Supplemental Digital Content is available in the text.
Keywords: blood pressure; fetal growth restriction; humans; hypertension, pregnancy-induced; preeclampsia; pregnancy outcome
Abstract
For hypertensive women in CHIPS (Control of Hypertension in Pregnancy Study), we assessed whether the maternal benefits of tight control could be achieved, while minimizing any potentially negative effect on fetal growth, by delaying initiation of antihypertensive therapy until later in pregnancy. For the 981 women with nonsevere, chronic or gestational hypertension randomized to less-tight (target diastolic blood pressure, 100 mm Hg), or tight (target, 85 mm Hg) control, we used mixed-effects logistic regression to examine whether the effect of less-tight (versus tight) control on major outcomes was dependent on gestational age at randomization, adjusting for baseline factors as in the primary analysis and including an interaction term between gestational age at randomization and treatment allocation. Gestational age was considered categorically (quartiles) and continuously (linear or quadratic form), and the optimal functional form selected to provide the best fit to the data based on the Akaike information criterion. Randomization before (but not after) 24 weeks to less-tight (versus tight) control was associated with fewer babies with birth weight <10th centile (Pinteraction=0.005), but more preterm birth (Pinteraction=0.043), and no effect on perinatal death or high-level neonatal care >48 hours (Pinteraction=0.354). For the mother, less-tight (versus tight) control was associated with more severe hypertension at all gestational ages but particularly so before 28 weeks (Pinteraction=0.076). In women with nonsevere, chronic, or gestational hypertension, there seems to be no gestational age at which less-tight (versus tight) control is the preferred management strategy to optimize maternal or perinatal outcomes.
Clinical Trial Registration—
URL: https://www.isrctn.com. Unique identifier: ISRCTN71416914.
Hypertension complicates ≤10% of pregnancies worldwide, and it is a leading cause of maternal and perinatal mortality and morbidity, in well and less-resourced settings. Hypertension may be because of chronic hypertension (≈1% of pregnancies), gestational hypertension (≈6%), or preeclampsia (≈3%) that appears de novo or evolves from chronic or gestational hypertension.1 Although preeclampsia is associated with the greatest maternal and perinatal risks, those risks are also elevated in women with chronic or gestational hypertension who are twice as prevalent.
Management of pregnancy hypertension is multifaceted. Although some decisions are dependent on the hypertensive disorder (such as prevention of progression to preeclampsia among women with chronic hypertension or administration of magnesium sulfate to women with eclampsia), decisions about antihypertensive therapy are common to all hypertensive pregnant women. It has been recognized that antihypertensive for nonsevere hypertension decreases the incidence of severe hypertension and additional antihypertensive therapy,2 but the concern has been that this may be achieved at the expense of fetal growth and well-being3,4; the latter meta-analysis of von Dadelszen et al3 showed that a greater antihypertensive-induced fall in mean arterial pressure was associated with a higher proportion of small-for-gestational-age infants, based on 14 trials (slope, 0.09; SD, 0.03; r2, 0.48; P=0.006). However, the absolute decrease in birth weight was 145 g for each 10-mm Hg fall in mean arterial pressure.
The CHIPS (Control of Hypertension in Pregnancy Study; ISRCTN 71416914, http://pre-empt.cfri.ca/CHIPS) compared the effectiveness of less-tight versus tight blood pressure (BP) control in improving pregnancy outcomes among women with nonsevere, nonproteinuric chronic or gestational hypertension at 14 to 33 weeks of pregnancy.5 In the CHIPS trial, 987 women were randomized to less-tight control (n=497; target diastolic BP [dBP] of 100 mm Hg) versus tight control (n=490; target dBP of 85 mm Hg); a planned 15 mm Hg difference in dBP goals aimed to achieve a 5-mm Hg actual difference in dBP, which was the case; mean systolic BP in less-tight control was 138.8±0.5 mm Hg (versus 133.1±0.3 mm Hg in tight), and mean dBP in less-tight control was 89.9±0.3 mm Hg (versus 85.3±0.3 mm Hg in tight). No statistically significant differences were seen in the primary perinatal outcome of perinatal death or high-level neonatal care for >48 hours (155, 31.4% versus 150, 30.7%; adjusted odds ratio [OR], 1.02 [0.77–1.35]; P=0.89) or secondary maternal outcome of serious maternal complications, including death (18, 3.7% versus 10, 2.0%; adjusted OR, 1.74 [0.79–3.84]; P=0.17). However, women in less-tight (versus tight) control more often developed severe maternal hypertension (200, 40.6% versus 134, 27.5%; adjusted OR, 1.80 [1.34–2.38]; P<0.001), platelet count <100×109 per liter (21, 4.3% versus 8, 1.6%; adjusted OR, 2.63 [1.15–6.05]; P=0.02), and elevated liver enzymes with maternal symptoms (21, 4.3% versus 9, 1.8%; adjusted odds ratio, 2.33 [1.05–5.16]; P=0.03). In exploratory analyses, severe hypertension was associated with an excess of adverse perinatal and maternal outcomes, especially in less-tight control and even after adjustment for the co-occurrence of preeclampsia.6
Taken together, the CHIPS results suggest that tight control might be the best clinical option because it minimizes maternal risk without increasing perinatal risk. However, some clinicians are concerned that in tight (versus less tight) control, there may have been an increase in birth weight <10th centile of potential clinical importance (96, 19.7% versus 79, 16.1%, respectively; adjusted OR, 1.28 [0.93–1.79]; P=0.14); the lack of statistical significance may have reflected a lack of statistical power, particularly for women with chronic hypertension.7 However, what has not been highlighted is that in tight (versus less-tight) control, there was also a nonsignificant trend of similar magnitude toward a decrease in preterm birth (153, 31.5% versus 175, 35.6%, respectively; adjusted OR, 0.85 [0.64–1.11]; P=0.18). These surrogate outcomes for adverse perinatal outcome may have balanced each other out to result in the lack of any observed effect of tight (versus less tight) control on the primary perinatal outcome of death or morbidity.
In this secondary, exploratory analysis, we sought to examine the relationship between gestational age at randomization and major CHIPS outcomes (including birth weight <10th centile and preterm birth) to investigate whether the maternal benefits of tight control could be achieved by delaying initiation of antihypertensive therapy until later in pregnancy, to minimize any potential negative impact of that therapy on fetal growth.
