ABSTRACT
We evaluated the amplitude and latency scores in the RAPDx® device together with other ophthalmic examinations, before and after treatment in four patients with optic nerve disease. In all patients, the visual acuity (VA) and visual field (VF) after treatment was resolved. Both scores after treatment were lower, with reduced laterality-based differences in VA and critical flicker fusion frequency (CFF). Even after treatment, 3 patients had laterality-based differences in circumpapillary retinal nerve fiber layer thickness (cpRFNLT). Both scores for evaluation of RAPD by RAPDx® correlated with subjective examinations and were useful for evaluation of the efficacy of treatment.
KEYWORDS: Optic nerve disease, relative afferent pupillary defect, treatment
Introduction
Evaluation of a relative afferent pupillary defect (RAPD) is useful for diagnosis of optic nerve disease and assessment of treatment efficacy.1 The RAPDx® (Konan Medical Inc., Irvine, CA) objectively determines the RAPD magnitude by alternately presenting light stimuli to each eye. The amplitude and latency scores derived by RAPDx® are used to calculate RAPD by using log units; the amplitude score is obtained by determining the constriction percentage of both eyes, and the latency score by determining the latency of both eyes. The amplitude and latency scores determined with the RAPDx®, particularly the standard value of the amplitude score,2 are useful for evaluating RAPD, and RAPDx® has been used to evaluate RAPD in patients with optic nerve disease.3
However, the treatment efficacy associated with the use of RAPDx® has not been evaluated. We evaluated the RAPD amplitude and latency scores together with the visual acuity (VA), critical flicker fusion frequency (CFF), sectoral analysis of circumpapillary retinal nerve fibre layer thickness (cpRNFLT), and visual field (VF) before and after treatment in four patients with optic nerve disease.
Methods
The study was approved by the Institutional Review Board of Kitasato University (approval number B15-35) and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all volunteers. Four patients who commenced treatment (steroid pulse therapy: 1000 mg/day for 3 days) for optic nerve disease were enrolled.
With the RAPDx® device, the dark-adaptation time, stimulus conditions, and methods for calculating the amplitude and latency scores were as reported previously;2 the latter were presented as positive scores for diseased eyes and negative scores for healthy eyes. We defined RAPD as non-positive when the absolute values of both the amplitude and latency scores were <0.5 log units and as positive when the absolute values were ≥0.5 log units.2 The patients did not have strabismus that could cause improper measurements.
VA was indicated as logMAR. CFF values (red light stimulus) were measured using the Handy Flicker (Neitz Inc., Chicago, IL) as follows. The flicker rate was gradually decreased, and the rate at which the subject considered that the light was flickering, rather than being continuous, was considered to be the CFF value. The cpRNFLT values were measured using spectral domain optical coherence tomography (Spectralis®; Heidelberg Engineering, Heidelberg, Germany), and the average values were analysed. The laterality-based difference was defined as the absolute value of the healthy eye minus that of the affected eye. The laterality-based differences in VA, CFF values, and cpRNFLT were assessed and were found to be related to both the amplitude and latency scores. The correlation was determined by the Spearman’s rank correlation coefficient. VF was measured using Goldmann perimetry in three patients and by Humphrey perimetry in one patient and evaluated with or without of central scotoma. No data related to colour vision were collected in this study.
Results
The VA (logMAR) of all patients after treatment was ≤0. The central scotoma in VF was detected in all patients but resolved after treatment. Table 1 and Figure 1 show the amplitude and latency scores and the laterality-based differences in VA and CFF values before and after treatment; laterality-based differences in cpRNFLT are shown only for post-treatment values. In one patient, RAPD was detected in amplitude score even after VA recovery, whereas it was not detected in the latency score. In all patients, the amplitude and latency scores after treatment were lower, with reduced laterality-based differences in VA and CFF; these were based on subjective examinations. Even after treatment, three patients showed laterality-based differences in cpRNFLT; the cpRNFLT of the affected eye was thinner. Figures 2 and 3 show the correlation of each parameter (e.g. the laterality-based differences in VA or CFF values, respectively) and both the amplitude and latency scores. Both scores were significantly correlated with the laterality-based differences in VA and CFF values (r = 0.76–0.93, p < 0.05).
Table 1.
