Supplemental digital content is available in the text.
Key Words: Bidirectional cannula, Cardiopulmonary bypass, Leg ischemia, Peripheral cannulation
Abstract
Objective
Leg ischemia is a serious complication of femoral artery cannulation. The primary aim of this study was to assess the safety and efficacy of a novel bidirectional femoral arterial cannula (Sorin Group USA, a wholly owned subsidiary of LivaNova PLC, Arvada, CO USA) that provides both antegrade and retrograde flow, in patients undergoing peripheral cannulation for cardiopulmonary bypass during cardiac surgery.
Methods
Patients undergoing routine cardiac surgery requiring femoral artery cannulation for cardiopulmonary bypass were identified preoperatively. Informed written consent was obtained in all cases. Bidirectional cannula insertion used either a surgical cut-down and wire through needle approach or a percutaneous technique. Flow in the superficial femoral artery was assessed using Doppler ultrasound after commencement of cardiopulmonary bypass. Lower limb perfusion was assessed using reflectance near-infrared spectroscopy to measure regional oxygen saturations in the cannulated limb during cardiopulmonary bypass.
Results
Fifteen patients (median age = 61.3 years, range = 26–79 years, 10 males, 5 females) underwent femoral arterial cannulation using the novel bidirectional femoral cannula between August 2016 and May 2017. Fourteen cannulae were inserted directly into the femoral artery via a surgical cut-down and wire through needle technique. One bidirectional cannula was inserted using a percutaneous insertion technique. Indications included minimally invasive mitral and aortic valve surgery, thoracic aortic aneurysm repair, and redo cardiac surgery. The median duration of cardiopulmonary bypass was 129 minutes (range = 53–228 minutes). The cannula was inserted and positioned without difficulty in 14 of 15 patients. Incorrect sizing and arterial spasm prevented correct cannula positioning in one patient. Antegrade flow in the superficial femoral artery was observed on Doppler ultrasound in 12 of 12 patients in which this was performed. Continuous stable distal perfusion was demonstrated in the cannulated limb in 14 of 15 patients. No procedural complications occurred in the immediate or convalescent postoperative period.
Conclusions
This study demonstrates that in patients undergoing femoral arterial cannulation for cardiopulmonary bypass during cardiac surgery, the use of a novel bidirectional cannula is safe and easy to insert and provides stable distal perfusion of the cannulated limb. Use of the device should largely obviate the need to insert a separate downstream perfusion cannula or use other techniques to protect against lower limb ischemia. Further research on a larger scale and in different patient populations is now warranted.
The femoral artery is a common site for peripheral cannulation in patients requiring cardiopulmonary bypass (CPB) for minimally invasive cardiac surgical procedures, redo cardiac surgical procedures, and procedures involving the thoracic aorta.
One of the inherent problems with current femoral artery cannulation techniques for CPB relates to compromised blood flow to the lower limb below the insertion point of the cannula. The diameter of the femoral cannula required to maintain adequate CPB flow is often approaching that of the patient's femoral artery, reducing antegrade perfusion to the lower limb.1,2 This can lead to lower limb ischemic complications unless a strategy to protect the lower limb is implemented.3
Ischemia results in the build-up of anaerobic waste products in the leg, which are subsequently released into the circulation once blood flow is re-established. As such, reperfusion can be associated with hemodynamic instability, decreased cardiac contractility, and changes in pulmonary vasculature resistance. If prolonged, lower limb ischemia will result in irreversible damage to leg structures. These include nerve and muscle damage, with eventual loss of limb function.2,4 Although the incidence of leg ischemia with femoral artery cannulation for CPB in cardiac surgery has not been precisely defined, there are numerous case reports of severe ischemic complications as a result of femoral cannulation, often requiring fasciotomy and sometimes below knee amputation.4–6
These events can be prevented by ensuring adequate oxygen delivery. Traditional methods to maintain distal perfusion after femoral cannulation include the use of a downstream cannula5 or sewing on a side graft.6,7 However, these techniques are cumbersome, time-consuming, and require additional equipment. As a result, current practice involves insertion of a standard femoral cannula into the femoral artery alone, relying on the very small volume of blood that will flow downstream (around the cannula) to keep the leg viable, in addition to any collateral circulation. Although clinicians closely monitor for ischemia in this setting, by the time this is clinically evident, irreversible cell damage may have already occurred.
To overcome this problem, a novel bidirectional femoral arterial cannula has been developed for clinical use (Sorin Group USA, a wholly owned subsidiary of LivaNova PLC, Arvada, CO USA), with specific design features to ensure stable distal perfusion, thereby reducing the risk of lower limb ischemia after femoral cannulation. The aim of this study is therefore to evaluate the safety and efficacy of the bidirectional cannula in patients undergoing femoral arterial cannulation for CPB during cardiac surgery.
