future research on the relational hypothesis, as well as relational conditional process models, is to test these associations in settings where therapist relational proficiency is more variable, such as naturalistic MI settings (e.g., community programs). The intrapersonal b path model for proportion change talk to outcome derived two homogeneous sub-groups for treatment seekers compared to non-treatment seekers, and the magnitude of effect in these two groups was similar. Therefore, we do not find evidence that the predictive validity of proportion change talk varies by whether or not an individual is seeking help for behavior change. Overall, the pattern of findings for moderator analysis was consistent with Magill and colleagues 2014 meta-analysis; heterogeneity was present but only moderate. From this, we can conclude that mixed findings exist in this literature, but on average, the general conclusions about the technical and relational hypotheses appear stable.
Limitations and Future Implications
Aggregate path analysis extends the traditional, bivariate model of meta-analysis to multiple links of a causal chain. While this is observational research, it enables a large body of eligible research to contribute to a single process model (Eagly & Wood, 1994). Findings in this study were stable to many variations in method, including random effects modeling, analyses of influential studies, homogeneity analyses, and moderator sub-groups. However, meta-analysis is only a tool for research synthesis. It summarizes empirical knowledge about studies; it does not provide cause-effect data about individuals. From this meta-analysis, we know MI consistency, on average, is associated with greater proportion of change talk, and greater proportion of change talk is associated with risk behavior reduction. While supportive of the technical hypothesis overall, we underscore these effect sizes were small. Therefore, more must be happening in the MI therapy room than has been specified in the theoretical model to date. Candidate processes to consider in future MI process research are measures of alliance and resistance (Aviram & Westra, 2011; Crits-Cristoph, Gallop, Temes, Woody, Martino, Ball, & Carroll, 2009). As noted above, future research should also consider whether the predictive role of client language mechanisms (i.e., change versus sustain talk) varies by population or other clinical factors.
Additional limitations to our study are less substantive, but are worthy of discussion. First, our pooled effect sizes could include more than on experimental condition from a single study (Apodaca et al., 2013; Boardman et al., 2006; Davis et al., 2016, Vader et al., 2010), which allowed some dependency in the data. However, none of these effect sizes were found to be ‘influential’ (Baujat et al., 2002) in sensitivity analyses. Second, we note that longitudinal process studies (i.e., multiple coded sessions) were quite limited within the present sample. Even when studies had multiple sessions, they elected to code only one or two. Therefore, we do not know if processes are the same or different in multi-session, in contrast to single session, MI. Finally, a limitation in this study was a restricted range of relational measures due to process analysis of highly monitored, clinical trial therapists. Future studies should consider MI process in more naturalistic contexts.
Conclusions
In this review, the MI technical hypothesis paths were mostly supported, and the proposed interpersonal and intrapersonal conditional process models were partially supported. The MI technical hypothesis has provided a sound foundation upon which to build. The task for the future is refinement, considering contextual moderators and novel mechanisms that might explain additional portions of the variance in MI efficacy and effectiveness. For the MI relational hypothesis, future MI process studies should occur in the field, rather than in the context of clinical trials.
Revised Statement of Public Health Significance.
Meta-analytic results suggest that MI clinician’s, trainers, and implementers should adhere to MI proficiency indicators in order to elicit change, rather than sustain, talk. When the balance of client ambivalence is in the direction of behavior change, this is prognostic of positive outcome. Finally, study results highlight MI technical proficiency, but the role of relational proficiency should be further examined in primary research with naturalistic clinical samples.
Acknowledgments
This research is supported by GRANT #AA023662 (PI: Magill) from National Institute on Alcohol Abuse and Alcoholism (NIAAA). The contents of this manuscript are those of the authors and do not necessarily represent the views of the NIAAA or the United States Government. The authors would like to sincerely thank the many researchers who contributed their data to this project.
Footnotes
There are no conflicts of interest associated with this manuscript.
Global scores on a 7-point scale from early versions of the Motivational Interviewing Skill Code (2003a; 2008a) were transformed to a 5-point scale. Therefore, ratings of “average” or lower and “good” or higher was consistent across studies.
Contributor Information
Molly Magill, Center for Alcohol and Addiction Studies, Brown University, USA.