The amplitude score and latency score and the laterality-based differences in VA and CFF values and the cpRNFLT of before and after treatment.
| Participants number |
1 |
2 |
3 |
4 |
||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis |
Idiopathic opticneuritis |
Anti-aquaporin-4 antibody-positive optic neuritis |
Idiopathic opticneuritis |
Idiopathic opticneuritis |
||||
| Steroid pulse |
Steroid pulse |
Steroid pulse |
Steroid pulse |
|||||
| Treatment | Before | After | Before | After | Before | After | Before | After |
| Amplitude score (log units) | 1.47 | 0.40 | 2.97 | 1.17 | 2.59 | 0.36 | 3.00 | 0.46 |
| Latency score (log units) | 0.71 | 0.21 | 0.43 | 0.32 | 0.65 | 0.08 | 0.74 | 0.19 |
| RAPD determined from amplitude score | Positive | Non-positive | Positive | Positive | Positive | Non-positive | Positive | Non-positive |
| Laterality-based differences in VA (logMAR) | 1.23 | 0 | 1.77 | 0.08 | 2.08 | 0 | 2.08 | 0 |
| Laterality-based differences in CFF (Hz) | 32 | 0 | 21 | 17 | 27 | 6 | 25 | 8 |
| Laterality-based differences in cpRFNLT (μm) | – | 23 | – | 60 | – | 0 | – | 7 |
VA: visual acuity; CFF: critical flicker fusion frequency; cpRFNLT: circumpapillary retinal nerve fibre layer thickness. Laterality-based differences in cpRNFLT were shown only for post-treatment.
Figure 1.
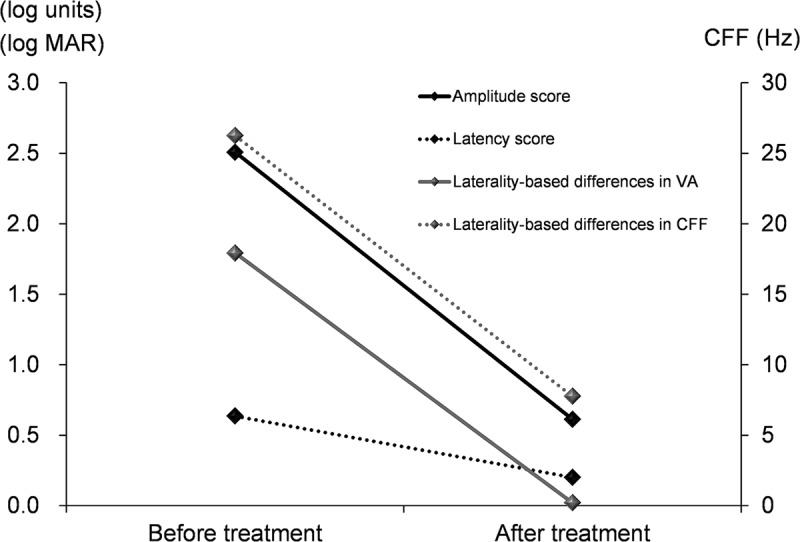
Trend of mean before and after treatment of the amplitude score and latency score and laterality-based differences in VA and CFF values. VA: visual acuity; CFF: critical flicker fusion frequency. The vertical axis on the left side indicates values of amplitude score, latency score, and VA (logMAR). The vertical axis on the right side indicates CFF (Hz).
Figure 2.
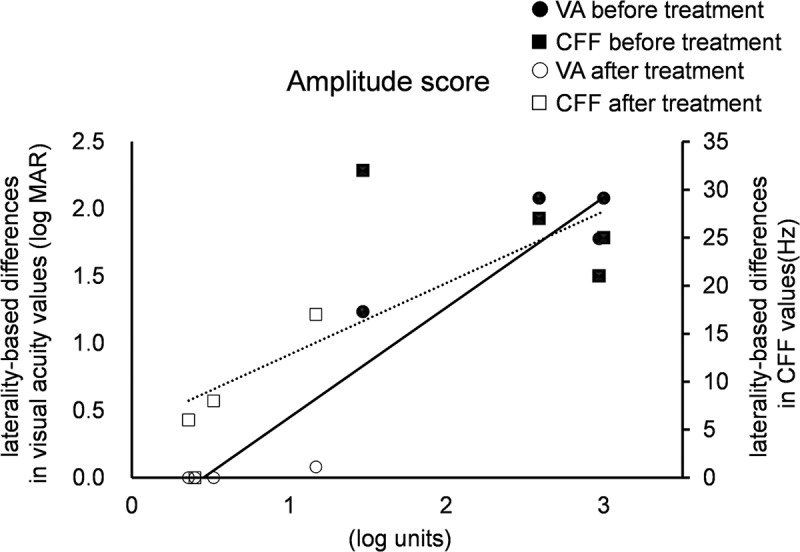
Correlations with amplitude score and the laterality-based differences in visual acuity and CFF values. VA: visual acuity; CFF: critical flicker fusion frequency. p value was <0.05 and correlation coefficient was 0.76 with CFF; p value was 0.05 and correlation coefficient was 0.76 with CFF. Solid line: VA; dotted line: CFF.
