Six geosexual archetypes were identified: hosters, house-callers, rovers, privates, travellers, and geoflexibles, each with different characteristic profiles. Prioritizing interventions to hosters, rovers, and geoflexibles may reduce sexually transmitted infection transmission.
Supplemental digital content is available in the text.
Abstract
Background
There are complex, synergistic, and persistent sexually transmitted infection (STI) epidemics affecting gay, bisexual and other men who have sex with men (gbMSM) in every major urban centre across North America. We explored the spatial architecture of egocentric sexual networks for gbMSM in Toronto, Canada.
Methods
Our integrative mixed methods study included in-depth interviews with 31 gbMSM between May and July 2016. During interviews, participants mapped their egocentric sexual network for the preceding 3 months geographically. At the end, a self-administered survey was used to collect sociodemographic characteristics, online technology use, and STI testing and history.
Results
We identified 6 geosexual archetypes: hosters, house-callers, privates, rovers, travellers, and geoflexibles. Hosters always, or almost always (≥80%), hosted sex at their home. House-callers always, or almost always (≥80%), had sex at their partner’s home. Rovers always or almost always (≥80%) had sex at public venues (eg, bath houses, sex clubs) and other public spaces (eg, parks, cruising sites). Privates had sex in private—their own home or their partner's (part hoster, part house-caller). Travellers had sex away from their home, either at a partner’s home or some other venue or public space (part house-caller, part rover). Geoflexibles had sex in a variety of locations—their home, their partner’s home, or public venues. All hosters and rovers, and to a lesser extent, geoflexibles, reported a history of syphilis and human immunodeficiency virus.
Conclusions
Prioritizing interventions to hosters, rovers, and geoflexibles may have an important impact on reducing STI transmission.
There are complex, synergistic, and persistent sexually transmitted infection (STI) epidemics affecting gay, bisexual and other men who have sex with men (gbMSM) in every major urban centre across North America.1–4 Reasons for the persistence of these epidemics are unclear because of the complex biological, behavioral, social, cultural, structural, environmental, and spatial mechanisms—and interactions between these mechanisms—that create a “system” within which STIs persist and circulate in a population.5
The geography of sex—defined as the spatial relationships between sexual partners, and their environment—is a necessary, yet understudied, part of STI transmission.5–10 As a framework, the geography of sex involves the individual and their relationship with self, sexual partners, individual activity space (the geographic area within which a person moves over the course of their daily activities),10,11 and dyad activity space (the combined geographic area accessed by both/all sexual partners over the course of relationship activities). The individual activity space provides the context within which the individual is immersed, including the individual, social, cultural, and environmental factors that may contribute to STI transmission, such as the availability of sexual partners, prevalence of STIs, and access to sexual health resources. The dyad activity space provides the context within which sexual dyads interact, move and function both independently and interdependently as sexual partners. The dyad activity space can provide insight into social and sexual interaction and sexual dynamics, including, distance between partners, travel patterns (eg, who travels to whom), where partners have sex, STI prevalence, and the spatial architecture of sexual networks.
The spatial architecture of a sexual network is the geographic map of the sexual network topology and can be visualized as the geographically referenced connections (lines/edges) between sexual partners (nodes) within sexual networks at both egocentric (an individual (ego) connected to their sexual partners [alters]) and sociocentric (the connections between all sexual network members) levels. The spatial architecture of a sexual network shows the pathways along which information and STIs can move and be transmitted through space and time.12–14 Those parts of the spatial architecture to which the individual and dyad are both contributing and exposed are defined by individual and dyad activity spaces. There is a dearth of research on the spatial architecture of sexual networks and activity space and how these relate to STI transmission.
The spatial architecture of the sexual network has been limited to the observation that sexual partners are selected within close geographic proximity.6 The development and uptake of online dating websites and geosocial networking applications (apps)15,16 may be changing the geography of sexual partner selection by expanding the geographic activity space to include places and people not normally encountered in daily life, thus, facilitating quicker and potentially more connections between sexual partners with diverse sex practices (eg, fetish-play; group sex) and safer sex practices (eg, sero-sorting; pre-exposure prophylaxis use; sex with/without condom). Apps are also redefining concepts of “local” by facilitating connections between partners who live in very close proximity, such as the same condominium complex, as well as partners who live far apart and happen to be in close geographic proximity while one or both partners are away from home. In short, how individuals navigate their sexual lives is shifting with technology, information, and culture. All of these changes may alter the spatial architecture of sexual networks, which may impact STI transmission and spread significantly.