Timothy R. Apodaca, Children’s Mercy Kansas City, University of Missouri – Kansas City School of Medicine, Kansas City, USA
Brian Borsari, San Francisco Veterans Affairs Health System and Department of Psychiatry, University of San Francisco, USA.
Jacques Gaume, Lausanne University Hospital, Lausanne, Switzerland.
Ariel Hoadley, School of Public Health, Brown University, USA.
Rebecca E.F. Gordon, Center for Alcohol and Addiction Studies, Brown University, USA
J. Scott Tonigan, Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico, USA.
Theresa Moyers, Center on Alcoholism, Substance Abuse, and Addictions, University of New Mexico, USA.
References
References marked with an asterisk indicate studies included in the meta-analysis.
- *.Amrhein PC, Miller WR, Yahne C, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2003;71(5):862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- *.Apodaca TR, Borsari B, Jackson KM, Magill M, Longabaugh R, Mastroleo NR, Barnett NP. Sustain talk predicts poorer outcomes among mandated college student drinkers receiving a brief motivational intervention. Psychology of Addictive Behaviors. 2014;28(3):631. doi: 10.1037/a0037296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apodaca T, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104(5):705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Apodaca TR, Magill M, Longabaugh R, Jackson KM, Monti PM. Effect of a significant other on client change talk in motivational interviewing. Journal of Consulting and Clinical Psychology. 2013;81(1):35–46. doi: 10.1037/a0030881.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arkowitz H, Miller WR, Westra HA, Rollnick S. Motivational Interviewing in the treatment of psychological problems: Conclusions and future directions (Ch.13, pp.324-41) In: Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational Interviewing in the Treatment of Psychological Problems. Guilford; New York: 2008. [Google Scholar]
- Atkins DC, Steyvers M, Imel ZE, Smyth P. Scaling up the evaluation of psychotherapy: evaluating motivational interviewing fidelity via statistical text classification. Implementation Science. 2014;9(1):49. doi: 10.1186/1748-5908-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aviram A, Westra H. The impact of motivational interviewing on resistance in cognitive behavioural therapy for generalized anxiety disorder. Psychotherapy Research. 2011;21(6):698–708. doi: 10.1080/10503307.2011.610832. [DOI] [PubMed] [Google Scholar]
- *.Baer JS, Beadnell B, Hartzler B, Wells EA, Peterson PL. Adolescent change language within a brief motivational intervention and substance use outcomes. Psychology of Addictive Behaviors. 2008;22:570–575. doi: 10.1037/a0013022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Barnett E, Moyers TB, Sussman S, Smith C, Rohrbach LA, Sun P, Spruijt-Metz D. From counselor skill to decreased marijuana use: Does change talk matter? Journal of Substance Abuse Treatment. 2014;46(4):498–505. doi: 10.1016/j.jsat.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baujat B, Mahe C, Pignon JP, Hill C. A graphical method for exploring heterogeneity in meta-analysis: Application to a meta-analysis of 65 trials. Statistics in Medicine. 2002;21(18):2641–52. doi: 10.1002/sim.1221. [DOI] [PubMed] [Google Scholar]
- *.Bertholet N, Palfai T, Gaume J, Daeppen JB, Saitz R. Do brief alcohol motivational interventions work like we think they do? Alcoholism: Clinical and Experimental Research. 2014;38(3):853–859. doi: 10.1111/acer.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS. Using motivational interviewing with smokers: Do therapist behaviors relate to engagement and therapeutic alliance? Journal of Substance Abuse Treatment. 2006;31(4):329–339. doi: 10.1016/j.jsat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- *.Borsari B, Apodaca TR, Jackson KM, Mastroleo NR, Magill M, Barnett NP, Carey KB. In-session processes of brief motivational interventions in two trials with mandated college students. Journal of Consulting and Clinical Psychology. 2015;83(1):56. doi: 10.1037/a0037635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Campbell SD, Adamson SJ, Carter JD. Client language during motivational enhancement therapy and alcohol use outcome. Behavioral and Cognitive Psychotherapy. 2010;38:399–415. doi: 10.1017/S1352465810000263. [DOI] [PubMed] [Google Scholar]
- *.Catley D, Harris K, Mayo MS, Hall S, Okuyemi KS, Boardman T, Ahluwalia JS. Adherence to principles of motivational interviewing and client within-session behavior. Behavioral and Cognitive Psychotherapy. 2006;34(1):43–56. [Google Scholar]
