Abstract
Normative (NF) and personalized feedback (PF) are moderately effective brief interventions for at-risk drinking middle-aged and older adults. This study tested the feasibility of online feedback for drinkers 50 and older. This study’s aims were to identify whether there is differential effectiveness of PF over NF in prompting drinkers 50 years old and older to plan for change and to determine potential preferences for intervention among adult drinkers 50 and older with practical knowledge about computers.
Method
Using Amazon’s Mechanical Turk, 138 male and female drinkers aged 50 to 75+ were recruited to complete an online survey that asked about their: perceptions of their drinking, quantity and frequency of drinking, and any comorbid health and/or mental health disorders/medications. They were then provided either NF or PF. NF provided information about how participants’ drinking compared to their same age and gendered peers. PF provided information about level of risk to health and provided recommendations for safe levels of drinking. After feedback, participants were evaluated for their reactions (e.g., “How much does this worry you?”) and their plan to change their drinking. Participants were asked about preferences for interventions.
Results
80% of participants rated themselves a no or low-risk drinker, yet 52.2% were found to be at-risk drinkers. Overall, participants reported feedback was helpful, and 43.9% made some kind of plan to change. Participants in NF were significantly more likely to make a plan for change than those in PF. Participants reported that they most preferred an online (40.9%) or a brief in-person (31.8%) intervention.
Conclusion
Findings revealed that brief online feedback was feasible, though limited to those who are computer knowledgeable. Unexpectedly, NF outperformed PF, suggesting that peer comparisons may be more motivating for adults 50 and older than previously thought. Finally, an online intervention appears to be a preferred intervention for alcohol use among this particular group of drinkers.
Keywords: normative feedback, personalized feedback, alcohol, older adults, online intervention
1. Introduction
With the aging of the US population, increasing attention is being given to substance use among adults in later life (Institute of Medicine, 2012). Among middle-aged and older adults, alcohol remains the most commonly used substance (Blazer & Wu, 2009b; Lin et al., 2011), and despite an overall decline in the rates of alcohol use as they age, the prevalence of at-risk drinking among adults 50 and older is quite high (Blazer & Wu, 2009a), and it is climbing (Han, Moore, Sherman, Keyes, & Palamar, 2017). For men under 65 years old, at-risk drinking is defined as consuming more than 14 standard drinks per week and/or more than 4 standard drinks on any one occasion (National Institute on Alcohol Abuse and Alcoholism, 2013). For women and men 65 and older, at-risk drinking is defined as consuming more than 7 standard drinks per week and/or more than 3 standard drinks on any one occasion. Using data from the National Survey on Drugs and Health (NSDUH), 19% of men and 13% of women ages 50 to 64 were found to be at-risk drinkers (Blazer & Wu, 2009a). Among those 65 and older, at-risk drinking occurred for 13% of men and 8.1% of women. Due to the fact this study defined at-risk drinking as an average of greater than 2 standard drinks per day, these prevalence rates likely underrepresent the true level of at-risk drinking among middle aged and older adults. A recent study using 2014 NSDUH data found that rates of heavy drinking (defined as drinking more than 5 drinks on more than 5 occasions in one month) were as high as 14.9% among adults 50 and older (ages 50–64: 19.1%, 65+: 9.0%), while rates of AUD were 3.5% (ages 50–64: 4.8%, 65+: 2.1%) (Han et al., 2017).
Adults in later life have unique vulnerabilities to the negative consequences of heavy drinking. Biological and cognitive changes that begin as early as age 50 (Hanson, 2011) increase the effects of alcohol (Gilbertson, Ceballos, Prather, & Nixon, 2009). Alcohol’s effects are also increased by age-related reductions in lean body mass, and total body water as well as gastrointestinal changes (Moore, Beck, Babor, Hays, & Reuben, 2002; Moore, Kuerbis, Sacco, Chen, & Garcia, 2017), subsequently causing higher blood alcohol levels for a longer period of time than in younger counterparts. Changes in the brain, including structural changes and thinning of the blood brain barrier (Moore et al., 1999; Oslin, 2000, 2004), also cause prolonged exposure to alcohol and potentially more acute effects.
In the context of these biological changes, at-risk drinking can have a deleterious effect on the health and well-being of aging adults. A premature loss of independence (Balsa, Homer, Fleming, & French, 2008), and a greater rate of falls among older adults are associated with at-risk drinking (Mukamal et al., 2004). At-risk drinking older adults screened in primary care were also found to have far poorer mental health functioning than those drinking at-low risk levels (Blow, Walton, & Barry, 2000). In addition, among individuals 50 and older, rates of comorbid medical conditions and taking medications for which drinking alcohol is proscribed increases with age (Moore, Whiteman, & Ward, 2007), often causing a worsening of symptoms.
While heavy drinking may pose a greater risk to adults later in life compared to young adults, adults 50 and older are less likely to access or seek help, either in primary or specialty care, for alcohol-related problems (Bartels et al., 2004; Kuerbis, Sacco, Blazer, & Moore, 2014). Middle-aged or older at-risk drinkers may not recognize problems as alcohol related—instead attributing them to a natural part of aging (Blow & Barry, 2000; Rodin, 1986). Barriers to specialized treatment that older adults may experience include stigma and shame around dealing with alcohol use and related problems later in life, geographical isolation, inability to pay, or difficulties with transportation (Center for Substance Abuse Treatment, 1998; Fortney, Booth, Blow, Bunn, & Cook, 1995; Kuerbis & Sacco, 2013). For these reasons, primary care and other non-traditional settings (e.g., senior and community centers) are the focal point of prevention and intervention for aging adults who are at-risk drinkers (Barry, Blow, Cullinane, Gordon, & Welsh, 2006; Sacco & Kuerbis, 2013; Schonfeld et al., 2010), usually in the form of screening and brief intervention (SBI).