Methods
CHIPS was an open, pragmatic, international multicenter trial. Women at 14+0 to 33+6 weeks of gestation with nonproteinuric chronic or gestational hypertension, elevated BP (office dBP, 90–105 or 85–105 mm Hg if on antihypertensives), and a live fetus were randomized (stratified by center and hypertension type) to less-tight (100 mm Hg) or tight control (85 mm Hg) of BP. Importantly, women had to have persistently elevated BP, either on 2 consecutive outpatient visits or for 4 hours at the same visit; so many women with chronic hypertension became eligible only later in pregnancy following the midtrimester nadir.
Data of this secondary analysis will be available on request of the author.
CHIPS was approved by the Research Ethics Boards both centrally at the University of British Columbia as the coordinating center (H08-00882) and locally at all study sites. All participants gave written informed consent. The study was designed following the principles of the Declaration of Helsinki and Guidelines for Good Clinical Practice.
The composite primary outcome was pregnancy loss or high-level neonatal care (greater than normal newborn care) for >48 hours in the first 28 days of life or until primary discharge home, whichever was later. The composite secondary outcome was serious maternal complications before 6 weeks postpartum or until hospital discharge, whichever was later. Serious maternal complications included death, stroke, eclampsia, blindness, uncontrolled hypertension, the use of inotropic agents, pulmonary edema, respiratory failure, myocardial ischemia or infarction, hepatic dysfunction, hepatic hematoma or rupture, renal failure, and transfusion, modeled on Delphi consensus.8 Additional major CHIPS outcomes were severe hypertension and preeclampsia for the mother and birth weight <10th centile and preterm birth for the baby (see Table S2 in the online-only Data Supplement for definitions).
For this secondary analysis, there were 981 women (of 987 randomized) available for analysis. Mixed-effects logistic regression was used to examine the effect, by gestational age at randomization, of less-tight (versus tight) control on major outcomes: primary perinatal outcome, preterm birth, birth weight <10th centile, serious maternal complications, persistent severe maternal hypertension, and preeclampsia. An interaction term between gestational age at randomization and treatment group was included to examine treatment effect as a function of gestational age at randomization. Gestational age was considered categorically in quartiles. Adjustment was made for baseline factors as in the primary CHIPS analysis (ie, stratification factors of hypertension type and center [as a random effect], prior severe hypertension in this pregnancy, in-hospital at enrollment, gestational diabetes mellitus at enrollment, and antihypertensive therapy at enrollment) and those that were different between less-tight and tight control in any gestational age quartile (ie, ethnicity, aspirin at enrollment, perinatal mortality ratio of recruiting country, and systolic BP within 1 week before randomization; Table S3). In a sensitivity analysis, we also considered gestational age at randomization continuously in either linear or quadratic form, and the optimal functional form was selected to provide the best fit to the data based on the Akaike information criterion. We conducted further subgroup analysis by hypertension type (chronic or gestational hypertension). Mixed-effects logistic regression was used for chronic hypertension, and Firth logistic regression without random effects was considered for gestational hypertension because of low outcome counts within a gestational age category or baseline factor level. A P value <0.05 for an interaction term was considered statistically significant. SAS software, version 9.3 (SAS Institute), was used for the statistical analysis.
Results
Of the 981 women in the CHIPS analysis, 493 were in less-tight and 488 in tight control. The results have been previously published.5 In brief, there were 736 (74.6%) women with chronic and 251 (25.4%) with gestational hypertension. At baseline, the less-tight and tight control groups were similar. Baseline BP was ≈140/92 mm Hg, but just <20% had experienced severe hypertension earlier in the index pregnancy. Just over half of women (566; 57.3%) were on antihypertensive therapy, usually (>80%) labetalol or methyldopa in equal measure, regardless of the type of antihypertensive (Table S4). Few women were either smokers or had gestational diabetes mellitus (≈6% each). Importantly, ultrasonographic assessment of gestational age was performed in 907 (91.9%) women (455, 91.5% in less tight and 452, 92.2% in tight).
Post-randomization, in the less-tight (versus tight) group, BP was higher (138.8±0.5/89.9±0.3 versus 133.1±0.5/85.3±0.3 mm Hg; P<0.001), and fewer women took antihypertensive therapy (362, 73.4% versus 452, 92.6%; P<0.001), usually 1 drug (209, 57.7% versus 281, 62.2%) and usually labetalol (242, 66.9% versus 304, 67.3%), methyldopa (154, 42.5% versus 182, 40.3%), or nifedipine (115, 31.8% versus 136, 30.1%; Appendix in the online-only Data Supplement5).
Perinatal Outcomes
The effect of less-tight (versus tight) control on the primary perinatal outcome did not differ between the treatment groups randomized at different gestational ages (Pinteraction=0.724; adjusted OR, 1.01 [0.75–1.34]; Table 1). There was, however, a significant interaction between treatment group and gestational age for birth weight <10th centile (Pinteraction=0.028) and a trend toward more preterm birth; however, no significant effect was seen (Pinteraction=0.061). Less-tight (versus tight) control was associated with fewer babies with birth weight <10th centile at <18 weeks (ORadjusted, 0.30 [0.14–0.65]) with a similar, nonsignificant effect seen at 18 to 23 weeks (ORadjusted, 0.63 [0.30–1.34]) but no obvious effect at 24 to 29 or 30+ weeks. Less-tight (versus tight) control was associated with a nonsignificant increase in preterm birth at <18 weeks (ORadjusted, 1.72 [0.91–3.27]) and at 18 to 23 weeks (ORadjusted, 1.73 [0.95–3.15]), with no significant effect from 24 weeks. A similar pattern was seen for delivery at <34 weeks, but the results did not reach statistical significance (Pinteraction=0.567; Table 1 overall; Table S5 for chronic and gestational hypertension subgroups).
Table 1.