- Collins FS, Varmus H. A new initiative on precision medicine. New England Journal of Medicine. 2015;372(9):793–795. doi: 10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Gallop R, Temes CM, Woody G, Ball SA, Martino S, Carroll KM. The Alliance in Motivational Enhancement Therapy and Counseling as Usual for Substance Use Problems. Journal of Consulting and Clinical Psychology. 2009;77(6):1125–1135. doi: 10.1037/a0017045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.D’Amico EJ, Houck JM, Hunter SB, Miles JN, Osilla KC, Ewing BA. Group motivational interviewing for adolescents: change talk and alcohol and marijuana outcomes. Journal of Consulting and Clinical Psychology. 2015;83(1):68. doi: 10.1037/a0038155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Davis JP, Houck JM, Rowell LN, Benson JG, Smith DC. Brief motivational interviewing and normative feedback for adolescents: Change language and alcohol use outcomes. Journal of Substance Abuse Treatment. 2015;65:66–73. doi: 10.1016/j.jsat.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, editor. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. Guilford Press; 1999. [Google Scholar]
- Eagly AH, Wood W. Using research syntheses to plan future research. In: Cooper H, Hedges LV, editors. The Handbook of Research Synthesis. New York, NY, US: Russell Sage Foundation; 1994. pp. 485–500. [Google Scholar]
- Feldstein Ewing SW, Filbey FM, Sabbineni A, Chandler LD, Hutchison KE. How psychosocial alcohol interventions work: A preliminary look at what fMRI can tell us. Alcoholism: Clinical and Experimental Research. 2011;35(4):643–651. doi: 10.1111/j.1530-0277.2010.01382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Feldstein Ewing SW, Gaume J, Ernst DB, Rivera L, Houck JM. Do therapist behaviors differ with Hispanic youth? A brief look at within-session therapist behaviors and youth treatment response. Psychology of Addictive Behaviors. 2015;29(3):779–786. doi: 10.1037/adb0000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Flickinger TE, Rose G, Wilson IB, Wolfe H, Saha S, Korthuis PT, Moore RD. Motivational interviewing by HIV care providers is associated with patient intentions to reduce unsafe sexual behavior. Patient Education and Counseling. 2013;93(1):122–129. doi: 10.1016/j.pec.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Gaume J, Bertholet N, Faouzi M, Gmel G, Daeppen JB. Counselor motivational interviewing skills and young adult change talk articulation during brief motivational interventions. Journal of substance abuse treatment. 2010;39(3):272–281. doi: 10.1016/j.jsat.2010.06.010. [DOI] [PubMed] [Google Scholar]
- *.Gaume J, Gmel G, Faouzi M, Daeppen J. Counsellor behaviours and patient language during brief motivational interventions: A sequential analysis of speech. Addiction. 2008a;103(11) doi: 10.1111/j.1360-0443.2008.02337.x. [DOI] [PubMed] [Google Scholar]
- *.Gaume J, Gmel G, Daeppen J. Brief Alcohol Interventions: Do Counsellors’ and Patients’ Communication Characteristics Predict Change? Alcohol & Alcoholism. 2008b;43(1):62–69. doi: 10.1093/alcalc/agm141. [DOI] [PubMed] [Google Scholar]
- *.Gaume J, Bertholet N, Faouzi M, Gmel G, Daeppen JB. Does Change Talk During Brief Motivational Interventions with Young Men Predict Change in Alcohol Use? Journal of Substance Abuse Treatment. 2013;44(2):177–185. doi: 10.1016/j.jsat.2012.04.005. [DOI] [PubMed] [Google Scholar]
- *.Gaume J, Gmel G, Faouzi M, Daeppen J. Counselor skill influences outcomes of brief motivational interventions. Journal of Substance Abuse Treatment. 2009;37(2):151–159. doi: 10.1016/j.jsat.2008.12.001. [DOI] [PubMed] [Google Scholar]
- *.Gaume J, Longabaugh R, Magill M, Bertholet N, Gmel G, Daeppen JB. Under what conditions? Therapist and client characteristics moderate the role of change talk in brief motivational intervention. Journal of Consulting and Clinical Psychology. 2016;84(3):211–220. doi: 10.1037/a0039918. [DOI] [PubMed] [Google Scholar]
- Glynn LH, Moyers TB. Chasing change talk: The clinician’s role in evoking client language about change. Journal of Substance Abuse Treatment. 2010;39(1):65–70. doi: 10.1016/j.jsat.2010.03.012. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3(4):486–504. doi: 10.1037/1082-989X.3.4.486. [DOI] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in meta-analysis. Statistics in Medicine. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Higgins J, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses [journal article as teaching resource, deposited by John Flynn] British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hodgins DC, Ching LE, McEwen J. Strength of commitment language in motivational interviewing and gambling outcomes. Psychology of Addictive Behaviors. 2009;23(1):122–130. doi: 10.1037/a0013010. [DOI] [PubMed] [Google Scholar]
- Houck JM, Moyers TB, Miller WR, Glynn LH, Hallgren KA. Motivational Interviewing Skill Code (MISC) version 2.5 2010 [Google Scholar]