SBI has been the mainstay of intervention among older adult at-risk drinkers (Blow & Barry, 2000; Kuerbis & Sacco, 2013), and there is compelling evidence that SBI is effective in reducing at-risk drinking within this population (e.g., Fink, Elliot, Tsai, & Beck, 2005; Fleming, Manwell, Barry, Adams, & Stauffacher, 1999; Moore et al., 2011; Schonfeld et al., 2010). A critical component of brief interventions is providing feedback about participants’ drinking, after participants complete an assessment. Feedback can be either normative, personalized, or a combination of both. Normative feedback (NF) is when a person’s quantity and frequency of drinking is compared to the average drinking rates among their same age and gender peers. Personalized feedback (PF) is when results of a more in depth assessment of drinking and health are provided, including a person’s level of risk for developing alcohol use disorder or exacerbating other health problems.
While feedback is a common element to all SBIs for this population, there have been no direct tests of the efficacy of either NF or PF alone in facilitating planning for change or drink reduction among adults 50 and older. Only one major study of older drinkers utilized NF (Barry et al., 2006), while a majority of other studies used some form of PF (Fink et al., 2005; Fleming et al., 1999; Gordon et al., 2003; Kuerbis et al., 2015; Moore et al., 2011). However, in every study of SBIs with older adults, feedback is combined with extensive education, time consuming follow ups with physicians, nurses, or social workers, and/or some kind of motivational or behavioral intervention, such as creating a plan for reduced drinking (e.g., Barry et al., 2006; Fleming et al., 1999). Thus, the impact of NF or PF alone on planning for change or drink reduction among older adults remains unknown. Understanding the specific impact of these types of feedback, and their potential for a differential effect, is key to providing the most effective, low-cost, parsimonious, and standardized intervention that can be used broadly with at-risk drinkers later in life.
Providing feedback online is one potential way to reach a broad range of aging adults who may not regularly access primary care. Online PF for a general population of adults demonstrates effectiveness in reducing drinking up to 6 months, when compared to a no-intervention control (Cunningham, 2012). Therefore, it is reasonable to assume that online feedback tailored for middle aged and older adults could be feasible and effective. A study of the individuals who visited alcoholscreening.org during 2013 (Masukawa, Rosenbloom, Helmuth, Liao, & Moore, 2015) reported that over 18,000 individuals between 50 and 64 years old and 3,485 individuals aged 65 to 80 years old visited the website for screening of alcohol use. Over 80% of the oldest group reported exceeding the recommended daily limit of drinking.
Efforts to provide online intervention specifically to at-risk drinking adults 50 and older are in their nascent stages, yet thus far, they demonstrate feasibility (Fink et al., 2016). It remains unknown which form of feedback is most effective for adults 50 and older—normative or personalized. While there is evidence that both are effective, it is theorized that personalized would be more effective due to evidence that opinions of health care providers and concerns about health are particularly important motivators for reduced substance use among this age group (Satre & Arean, 2005) and given findings that PF outperforms NF in a general population in reducing drinking (Cunningham, Murphy, & Hendershot, 2015).
Given the continued need for intervention in settings other than primary care and existing gaps in the literature, a pilot study was implemented to address three primary research aims: (1) to determine the feasibility and acceptability of providing simple online feedback for adults 50 and older; (2) to identify whether there is differential effectiveness of personalized feedback over normative feedback in prompting drinkers 50 years old and older to plan for change, and (3) to determine potential preferences for intervention among adult drinkers 50 and older with practical knowledge about computers and the internet.
2. Method
To address these aims, a quasi-experimental pilot study was conducted.
2.1 Recruitment
Amazon Mechanical Turk (MTurk), an online labor market, was used to recruit participants. MTurk provides an online interface through which “workers” are asked to complete “human intelligence tasks” (HITs). HITs range in their content but can include beta-testing software or other products, cleaning data, and completing surveys. "Requesters" publish HITs and are responsible for paying the workers for completing the HIT or task. Compensation for successfully completing a HIT ranges in value but is often below $1. MTurk increasingly is used for behavioral and social sciences research (Mason & Suri, 2012), and it demonstrates a track record of comparable demographics and task performance to more traditional sampling methods (Buhrmester, Kwang, & Gosling, 2011; Rand, 2012), particularly to other online recruitment methods.
2.2 Procedures
2.2.1. Initial eligibility
Participants had to be workers registered on MTurk. To complete the HIT associated with this study, workers had to have received a HIT approval rating of 90% out of at least 500 completed HITs by other requesters. This limited the potential sample to workers who had been evaluated by other requesters as performing well (i.e., completed a task successfully without error) and to those with practical knowledge of computers and internet use. Eligibility was restricted to only United States residents.
2.2.2. Condition assignment through alternating recruitment
Due to technical limitations of the online survey platform, random assignment to the two conditions (NF and PF) was not possible. Two separate surveys, one for NF and one for PF, were created. Condition assignment occurred as individuals enrolled in the study. The first 100 people recruited were assigned to the NF survey, the second 100 to the PF survey and so on. There were a total of six samples recruited, three for normative feedback (NF) and three for personalized feedback (PF). These samples were aggregated into one group for analysis.