METHODS
Study Setting
This phase 1, open-label, noncomparative, single-center, device study of the novel bidirectional cannula was undertaken at The Alfred Hospital, Melbourne, VIC Australia, a quaternary level, university-affiliated cardiothoracic center. The study protocol was compliant with the Australian Therapeutic Goods Administration Clinical Trial Notification Scheme, the International Standards Organization 14155-2011 (Clinical investigation of medical devices for human subjects – Good clinical practice guideline), and the Australian National Health and Medical Research Council (National Statement on Ethical Conduct in Human Research (2007) – Updated May 2015). Ethical approval to undertake the study was provided by the institutional human research ethics committee (Project Number: 14/15). All participants provided written informed consent before any study intervention.
Bidirectional Cannula Design and Insertion Technique
The novel bidirectional cannula (Fig. 1) is similar to a standard cannula except that it is has an angled elbow with a proximal shoulder and a side hole for distal limb perfusion. It is circumferentially tapered to prevent leak during insertion and use. The 120-degree angle at the elbow alleviates the compression of the femoral artery below the insertion point, which commonly contributes to a reduction in downstream flow with currently available femoral cannulae (Fig. 2). The downstream perfusion channel diameter has been calibrated to provide 7% to 10% of cannula flow to the lower limb. In preclinical studies, unobstructed distal flow has been demonstrated in a large animal model.8 Insertion uses a standard needle and guidewire Seldinger technique and is no more time-consuming than regularly employed cannulae. The cannula elbow has a gentle tapered introduction angle that minimizes resistance and arterial trauma on insertion. It has a more significant shoulder angle that provides tactile feedback during positioning of the cannula and prevents accidental dislodgement. The external diameter of the distal section of the 19F bidirectional cannula is 7 mm and the external diameter obliquely at the cannula elbow is 8.4 mm.
FIGURE 1.
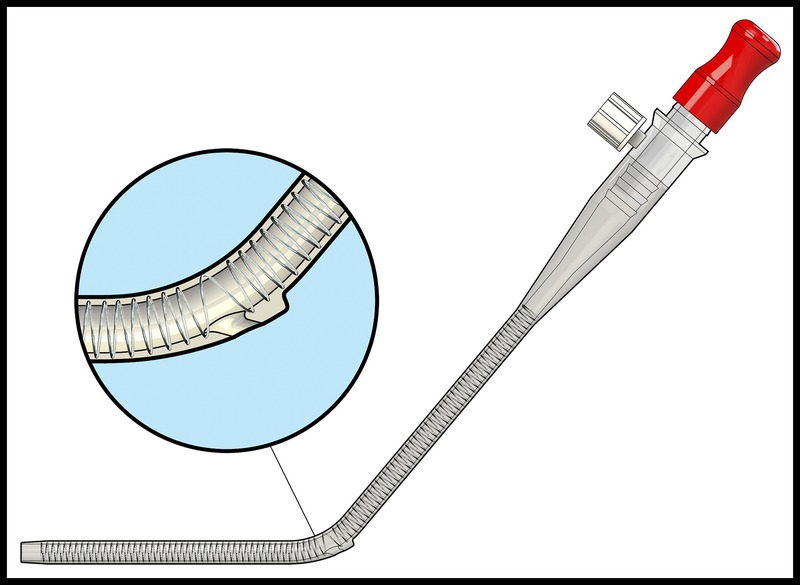
Schematic drawing of the novel bidirectional cannula.
FIGURE 2.
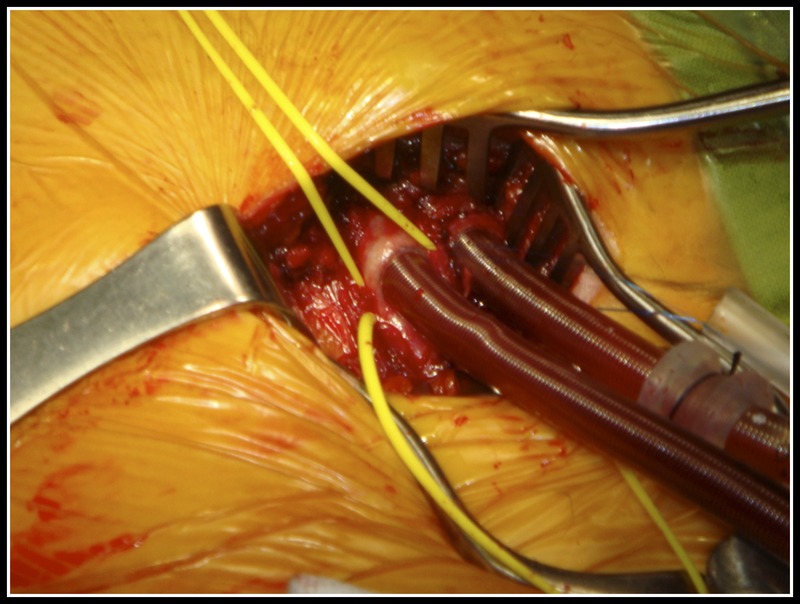
Downstream compression of the distal femoral artery by the body of a standard femoral cannula.