- Huebner RB, Tonigan JS. The Search for Mechanisms of Behavior Change in Evidence‐Based Behavioral Treatments for Alcohol Use Disorders: Overview. Alcoholism: Clinical and Experimental Research. 2007;31(s3) doi: 10.1111/j.1530-0277.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- Hunter JE, Schmidt FL. Methods of Meta-analysis: Correcting Error and Bias in Research Findings. 2nd. Newbury Park, CA: Sage Publications; 2004. [Google Scholar]
- *.Kahler CW, Caswell AJ, Laws MB, Walthers J, Magill M, Mastroleo NR, Monti PM. Using topic coding to understand the nature of change language in a motivational intervention to reduce alcohol and sex risk behaviors in emergency department patients. Patient Education and Counseling. 2016;99(10):1595–1602. doi: 10.1016/j.pec.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kaplan JE, Keeley RD, Engel M, Emsermann C, Brody D. Aspects of patient and clinician language predict adherence to antidepressant medication. The Journal of the American Board of Family Medicine. 2013;26(4):409–420. doi: 10.3122/jabfm.2013.04.120201. [DOI] [PubMed] [Google Scholar]
- Klonek FE, Lehmann-Willenbrock N, Kauffeld S. Dynamics of resistance to change: a sequential analysis of change agents in action. Journal of change management. 2014;14(3):334–360. [Google Scholar]
- *.Knittle K, De Gucht V, Mejino A, Hurkmans E, Vlieland TV, Maes S. Are Aspects of a Motivational Interview Related to Subsequent Changes in Physical Activity and Regulatory Style? Examining Relationships among Patients with Rheumatoid Arthritis. Motivational Interviewing: Training, Research, Implementation, Practice. 2014;1(3):42–47. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Laws MB, Rose GS, Beach MC, Lee Y, Rogers WS, Velasco AB, Wilson IB. Patient-provider concordance with behavioral change goals drives measures of motivational interviewing consistency. Patient Education and Counseling. 2015;98(6):728–733. doi: 10.1016/j.pec.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lee CM, Kilmer JR, Neighbors C, Atkins DC, Zheng C, Walker DD, Larimer ME. Indicated prevention for college student marijuana use: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2013;81(4):702. doi: 10.1037/a0033285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Lee CM, Neighbors C, Lewis MA, Kaysen D, Mittmann A, Geisner IM, Larimer ME. Randomized controlled trial of a Spring Break intervention to reduce high-risk drinking. Journal of Consulting and Clinical Psychology. 2014;82(2):189. doi: 10.1037/a0035743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical Meta-Analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Longabaugh R, Magill M. Recent advances in behavioral addiction treatments: focusing on mechanisms of change. Current Psychiatry Reports. 2011;13(5):382. doi: 10.1007/s11920-011-0220-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Magill M, Morgenstern J, Huebner R. Mechanisms of behavior change in treatment for alcohol and other drug use disorders. In: McCrady BS, Epstein EE, editors. Addictions: A Comprehensive Guidebook. 2nd. USA: Oxford University Press; 2013. Ch 27. [Google Scholar]
- Lord SP, Sheng E, Imel ZE, Baer J, Atkins DC. More than reflections: empathy in motivational interviewing includes language style synchrony between therapist and client. Behavior Therapy. 2015;46(3):296–303. doi: 10.1016/j.beth.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology. 2009;65(11) doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, Rollnick S. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling. 2013;93(2):157–168. doi: 10.1016/j.pec.2013.07.012. [DOI] [PubMed] [Google Scholar]
- Magill M. The future of evidence in evidence based practice: Who will answer the call for clinical relevance? Journal of Social Work. 2006;6(2):101–115. [Google Scholar]
- Magill M, Gaume J, Apodaca TR, Walthers J, Mastroleo NR, Borsari B, Longabaugh R. The technical hypothesis of motivational interviewing: A meta-analysis of MI’s key causal model. Journal of Consulting and Clinical Psychology. 2014;82(6):973–983. doi: 10.1037/a0036833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Longabaugh R. Efficacy combined with specified ingredients: a new direction for empirically supported addiction treatment. Addiction. 2013;108(5):874–881. doi: 10.1111/add.12013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin T, Moyers TB, Houck JM, Christopher PJ, Miller WR. Motivational interviewing sequential code for observing process exchanges (MI-SCOPE) coder’s manual. 2005 doi: 10.1037/a0033041. Unpublished Manual. [DOI] [PubMed] [Google Scholar]