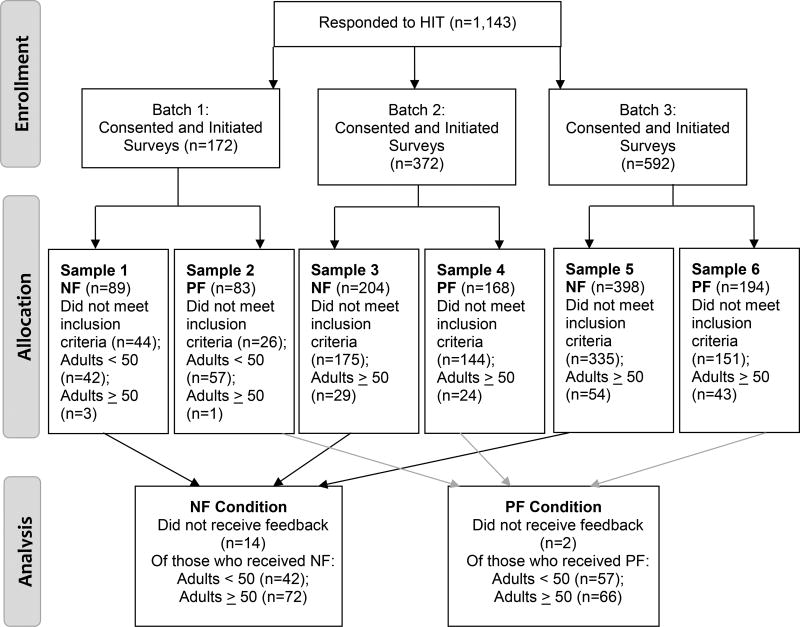
Samples were recruited in pairs, such that a NF and a PF sample were recruited at the same time of day and day of week on consecutive weeks (rather than simultaneously). Pairing the samples in this way was an attempt to control for consistency across the two survey types in the availability of the labor pool during that time and day. Each pair of samples was called a batch. There were a total of three batches, and they each varied by time of day and day of week. This varied the potential labor pool across batches in which our recruitment took place. All batches were implemented within a period of three weeks during early 2016. Figure 1 represents the flow of study enrollment.
Figure 1.
2.2.3. Connecting to the survey
The HIT for this study was entitled: “Answer a brief survey about your lifestyle for a research study”. Within the HIT, there was a brief description of the task, and then workers were provided a link to an external, web-based survey. The survey was implemented using SurveyMonkey.com. On the opening page of the survey was a fuller description of the study and a statement of consent to participate. Participants were required to click on a button labeled "I consent to participate" to proceed to the screening for eligibility (N=1,143).
2.2.4. Study eligibility screening
Initial information about the survey's purpose related to age and drinking were deliberately kept vague (i.e., we did not mention the age group of interest) to encourage potential participants to report on their age and drinking honestly. For study eligibility, within the survey, participants answered the question: “do you drink alcohol?” For participants who answered no, the survey ended, and they were excluded from the study. To further discourage workers to misreport their age, younger adults were included in our study recruitment during Batch 1. Due to the low response rate of adults 50 and older, the next two batches excluded individuals reporting age younger than 50.
2.2.4.1. Study exclusion due to potential participant fraud
Any participant who reportedly completed the entire survey in less than 3 minutes was assumed to have not completed the survey correctly and was excluded from the final sample. Additionally, the age question was repeated once in the middle of the survey as a validity check. Anyone who responded with a different age was excluded. About four respondents per sample were excluded for these reasons.
2.2.5. Survey completion and study compensation
Those who responded that they were a drinker and in the appropriate age group were directed to a 25-item survey. Survey questions included items about demographics, alcohol use, attitudes towards alcohol use, health related questions, feedback (either NF or PF, described further below), and then questions about perceptions of the feedback and any changes they planned on making to their drinking. Participants completed the survey in about five minutes, on average. After the participants completed the survey and their response set was vetted by the researcher (i.e., the time it took to complete the survey was at least longer than a minute), the participant was compensated 80 cents via MTurk. Once a worker is compensated for a completed HIT, whether they were eligible for the study or not, that worker cannot reopen the HIT to connect to the survey link again. Additionally, IP addresses of the workers were blocked via SurveyMonkey so they could not retake the survey from the same device. From the first batch, a total of 99 younger adult drinkers completed the survey. A total of 138 adult drinkers 50 and older completed the surveys.
2.3 Measures
2.3.1. Pre-feedback
2.3.1.1. Demographics
Participants were asked their age and gender (female, male, transgender, other).
2.3.1.2. Health questions
Participants were asked six questions from the Comorbid Alcohol Risk Evaluation Tool (CARET) (Moore et al., 2002; Moore et al., 2011), a descendent of the Alcohol Related Problems Survey (Fink et al., 2002). Questions focused on their medical conditions, physical and psychiatric symptoms, and medications they were currently taking. Responses were used to provide feedback for the PF condition only.
2.3.1.3. Self-perceptions of drinking
Participants were asked five questions about their perceptions of their drinking prior to feedback. On a scale of 1 (Not at all) to 8 (Extremely), participants were asked 1) if the amount that they drank was excessive (excessive); 2) how much their current drinking is a problem; 3) how much their current drinking is a problem for others (problem for others) in their lives; 4) how much their current drinking worries them; and a variable attempting to capture level of control over drinking, 5) “when you have planned to not drink, how much effort does it take for you not to drink alcohol when it is presented to you?” (effort).
2.3.1.4. Self-reported quantity and frequency of drinking
Participants reported on their actual drinking through a series of questions based on the Form 90 QFV-30 (Miller & Del Boca, 1994). Responses were used to provide feedback, described below.
2.3.2. Post-feedback
After either NF or PF were provided, participants were asked a series of questions about their reactions and perspectives related to that experience.
2.3.2.1. Personal reaction
Participants responded on a scale of 1 (Not at all) to 8 (Extremely) to the questions "how surprised are you by the feedback?" (surprise) and "how much does the feedback worry you?" (worry).
2.3.2.2. Expectation
Participants were asked to rate the feedback as "better than expected", "as expected" or "worse than expected".
2.3.2.3. Newness of information
Participants were asked if the information provided in the feedback was new. Response set was yes or no.
2.3.2.4. Plan to change
Next, participants were asked to describe their plan to change related to drinking in the next 30 days. Responses ranged from (0) “I do not plan to change my drinking” to (3) “I plan to quit drinking”. Next participants were prompted to report on their commitment to and confidence in their ability to achieve their plan on separate scales ranging from (1) Not at all to (8) Extremely.
2.3.2.5. Belief in the accuracy of feedback
To avoid biasing item responses earlier in the survey, the last section of the survey asked about believability of the feedback. First asked was “how accurate does the information you received about your drinking seem to you?” (pre-belief). A 5-point Likert response scale included anchors (0) Not at all accurate to (8) Definitely accurate. We next informed the participants of the sources of the information used for the feedback and repeated the above question (post-belief).