The cannula is inserted into the femoral artery until the elbow passes through the arterial wall. At this stage, a loss of resistance is felt by the operator. The cannula is then gently withdrawn until resistance is felt indicating correct positioning of the elbow and downstream perfusion channel within the artery (Video 1, Supplemental Digital Content 1, http://links.lww.com/INNOV/A172). This feature is important during open insertion, so the operator is confident that the cannula is in the correct position (Video 2, Supplemental Digital Content 2, http://links.lww.com/INNOV/A173). It is even more important during percutaneous insertion, where the clinician cannot directly visualize the artery (Video 3, Supplemental Digital Content 3, http://links.lww.com/INNOV/A174).
The elbow also plays an integral role in overcoming the mechanism of “downstream compression.” The shape of the elbow combined with the self-locating mechanism of the cannula results in the elbow acting as a scaffold, effectively stenting open the downstream artery and creating a channel for blood to flow unobstructed to the lower limb (Fig. 3). The elbow straightens out when the introducer is inserted into the cannula for ease of insertion and returns to its preformed angle when the introducer is removed.
FIGURE 3.
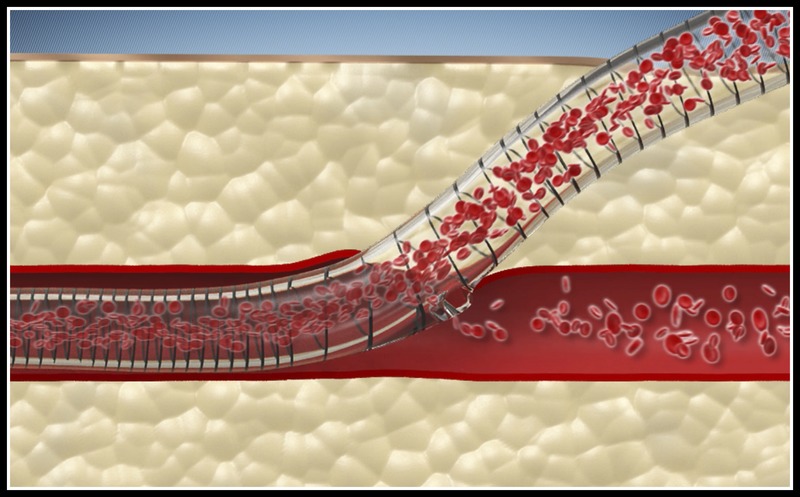
Angled elbow of the bidirectional cannula overcomes downstream compression of the distal femoral artery seen with standard femoral arterial cannulae.
Study Protocol
Patients were screened at preadmission. The following inclusion criteria were applied: 18 years or older and 80 years or younger, cardiac surgery requiring peripheral cannulation for CPB, and weight of greater than 45 kg and less than 130 kg. Patients with the following were then excluded: previous vascular surgery of the femoral artery, emergency cardiac surgery including type A aortic dissections, internal diameter of the common femoral artery less than 7.5 mm, concurrent enrolment in another investigational drug or device study, or use of any experimental or investigational drug or device within 30 days of CPB, any other medical condition, which, in the view of the investigator, would interfere with the study or put the patient at risk, and where the investigator felt adequate flow rates and line pressures would not be achievable with a 19F cannula, because of the patient's weight and body surface area. Where the patient met all of the inclusion and none of the exclusion criteria, they were enrolled, after providing written informed consent.
The study duration consisted of a screening visit within 3 weeks of femoral cannulation for cardiac surgery, the cannulation period, and a follow-up period of at least 30 days (or the first outpatient visit) after removal of the cannula.