- *.Mastroleo NR, Magill M, Barnett NP, Borsari B. A pilot study of two supervision approaches for peer-led alcohol interventions with mandated college students. Journal of Studies on Alcohol and Drugs. 2014;75(3):458–466. doi: 10.15288/jsad.2014.75.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastroleo NR, Mallett KA, Turrisi R, Ray AE. Psychometric properties of the Peer Proficiency Assessment (PEPA): A tool for evaluation of undergraduate peer counselors’ motivational interviewing fidelity. Addictive behaviors. 2009;34(9):717–722. doi: 10.1016/j.addbeh.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.McCambridge J, Day M, Thomas BA, Strang J. Fidelity to motivational interviewing and subsequent cannabis cessation among adolescents. Addictive Behaviors. 2011;36(7):749–754. doi: 10.1016/j.addbeh.2011.03.002. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Islam NY, Wheat E. Designing, conducting, and evaluating therapy process research. The Oxford Handbook of Research Strategies for Clinical Psychology. 2013:142–164. [Google Scholar]
- Miller WR. Manual for the Motivational Interviewing Skill Code (MISC) 2000 Unpublished Manual. [Google Scholar]
- Miller WR, Benefield GR, Tonigan JS. Enhancing motivation for change in problem drinking: A controlled comparison of two therapist styles. Journal of Consulting and Clinical Psychology. 1993;61(3):455–461. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- Miller WR, Moyers TB, Ernst D, Amrhein P. Manual for the Motivational Interviewing Skill Code Version 2.0 (MISC) 2003 Unpublished Manual. [Google Scholar]
- Miller WR, Moyers TB, Ernst D, Amrhein P. Manual for the Motivational Interviewing Skill Code Version 2.1 (MISC) 2008a Unpublished Manual. [Google Scholar]
- Miller WR, Moyers TB, Manuel JK, Christopher P, Amrhein P. Revision for Client Language Coding: MISC 2.1: Client Language Assessment in Motivational Interviewing (CLAMI) Segment. 2008b Unpublished Manual. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 1st. New York: Guilford; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd. New York: Guilford; 2002. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd. New York, NY: Guilford Press; 2013. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64:527–37. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomized controlled trials: The QUOROM statement. The Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- *.Morgenstern J, Kuerbis A, Amrhein P, Hail L, Lynch K, McKay JR. Motivational interviewing: A pilot test of active ingredients and mechanisms of change. Psychology of Addictive Behaviors. 2012;26(4):859–69. doi: 10.1037/a0029674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, McKay JR. Rethinking the paradigms that inform behavioral treatment research for substance use disorders. Addiction. 2007;102(9):1377–1389. doi: 10.1111/j.1360-0443.2007.01882.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Houck JM, Glynn LH, Hallgren KA, Manual JK. A randomized controlled trial to influence client language in substance use disorder treatment. Drug and Alcohol Dependence. 2017;172:43–50. doi: 10.1016/j.drugalcdep.2016.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, Martin TB, Christopher PJ, Houck JM, Tonigan JS, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31(3):40S–47S. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- *.Moyers TB, Martin T, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology. 2009;77(6):1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. The motivational interviewing treatment integrity MITI code Version 2.0. 2003 Unpublished Manual. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. The Motivational Interviewing Treatment Integrity (MITI) code: Version 3.0. Albuquerque, NM: University of New Mexico; 2007. Unpublished manuscript. [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. Revised global scales: Motivational interviewing treatment integrity 3.1.1 (MITI 3.1.1) 2010 Unpublished Manual. [Google Scholar]
- *.Moyers TB, Miller WR, Hendrickson SL. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. Journal of Consulting and Clinical Psychology. 2005;73(4):590–598. doi: 10.1037/0022-006X.73.4.590. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Rowell LN, Manuel JK, Ernst D, Houck JM. The motivational interviewing treatment integrity code (MITI 4): Rationale, preliminary reliability and validity. Journal of Substance Abuse Treatment. 2016;65:36–42. doi: 10.1016/j.jsat.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Neighbors C, Lee CM, Atkins DC, Lewis MA, Kaysen D, Mittmann A, Larimer ME. A randomized controlled trial of event-specific prevention strategies for reducing problematic drinking associated with 21st birthday celebrations. Journal of Consulting and Clinical Psychology. 2012;80(5):850. doi: 10.1037/a0029480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIH Common Fund. Science of behavior change. 2016 http://commonfund.nih.gov/behaviorchange/index.