2.3.2.6. Preferred motivator
At the end of the survey, participants were asked “What information or scenario would motivate you to change your drinking habits?” The response set included selection of possible situations, such as “A family member expresses concern about your drinking” and “You are seriously ill”. Participants could also write in the scenario that would be most motivating.
2.3.2.7. Preferences for intervention
Participants were asked the same question about their preferences for potential help with their drinking in two ways. The question was “If you were interested in getting help to reduce or abstain from drinking, which of the following would interest you?” The first time it was asked participants could select all that applied. The second question asked which they most preferred. The response set included: an online intervention, a text messaging intervention, brief telephone based counseling, brief in-person counseling. A space was also provided for them to fill their own options for both questions.
2.4 Conditions
2.4.1. Normative feedback (NF)
NF comprised two sentences of information for the participant. Participants were directed to one of 24 possible statements of feedback. Each statement provided a unique percentile rank of drinking in relation to peers based on participants’ reported average number of standard drinks per week, age and gender. For example, for a man: “You reported drinking 1 standard drink per week. You drink more than 27% of men your age.” Percentile ranks for the normative comparisons were made using data from the 2009 National Survey on Drug Use and Health (Substance Abuse and Mental Health Services Administration, 2010). Although binge drinking was assessed, it was not a factor in determining feedback nor included in participant education about drinking.
2.4.2 Personalized Feedback (PF)
PF was based on evaluation of risk via the CARET. Based on participants’ responses to the questions about weekly drinking, medical conditions and symptoms, and medications, participants were directed to one of five different possible statements of feedback. In addition to being told their level of risk, participants were given safe drinking guidelines relevant to their risk level, as recommended by the National Institute of Alcohol Abuse and Alcoholism’s Rethinking Drinking (National Institute on Alcohol Abuse and Alcoholism, 2013). An example of personalized feedback for someone reporting a serious medical condition was “Given your age, gender and health profile you are considered an at-risk drinker. Given your health profile, it’s possible that having any alcohol could negatively affect your health. For your optimal health, it is recommended that you abstain from drinking.” Again, while binge drinking was assessed, it was not a factor in determining feedback, and participants were not educated about binge drinking.
2.5 Analytic Plan
All analyses were performed using SPSS 22.0 (IBM Corp., Released 2013). For the purposes of this analysis the younger adult sample was excluded. Later analyses will compare the two age groups. Our first aim, to assess the feasibility and acceptability of the online intervention was explored last, described further below. To address our second aim examining the differential effectiveness of the two types of feedback, basic descriptives of the two condition groups were conducted. We assessed for condition differences using t-tests and chi-square, where appropriate, on demographics, health conditions, pre-feedback perceptions of drinking, and drinking itself. Six people did not answer any of the post-feedback questions and thus were excluded from subsequent analyses. Next, OLS regression, using the hierarchical method, was used to determine whether there was a differential response on plan for change based on feedback type. Pre-feedback variables on which there were condition differences were used as covariates and entered into the model first before condition.
For our third aim, to explore the preferences of our respondents for formats of potential intervention, we generated descriptives of preferences for brief interventions related to drinking among this sample of adults. Finally, for our first aim, we evaluated the response rate, the perceptions of feedback and rated helpfulness of the interventions overall.
3. Results
3.1 Condition Differences
3.1.1 Descriptives of the Sample Pre-feedback
3.1.1.1. Demographics and health related items
Table 1 shows the demographics of the 138 adults 50 and older. A little over half the sample (54.1%) was male. A majority of the sample (63%) was just over 50 years old, with the remaining proportion ranging in age from 56 to 70 and older. Just over a third (35.5%) reported having a medical condition, with high blood pressure being the most common. A total of 60% of the sample reported experiencing at least one medical symptom, with problems sleeping being the most common (42.9%). Over half (56.7%) of the sample reported taking no medication—prescribed or otherwise. Blood pressure medication was the most common reported medication (18.8%). There were no significant condition differences on any demographic or health related item, with one exception, proportion of experiencing medical symptoms. Within the NF condition, 71.8% of participants reported having at least one medical symptom compared to 52.4% of PF participants, Fisher’s exact χ2 (1) = 5.4, p < .05.
Table 1.
Characteristics of Participants
| (N=138) M (SD) or % |
|
|---|---|
| Male | 54.1 |
| Age | |
| 50–55 | 63.0 |
| 56–59 | 14.5 |
| 60–64 | 14.5 |
| 65–70 | 6.5 |
| 70+ | 1.4 |
| Medical Conditions | |
| High blood pressure | 24.8 |
| Depression | 19.5 |
| Diabetes | 5.3 |
| Medical Symptoms | |
| Problems sleeping, sometimes or often | 42.9 |
| Feeling sad or blue, sometimes or often | 33.8 |
| Heartburn, stomach pain, nausea or vomiting | 20.8 |
| Memory problems | 21.1 |
| Having a fall or being unsteady on your feet | 7.5 |
| Medications Taken a Minimum of 3–4 Times per Week | |
| No medications | 56.7 |
| Blood pressure medication | 18.8 |
| Arthritis and pain medications (ibuprofen, Celebrex) | 13.0 |
| Depression medications (SSRIs, SNRIs) | 10.9 |
| Ulcer and stomach medications (Zantac, Pepcid, Prilosec) | 8.7 |
| Non-prescription medications for allergies or sleep | 8.7 |
| Coumadin (blood thinner) | 3.6 |
| Prescription sedatives or sleeping medications | 3.6 |
| Nitrate medicines for heart problems | 2.9 |
| Plavix (blood thinner) | 2.9 |
| Stronger pain medications (opiates) | 2.9 |
3.1.1.2. Perceptions of and reported amount of drinking
Table 2 reports the pre-feedback descriptives of participants’ perceptions of their drinking by condition. On the whole, participants’ perceptions were at the low end of the scale, indicating that they perceived their drinking was not excessive; not a problem or a problem for others; little effort was required to refuse a drink; and their drinking did not worry them. There were statistically significant condition differences on perceptions of drinking, with PF participants reporting that their drinking was significantly more excessive, a problem, needed effort to control, and worrisome than their NF counterparts. Interestingly, there were no condition differences on reports of actual drinking (Table 2), which was on average in the low-risk range. A large majority of the sample rated themselves as either a no or low risk drinker. According to CARET ratings of risk, 52.2% of the sample overall was deemed an at-risk drinker. There were no condition differences on proportion of type of risk drinker (Table 2).