Premedication, induction of anesthesia, and insertion of hemodynamic monitoring were all performed as per standard practice. Similarly, the study protocol did not mandate a particular surgical approach nor any aspects of CPB circuit setup. The femoral artery was exposed using a standard approach (where a cut-down procedure was used), and an ultrasound was then performed to measure the internal diameter of the femoral artery. If a percutaneous approach was employed, the ultrasound was performed transcutaneously before need puncture. A single-size (19F) bidirectional cannula was available for the study. If the internal diameter of the femoral artery was found to be less than 7.5 mm, the patient was deemed ineligible and removed from the study. All study operators received familiarization training with the device (using a mechanical training model), before clinical use. Unilateral femoral or central venous cannulation was performed depending on the procedure. Cannulation (including the bidirectional cannula) was performed by the specialist cardiothoracic surgeon performing the surgery in all cases. Cardiopulmonary bypass was established in a standard fashion. The bidirectional cannula was removed once the patient was stable and bypass no longer required. There was a follow-up visit at 24 hours after the cannula was removed where the cannulation site was observed for any complications and again at the first cardiothoracic outpatient visit.
Participant demographics, indication for cardiac surgery, measurement of common femoral artery diameter, and hemodynamic/perfusion parameters were collected prospectively. Lower limb perfusion was assessed using reflectance near-infrared spectroscopy (NIRS; Sensmart, Nonin Medical, Plymouth, MN USA) as a measure of regional oxygen saturation (rSO2). A transducer was applied over the calf muscles on both legs. A drop in oxygen saturation level of more than 20% in the cannulated limb in comparison with baseline triggered a clinical review. Oxygen saturation of both limbs was measured and recorded before cannulation, at the commencement of CPB, and every 15 minutes after cannulation until the cannula was removed. A Doppler ultrasound of the superficial femoral artery (SFA) in the cannulated limb was also performed after commencing CPB. The ultrasound probe was positioned by the operating surgeon and the ultrasound images were interpreted by a cardiothoracic anesthetist with echocardiographic qualifications.
The mean arterial pressure (millimeter of mercury), line pressure (millimeter of mercury), and bypass circuit flow (liter per minute) were measured and recorded every 15 minutes after cannulation until the time the cannula was removed. All adverse events (AEs)/adverse device effects, and serious adverse events (SAEs)/serious adverse device effects were collected.
Sample Size Calculation
As a first-in-human study, no formal sample size calculations were performed. Based on clinical considerations, 15 participants were deemed sufficient to explore the efficacy and safety of the device in this phase 1 study. Patients who provided consent but did not undergo any study intervention were replaced.
Statistical Analysis
Descriptive statistical analyses are reported for all study endpoints. Summary statistics include counts and percentages for categorical variables and the number of participants, mean, standard deviation (SD), median, minimum, and maximum for continuous variables. All performance variables are listed for all patients who met the eligibility criteria and were enrolled in the study.
RESULTS
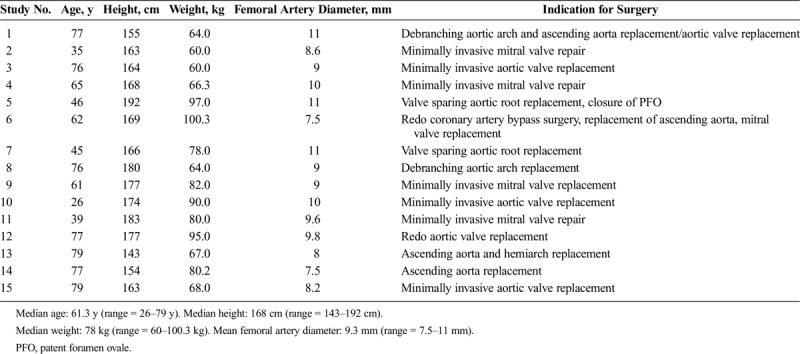
Fifteen patients (median age = 61.3 years, range = 26–79 years) underwent femoral arterial cannulation using the novel bidirectional femoral arterial cannula between August 2016 and May 2017. Indications included minimally invasive mitral and aortic valve surgery, thoracic aortic aneurysm repair, and redo cardiac surgery (Table 1). The mean duration of cannulation was 151.9 minutes (median = 136 minutes, range = 67–298 years). The mean duration of CPB was 129 minutes (median = 123 minutes, range = 53–228 years). The mean internal diameter of the femoral artery as measured on ultrasound was 9.3 mm (median = 9.0 mm, range = 7.5–11 mm) (Table 1). The bidirectional cannula was inserted directly into a surgically exposed femoral artery using a wire through needle technique in 14 patients. In one patient, the cannula was inserted using a percutaneous insertion technique.
TABLE 1.
Patient Characteristics
In 14 of 15 patients, the cannula was inserted and positioned without difficulty. The cannula glided freely with good tactile feedback during positioning of the cannula elbow and downstream perfusion port. In one patient with a 7.5-mm femoral artery, the operator had difficulty inserting the body of the bidirectional cannula into the artery. Subsequently, the bidirectional cannula did not glide in and out freely resulting in incorrect positioning of the cannula elbow and downstream perfusion port. There were no bleeding issues or excess trauma to the vessel during insertion and CPB support in any patient.