Major CHIPS PERINATAL Outcomes in Less-Tight (vs Tight) Control Groups, According to Gestational Age at Randomization (n, Percentage of Women)*†
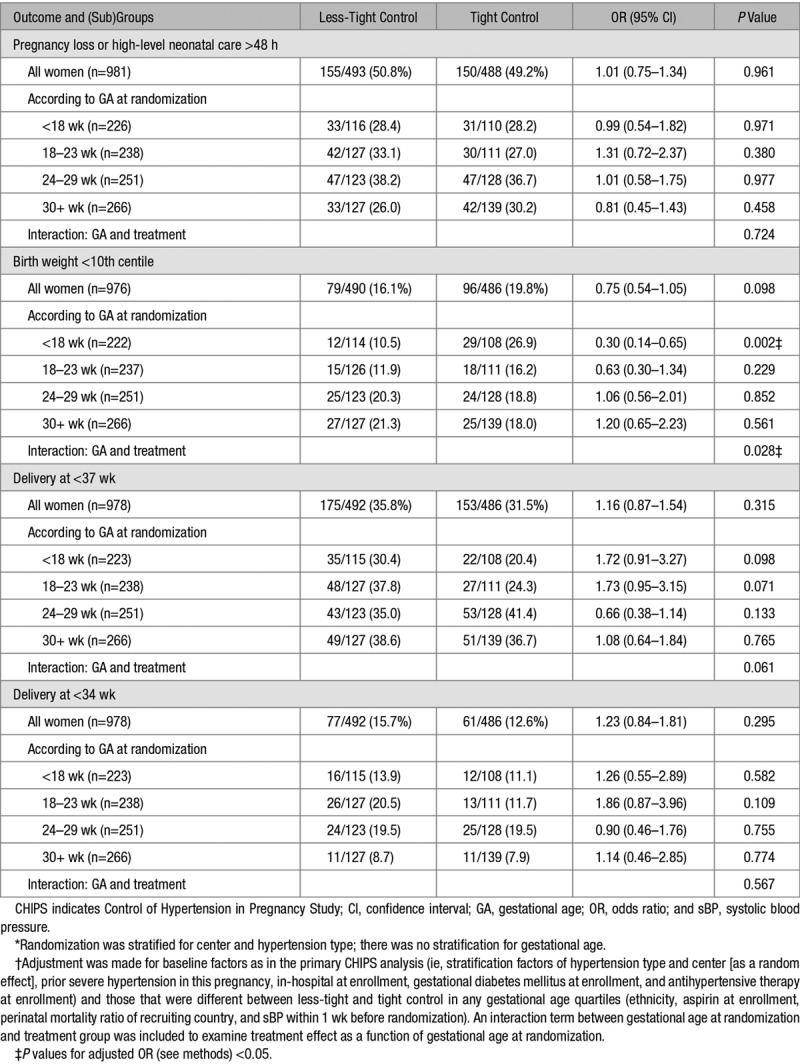
These effects are demonstrated graphically in Figure 1 in which gestational age was treated as a continuous variable; the effects were similar in that less tight (versus tight) at <24 weeks was associated with both a decrease in birth weight <10th centile (small for gestational age; Pinteraction=0.005) and an increase in preterm birth at <37 weeks (Pinteraction=0.043), with no effect on the primary outcome (Pinteraction=0.354).
Figure 1.

Odds ratio and 95% confidence intervals for major CHIPS (Control of Hypertension in Pregnancy Study) PERINATAL outcomes in less-tight (LT; vs tight [T]) control groups, according to gestational age at randomization (wk). Small for gestational age (SGA) defined as birth weight <10th centile. The P value shown is for the interaction between treatment group and gestational age at randomization treated as a continuous variable on the relevant outcome.
In CHIPS, 213 women delivered spontaneously (21.7%; 109 in less tight and 104 in tight), 442 were induced (45.1%; 224 in less tight and 218 in tight), and 323 had a caesarean before labor (32.9%; 159 in less tight and 164 in tight).5 The relationship between less-tight (versus tight) control at <24 weeks and an increase in preterm birth was restricted to an effect on iatrogenic (ie, induced or elective delivery; Pinteraction=0.063) and not spontaneous preterm birth (Pinteraction=0.329; Figure S1). The reasons for iatrogenic preterm birth were not systematically reported in CHIPS.
In subgroup analyses, the overall relationship between initiation of less-tight (versus tight) control at <24 weeks and perinatal outcomes was demonstrable only among women with chronic, but not gestational, hypertension, whether gestational age was analyzed by quartile (Table S5) or continuously (Figures S2 and S3).
Maternal Outcomes
There was no demonstrable interaction between gestational age at initiation of less-tight versus tight control and serious maternal complications when gestational age was considered categorically (Table 2). However, when gestational age was considered as a continuous variable, later initiation (beyond 24 weeks) of less-tight (versus tight) control seemed to be associated with an increase in serious maternal complications (Figure 2; Pinteraction=0.205); this finding appeared to be related to findings within women with gestational hypertension (Figure S3; Table 2 overall; Table S5 chronic and gestational hypertension subgroups).
Table 2.
Major CHIPS MATERNAL Outcomes in Less-Tight (vs Tight) Control Groups, According to Gestational Age at Randomization (n, Percentage of Women)*†

Figure 2.