Table 2.
Pre-feedback Descriptives of Participants
| NF (N=70) |
PF (N=66) |
|
|---|---|---|
|
| ||
| M (SD) or % | M (SD) or % | |
| Perceptions of drinking | ||
| Alcohol use is excessivea* | 2.5(1.9) | 3.4 (2.4) |
| Drinking is a problema* | 2.2 (1.7) | 3.0 (2.3) |
| My drinking is a problem for othersa | 2.0 (1.7) | 2.6 (2.1) |
| Effort needed to refuse a drinka* | 2.5 (2.0) | 3.6 (2.7) |
| My drinking worries mea* | 2.3 (1.9) | 3.1 (2.3) |
| Drinking | ||
| Number of days drink per week | 2.8 (1.9) | 3.2 (1.8) |
| Drinks per drinking day | 2.5 (1.6) | 3.0 (2.4) |
| Typical number of drinks on heaviest days | 4.7 (3.0) | 4.8 (3.2) |
| Mean standard drinks per week | 7.4 (7.7) | 8.6 (7.6) |
| How many days in the past 30 binge drankb | 2.4 (1.6) | 2.3 (1.4) |
| Perception of at-risk drinking | ||
| I would rate myself as: | ||
| A no-risk drinker. (I feel like I hardly drink.) | 33.8 | 44.3 |
| A low-risk drinker. (I drink moderately, about the same as everyone.) | 51.5 | 44.3 |
| An at-risk drinker (I drink more than I should.) | 13.6 | 11.4 |
| CARET rated at-risk drinker | ||
| A low- or no risk drinker | 41.7 | 54.5 |
| An at-risk drinker | 58.3 | 45.5 |
Range was 1 Not at all to 9 Extremely
Binge defined as 5 or more drinks for men, 3 or more for women.
p < .05,
p < .01
3.1.2 Perceptions of Feedback
Table 3 reports the reactions of participants to the respective feedback types. Overall, participants were mildly surprised and mildly worried by the feedback. Those who received PF were significantly more surprised by the feedback than those in NF, (t(130) = 3.2, p < .01). A majority reported the feedback was as expected, demonstrating a high level of knowledge pre-feedback of their drinking levels. Participants found the feedback, regardless of type, moderately helpful. They also rated the feedback to be highly believable, particularly after informing them of the source of the data used in the feedback (e.g., 2009 National Survey on Drugs and Health for NF and Rethinking Drinking for PF, see above).
Table 3.
Post Feedback Descriptives
| NF (N=69) M (SD) or % |
PF (N=63) M (SD) or % |
|
|---|---|---|
| Surprise** | 3.2 (2.5) | 4.7 (2.8) |
| Worry | 2.6 (2.3) | 3.1 (2.2) |
| Expectation. This information was: | ||
| Better than Expected | 15.9 | 14.3 |
| As Expected | 65.2 | 49.2 |
| Worse than Expected | 18.8 | 36.5 |
| Yes, this information was new. | 45.2 | 63.5 |
| How helpful was this information about your drinking? | 5.1 (2.2) | 5.1 (2.3) |
| Belief the Feedback was Accuratea | ||
| Before given source of information | 6.2 (1.9) | 5.8 (2.5) |
| After given source of informationb | 7.1 (1.9) | 6.4 (2.3) |
| Plan for Changec | 1.7 (0.9) | 1.5 (0.6) |
| Confidence to Change Drinking | 6.2 (1.6) | 5.9 (1.9) |
| Commitment to Change Drinking | 6.4 (1.8) | 6.5 (1.4) |
Range was from 0 (Not at all accurate) to 5 (Somewhat accurate) to 8 (Definitely accurate).
Difference between belief in accuracy of feedback before and after information was given was significant (t(131) = −6.5, p < .001)
Anchors for plan for were 0 “I am not planning on changing my drinking” to 3 “I’m planning to quit drinking”
Note: No significant gender differences. Only significant difference by feedback type was in regards to surprise. Significant mean differences emerged: (t(130) = 3.2, p < .01);
p < .05,
p < .01,
p < .001
3.2. Aim 2: Plan for Change
Just under half of the entire sample (43.9%) reported planning for at least some reduction in their drinking. Table 3 reports the means and standard deviations for plan for change, commitment to the plan, and confidence in achieving the plan by condition. Participants were moderately to highly committed to the plan for change and confident that they could achieve their plan.
3.2.1 Feedback Type Predicting Plan for Change
Pre-feedback worry was significantly and highly correlated (r ranged from .63 to .86, ps < .001) with all of the pre-feedback variables in which conditions were found to be significantly different from one another. Therefore, to prevent issues of multicollinearity, pre-feedback worry was the sole covariate used to account for condition differences on these variables. Pre-feedback worry was a highly significant predictor of plan for change (B = .16, SE = .03, p < .001), such that with an increase in pre-feedback worry, plan for change also increased. Medical symptoms did not predict plan for change (B = .02, SE = .13, p = .89). When condition was entered into the model there was a significant change in adjusted R2, F change (1, 128) = 4.2, p <.05, such that the model with condition explained 19.9% of the variance in plan for change. There were significant condition differences such that being in NF predicted a more drastic plan for change than PF (B = −.26, SE = .13, p < .05).
3.3 Aim 3: Personal Motivators and Preferences for Intervention
3.3.1. Self-identified Motivators for Change
Table 4 reports the percentage of participants who endorsed the listed reasons for change. Over half of the respondents reported that advice from a doctor or being seriously ill would be a primary motivator for planning to quit drinking. Family members’ perspectives also ranked as motivating among a large proportion of participants. Response written for “Other” included wanting to lose weight, wanting to save money, and “if it affected my ability to work”.