Figure 3.
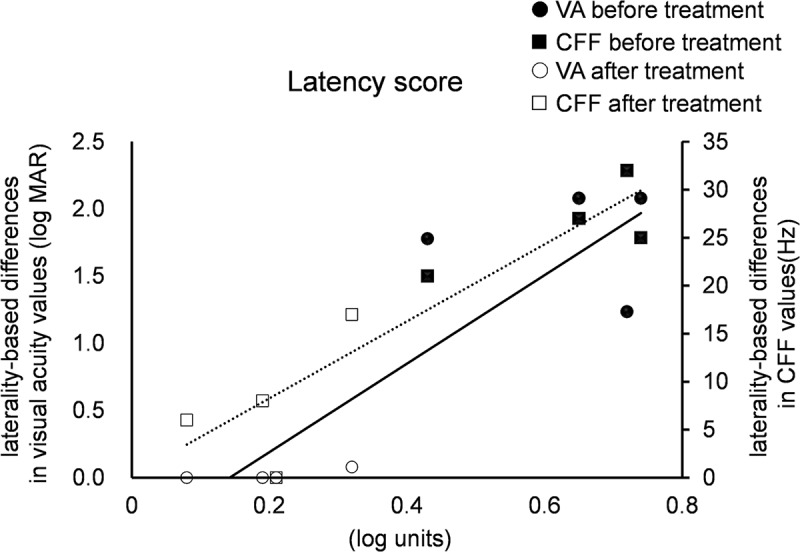
Correlations with latency score and the laterality-based differences in visual acuity and CFF values. VA: visual acuity; CFF: critical flicker fusion frequency. p value was <0.01 and correlation coefficient was 0.86 with CFF. p value was 0.01 and correlation coefficient was 0.86 with CFF. Solid line: VA; dotted line: CFF.
Discussion
We show that RAPD may be detected after treatment-related recovery in VA and VF and can be quantitatively evaluated by RAPDx®. According to previous reports, the cpRNFLT of subjects with anterior ischemic optic neuropathy was markedly reduced,4 and cpRNFLT and RAPD were significantly correlated.5 In this study, amplitude scores tended to increase proportionally with increased laterality-based differences in cpRNFLT. Thus, optic nerve disease causes irreversible damage to the retinal nerve fibre layer (RNFL). Furthermore, both parameters for evaluation of RAPD by the RAPDx® device correlated with subjective examinations (i.e. VA and VF) and were useful for evaluation of the efficacy of treatment; in particular, the amplitude score might detect laterality of the visual input more sensitively than VA and more objectively than the CFF.
The study was limited in that the case number was small. However, it demonstrates the efficacy of treatment using the RAPDx® device in patients with optic nerve disease, which has not been reported previously. Future studies with larger sample sizes are warranted.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- 1.Thompson HS, Corbett JJ, Cox TA.. How to measure the relative afferent pupillary defect. 1981;26:39–42. doi: 10.1016/0039-6257(81)90124-7. [DOI] [PubMed] [Google Scholar]
- 2.Satou T, Goseki T, Asakawa K, Ishikawa H, Shimizu K.. Effects of age and gender on measurement values and determination of the standard values. 2016;5:18 eCollection. doi: 10.1167/tvst.5.2.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Satou T, Ishikawa H, Asakawa K, Goseki T, Niida T, Shimizu K. Evaluation of relative afferent pupillary defect using RAPDx® device in patients with optic nerve disease. 2016;40:120–124. doi: 10.3109/01658107.2016.1169550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hood DC, Anderson S, Rouleau J, Wenick AS, Grover LK, Behrens MM, Odel JG, Lee AG, Kardon RH. Retinal nerve fiber structure versus visual field function in patients with ischemic optic neuropathy. A test of a linear model. 2008;115:904–910. doi: 10.1016/j.ophtha.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang DS, Boland MV, Arora KS, Supakontanasan W, Chen BB, Friedman DS. Symmetry of the pupillary light reflex and its relationship to retinal nerve fiber layer thickness and visual field defect. 2013;54:5596–5601. doi: 10.1167/iovs.13-12142. [DOI] [PMC free article] [PubMed] [Google Scholar]


