Introduction
Primary renal lymphoma, a rare lymphoproliferative disorder of the genitourinary tract, is characterized by localization of the disease to the kidney with no overt signs of other organ involvement. It comprises 0.7% of extra nodal lymphomas and 0.1% of all malignant lymphomas. The criteria used to diagnose primary renal lymphoma are inclusive of acute renal failure in the absence of other causes of renal impairment, rapid improvement of renal function after treatment, increase in kidney size without urinary tract obstruction, and absence of nodal or extra nodal involvement.1
The first reported case of kidney involvement in malignant lymphoma is believed to be in 1878. There are less than 80 cases of primary renal lymphoma in the literature.
To date, there have been 3 reported cases of renal lymphoma that presented as solitary renal masses with inferior vena cava (IVC) tumor thrombi.2 In 10–25% of patients, renal lymphoma presents as a solitary renal mass and can mimic renal cell carcinoma (RCC).1 Unlike renal cell carcinoma, renal lymphoma is softer and infiltrates into existing structures whereby renal cell carcinoma often displaces the kidney.
Renal lymphoma is typically secondary to renal or perinephric involvement from lymphadenopathy and is most often non- Hodgkin in form. The presence of an IVC thrombus is rarely seen as sequela of renal lymphoma and presents a diagnostic challenge.
Case presentation
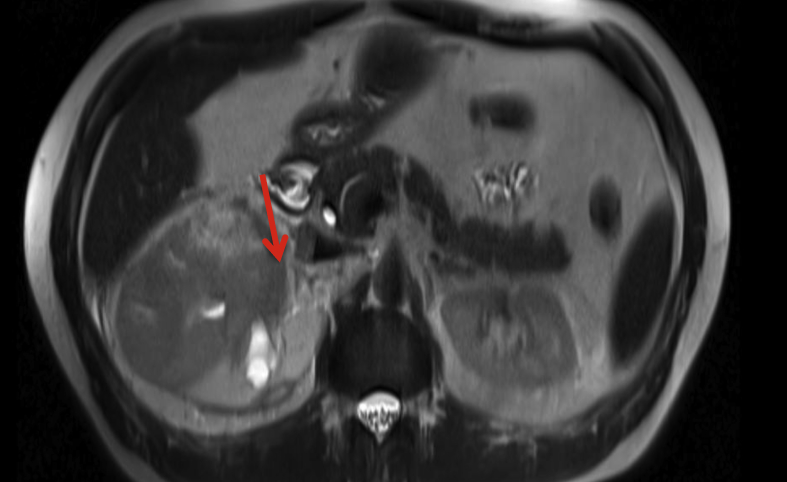
A 51-year old man presented for evaluation on ongoing right flank pain. An MRI revealed a large right renal mass involving more than 75% of the renal parenchyma. There was extension beyond the renal capsule and Gerota's fascia (Fig. 1, Fig. 2). An IVC tumor thrombus, extending into the right renal vein and involving approximately 50% of the IVC circumference was noted. Imaging findings were consistent with a clinical diagnosis of invasive renal cell carcinoma. The patient underwent a right radical nephrectomy with IVC thrombectomy and patch graft of the IVC. Pathology revealed an immunophenotype characteristic of large B-cell, non- Hodgkin lymphoma (NHL). He underwent chemotherapy and remains disease free with a functional solitary renal unit.
Fig. 1.
MRI abdomen pelvis with and without contrast, showing large right renal mass, mimicking renal cell carcinoma.
Fig. 2.
MRI abdomen pelvis with and without contrast, showing large right renal mass, mimicking renal cell carcinoma.
Discussion
RCC is unique in that it has the tropism for vascular invasion, specifically invasion into the renal vein and the IVC, forming a tumor thrombus. This is characteristic and diagnostic of RCC. It is very atypical for NHL to result in a solitary renal mass with IVC tumor thrombus. The first reported case of NHL and IVC tumor thrombus was in 1993. Involvement of the kidney by lymphoma is not only rare but is often a late manifestation of advanced nodal disease.1 Without aggressive chemotherapy, 75% of patients die within one year. It remains a diagnostic conundrum. Though renal lymphoma commonly results in vascular and ureteral encasement, intraluminal vascular involvement (i.e., IVC tumor thrombus) is rare. The standard of care for large B-cell lymphoma of the kidney is chemotherapy. A renal mass in conjunction with IVC tumor thrombus (no IVC wall infiltration and no other metastases) is the classic presentation of advanced renal cell carcinoma for which the standard of care is nephrectomy and IVC thrombectomy. While renal cell carcinoma is the most common tumor that has been associated with IVC tumor thrombi, there have been reports of IVC tumor thrombi in patients with adrenal cancer, testicular cancer, colon cancer, gastric cancer, transitional call carcinoma of the bladder and Wilms tumor. To date, there have been three reports of patients with NHL associated renal masses with IVC tumor thrombi. One of the three patients underwent nephrectomy.