Table 4.
Motivators and Preferences for Intervention
| (N=132) M (SD) or % |
|
|---|---|
| Potentially Motivating Situations | |
| You are seriously ill. | 58.3 |
| A doctor says you should reduce your drinking. | 56.8 |
| You start to feel run down. | 40.9 |
| A family member expresses concern about your drinking. | 39.4 |
| Your friends suggest you drink less. | 28.0 |
| Learning about recommended limits. | 25.0 |
| Nothing would motivate me to change my drinking. | 7.6 |
| Other | 6.8 |
| Types of Interventions in which Participants would be Interested | |
| An internet based intervention with dedicated website. | 42.5 |
| A brief number of in-person counseling sessions. | 35.5 |
| A brief number of telephone based counseling sessions. | 17.4 |
| A text messaging intervention to motivate towards goals. | 15.2 |
| Other | 10.9 |
| Types of Interventions Participants Preferred Most | |
| An internet based intervention with dedicated website. | 44.3 |
| A brief number of in-person counseling sessions. | 34.4 |
| A text messaging intervention to motivate towards goals. | 14.8 |
| A brief number of telephone counseling sessions. | 6.6 |
3.3.2. Preferences for Intervention
The most popular types of interventions reported by respondents were a dedicated website and a brief number of in-person counseling sessions. These two types of interventions also had the highest endorsement of intervention most preferred, with a dedicated website being the most preferred among this group of computer knowledgeable adults over 50.
4. Discussion
Given the overall response and survey completion rates, this study found that an online feedback intervention is feasible and acceptable (Aim 1) to adults 50 years and older who are computer knowledgeable. These results are consistent with the limited existing literature on online interventions for middle aged and older adult drinkers (Fink et al., 2016; Masukawa et al., 2015). With just these brief feedback interventions, 43.9% of participants planned for some kind of reduction to their drinking and, on average, they reported the feedback was moderately helpful. In addition, participants reported an overwhelming preference for an online intervention (Aim 3) to help with drinking over other options, including in-person counseling. This preference is not surprising given the potential older adults have for avoiding traditional routes of treatment due to stigma or other concrete barriers to treatment. Taken together, these findings have important implications for broadening access to a set of frontline online interventions for middle aged and older adults, providing not only an initial educational intervention but also a gateway for higher levels of care for individuals who may unknowingly be drinking at at-risk levels.
Contrary to hypotheses (Aim 2), individuals in NF made more drastic plans for change based on feedback than those in PF. This finding is inconsistent with previous studies that examined the efficacy of online NF with a general adult population (Cunningham et al., 2015; Kuerbis, Muench, Lee, Pena, & Hail, 2016), which found online NF to be ineffective in reducing drinking or planning for change. It would appear that for this group of adult drinkers, peer comparisons may be more compelling (or at least less aversive) than basic health information in prompting plans for change. This finding is especially interesting given that the top three listed motivators for changing drinking were health related. One possible explanation for why this might be is the difference in tone and inferred message of each type of feedback. NF was neutral and did not provide guidance for safe drinking, allowing for a bit more autonomy of decision making. PF not only provided feedback about their level of risk but also recommended safe guidelines. Given how differently at-risk drinking is defined according to the CARET, the recommendations may have been perceived as overly drastic (e.g., abstinence) or aversive. Participants who received PF may have found it harder to take seriously they were at such high risk, given their generally low rates of drinking. Indeed, PF participants were significantly more likely to be surprised by the feedback than those in NF. Whatever the explanation, this finding should be taken into consideration when developing online interventions for this group of drinkers. Providing more information than normative feedback may not be helpful to the adult drinker 50 and older in helping them to achieve low or no-risk drinking.
Regardless of condition, an overwhelming majority of the drinkers 50 and older rated themselves initially as no or low risk drinkers, upwards of 85% in each condition. CARET ratings of at-risk drinking were substantially different. According to the CARET, over half (52.2%) were deemed at-risk drinkers due to medical conditions or symptoms and their quantity and frequency of drinking. This alarming difference would suggest that a vast majority of drinkers 50 and older are unaware of the risk related to comorbid health conditions or symptoms or the increasing risk of drinking to their health and well-being as they age.
4.1 Limitations
This study is an exploratory pilot study and findings should be interpreted cautiously with its limitations in mind. Results are only generalizable to drinkers 50 and older who have practical knowledge of computers and the internet, particularly those between the ages of 50–64, which made up 90% of the sample. Given how few adults 65 and older were recruited, no generalizations can be made for their age group about their response or preferences.
In addition, contextual factors may greatly impact the interpretation and application of findings. These drinkers were not treatment seekers, and they entered the survey not knowing they would be asked about drinking. It is possible that an information seeking sample of middle aged and older adult drinkers would respond differently to NF and PF. Still, this study allowed for the opportunity to understand feedback in the context of a heterogeneous sample of drinkers, many of whom were unknowingly at-risk. This is not unlike a potential community based sample that would not otherwise be seeking information on their drinking. Additionally, because there was no random assignment to condition, the comparison of the two conditions is imperfect, despite the fact that we controlled for baseline differences between the groups. It is important to also note that drinking was entirely self-report and was not corroborated by collateral sources. Finally, the outcome variable, plan to change, was a measure of intention to change only and did not capture actual behavior change. While other studies have used a similar outcome, it is not equivalent to behavior.
4.2 Future Research
Future research will include additional analyses of data from the present study to assess for moderation by gender, potential mediators of the respective conditions, and comparison to the younger sample. More broadly, future research should include a direct experimental test of these interventions and their impact on actual drinking, coupled with qualitative follow up study about what participants perceived as helpful to provide more insight into the potential mechanisms of action of feedback for this group. In particular, studying the impact of an extremely brief online intervention across a sample with a wide array of computer skill would be important. Such information would enable health care providers to better tailor interventions to specific groups of at-risk drinkers.