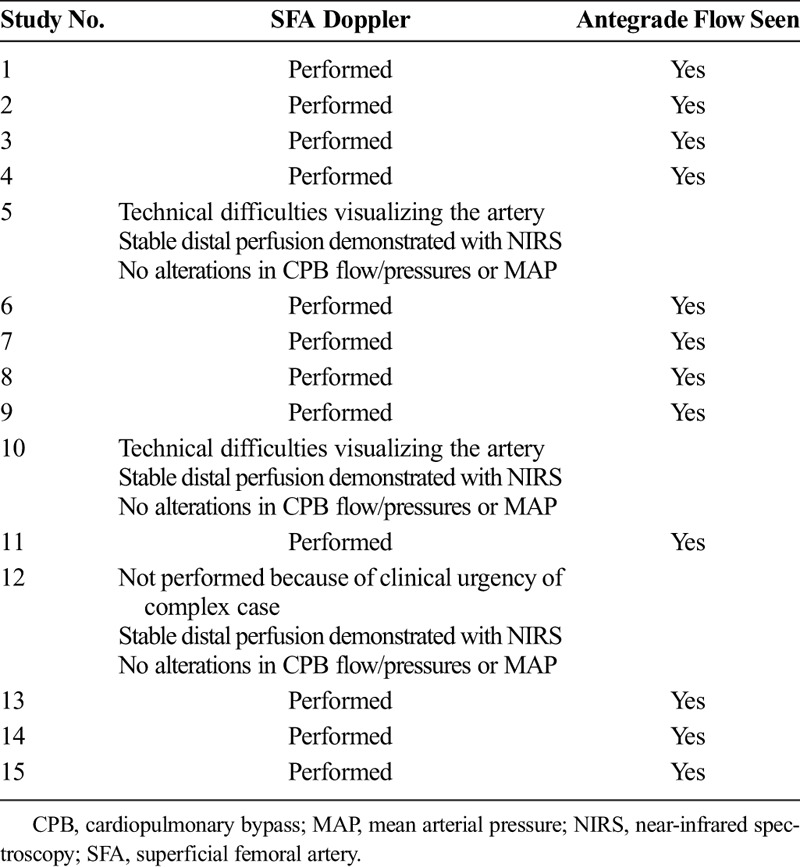
Antegrade flow in the SFA was observed on Doppler ultrasound in 12 of 12 patients in which this was completed. Ultrasound was not attempted or performed in three patients (Table 2). In two patients (participants 5 and 10) where the femoral artery was quite deep and a small skin incision was made, the ultrasound probe was unable to be placed directly on the SFA and the SFA was unable to be visualized when the probe was placed on the skin. The assessments were then abandoned in these cases. In one patient (participant 12), the SFA Doppler was not attempted because of the clinical urgency of the case. In all three patients where a Doppler ultrasound was not attempted or completed, continuous stable lower limb regional oxygen saturation levels were present throughout the period on CPB.
TABLE 2.
Superficial Femoral Artery Doppler Ultrasound Study
Continuous stable distal perfusion was demonstrated using NIRS in the cannulated limb in 14 of 15 patients (Fig. 4). In one patient where the operator had difficulty positioning the cannula because of a size mismatch with the femoral artery, poor distal perfusion was present. At all times, there were satisfactory flows and line pressures through the CPB circuit in this patient. Clinical review prompted repositioning of the cannula; however, despite correct positioning, arterial spasm around the cannula insertion site resulted in reduced lower limb regional oxygen saturation levels. There was no clinical evidence of leg ischemia during the procedure or in the follow-up period for this patient. Regional oximetry dropped to 8% for less than a minute in another participant, indicating altered cannula position after connecting the cannula to the CPB circuit. The operator quickly and easily repositioned the cannula, and oxygen saturation levels immediately returned to precannulation levels.
FIGURE 4.
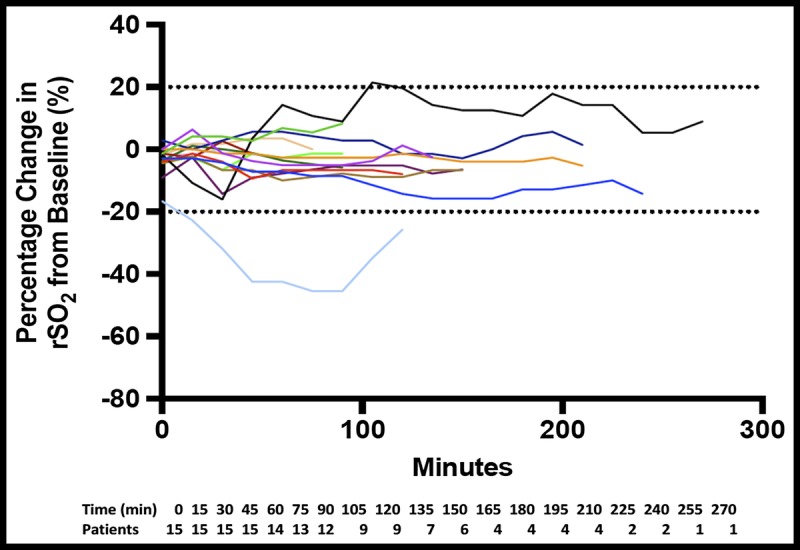
Percentage change in regional oxygen saturation (rSO2). A reduction in rSO2 of more than 20% from baseline is considered to be significant and an indicator of local ischemia.