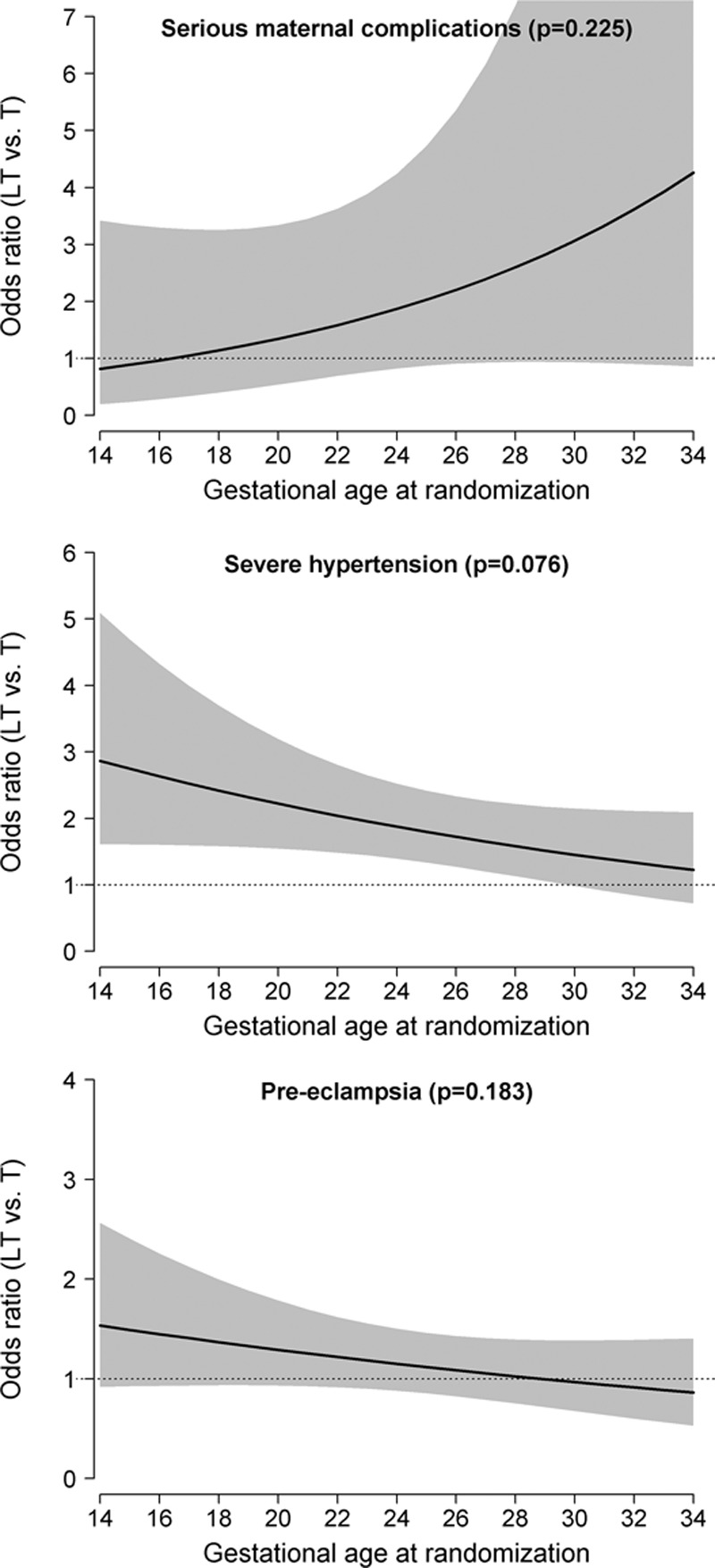
Odds ratio and 95% confidence intervals for major CHIPS (Control of Hypertension in Pregnancy Study) MATERNAL outcomes in less-tight (LT; vs tight [T]) control groups, according to gestational age at randomization (wk). The P value shown is for the interaction between treatment group and gestational age at randomization treated as a continuous variable on the relevant outcome.
Women in less-tight (versus tight) control had more severe hypertension overall (ORadjusted, 1.82 [1.36–2.44]) and in particular, at <18 weeks (ORadjusted, 2.49 [1.34–4.63]) and 18 to 23 weeks (ORadjusted, 2.43 [1.30–4.55]), with a nonsignificant interaction demonstrated with gestational age (Pinteraction=0.336; Table 2). However, in sensitivity analyses with gestational age as a continuous variable (Figure 2), initiation of less-tight (versus tight) control before 28 weeks seemed to be associated with more severe hypertension (Pinteraction=0.076). A similar nonsignificant trend toward early initiation of less-tight (versus tight) control being associated with more preeclampsia was seen whether gestational age was considered categorically (Pinteraction=0.621; Table 2) or continuous (Pinteraction=0.183; Figure 2). In subgroup analyses, the relationship described between gestational age at initiation of less-tight (versus tight) control and severe hypertension or preeclampsia seemed to be similar among women with chronic or gestational hypertension (Table S5; Figure S3).
Discussion
Main Findings
In this secondary, exploratory analysis of the CHIPS trial of less-tight (versus tight) control of nonsevere pregnancy hypertension, significant differences in outcomes were found according to the gestational age at randomization. At no gestational age at which randomization to treatment occurred were overall outcomes better if a strategy of less-tight (versus tight) BP control was pursued. This finding held true when considering women overall or for those with either chronic or gestational hypertension.
Less-tight (versus tight) control commenced before 24 weeks was associated with fewer babies born with birth weight <10th centile but more babies born at <37 weeks; importantly, there was no overall effect on the primary outcome of pregnancy loss or high-level neonatal care for >48 hours. In the subgroups by type of hypertension, the findings were apparent only among women with chronic (not gestational) hypertension, among which there was no gestational age interaction; of note, by definition, women with gestational hypertension could be diagnosed only from 20 weeks.
For the mother, less-tight (versus tight) control was associated with more severe maternal hypertension at all gestational ages (as reported in the main trial publication), but this was particularly so when women were randomized before 28 weeks; a nonsignificant similar trend was seen in preeclampsia, and the effects were not obviously different by type of hypertension. Also, less-tight (versus tight) control seemed to be associated with more serious maternal complications after 28 weeks and particularly among women with gestational hypertension.
Current Literature
Both small for gestational age and preterm birth are surrogates for adverse perinatal outcome.9–14 As each increases risk of perinatal mortality and morbidity, each is used commonly as a primary or secondary outcome in randomized trials, and in particular, those in pregnancy hypertension.
It has long been debated in the obstetric literature whether antihypertensive therapy in pregnancy may impair uteroplacental perfusion and through this, fetal growth and well-being. Although this concern has not been clearly documented in traditional meta-analysis of randomized trials (49 trials, 4723 women),2 meta-regression analysis of 34 trials has suggested that lowering maternal BP (as in tight control in CHIPS) is associated with lower birth weight.3,15 Some studies published after this meta-regression analysis confirmed this hypothesis,4,16,17 whereas others challenged it2; none were able to account fully for associated maternal comorbidity or target BP. In addition, observational literature has suggested that initiation of antihypertensive therapy early in pregnancy may be a particular concern with regard to a negative impact on fetal growth.18 No demonstrable effects have been seen on preterm birth.
Although our secondary analysis of CHIPS data support these concerns and show that minimizing antihypertensive therapy through less-tight control before 24 weeks (through less-tight [versus tight] control) may have a favorable effect on fetal growth, what we have demonstrated for the first time is how a contrasting effect on preterm birth results in no impact on perinatal mortality and morbidity—the hard clinical outcomes that are the focus of our concern.
Strengths and Limitations
Strengths of this study relate mainly to the quality of the trial data set on which the analyses were based, including its large size and international nature, which improves generalizability. Gestational age at randomization was ascertained accurately at randomization and there was a balance between groups, including type of pregnancy hypertension (as a risk factor for fetal growth restriction) and use (and nature) of antihypertensive therapy for which the analyses were adjusted.