4.3 Conclusion
Clearly, online interventions are not a panacea for at-risk drinking among middle aged and older adults, but they should be considered an important part of a spectrum of interventions available for this group of drinkers, particularly given their long-term low cost and ease of dissemination. Consistent with previous research (Kuerbis et al., 2015), the briefest of interventions, such as those utilized here, could have important impact with relatively little cost to the health care system—assuring that precious resources are spent where they are needed most. Given that the vast majority of SBIs utilized with this population are quite extensive, with multiple components and visits with healthcare providers, online interventions offer a parsimonious and potentially cost-effective supplement to existing primary care services and in other community settings.
Acknowledgments
This study was supported with funding from the Professional Staff Congress of the City University of New York (PI: Kuerbis).
Contributor Information
Alexis N. Kuerbis, Hunter College at the City University of New York
Lisa Hail, Department of Psychiatry, University of California San Francisco.
Alison A. Moore, Division of Geriatrics, University of California San Diego
Frederick J. Muench, Northwell Health
References
- Balsa AI, Homer JF, Fleming MF, French MT. Alcohol consumption and health among elders. The Gerontologist. 2008;48(5):622–636. doi: 10.1093/geront/48.5.622. [DOI] [PubMed] [Google Scholar]
- Barry KL, Blow FC, Cullinane P, Gordon C, Welsh D. The effectiveness of implementing a brief alcohol intervention with older adults in community settings. Washington, DC: 2006. Retrieved from: http://www.ncoa.org/improve-health/center-for-healthy-aging/content-library/BI_StayingHealthyProject.pdf. [Google Scholar]
- Bartels SJ, Coakley EH, Zubritsky C, Ware JH, Miles KM, Arean PA, Levkoff SE. Improving access to geriatric mental health services: A randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. The American Journal of Psychiatry. 2004;161:1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- Blazer DG, Wu L. The epidemiology of at risk and binge drinking among middle-aged and elderly community adults: National Survey on Drug Use and Health. American Journal of Psychiatry. 2009a;166:1162–1169. doi: 10.1176/appi.ajp.2009.09010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer DG, Wu L. The epidemiology of substance use and disorders among middle aged and elderly community adults: National survey on drug use and health. American Journal of Geriatric Psychiatry. 2009b;17:237–245. doi: 10.1097/JGP.0b013e318190b8ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Barry KL. Older patients with at-risk and problem drinking patterns: New developments in brief interventions. Journal of Geriatric Psychiatry and Neurology. 2000;13:115–123. doi: 10.1177/089198870001300304. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL. The relationship between alcohol problems and health functioning of older adults in primary care settings. Journal of the American Geriatrics Society. 2000;48(7):769–774. doi: 10.1111/j.1532-5415.2000.tb04751.x. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, Gosling SD. Amazon's Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspect Psychol Sci. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance abuse among older adults: Treatment Improvement Protocol (TIP) Series 26. Rockville, MD: Substance Abuse and Mental Health Services Administration; 1998. [PubMed] [Google Scholar]
- Cunningham J. Comparison of two internet-based interventions for problem drinkers: randomized controlled trial. J Med Internet Res. 2012;14(4):e107. doi: 10.2196/jmir.2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham J, Murphy M, Hendershot CS. Treatment dismantling pilot study to identify the active ingredients in personalized feedback interventions for hazardous alcohol use: randomized controlled trial. Addict Sci Clin Pract. 2015;10:1–5. doi: 10.1186/s13722-014-0022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink A, Elliot MN, Tsai M, Beck JC. An evaluation of an intervention to assist primary care physicians in screening and educating older patients who use alcohol. Journal of American Geriatrics Society. 2005;53:1937–1943. doi: 10.1111/j.1532-5415.2005.00476.x. [DOI] [PubMed] [Google Scholar]
- Fink A, Kwan L, Osterweil D, Van Draanen J, Cooke A, Beck JC. Assessing the usability of web-based alcohol education for older adults: A feasibility study. Jmir Research Protocols. 2016;5(1) doi: 10.2196/resprot.4545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink A, Morton SC, Beck JC, Hays RD, Spritzer K, Oishi SM, Moore AA. The Alcohol-Related Problems Survey: Identifying hazardous and harmful drinking in older primary care patients. Journal of American Geriatrics Society. 2002;50:1717–1722. doi: 10.1046/j.1532-5415.2002.50467.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Manwell LB, Barry KL, Adams W, Stauffacher EA. Brief physician advice for alcohol problems in older adults: A randomized community-based trial. The Journal of Family Practice. 1999;48(5):378–384. [PubMed] [Google Scholar]
- Fortney JC, Booth BM, Blow FC, Bunn JY, Cook CL. The effects of travel barriers and age on utilization of alcoholism treatment aftercare. American Journal of Drug and Alcohol Abuse. 1995;21(3):391–407. doi: 10.3109/00952999509002705. [DOI] [PubMed] [Google Scholar]
- Gilbertson R, Ceballos NA, Prather R, Nixon SJ. Effects of acute alcohol consumption in older and younger adults: Perceived impairment versus psychomotor performance. Journal of Studies on Alcohol and Drugs. 2009;70(2):242–252. doi: 10.15288/jsad.2009.70.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AJ, Conigliaro J, Maisto SA, McNeil M, Kraemer KL, Kelley ME. Comparison of consumption effects of brief interventions for hazardous drinking elderly. Substance Use & Misuse. 2003;38(8):1017–1035. doi: 10.1081/JA-120017649. [DOI] [PubMed] [Google Scholar]
