ABSTRACT
Eyelid myokymia is a localised movement disorder of the orbicularis oculi muscle with involuntary, fine, continuous, and undulating contractions. Although this entity is thought to be peripheral nerve origin, it rarely occurs with an intracranial lesion. The authors report a case of eyelid myokymia with concomitant cerebral tumour. A 52-year-old woman had a 6-month history of left eyelid myokymia accompanied by upper eyelid ptosis and lower eyelid reverse ptosis. Magnetic resonance imaging showed a solid mass measuring 20 × 25 × 20 mm in the temporal lobe of the cerebral cortex, showing isointense on T1-weighted and hyperintense on T2-weighted images. The clinical diagnosis was cerebral astrocytoma.
KEYWORDS: Cerebral tumour, eyelid, myokymia, ptosis
Introduction
Eyelid myokymia is a localised movement disorder of the orbicularis oculi muscle with involuntary, fine, continuous, and undulating contractions. It is characterised by rhythmic or semi-rhythmic bursts of a single motor unit discharging at a rate of 3 to 8 Hz.1 Eyelid myokymia is the most common type of facial myokymia, in which one or more muscles of the face are affected.2
Eyelid myokymia is mainly of peripheral nerve origin, whereas facial myokymia is often associated with brain lesions.2 The eyelid myokymia typically shows a self-limiting course lasting for a couple of days to months and often involves the lower eyelid in cases of fatigue, stress, physical exertion, or excessive caffeine intake.2–4
Eyelid myokymia, although benign in nature, rarely occurs with an intracranial lesion. Only three cases with multiple sclerosis have been reported with regard to the eyelid myokymia.1–3 We report here the first case of eyelid myokymia with a concomitant cerebral tumour.
Case report
A 52-year-old female was referred to our clinic for left eyelid myokymia associated with a lateral pulling sensation, presenting persistently for 6 months. She had no relevant medical history.
Physical examination revealed fine, rhythmic contractions of the left upper and lower eyelids, without involvement of the other part of the face. Although she also had upper eyelid blepharoptosis with brow elevation as well as mild lower eyelid reverse ptosis (Figure 1), she illustrated no signs of an oculomotor nerve palsy. No other neurological manifestations were demonstrated in relation to the central and peripheral nervous systems.
Figure 1.
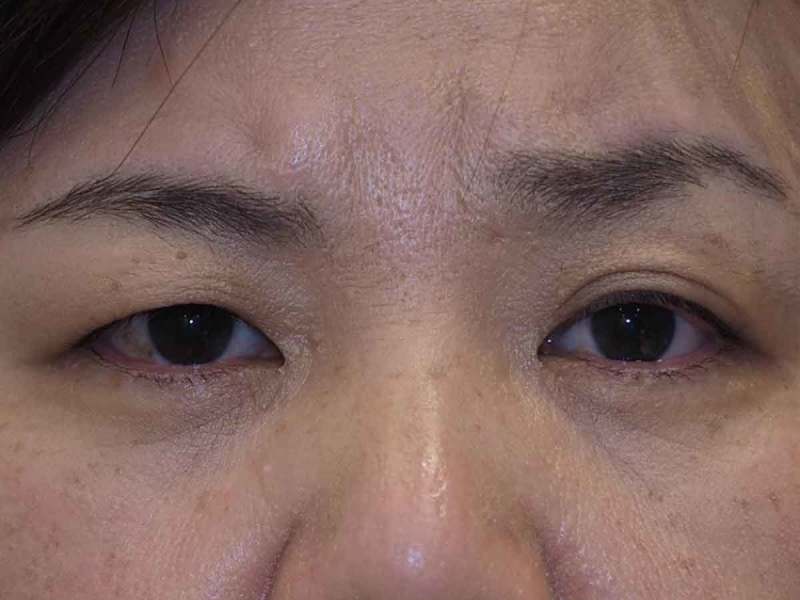
Face photograph. Left upper eyelid ptosis with mild reverse ptosis is shown. Brow elevation is also demonstrated, which further makes the upper eyelid crease more conspicuous than the contralateral side.
Magnetic resonance imaging (MRI) depicted a solid mass in the temporal lobe of the cerebral cortex with extension to the cerebral peduncle (Figure 2A–D). It was 20 × 25 × 20 mm in size and was isointense on T1-weighted and hyperintense on T2-weighted images, both with respect to grey matter (Figure 2A–C). The tumour showed no contrast enhancement with gadolinium. Constructive interference in steady-state MRI illustrated no compressive lesions at the exit of the left facial nerve (Figure 2D).
Figure 2.