First, our analysis had limited statistical power to examine the relationship between gestational age and outcome because as with all trials, the sample size was based on achieving a difference between groups in the primary outcome. Power was improved by considering gestational age as a continuous variable, in addition to categorical. Also, power was particularly limited in analyses of women with gestational hypertension who made up 25.4% of the study population and by definition were not randomized before 20 weeks. Second, we used earlier gestational age at initiation of less-tight (versus tight) control as an unbiased (prerandomization) proxy for duration of therapy—a postrandomization characteristic. Third, our results are relevant to less-tight (versus tight) control as applied in the CHIPS trial, although the antihypertensive agents used most commonly (ie, primarily labetalol and methyldopa, and to a lesser extent, nifedipine) are those used most commonly internationally.
Perspectives
In summary, this secondary exploratory analysis of CHIPS data has shown that there is no gestational age at which less-tight (versus tight) control is the preferred clinical option, for women with chronic or gestational hypertension. Although this secondary analysis of the CHIPS trial data confirmed the hypothesis that initiating less-tight (versus tight) control at <24 weeks is associated with fewer babies with birth weight <10th centile, an effect that was counterbalanced by an increase in iatrogenic preterm birth such that there was no overall effect on perinatal death or morbidity. In addition, such early initiation of less-tight (versus tight) control was associated with a particular increase in the risk of severe hypertension. Initiation of less-tight (versus tight) control after 28 weeks may increase serious maternal complications, particularly among women with gestational hypertension. Future work should address clinicians’ views about timing of delivery among women with higher BP and in particular, severe hypertension.
Acknowledgments
We sincerely thank all of the women who gave of themselves by participating in CHIPS (Control of Hypertension in Pregnancy Study). We continue to dedicate our analyses to Dr Andree Gruslin, our friend, and colleague.
Sources of Funding
CHIPS was funded by the Canadian Institutes of Health Research (MCT 87522).
Disclosures
None.
Supplementary Material
Appendix
The CHIPS Study Group
Laura A. Magee, Elizabeth Asztalos, Amiram Gafni, Andrée Gruslin, Michael Helewa, Eileen Hutton, Shoo Lee, Alexander Logan, Jennifer Menzies, Jean-Marie Moutquin, Kellie Murphy, Evelyne Rey, Sue Ross, Johanna Sanchez, Joel Singer, Peter von Dadelszen, Wessel Ganzevoort, Jim G. Thornton, Ross Welch, Trinh Hoac, Joanne Kirton, Katherine Trigiani, Ainy Zahid, Michael B. Bracken, Patricia Crowley, Lelia Duley, Richard Ehrenkranz, Kevin Thorpe, Sunny Chan, Michael Shi, Shelley Yu, Raquel de Lourdes Martin, Maria Florencia Bassi, Mirta Clara Caruso, Valeria Lagunas, Fernando Vera, Maria Mohedano de Duhalde, Alicia Beatriz Roque, Patricia Roldan, Esteban Marcos Duhalde, Viviana Dip, Jesus Daniel Aguirre, Elba Mirta Alicia Morales, Griselda Itati Abreo, Teresa De Sagastizabal, Carolina Gomez, Nadia Rizzi, Carlos Arias, Ricardo Antonio Bruno, Kassam Mahomed, Alison Drew, Ann Green, Jane Hoare, Bill Hague, Suzette Coat, Caroline Crowther, Peter Muller, Sophie Trenowden, Barry Walters, Claire Parker, Dorothy Graham, Craig Pennell, Eileen Sung, Angela Makris, Gaksoo Lee, Charlene Thornton, Annemarie Hennessy, Louise Farrell, Nelson Sass, Henri Korkes, Dayana Couto Ferreira, Renato Augusto Moreira de Sa, Monique Schmidt Marques Abreu, Rita Guerios Bornia, Nancy Ribeiro da Silva, Fernanda Freitas Oliveira Cardoso, Caio Coelho Marques, Jorge Hornos, Ricardo Leal Davdt, Letícia Germany Paula, Pedro Luis Zanella, Gabrielle Inglis, Ruth Dillon, Ashley Docherty, Anna Hutfield, Keith Still, Sayrin Lalji, Tamara Van Tent, Chris Hotz, Tracy Messmer, Joel G. Ray, Howard Berger, Leanne De Souza, Andrea Lausman, Tatiana Freire-Lizama, Kate Besel, Paul Gibson, Greta Ellsworth, Leslie Miller, T. Lee-Ann Hawkins, Michelle Hladunewich, Anna Rogowsky, Dini Hui, Virginia Collins, Isabelle Delisle, Cora Fanning, Nestor Demianczuk, Rshmi Khurana, Winnie Sia, Catherine Marnoch, Carmen Young, Cheryl Lux, Sophie Perreault, Valerie Tremblay, Sophie Desindes, Anne-Marie Côté, Veronique Dagenais, Heather Clark, Elaine O’Shea, Ruth Rennicks White, Shital Gandhi, Mary-Jean Martin, Cheryl Brush, Gareth Seaward, Jill Newstead-Angel, Judy Brandt, Jocelyne Martel, Kristine Mytopher, Elise Buschau, Erin Keely, Patti Waddell, Svetlana Shachkina, Alan Karovitch, Robert Anderson, Nicole Koenig, Theresa Yong, Marie Vasiliou, Peri Johnson, Beth Allan, Renato Natale, Laura Kennedy, Lucie Opatrny, Lorraine Lavigne, George