The purpose of this study was to better understand the deep structure of STI transmission by exploring the spatial architecture of egocentric sexual networks for gbMSM in Toronto, Canada.
MATERIALS AND METHODS
Study Design
The data for this study were derived from an integrative mixed methods study.17 Unified qualitative and quantitative evidences were collected simultaneously during in-depth interviews with gbMSM (described below). Gay, bisexual and other men who have sex with men were recruited and interviewed between May and July 2016 in Toronto, Canada. The University of Toronto Research Ethics Board approved this study (protocol 32953).
Study Setting
Toronto is the largest city in Canada (2011 population, 2.6 M; metropolitan area, 5.5 M), the fourth largest metropolitan area in North America, and the most multicultural city in the world. It has a large gbMSM community and an ongoing syphilis epidemic since the year 2000.1,18 The geographic distribution of infectious syphilis in Toronto is concentrated in 1 core area (east side of central downtown), and several surrounding outbreak areas (immediately east, west, and north of the core area).1 Gonorrhea rates have been increasing among men (60% reporting same sex partners) over the past year, though human immunodeficiency virus (HIV) rates have been declining.18 For context, Toronto has a very high immigrant population, very low crime rates (especially compared to other North American cities), universal access to health care, and a comprehensive transit and bicycle system. Toronto also has the highest child poverty rate (note that overall Canada is a wealthy country) and second highest unaffordable housing rate in the country. None of these factors characterize core from noncore areas, though it was previously observed that neighborhoods with a higher proportion of immigrants were associated with lower syphilis rates and neighborhoods with greater residential instability were associated with higher syphilis rates.1
Participants
We purposively recruited a diverse sample of gbMSM using a multipronged recruitment strategy. Specifically, gbMSM were recruited through social media, dating/sex-seeking websites and geosocial networking apps, email databases of organizations invested in the gbMSM community willing to assist with recruitment, word of mouth, and posting flyers in neighborhoods with a large gbMSM presence, including coffee shops, bars, sex shops, community centers, cruising sites, and community poster boards. We monitored the characteristics of potential participants and made special effort to ensure diversity by recruiting a geographically (core and noncore areas, from urban and suburban communities), sexually (gay, bisexual, straight-identified, 2-spirit), ethnically, and age diverse sample of gbMSM both online and offline. The gbMSM were eligible for inclusion in our study if they lived, worked or socialized in Toronto or the Greater Toronto Area (GTA), and identified as: gay, bisexual, 2-spirit, or a man who has sex with other men; 18 years or older; actively or passively seeking male sex partners; and comfortable talking about sex.
Data Collection
Interviewer-administered, structured, in-depth interviews were used to ask participants about their sexual partner-seeking strategies, sexual risk-taking and knowledge of the syphilis epidemic, and to map their egocentric sexual network for up to 10 sexual partners (alters) over the preceding 3 months, including where they (ego) lived, where their partners (alters) lived, where they met (ie, online vs in-person location), and where they had sex the first time. Substance use and sexual partner characteristics (including HIV status) were documented for each sexual partner in a participant’s egocentric network. Finally, a short quantitative survey was self-administered at the end of the interview regarding participant sociodemographic characteristics, online and app sex/dating site use, and STI history, including testing. Interviews were conducted until no new information emerged from additional interviews.
All interviews were anonymous, conducted at the university (except one at a local community centre), audio recorded digitally, and transcribed verbatim. Interviews lasted 45 to 90 minutes. Egocentric sexual networks were mapped by hand during the interview by the interviewer and interviewee using a paper map of Toronto. Paper maps were digitized using ArcGIS (ESRI, Redlands, CA). Participants were remunerated for their time and knowledge.
Data Analysis
Descriptive statistics were used to summarize survey data and characterize participants’ demographics and previous STIs/STI testing history, specifically for syphilis, HIV, gonorrhea, chlamydia, herpes, human papillomavirus (HPV), genital warts, and self-defined “other” STI.