The lowest mean arterial pressure was 56.8 mm Hg and highest 72.6 mm Hg. Although fluctuations were noted in all patients, these were consistent with clinical interventions undertaken during the procedure (e.g., periods of reduced CPB flow). Overall, in 100% (N = 15) of cases, mean arterial pressure was deemed sufficient to ensure adequate organ perfusion, being representative of adequate flow through the bidirectional cannula. Line pressures were in a satisfactory range for a 19F cannula in all patients throughout the period on CPB. The lowest mean flow was 3.33 L/min and the highest mean flow was 5.34 L/min. Fluctuations were noted over time in each patient, although these were consistent with clinical interventions (e.g., weaning from CPB at the completion of the case). In all patients, flow in the bypass circuit and bidirectional cannula was considered satisfactory.
The cannula was removed without difficulty in all cases, and there were no reported procedural complications. All 15 patients completed the 24-hour follow-up, at which time, there was no evidence of infection, active bleeding, significant hematoma formation (>5 cm diameter), or leg ischemia in any patient.
Thirteen patients (87%) completed their outpatient follow-up visit. Mean time to follow-up in outpatients was 49 days (range = 31–79 days). One patient died before their outpatient visit from an unrelated cause and one patient was reluctant to return for their assessment. This patient had seen his local practitioner, and there was no suggestion of any complications related to the cannulation site. All 13 patients had well-healed vascular access sites. There was no clinical evidence of hematoma, infection, or pseudo-aneurysm formation. One patient reported that subsequent to hospital discharge he had an infection in the femoral incision, which was treated with penicillin by his local doctor. The cannula site was clean and dry on the day of follow-up.
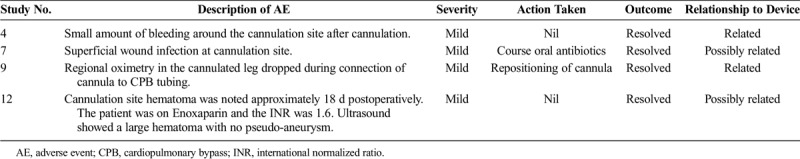
Ten participants (66%) experienced a total of 18 AEs. All were mild in severity. Of the 18 AEs, there were four (22%) that were related or possibly related to the bidirectional cannula. All were mild and required little or no intervention, and all resolved (Table 3).
TABLE 3.
Adverse Events Related to the Bidirectional Cannula
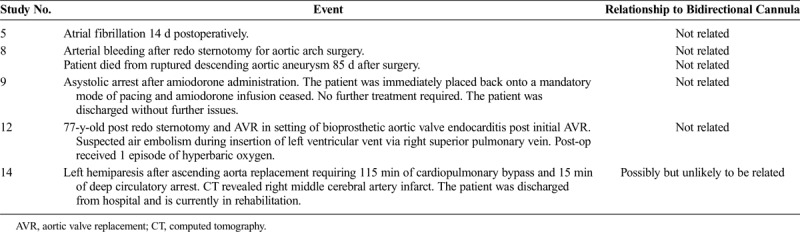
Six SAEs were reported in five participants (Table 4). Five were unrelated to the cannula. One SAE [participant 14; cerebrovascular accident (CVA)] was reported as possibly but highly unlikely to be related to the bidirectional cannula. All events were reported to the human research ethics committee and to the medical monitor, and no further action was considered necessary.
TABLE 4.
Serious Adverse Events
DISCUSSION
Key Findings
Fifteen participants underwent femoral artery cannulation with a 19F bidirectional cannula for CPB during cardiac surgery. All participants were supported on CPB with adequate bypass flows, satisfactory line pressures, and mean arterial pressures that were sufficient to support organ perfusion. Antegrade flow within the SFA was present in all 12 participants where a SFA Doppler study was performed.