Carson, Sheila Kelly, Joan Crane, Donna Hutchens, Juan Pedro Kusanovic, Christian Figueroa, Karla Silva Neculman, Juan Andres Ortiz, Paula Vargas, Pedro Ferrand, Jorge Carrillo, Rodrigo Cifuentes Borrero, Dahiana Marcela Gallo, Luisa Fernanda Moreno, Fred Kirss, Kristiina Rull, Anne Kirss, Tamas Major, Andrea Fodor, Tunde Bartha, Mordechai Hallak, Nardin Aslih, Saja Anabousi-Murra, Ester Pri-Or, Linda Harel, Sima Siev, Marwan Hakim, Christina Simona Khoury, Najla Hamati, Mazen El-Zibdeh, Lama Yousef, Ruth Hughes, Di Leishman, Barbra Pullar, Matthew Farrant, Malgorzata Swiatkowska-Freund, Krzysztof Preis, Anette Aleksandra Traczyk-Los, Anna Partyka, Joanna Preis-Orlikowska, Mariusz Lukaszuk, Grzegorz Krasomski, Michael Krekora, Anna Kedzierska-Markowicz, Katarzyna Zych-Krekora, Grzegorz H. Breborowicz, Anna Dera-Szymanowska, Jannet Bakker, Joost Akkermans, Anouk Pels, Eline van den Akker, Sabine Logtenberg, Steven Koenen, Maartje de Reus, David Borman, Martijn A. Oudijk, Annemiek Bolte, Viki Verfaille, Bart Graaf, Martina Porath, Corine Verhoeven, Ben Willem J. Mol, Maureen T.M. Franssen, Lida Ulkeman, Ineke Hamming, Jose H.M. Keurentjes, Ina van der Wal, S.W.A. Nij Bijvank, A.A. Lutjes, Henricus Visser, Hubertina Catharina Johanna Scheepers, Erik van Beek, Coby van Dam, Kathy van den Berg-Swart, Paula Pernet, Birgit van der Goes, Nico Schuitemaker, Gunilla Kleiverda, Marcel van Alphen, Ageeth Rosman, Ingrid Gaugler-Senden, Marieke Linders, Catherine Nelson-Piercy, Annette Briley, May Ching Soh, Kate Harding, Hayley Tarft, David Churchill, Katherine Cheshire, Julia Icke, Mausumi Ghosh, James Thornton, Yvonne Toomassi, Karen Barker, Joanne Fisher, Nicky Grace, Amanda Green, Joanne Gower, Anna Molnar, Shobhana Parameshwaran, Andrew Simm, George Bugg, Yvette Davis, Ruta Desphande, Yvette Gunn, Mohammed Houda, Nia Jones, Jason Waugh, Carly Allan, Gareth Waring, Steve A. Walkinshaw, Angela Pascall, Mark Clement-Jones, Michelle Dower, Gillian Houghton, Heather Longworth, Tej Purewal, Derek Tuffnell, Diane Farrar, Jennifer Syson, Gillian Butterfield, Vicky Jones, Rebecca Palethorpe, Tracey Germaine, Marwan Habiba, Debbie Lee, Olufemi Eniola, Lynne Blake, Jane Khan, Helen M. Cameron, Kim Hinshaw, Amanda Bargh, Eileen Walton, Olanrewaju Sorinola, Anna Guy, Zoe D’Souza, Rhiannon Gabriel, Jo Williams, Heidi Hollands, Olujimi Jibodu, Sara Collier, Pauline Tottie, Claire Oxby, James Dwyer, Franz Majoko, Helen Goldring, Sharon Jones, Janet Cresswell, Louise Underwood, Mary Kelly-Baxter, Rebecca Robinson, Dilly Anumba, Anne Chamberlain, Clare Pye, Clare Tower, Sue Woods, Lisa Horrocks, Fiona Prichard, Lynsey Moorhead, Sarah Lee, Louise Stephens, Cara Taylor, Suzanne Thomas, Melissa Whitworth, Jenny Myers, Ellen Knox, Katie Freitas, Mark Kilby, Amanda Cotterill, Khalil Abdo, Katrina Rigby, Julie Butler, Fiona Crosfill, Sean Hughes, Sanjeev Prashar, Fatimah Soydemir, Janet Ashworth, Lorraine Mycock, Jill Smith, Amaju Ikomi, Kerry Goodsell, Jean Byrne, Maxwell Masuku, Alice Pilcher, Meena Khandelwal, Gunda Simpkins, Michelle Iavicoli, Yon Sook Kim, Richard Fischer, Robin Perry, Eugene Y. Chang, Tamara D. Saunders, Betty W. Oswald, Kristin D. Zaks, Sarosh Rana, Dawn McCullough, Anna Sfakianaki, Cheryl Danton, Erin Kustan, Luisa Coraluzzi, Helen How, Christina Waldon, Jeffrey Livingston, Sherry Jackson, Lisa Greene, Dinesh Shah, Jorge E. Tolosa, Monica Rincon, Leonardo Pereira, Amy E. Lawrence, Janice E. Snyder, D. Michael Armstrong, Teresa Blue, Austin Hester, Kathryn Salisbury.
Footnotes
A list of all CHIPS Study Group members is given in the Appendix and in Table S1 in the online-only Data Supplement.
The online-only Data Supplement is available with this article at http://hyper.ahajournals.org/lookup/suppl/doi:10.1161/HYPERTENSIONAHA.117.10689/-/DC1.
Contributor Information
Collaborators: Amiram Gafni, Andrée Gruslin, Michael Helewa, Eileen Hutton, Shoo Lee, Alexander Logan, Jennifer Menzies, Jean-Marie Moutquin, Kellie Murphy, Evelyne Rey, Sue Ross, Johanna Sanchez, Jim G. Thornton, Ross Welch, Trinh Hoac, Joanne Kirton, Katherine Trigiani, Ainy Zahid, Michael B. Bracken, Patricia Crowley, Lelia Duley, Richard Ehrenkranz, Kevin Thorpe, Sunny Chan, Michael Shi, Shelley Yu, Raquel de Lourdes Martin, Maria Florencia Bassi, Mirta Clara Caruso, Valeria Lagunas, Fernando Vera, Maria Mohedano de Duhalde, Alicia Beatriz Roque, Patricia Roldan, Esteban Marcos Duhalde, Viviana Dip, Jesus Daniel Aguirre, Elba Mirta Alicia Morales, Griselda Itati Abreo, Teresa De Sagastizabal, Carolina Gomez, Nadia Rizzi, Carlos Arias, Ricardo Antonio Bruno, Kassam Mahomed, Alison Drew, Ann Green, Jane Hoare, Bill Hague, Suzette Coat, Caroline Crowther, Peter Muller, Sophie Trenowden, Barry Walters, Claire Parker, Dorothy Graham, Craig Pennell, Eileen Sung, Angela Makris, Gaksoo Lee, Charlene