We mapped the spatial architecture of each participant’s egocentric sexual network using the digitized maps of participant residence, partner residence, and where partners had sex the first time. Data from the in-depth interviews were used to add “direction of travel for sex” arrows between partners (Fig. 1). We also used where sexual partners met to stratify arrows into sexual partners met online (dashed arrow) versus in-person (solid arrow).
Figure 1.
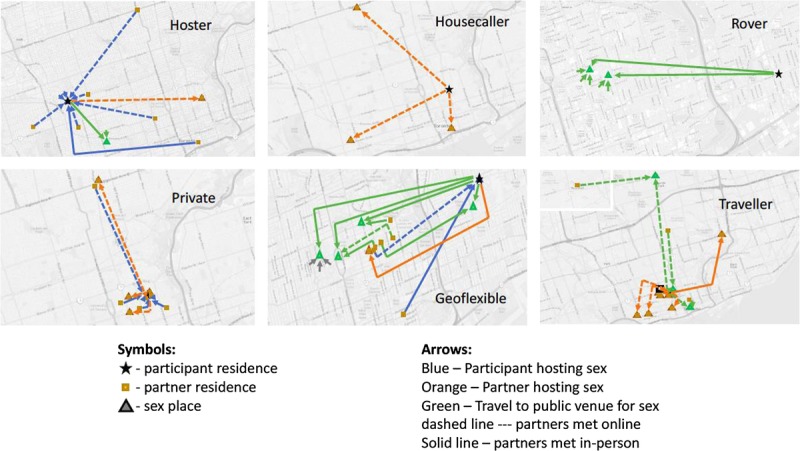
Example maps of egocentric sexual networks for each geosexual archetype. Archetypes were developed from the geographic patterns of egocentric sexual networks for 31 men who have sex with men in Toronto, Canada, 2016, based on participant residence, sexual partner residence, and where each participant had sex the first time with sexual partners from the preceding 3 months. Notes: north is at the top of each map; maps are not to scale; and scales and map centers differ between maps.
We visually interpreted the spatial architecture of each participant's egocentric network map with particular attention to the patterns of where and how far participants were travelling for sex, and which sexual networks (online vs in-person) were being accessed.
We calculated the total number of sexual partners, measured the distance travelled for sex within the GTA, and measured the distance travelled for sex outside the GTA. Distance travelled was estimated for sexual partners with a known residential location (129 partner residence known of 175 partners, or 74% of the partners). Shortest travel path based on Toronto's street network was used to estimate travel distance within the City of Toronto. Straight-line distance was used to estimate travel distance for sexual partners outside of Toronto (for example, sexual partners living in Hamilton, Vancouver, Brazil). We also quantified where each participant had sex by calculating the proportion of sex at home, at partners' homes, and at public venues and visualized the distribution of these triplets (proportions of locations of sex) on a triangle plot—also known as a ternary diagram.19 Triangle plots are ideal for visualizing data where observations must sum to a constant; in our case, the probabilities of sex with partner in a given location had to sum to 1. The closer to a vertex of the triangle a participant fell, the more homogenous the participant’s choice of sex location.
We aggregated individual egocentric sexual network patterns into group-level geosexual archetype classifications and characterized each archetype post hoc by number of sexual partners, proportion of sexual partners met online, basic sociodemographic characteristics, distance travelled for sex (separately for within the GTA and outside of the GTA), STI testing in the preceding year, and history of STIs. Archetypes were compared across group-level characteristics.
Finally, we mapped the spatial distribution of egocentric archetypes in relation to core and noncore areas. We also began to conceptualize the role of geography and geosexual archetype on STI transmission based on the results.