- *.Pirlott AG, Kisbu-Sakarya Y, DeFrancesco CA, Elliot DL, MacKinnon DP. Mechanisms of motivational interviewing in health promotion: a Bayesian mediation analysis. International Journal of Behavioral Nutrition and Physical Activity. 2012;9(1):69. doi: 10.1186/1479-5868-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Research Methods. 2007;41(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and Data Analysis Methods. Vol. 1. Sage Publications, Inc; 2002. [Google Scholar]
- Romano M, Peters L. Evaluating the mechanisms of change in motivational interviewing in the treatment of mental health problems: A review and meta-analysis. Clinical Psychology Review. 2015;38:1–12. doi: 10.1016/j.cpr.2015.02.008. [DOI] [PubMed] [Google Scholar]
- Romano M, Peters L. Understanding the process of motivational interviewing: A review of the relational and technical hypotheses. Psychotherapy Research. 2016;26(2):220–240. doi: 10.1080/10503307.2014.954154. [DOI] [PubMed] [Google Scholar]
- *.Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, Joesch JM. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. Jama. 2014;312(5):492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R. Parametric measures of effect size. The Handbook of Research Synthesis. 1994:231–244. [Google Scholar]
- *.Saitz R, Palfai TP, Cheng DM, Horton NJ, Freedner N, Dukes K, Samet JH. Brief Intervention for Medical Inpatients with Unhealthy Alcohol Use: A Randomized, Controlled Trial. Annals of Internal Medicine. 2007;146(3):167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- *.Shorey RC, Martino S, Lamb KE, LaRowe SD, Santa Ana EJ. Change talk and relatedness in group motivational interviewing: A pilot study. Journal of Substance Abuse Treatment. 2015;51:75–81. doi: 10.1016/j.jsat.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tollison SJ, Lee CM, Neighbors C, Neil TA, Olson ND, Larimer ME. Questions and reflections: the use of motivational interviewing microskills in a peer-led brief alcohol intervention for college students. Behavior Therapy. 2008;39(2):183–194. doi: 10.1016/j.beth.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Tollison SJ, Mastroleo NR, Mallett KA, Witkiewitz K, Lee CM, Ray AE, Larimer ME. The relationship between baseline drinking status, peer motivational interviewing microskills, and drinking outcomes in a brief alcohol intervention for matriculating college students: a replication. Behavior Therapy. 2013;44(1):137–151. doi: 10.1016/j.beth.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonigan JS. Process Matching: The Application of Precision Medicine in Behavioral Treatment for Alcohol and Substance Use Disorders. Keynote presentation at the 12th Annual Pre-Conference Satellite Meeting on Mechanisms of Behavior Change; New Orleans, LA. 2016. Jun, [Google Scholar]
- *.Vader AM, Walters ST, Prabhu GC, Houck JM, Field CA. The language of motivational interviewing and feedback: Counselor language, client language, and client drinking outcomes. Psychology of Addictive Behaviors. 2010;24(2):190–197. doi: 10.1037/a0018749. [DOI] [PMC free article] [PubMed] [Google Scholar]