Thornton, Annemarie Hennessy, Louise Farrell, Nelson Sass, Henri Korkes, Dayana Couto Ferreira, Renato Augusto Moreira de Sa, Monique Schmidt Marques Abreu, Rita Guerios Bornia, Nancy Ribeiro da Silva, Fernanda Freitas Oliveira Cardoso, Caio Coelho Marques, Jorge Hornos, Ricardo Leal Davdt, Letícia Germany Paula, Pedro Luis Zanella, Gabrielle Inglis, Ruth Dillon, Ashley Docherty, Anna Hutfield, Keith Still, Sayrin Lalji, Tamara Van Tent, Chris Hotz, Tracy Messmer, Joel G. Ray, Howard Berger, Leanne De Souza, Andrea Lausman, Tatiana Freire-Lizama, Kate Besel, Paul Gibson, Greta Ellsworth, Leslie Miller, T. Lee-Ann Hawkins, Michelle Hladunewich, Anna Rogowsky, Dini Hui, Virginia Collins, Isabelle Delisle, Cora Fanning, Nestor Demianczuk, Rshmi Khurana, Winnie Sia, Catherine Marnoch, Carmen Young, Cheryl Lux, Sophie Perreault, Valerie Tremblay, Sophie Desindes, Anne-Marie Côté, Veronique Dagenais, Heather Clark, Elaine O’Shea, Ruth Rennicks White, Shital Gandhi, Mary-Jean Martin, Cheryl Brush, Gareth Seaward, Jill Newstead-Angel, Judy Brandt, Jocelyne Martel, Kristine Mytopher, Elise Buschau, Erin Keely, Patti Waddell, Svetlana Shachkina, Alan Karovitch, Robert Anderson, Nicole Koenig, Theresa Yong, Marie Vasiliou, Peri Johnson, Beth Allan, Renato Natale, Laura Kennedy, Lucie Opatrny, Lorraine Lavigne, George Carson, Sheila Kelly, Joan Crane, Donna Hutchens, Juan Pedro Kusanovic, Christian Figueroa, Karla Silva Neculman, Juan Andres Ortiz, Paula Vargas, Pedro Ferrand, Jorge Carrillo, Rodrigo Cifuentes Borrero, Dahiana Marcela Gallo, Luisa Fernanda Moreno, Fred Kirss, Kristiina Rull, Anne Kirss, Tamas Major, Andrea Fodor, Tunde Bartha, Mordechai Hallak, Nardin Aslih, Saja Anabousi-Murra, Ester Pri-Or, Linda Harel, Sima Siev, Marwan Hakim, Christina Simona Khoury, Najla Hamati, Mazen El-Zibdeh, Lama Yousef, Ruth Hughes, Di Leishman, Barbra Pullar, Matthew Farrant, Malgorzata Swiatkowska-Freund, Krzysztof Preis, Anette Aleksandra Traczyk-Los, Anna Partyka, Joanna Preis-Orlikowska, Mariusz Lukaszuk, Grzegorz Krasomski, Michael Krekora, Anna Kedzierska-Markowicz, Katarzyna Zych-Krekora, Grzegorz H. Breborowicz, Anna Dera-Szymanowska, Jannet Bakker, Joost Akkermans, Eline van den Akker, Sabine Logtenberg, Steven Koenen, Maartje de Reus, David Borman, Martijn A. Oudijk, Annemiek Bolte, Viki Verfaille, Bart Graaf, Martina Porath, Corine Verhoeven, Maureen T.M. Franssen, Lida Ulkeman, Ineke Hamming, Jose H.M. Keurentjes, Ina van der Wal, S.W.A. Nij Bijvank, A.A. Lutjes, Henricus Visser, Hubertina Catharina Johanna Scheepers, Erik van Beek, Coby van Dam, Kathy van den Berg-Swart, Paula Pernet, Birgit van der Goes, Nico Schuitemaker, Gunilla Kleiverda, Marcel van Alphen, Ageeth Rosman, Ingrid Gaugler-Senden, Marieke Linders, Catherine Nelson-Piercy, Annette Briley, May Ching Soh, Kate Harding, Hayley Tarft, David Churchill, Katherine Cheshire, Julia Icke, Mausumi Ghosh, James Thornton, Yvonne Toomassi, Karen Barker, Joanne Fisher, Nicky Grace, Amanda Green, Joanne Gower, Anna Molnar, Shobhana Parameshwaran, Andrew Simm, George Bugg, Yvette Davis, Ruta Desphande, Yvette Gunn, Mohammed Houda, Nia Jones, Jason Waugh, Carly Allan, Gareth Waring, Steve A. Walkinshaw, Angela Pascall, Mark Clement-Jones, Michelle Dower, Gillian Houghton, Heather Longworth, Tej Purewal, Derek Tuffnell, Diane Farrar, Jennifer Syson, Gillian Butterfield, Vicky Jones, Rebecca Palethorpe, Tracey Germaine, Marwan Habiba, Debbie Lee, Olufemi Eniola, Lynne Blake, Jane Khan, Helen M. Cameron, Kim Hinshaw, Amanda Bargh, Eileen Walton, Olanrewaju Sorinola, Anna Guy, Zoe D’Souza, Rhiannon Gabriel, Jo Williams, Heidi Hollands, Olujimi Jibodu, Sara Collier, Pauline Tottie, Claire Oxby, James Dwyer, Franz Majoko, Helen Goldring, Sharon Jones, Janet Cresswell, Louise Underwood, Mary Kelly-Baxter, Rebecca Robinson, Dilly Anumba, Anne Chamberlain, Clare Pye, Clare Tower, Sue Woods, Lisa Horrocks, Fiona Prichard, Lynsey Moorhead, Sarah Lee, Louise Stephens, Cara Taylor, Suzanne Thomas, Melissa Whitworth, Jenny Myers, Ellen Knox, Katie Freitas, Mark Kilby, Amanda Cotterill, Khalil Abdo, Katrina Rigby, Julie Butler, Fiona Crosfill, Sean Hughes, Sanjeev Prashar, Fatimah Soydemir, Janet Ashworth, Lorraine Mycock, Jill Smith, Amaju Ikomi, Kerry Goodsell, Jean Byrne, Maxwell Masuku, Alice Pilcher, Meena Khandelwal, Gunda Simpkins, Michelle Iavicoli, Yon Sook Kim, Richard Fischer, Robin Perry, Eugene Y. Chang, Tamara D. Saunders, Betty W. Oswald, Kristin D. Zaks, Sarosh Rana, Dawn McCullough, Anna Sfakianaki, Cheryl Danton, Erin Kustan, Luisa Coraluzzi, Helen How, Christina Waldon, Jeffrey Livingston, Sherry Jackson, Lisa Greene, Dinesh Shah, Jorge E. Tolosa, Monica Rincon, Leonardo Pereira, Amy E. Lawrence, Janice E. Snyder, D. Michael Armstrong, Teresa Blue, Austin Hester, and Kathryn Salisbury
Novelty and Significance
What Is New?