RESULTS
Thirty-one gbMSM were interviewed (63 individuals expressed interest in response to recruitment ads, of which 16 were not assessed due to dropped communication, 10 were not eligible based on inclusion criteria, and 6 did not show up for their interview). Participants ranged in age from 18 to 72 years (average, 37 years). Slightly more than half the participants identified as white (55%) and the remainder as Asian (10%), Latin (10%), mixed race (10%), black (6%), indigenous (3%), or unreported race (10%). Self-reported number of sexual partners in the preceding 3 months ranged from having 1 to 10 or more sexual partners, with an average of 5 partners (Table 1). The majority used websites and geosocial networking apps to find sex partners and had been tested for STIs in the preceding year (Table 1). Almost 30% of participants had sex out of town, with some travelling to the suburbs and others traveling much greater distances (maximum distance travelled, approximately 5000 km; Table 1). The most commonly reported previous STIs (lifetime) in descending order were gonorrhea and chlamydia, followed by syphilis, HIV, herpes, and HPV (Table 1).
TABLE 1.
Characteristics of Participants by Geosexual Archetypes
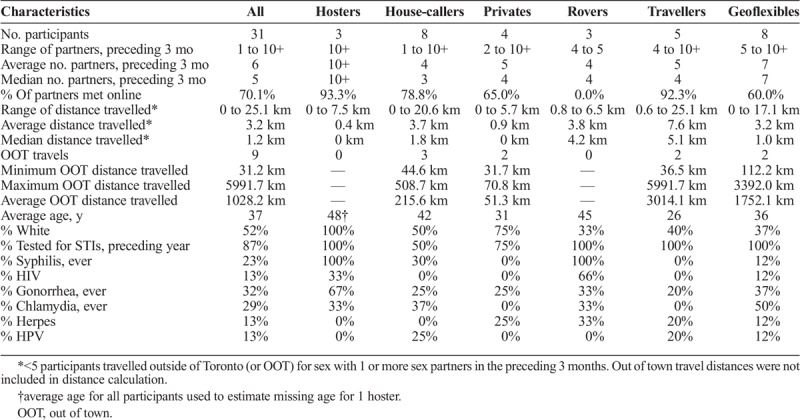
We identified 6 geosexual archetypes: hosters, house-callers, rovers, privates, travellers, and geoflexibles (Fig. 1). Hosters always, or almost always (≥80%), hosted sex at their residence (Fig. 2). Similarly, house-callers always, or almost always (≥80%), had sex at their partner's residence, and rovers always or almost always (≥80%) had sex at public venues (eg, bath houses, sex clubs) and other public spaces (eg, parks, cruising sites) and did not have sex at their own residence nor a partner’s residence. Privates only had sex at private residences—their own or their partners making them part hoster, part house-caller. Travellers only had sex away from their residence, either at a partner’s residence or some other venue or public space, making them part house-caller, part rover. Geoflexibiles had sex in any of the 3 environments—their home, their partner’s home, or public places and spaces, making them part hoster, part house-caller, part rover. Each participant could be classified into 1 of these 6 archetypes according to their own accounts of their sexual travel. Most participants were geoflexibles or house-callers (Table 1, Fig. 2). There was theoretical evidence suggesting a seventh geosexual archetype that would be part hoster, part rover; however, this classification was not observed.
Figure 2.
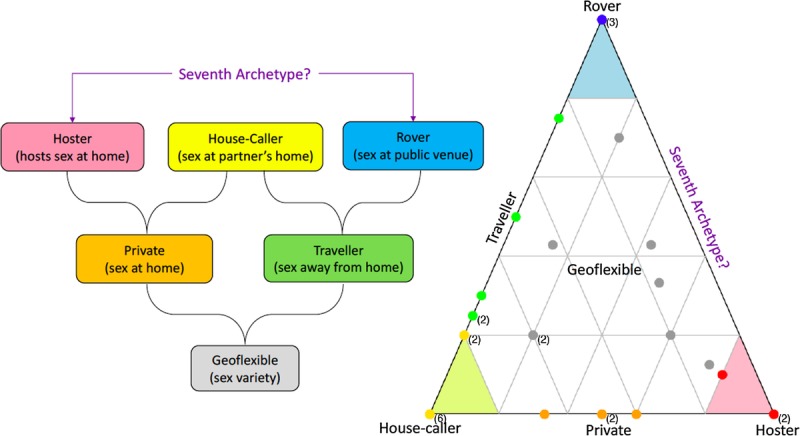
Relationship between, and distribution of, sexual archetypes defined by where participant had sex the first time with each sexual partner in the preceding 3 months. Specifically, hosters (red) hosted sex at their home; house-callers (yellow) travelled to their partner(s) home(s); privates (orange) hosted or travelled to their partner’s home; rovers (blue) had sex in public venues; travellers (green) travelled to their partner's home or a public venue; and geoflexibles (grey) had sex in a variety of locations. Theoretically, there could be a seventh archetype that is part hoster, part rover; however, no participants fell along this edge. Note: numbers in brackets represent the number of participants in the same location on the graph. Grey lines on the triangle graph are in 20% increments. The closer to a vertex of the triangle a participant falls the more homogenous this participant’s choice of sex destination.