Given the malignant lymphoproliferation of the kidney in renal lymphoma, one question that arises is if the presence of NHL poses an increased risk of RCC and/or if the presence of RCC increases the risk of NHL. Rabbani et al. conducted a Surveillance Epidemiology and End Results (SEER) database study and concluded that aside from the first year of follow up, there is no higher risk of developing NHL after RCC and RCC after NHL.3 An independent report identified 9 patients with both RCC and lymphoma. Of these, 2 patients were diagnosed with NHL after the diagnosis of RCC, 1 was diagnosed at the same time and the remaining 6 were diagnosed with lymphoma and subsequently RCC. This raises the question of a component of lymphoproliferation, which is a hallmark of renal lymphoma, that may lead to solid tumor formation in the kidney.
Regarding diagnostic modalities, Computed Tomography (CT) is the most sensitive imaging modality for the evaluation of the kidneys in patients with renal lymphoma. CT findings consistent with renal lymphoma include multiple renal masses (most common), lymphadenopathy, solitary masses, and renal invasion from disease in the retroperitoneum. Retroperitoneal extension is seen in 25-30% of patients with primary renal lymphoma and would be a large, bulky retroperitoneal mass surrounding renal vasculature and invading into the renal hilum. Unlike RCC, lymphoma often does not compress or shift vasculature and thereby vasculature would remain patent. Biopsy is still required for definitive diagnosis of lymphoma. Unlike years ago, studies show that today renal biopsy is utilized more often and has been documented to alter clinical management in 60.5% of patients in whom biopsy is performed.4 These studies however were predominantly done in patients with solitary renal masses not associated with IVC tumor thrombi. Additionally, for masses that have features of malignancy, a negative biopsy is unlikely to change management. Furthermore, there is report in the literature of a single tumor harboring hybrid histology of both RCC and renal lymphoma; in such a case, a biopsy would be unreliable.
Another imaging adjunct that can be useful for distinguishing renal cell lymphoma and renal cell carcinoma is Fluorine-fluorodeoxyglucose positron emission tomography/computed tomography (F-FDG PET/CT). Ye et al. completed a report comparing patients with lymphoma and renal cell carcinoma and noted that F-FDG uptake by the lymphoma lesions of the kidney was much higher than that of the renal cell carcinomas. This study suggested that F-FDG-PET may be a useful adjunct in differentiating the two, however one must have a high index of suspicion.5
Conclusion
It is crucial to differentiate renal lymphoma from renal cell carcinoma as a missed diagnosis can lead to disseminated disease and unnecessary nephrectomy. This can be quite challenging in cases of renal lymphoma that present with IVC tumor thrombi given this is a hallmark of RCC. In this case, given that tumor thrombi are seen in 4–10% of cases of RCC and rarely in renal cell lymphoma, the treatment rendered was based ona clinical diagnosis of renal cell carcinoma. The diagnosis of primary renal cell lymphoma poses a challenge; this challenge is even greater when renal lymphoma presentswith intraluminal vascular invasion. It is important to disseminate reported cases given the rarity of this disease process and to emphasize that cancers of lymphatic origin can originate from the kidney.
Competing interests
None to declare.
Funding
None.
Authors contributions
All authors contributed equally to each section of the manuscript.
Acknowledgements
None.
Declarations of interest
None.
References
- 1.Belbaraka R., Elyoubi M.B., Boutayeb S., Errihani H. Primary renal non-Hodgkin lymphoma: an unusual diagnosis for a renal mass. Indian J Cancer. 2011;48(2):255–256. doi: 10.4103/0019-509X.82880. [DOI] [PubMed] [Google Scholar]
- 2.Wagner J.R., Honig S.C., Siroky M.B. Non- Hodgkin's lymphoma can mimic renal adenocarcinoma with inferior vena caval involvement. Urology. 1993;42(6):720–724. doi: 10.1016/0090-4295(93)90543-j. [DOI] [PubMed] [Google Scholar]
- 3.Rabbani F., Russo P. Lack of association between renal cell carcinoma and non-Hodgkin's lymphoma. Urology. 1999;54(1):28–33. doi: 10.1016/s0090-4295(99)00066-7. [DOI] [PubMed] [Google Scholar]
- 4.Maturen K.E., Nghiem H.V., Caoili E.M., Higgins E.G., Wolf J.S., Jr., Wood D.P., Jr. Renal mass core biopsy: accuracy and impact on clinical management. AJR Am J Roentgenol. 2007;188(2):563–570. doi: 10.2214/AJR.06.0220. [DOI] [PubMed] [Google Scholar]
- 5.Ye X.H., Chen L.H., Wu H.B. 18F-FDG PET/CT evaluation of lymphoma with renal involvement: comparison with renal carcinoma. South Med J. 2010;103(7):642–649. doi: 10.1097/SMJ.0b013e3181e23cb0. [DOI] [PubMed] [Google Scholar]