- Han BH, Moore AA, Sherman S, Keyes KM, Palamar JJ. Demographic trends of binge alcohol use and alcohol use disorders among older adults in the United States, 2005–2014. Drug Alcohol Depend. 2017;170:198–207. doi: 10.1016/j.drugalcdep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson VL. Technology skill and age: What will be the same 20 years from now? Universal Access in the Information Society. 2011;10(4):443–452. doi: 10.1007/s10209-011-0224-1. [DOI] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: Author; (Released 2013) [Google Scholar]
- Institute of Medicine. The mental health and substance use workforce for older adults: In whose hands? Washington, DC: The National Academies Press; 2012. [PubMed] [Google Scholar]
- Kuerbis A, Muench F, Lee R, Pena J, Hail L. An exploratory pilot study of mechanisms of action within normative feedback for adult drinkers. Peer J. 2016;4:e2114. doi: 10.7717/peerj.2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Sacco P. A review of existing treatments for substance abuse among the elderly and recommendations for future directions. Substance Abuse: Research and Treatment. 2013;7:13–37. doi: 10.4137/SART.S7865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Sacco P, Blazer DG, Moore AA. Substance use in older adults. Clinics in Geriatric Medicine. 2014;30(3):629–654. doi: 10.1016/j.cger.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Yuan SE, Borok J, LeFevre P, Kim G, Lum D, Moore AA. Testing the initial efficacy of a mailed screening and brief feedback intervention to reduce at-risk drinking in middle-aged and older adults: The Comorbidity Alcohol Risk Evaluation (CARE) Study. Journal of American Geriatrics Society. 2015;63(2):321–326. doi: 10.1111/jgs.13237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JC, Karno MP, Grella CE, Warda U, Liao DH, Hu P, Moore AA. Alcohol, tobacco and nonmedical drug use disorders in U.S. adults aged 65 years and older: Data from the 2001–2002 National Epidemiologic Survey of Alcohol and Related Conditions. American Journal of Geriatric Psychiatry. 2011;19(3):292–299. doi: 10.1097/JGP.0b013e3181e898b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason W, Suri S. Conducting behavioral research on Amazon's Mechanical Turk. Behavior Research Methods. 2012;44(1):1–23. doi: 10.3758/s13428-011-0124-6. [DOI] [PubMed] [Google Scholar]
- Masukawa K, Rosenbloom D, Helmuth E, Liao D, Moore AA. Older adults visit online sites for screening and brief intervention (SBI) for unhealthy alcohol use; Paper presented at the Annual Scientific Meeting of the American Geriatrics Society; Washington, DC. 2015. [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;(Suppl. 12):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Moore AA, Beck JC, Babor TF, Hays RD, Reuben DB. Beyond alcoholism: Identifying older, at-risk drinkers in primary care. Journal of Studies on Alcohol. 2002;63(3):316–324. doi: 10.15288/jsa.2002.63.316. [DOI] [PubMed] [Google Scholar]
- Moore AA, Blow FC, Hoffing M, Welgreen S, Davis JW, Lin JC, Barry KL. Primary care-based intervention to reduce at-risk drinking in older adults: A randomized controlled trial. Addiction. 2011;106(1):111–120. doi: 10.1111/j.1360-0443.2010.03229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore AA, Kuerbis A, Sacco P, Chen G, Garcia MB. Screening and assessment of unhealthy alcohol use in older adults. In: Kuerbis A, Moore AA, Sacco P, Zanjani F, editors. Alcohol and aging: Clinical and public health perspectives. New York: Springer; 2017. pp. 169–180. [Google Scholar]
- Moore AA, Morton SC, Beck JC, Hays RD, Oishi SM, Partridge JM, Fink A. A new paradigm for alcohol use in older persons. Medical Care. 1999;37(2):165–179. doi: 10.1097/00005650-199902000-00007. [DOI] [PubMed] [Google Scholar]
- Moore AA, Whiteman EJ, Ward KT. Risks of combined alcohol/medication use in older adults. American Journal of Geriatric Pharmacology. 2007;5(1):64–74. doi: 10.1016/j.amjopharm.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamal KJ, Mittleman MA, Longstreth WT, Jr, Newman AB, Fried LP, Siscovick DS. Self-reported alcohol consumption and falls in older adults: cross-sectional and longitudinal analyses of the cardiovascular health study. Journal of American Geriatrics Society. 2004;52(7):1174–1179. doi: 10.1111/j.1532-5415.2004.52318.x. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking. Bethesda, MD: 2013. Retrieved from. [Google Scholar]
- Oslin DW. Alcohol use in late life: Disability and comorbidity. Journal of Geriatric Psychiatry and Neurology. 2000;13:134–140. doi: 10.1177/089198870001300307. [DOI] [PubMed] [Google Scholar]
- Oslin DW. Late-life alcoholism: Issues relevant to the geriatric psychiatrist. The American Journal of Geriatric Psychiatry. 2004;12(6):571–583. doi: 10.1176/appi.ajgp.12.6.571. [DOI] [PubMed] [Google Scholar]
- Rand DG. The promise of Mechanical Turk: How online labor markets can help theorists run behavioral experiments. Journal of Theoretical Biology. 2012;299:172–179. doi: 10.1016/j.jtbi.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Rodin J. Aging and health: Effects of the sense of control. Science. 1986;233:1271–1276. doi: 10.1126/science.3749877. [DOI] [PubMed] [Google Scholar]
- Sacco P, Kuerbis A. Older adults. In: Vaughn MG, Perron BE, editors. Social work practice in the addictions. New York: Springer; 2013. pp. 213–229. [Google Scholar]
- Satre DD, Arean PA. Effects of gender, ethnicity, and medical illness on drinking cessation in older primary care patients. Journal of Aging and Health. 2005;17:70–84. doi: 10.1177/0898264304272785. [DOI] [PubMed] [Google Scholar]
- Schonfeld L, King-Kallimanis BL, Duchene DM, Etheridge RL, Herrera JR, Barry KL, Lynn N. Screening and brief intervention for substance misuse among older adults: The Florida BRITE project. American Journal of Public Health. 2010;100(1):108–114. doi: 10.2105/AJPH.2008.149534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Summary of national findings, NSDUH Series H-38A, HHS Publication No. (SMA) 10-4856. Rockville, MD: 2010. Retrieved from. [Google Scholar]