Each of the 6 geosexual archetypes could be found in core, outbreak, and noncore areas (see supplemental map, http://links.lww.com/OLQ/A215). We also found evidence suggesting the geosexual archetypes had different characteristic profiles when we stratified our descriptive analysis by archetype (Table 1). For example, all hosters and rovers and some geoflexibles had a history of syphilis. These were also the only archetypes to include participants living with HIV. Hosters were white, did not travel for sex, had the highest number of sexual partners in the preceding 3 months, and met most of their partners online. House-callers had the fewest sexual partners in the preceding 3 months, and although they usually stayed local, sometimes travelled out of town for sex. Rovers were predominantly nonwhite, only had a few partners in the preceding 3 months that they met in-person, and they stayed local for sex (5 km or less). Travellers found most partners online and traveled the furthest for sex, including out of town. Privates did not travel very far on average for sex, though may travel out of town locally on occasion. Finally, geoflexibles were the most flexible and diverse archetype, having the greatest ethnic diversity, the second highest number of partners in the preceding 3 months, meeting partners online and in-person, and having sex in a variety of locations locally and out of town.
DISCUSSION
We identified and began profiling 6 geosexual archetypes based on the spatial architecture of 31 diverse gbMSM egocentric sexual networks mapped using sexual partners over the preceding 3 months. Specifically, we identified: hosters, house-callers, privates, rovers, travellers, and geoflexibles (Figs. 1 and 2). A seventh archetype, sirens, was theoretically identified but not observed (Fig. 2). We hypothesize this archetype may be uncommon, if it exists at all. One scenario under which this archetype could occur is a roving-hoster, meaning an individual who does not travel for sex and rather gathers or calls in partners by hosting sex at home, the bathhouse, or a sex party or club, hence the title sirens.
Previous gonorrhea diagnosis was observed for all geosexual archetypes and highest for hosters, rovers, and geoflexibles (Table 1). This finding merits further investigation given the multidrug-resistant gonorrhea epidemic emerging in Toronto and other cities around the world.20 The HIV positivity was also highest for hosters, rovers, and geoflexibles (Table 1), and all hosters and rovers and some geoflexibles reported a previous syphilis diagnosis (Table 1). Applying core theory21–23 to these findings suggests that hosters, rovers, and to some extent, geoflexibles may be part of a core group(s), which may account for STI transmission both inside and outside core areas, and between core and noncore areas. This hypothesis of core groups is underscored by the finding that geosexual archetypes were observed in core, outbreak and noncore-nonoutbreak areas and did not cluster geographically (see supplemental map, http://links.lww.com/OLQ/A215), and further supported by the persistence of the syphilis epidemic in Toronto despite resources and interventions targeting the core area.
The hypothesized connectivity between geosexual archetypes (Fig. 3) could shed further light on STI transmission dynamics and mixing patterns between core and noncore areas.24 For example, geoflexibles met partners both online and in-person and were willing to having sex with a new partner at home, which accommodated house-callers, privates, travellers, and other geoflexibles; at their partner's home, which accommodated hosters, privates and other geoflexibles; or in a public space, which accommodated rovers, travellers, and other geoflexibles. This flexibility suggests geoflexibles could connect with any other geosexual archetype, including their own. It also makes geoflexibles ideal bridge contacts.
Figure 3.

Hypothesized connections (solid lines) between geosexual archetypes based on egocentric sexual network spatial architecture and archetype characteristics. Hypothetical sexual network connections of a siren are included (dashed lines).