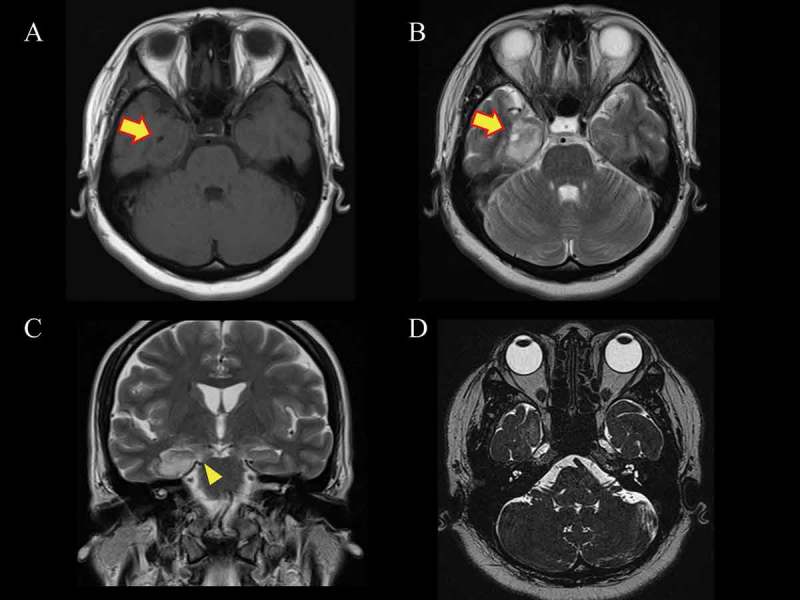
Magnetic resonance imaging (MRI) studies. Axial images show (A) isointensity (arrow) in T1-weighted and (B) hyperintensity (arrow) in T2-weighted images. (C) A coronal T2-weighted image shows extension of the tumour to the cerebral peduncle (arrowhead). (D) Constructive interference in steady-state MRI demonstrates no tumour involvement on the facial nucleus or facial nerve.
A diffuse cerebral astrocytoma was suspected based on the above findings. She was treated conservatively, as she had no other neurological findings except for eyelid myokymia. The eyelid myokymia was still persistent at 3-month follow-up.
Discussion
We reported the first case of eyelid myokymia with concomitant cerebral tumour. A cerebral tumour generally shows neurological deficits, visual impairment, headache, nausea, and seizures as accompanying symptoms.5 Left eyelid myokymia was, however, the only symptom of the present case.
Eyelid myokymia demonstrates facial nerve hyperexcitability of peripheral or central origin.2–4 The nucleus and/or the supranuclear portion of the facial nerve are thought to be the causative lesions.3 The tumour extension to the cerebral peduncle in our case has likely resulted in suppression of the inhibitory pathway on the supranuclear level. The current case did not illustrate a facial nucleus lesion in the pontine tegmentum on MRI, which was similar to the three reported cases with multiple sclerosis.2–4
Upper eyelid ptosis with reverse ptosis is a common presentation of eyelid myokymia. This appearance results from the continuous involuntary contractions of the orbicularis oculi muscle.6 Facial nerve palsy, Horner syndrome, and enophthalmos also illustrate similar symptoms with different pathologies.7 The facial nerve palsy decreases the tone of the orbicularis oculi muscle, resulting in disuse atrophy of the upper and lower eyelid retractors.8 Horner syndrome, in relation to an interrupted oculosympathetic pathway, attenuates the smooth muscle component of the eyelids. The enophthalmos lowers the position of the Whitnall’s ligament with decreased support by the globe, which causes functional lengthening of the levator palpebrae superioris9; pseudo-reverse ptosis may be seen when the globe is depressed.
There were several atypical features of eyelid myokymia in the present case. The symptoms were present in the upper eyelid, in addition to the lower eyelid, which is typically involved in this entity.2–4 The symptoms continued for 6 months, whereas eyelid myokymia is usually self-limiting. The subjective experience of a lateral pulling sensation was the other atypical feature in the current case.2 These features motivated us to take an MRI to search for a possible intracranial lesion causing hemifacial spasm and eyelid myoclonus,10 although a tonic or a jerking movement was not apparent on physical examination.
In conclusion, we report the first case of eyelid myokymia with a concomitant cerebral tumour. Eyelid myokymia in this report has probably resulted from tumour extension to the cerebral peduncle. An imaging study is necessary when an atypical presentation of eyelid myokymia is demonstrated.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- [1].Horowitz SH. Hemifacial spasm and facial myokymia: electrophysiological findings. 1987;10:422–427. [DOI] [PubMed] [Google Scholar]
- [2].Banik R, Miller NR.. Chronic myokymia limited to the eyelid is a benign condition. 2004;24:290–292. [DOI] [PubMed] [Google Scholar]
- [3].Palasí A, Martínez-Sánchez N, Bau L, Campdelacreu J.. Unilateral eyelid myokymia as a form of presentation of multiple sclerosis. 2013;28:187–189. [DOI] [PubMed] [Google Scholar]
- [4].Barmettler A, Dinkin MJ, Lelli GJ Eyelid myokymia: not always benign. 2011;30:289–290. [DOI] [PubMed] [Google Scholar]
- [5].Behin A, Hoang-Xuan K, Carpentier AF, Delattre JY.. Primary brain tumours in adults. 2003;361:323–331. [DOI] [PubMed] [Google Scholar]
- [6].Shome D, Jain V, Natarajan S.. Ptosis caused by orbicularis myokymia and treated with botulinum toxin: a case report. 2007;21:444–445. [DOI] [PubMed] [Google Scholar]
- [7].Kakizaki H, Zako M, Iwaki M.. Reverse ptosis repair targeting the posterior layer of the lower eyelid retractor. 2007;23:288–291. [DOI] [PubMed] [Google Scholar]
- [8].Nielsen PJ. Upside down ptosis in patients with Horner’s syndrome. 1983;61:952–957. [DOI] [PubMed] [Google Scholar]
- [9].Guyuron B, Harvey D.. Periorbital and orbital aging: senile enophthalmos as a cause of upper eyelid ptosis. 2016;138:31e–37e. [DOI] [PubMed] [Google Scholar]
- [10].Wang A, Jankovic J.. Hemifacial spasm: clinical findings and treatment. 1998;21:1740–1747. [DOI] [PubMed] [Google Scholar]