Continuous stable distal perfusion of the cannulated limb was demonstrated in more than 90% of participants (n = 14), as evidenced by stable regional oxygen saturation levels recorded every 15 minutes during CPB. In these cases, the bidirectional cannula was inserted and positioned without difficulty. The cannula glided freely within the femoral artery, and there was excellent tactile feedback with positioning of the bidirectional cannula shoulder.
In one patient, difficulties were encountered with inserting the body and shoulder of the bidirectional cannula into the femoral artery. Positioning the cannula was difficult, because the cannula would not glide freely within the artery due to the artery being too small to accommodate a 19F cannula.
No events relating to the safety of the cannula occurred during the study. Specifically, there was no dislodgement of the cannula and no significant bleeding around the insertion point. The cannula was removed without difficulty in all cases, and there were no reported procedural complications.
We found the use of NIRS to be a very sensitive and responsive measure of regional perfusion. Indeed, in one case, the operator was able to respond to a change in oximetry by altering the cannula position, with an immediate improvement in saturation levels. As a result of this incident, the instructions for use were modified to include confirmation of correct cannula shoulder position after connection to CPB tubing and before securing the cannula to the skin.
In one case, the patient experienced a CVA, which was deemed possibly, although unlikely related to the investigational device. In this respect, CVA is a recognized complication of CPB and deep circulatory arrest in cardiothoracic surgery. It can also be related to retrograde aortic perfusion associated with femoral cannulation. This risk is the same with a standard or bidirectional femoral cannula and was not deemed to be a specific device-related AE.
Relationship With Previous Studies
No previous clinical studies have been performed with this device. This work therefore provides first-in-human data with this product, although our study findings (suggesting satisfactory performance) are consistent with preclinical data obtained in a large animal model.8
Other novel femoral arterial cannulae have been investigated previously, principally in large animal models.9–11 Specifically, Matsui et al.11 reported their preliminary experience in both a porcine experimental model and six patients undergoing CPB. Of note, in three patients (50%), distal limb ischemia was still noted after initial insertion, albeit perfusion was improved after cannula repositioning. In comparison, distal perfusion was adequate after cannula insertion in 14 of 15 cases in our study. Cannula repositioning was only required once, after shoulder displacement occurred during connection of the cannula to the CPB circuit.
Study Implications
This data implies that the novel bidirectional cannula can be used safely and effectively in patients requiring femoral arterial cannulation for CPB. This represents a significant advance in peripheral arterial cannulation for extracorporeal cardiorespiratory support and may largely obviate the need to insert a separate downstream perfusion cannula or use other techniques to protect against lower limb ischemia. Importantly, such a complication can have devastating effects on patients, particularly in terms of mobility and quality of life, and this product represents a long-awaited innovation in this field.
Strengths and Weaknesses
This study was a phase 1, open-label, noncomparative, single-center study. As such, selection and performance bias may be present because of the unblinded nature of the study intervention. Similarly, we did not include a control group and therefore do not report contemporary data concerning the magnitude of complications (ischemic or otherwise) using standard cannulation techniques in this patient group. Our sample size was pragmatic, with the primary aim of establishing the initial safety and efficacy of the device in clinical practice. It is acknowledged however that with a larger cohort, a greater number and variety of potential complications may be apparent. It should also be noted that we only assessed one size of bidirectional cannula (19F), in a group of patients with a mean femoral artery diameter of 9.3 mm.
Our use of NIRS to quantify regional oxygenation in the cannulated limb represents a unique strength of the study protocol. Specifically, NIRS has been previously validated as a measure of regional oxygen saturation12 and was highly sensitive to changes in distal perfusion. This method provides a measure of oxygen delivery at the tissue level, which is arguably more informative than simply quantifying macrovascular blood flow. Indeed, by using both NIRS and Doppler ultrasound, we have established that the bidirectional cannula provides satisfactory distal limb perfusion, principally by achieving adequate flow in the SFA, as opposed to any collateral circulation. Finally, we had minimal loss to follow-up, with all patients completing a 24-hour assessment, and 13 being reviewed at least 30 days after surgery.
Future Research
The findings from this phase 1 study require validation in a larger multicenter cohort, involving a greater number of clinical indications, cannula sizes, and operators. In addition, significant additional work is required to assess the feasibility, safety, and efficacy of the device in patients requiring longer-term femoral arterial cannulation, as is the case in venoarterial extracorporeal membrane oxygenation. In this respect, a parallel clinical study using a percutaneous insertion technique in patients requiring venoarterial extracorporeal membrane oxygenation is currently in progress.
CONCLUSIONS
This study demonstrates that in patients undergoing femoral arterial cannulation for CPB during cardiac surgery, the use of a novel bidirectional cannula is safe and easy to insert and provides stable distal perfusion of the cannulated limb. Use of the device should largely obviate the need to insert a separate downstream perfusion cannula or use other techniques to protect against lower limb ischemia. Further research on a larger scale and in different patient populations is now warranted.