An association was found between initiation of less-tight (versus tight) maternal blood pressure control with antihypertensive therapy before 24 weeks of pregnancy and both fewer small-for-gestational-age babies and more iatrogenic preterm birth, such that there was no overall effect on death or morbidity for babies.
Also, we found that although less-tight (versus tight) maternal blood pressure control was associated with more-severe hypertension throughout pregnancy, the excess risk was particularly marked when less-tight control was initiated before 24 weeks.
What Is Relevant?
There is no gestational age at which commencement of less-tight (versus tight) control is the preferred strategy for mother or baby. Any potential gains in fetal growth are balanced by earlier delivery such that perinatal mortality and morbidity are unchanged. However, less-tight (versus tight) control increases maternal risk.
Summary
This secondary analysis of CHIPS (Control of Hypertension in Pregnancy Study) data reinforces the message that at no point in pregnancy is less-tight blood pressure control the preferred clinical strategy over tight control, from maternal or perinatal perspectives.
References
- 1.Magee LA, von Dadelszen P, Stones W. The FIGO Textbook of Pregnancy Hypertension–An Evidence-Based Guide to Monitoring, Prevention and Management. London, UK: The Global Library of Women’s Medicine 2016; http://www.glowm.com. [Google Scholar]
- 2.Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2014:CD002252. doi: 10.1002/14651858.CD002252.pub3. [DOI] [PubMed] [Google Scholar]
- 3.von Dadelszen P, Ornstein MP, Bull SB, Logan AG, Koren G, Magee LA. Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis. Lancet. 2000;355:87–92. doi: 10.1016/s0140-6736(98)08049-0. [DOI] [PubMed] [Google Scholar]
- 4.Nakhai-Pour HR, Rey E, Bérard A. Antihypertensive medication use during pregnancy and the risk of major congenital malformations or small-for-gestational-age newborns. Birth Defects Res B Dev Reprod Toxicol. 2010;89:147–154. doi: 10.1002/bdrb.20238. doi: 10.1002/bdrb.20238. [DOI] [PubMed] [Google Scholar]
- 5.Magee LA, von Dadelszen P, Rey E, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372:407–417. doi: 10.1056/NEJMoa1404595. doi: 10.1056/NEJMoa1404595. [DOI] [PubMed] [Google Scholar]
- 6.Magee LA, von Dadelszen P, Singer J, et al. CHIPS Study Group*. The CHIPS Randomized Controlled Trial (Control of Hypertension in Pregnancy Study): is severe hypertension just an elevated blood pressure? Hypertension. 2016;68:1153–1159. doi: 10.1161/HYPERTENSIONAHA.116.07862. doi: 10.1161/HYPERTENSIONAHA.116.07862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tita AT, Sibai BM, Oparil S. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372:2366–2367. doi: 10.1056/NEJMc1503870. doi: 10.1056/NEJMc1503870#SA1. [DOI] [PubMed] [Google Scholar]
- 8.von Dadelszen P, Payne B, Li J, et al. PIERS Study Group. Prediction of adverse maternal outcomes in pre-eclampsia: development and validation of the fullPIERS model. Lancet. 2011;377:219–227. doi: 10.1016/S0140-6736(10)61351-7. doi: 10.1016/S0140-6736(10)61351-7. [DOI] [PubMed] [Google Scholar]
- 9.Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124:717–728. doi: 10.1542/peds.2008-2816. doi: 10.1542/peds.2008-2816. [DOI] [PubMed] [Google Scholar]
- 10.Teune MJ, Bakhuizen S, Gyamfi Bannerman C, Opmeer BC, van Kaam AH, van Wassenaer AG, Morris JM, Mol BW. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011;205:374.e1–374.e9. doi: 10.1016/j.ajog.2011.07.015. doi: 10.1016/j.ajog.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Gouyon JB, Iacobelli S, Ferdynus C, Bonsante F. Neonatal problems of late and moderate preterm infants. Semin Fetal Neonatal Med. 2012;17:146–152. doi: 10.1016/j.siny.2012.01.015. doi: 10.1016/j.siny.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Bardin C, Piuze G, Papageorgiou A. Outcome at 5 years of age of SGA and AGA infants born less than 28 weeks of gestation. Semin Perinatol. 2004;28:288–294. doi: 10.1053/j.semperi.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Kok JH, den Ouden AL, Verloove-Vanhorick SP, Brand R. Outcome of very preterm small for gestational age infants: the first nine years of life. Br J Obstet Gynaecol. 1998;105:162–168. doi: 10.1111/j.1471-0528.1998.tb10046.x. [DOI] [PubMed] [Google Scholar]
- 14.Lee MJ, Conner EL, Charafeddine L, Woods JR, Jr, Del Priore G. A critical birth weight and other determinants of survival for infants with severe intrauterine growth restriction. Ann NY Acad Sci. 2001;943:326–339. doi: 10.1111/j.1749-6632.2001.tb03813.x. [DOI] [PubMed] [Google Scholar]
- 15.von Dadelszen P, Magee LA. Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: an updated metaregression analysis. J Obstet Gynaecol Can. 2002;24:941–945. doi: 10.1016/s1701-2163(16)30592-8. [DOI] [PubMed] [Google Scholar]
- 16.Ersbøll AS, Hedegaard M, Søndergaard L, Ersbøll M, Johansen M. Treatment with oral beta-blockers during pregnancy complicated by maternal heart disease increases the risk of fetal growth restriction. BJOG. 2014;121:618–626. doi: 10.1111/1471-0528.12522. doi: 10.1111/1471-0528.12522. [DOI] [PubMed] [Google Scholar]
- 17.Xie RH, Guo Y, Krewski D, Mattison D, Walker MC, Nerenberg K, Wen SW. Beta-blockers increase the risk of being born small for gestational age or of being institutionalised during infancy. BJOG. 2014;121:1090–1096. doi: 10.1111/1471-0528.12678. doi: 10.1111/1471-0528.12678. [DOI] [PubMed] [Google Scholar]
- 18.Bayliss H, Churchill D, Beevers M, Beevers DG. Anti-hypertensive drugs in pregnancy and fetal growth: evidence for “pharmacological programming” in the first trimester? Hypertens Pregnancy. 2002;21:161–174. doi: 10.1081/PRG-120013785. doi: 10.1081/PRG-120013785. [DOI] [PubMed] [Google Scholar]