Supplementary Material
CLINICAL PERSPECTIVE
Leg ischemia remains a serious and morbid complication of femoral artery cannulation, particularly in patients undergoing prolonged support on cardiopulmonary bypass. This phase-one clinical study examined a novel bidirectional perfusion cannula. Fifteen patients having cardiac surgery underwent femoral cannulation with this cannula. The median duration of cardiopulmonary bypass was 120 minutes. The cannula was inserted and positioned successfully in 14 of 15 patients. Antegrade flow in the superficial femoral artery was observed in 12 of 12 patients in which Doppler ultrasound was performed. Continuous stable distal perfusion as measured by reflectance near-infrared spectroscopy was present in the 14 patients in which this cannula was successfully placed. The cannula was removed without difficulty in all cases. There were no peripheral ischemic complications.
This is encouraging early information. However, this was an open-label, noncomparative, single-center trial and as such could be subject to selection and performance bias.Moreover, the time on cardiopulmonary bypass was relatively short, particularly when compared with the prolonged times that are often seen in patients undergoing venoarterial extracorporeal membrane oxygenation, where peripheral ischemia is more common. Further studies are keenly anticipated, and the group is to be congratulated for this small successful clinical trial.
Footnotes
A video clip is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.innovjournal.com).
Presented at the Annual Scientific Meeting of the International Society for Minimally Invasive Cardiothoracic Surgery, June 7–10, 2017, Rome, Italy.
The study was conducted with support from a Health Market Validation Program Grant from the Victorian State Government, Melbourne, VIC Australia.
Disclosures: Elli Tutungi, FANZCA, and Randall A. Moshinsky, FRACS, have a commercial relationship with LivaNova, London, UK. Silvana F. Marasco, FRACS, Shirley A. Vallance, MClinResMeth, Andrew A. Udy, PhD, Justin C. Negri, FRACS, Adam D. Zimmet, FRACS, David C. McGiffin, FRACS, and Vincent A. Pellegrino, FRACP, declare no conflicts of interest.
REFERENCES
- 1.Foley PJ, Morris RJ, Woo EY, et al. Limb ischemia during femoral cannulation for cardiopulmonary support. . 2010;52:850–853. [DOI] [PubMed] [Google Scholar]
- 2.Bisdas T, Beutel G, Warnecke G, et al. Vascular complications in patients undergoing femoral cannulation for extracorporeal membrane oxygenation support. . 2011;92:626–631. [DOI] [PubMed] [Google Scholar]
- 3.Jaski BE, McClendon PS, Branch KR, et al. Anterograde perfusion in acute limb ischemia secondary to vascular occlusive cardiopulmonary support. . 1995;35:373–376. [DOI] [PubMed] [Google Scholar]
- 4.McGee E, McCarthy PM, Moazami N. Temporary mechanical circulatory support. In Cohn L, ed. Cardiac Surgery in the Adult. New York: McGraw-Hill; 2008:507–534. [Google Scholar]
- 5.Hendrickson SC, Glower DD. A method for perfusion of the leg during cardiopulmonary bypass via femoral cannulation. . 1998;65:1807–1808. [DOI] [PubMed] [Google Scholar]
- 6.Satta J, Rimpilainen J, Rainio P, et al. A feasible femoral cannulation method during cardiopulmonary bypass. . 1998;65:1194–1195. [DOI] [PubMed] [Google Scholar]
- 7.Vander Salm TJ. Prevention of lower extremity ischemia during cardiopulmonary bypass via femoral cannulation. . 1997;63:251–252. [DOI] [PubMed] [Google Scholar]
- 8.Chen Y, Tutungi E, McMillan J, et al. Pressure and flow characteristics of a novel bidirectional cannula for cardiopulmonary bypass. . 2017;12:430–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berdajs D, Ferrari E, Michalis A, et al. New prototype of femoral arterial SmartCannula with anterograde and retrograde flow. . 2011;26:271–275. [DOI] [PubMed] [Google Scholar]
- 10.Magovern JA, Fonger JD, Wang DH, et al. A femoral artery cannula that allows distal blood flow. . 2005;130:684–686. [DOI] [PubMed] [Google Scholar]
- 11.Matsui Y, Shimura S, Suto Y, et al. A novel femoral arterial cannula to prevent limb ischemia during cardiopulmonary support: preliminary report of experimental and clinical experiences. . 2006;30:557–560. [DOI] [PubMed] [Google Scholar]
- 12.MacLeod D, Ikeda K, Vacchiano C, et al. Development and validation of a cerebral oximeter capable of absolute accuracy. . 2012;26:1007–1014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