On the contrary, hosters, house-callers, and rovers had sex with new partners in a single location, suggesting these archetypes may have more limited connectivity with other geosexual archetypes, including their own, depending on the archetype. For instance, hosters and rovers were not likely to connect because hosters found new partners online and did not leave their home for sex and rovers did not have sex at anyone's home and found partners in-person (Table 1, Fig. 3). From an epidemic perspective, the incompatible sexual behaviours of hosters and rovers suggest that the syphilis epidemic in Toronto either involves two simultaneously co-occurring outbreaks in different core groups (hosters and rovers), or 1 outbreak being spread between core groups by geoflexibles, who have much lower reports of previous syphilis diagnosis but are likely to bridge hosters and rovers given their potential to have sex with partners from either archetype (Fig. 3).
The act of sex is a time-varying event13,25,26 where the temporality of sex can be conceptualized and recalled using calendar time (eg, days, weeks, months, years, lifetime) and event time (eg, first time had sex, last time had sex). We restricted our exploration to sexual partners in the preceding 3 calendar months to both aid recall and focus on the most current components of the egocentric sexual network. We selected a single reference point in event time—first time had sex with partner—recognizing the need for consistency and comparability in sex event within and across participants, that the first time is one of the most memorable and thus recalled more reliably, and that “new sexual partner” is a risk factor for STIs transmission. One major tradeoff was that event time (the first time someone had sex with a partner) was out of synchronicity with calendar time (preceding 3 months) for sexual partnerships longer than 3 months. Very few participants reported long-term partners in our study, though some did. The spatial architecture of egocentric sexual networks may have appeared differently had we chosen a different reference sex event, such as where sex happened most frequently, or most recently. The spatial architecture may also change over calendar time, especially for geographies impacted by significant seasonality (such as Toronto). Future studies should explore different sex event times; determine the impact of time on the geography of sex longitudinally; and determine geosexual archetype stability within individual, by stages of life, aging, and season.
Our geosexual archetypes were generated under the assumption of equal weighting for each sexual partner and did not account for relationship type (eg, long-term commitment versus a hook-up) or frequency of sex with that partner. The 80% classification threshold for a hoster, house-caller, or rover meant that long-term partnerships weighed the same as one-time encounters. For example, if a married participant had most sex at home with his spouse, but also had sex with 4 other hook-ups—1 at one partner’s home and 3 others while cruising—they would be classified as geoflexible (20% home, 20% partners home, 60% public venue). If that same married participant had sex with all the 4 hook-ups at cruising sites and bars around the city, they would be classified as a rover (20% home, 80% public venue). Therefore, our archetype classification is insensitive to relationship type but is sensitive to where sex is occurring (geographic location of sex). We selected a threshold of 80% to classify participants into 1 of these 3 categories based on the observation that a 100% threshold was too strict and could cause misclassification (eg, a participant who had sex with 8/10 partners at home but went to 1 partner's house for sex and had sex in 1 public venue would be classified geoflexible rather than a hoster, which did not accurately reflect their behavior), whereas a threshold of 75% was too lax (Fig. 2).
We did not collect information on the gender of each sexual partner explicitly; however, this study was targeted to gbMSM so it is likely that participants focused their interview on male partners. The interview transcripts suggested that all reported sexual partners were male-identified. However, it is also likely that some participants had female partners in the preceding 3 months that they did not report, especially bisexual participants (6% of sample). Egocentric sexual networks that include female sexual partners may have different geographic patterns and spatial architecture, with different implications for STI transmission.
Our geosexual archetype classifications are based on an integration of qualitative and quantitative analysis of interviews detailing the egocentric sexual networks of 31 gbMSM. Statistical inferences cannot be made about differences between archetypes given the small sample size. Our findings are preliminary and need to be verified using a larger sample of gbMSM. At the same time, the 3-axis structure of the 7 geosexual archetype classification system (percent sex at home, percent sex at partner’s home, percent sex at a public venue; Fig. 2) should be comprehensive and robust, and thus, the classification system should be transferable to other settings and populations, even if the proportional composition and characteristics of archetypes differ by place and context. For instance, a more suburban environment with limited transit and fewer public spaces may have more privates or geoflexibles, all archetypes may travel further (on average) for sex, and the reasons for being a suburban hoster (eg, disability) may differ from those for being an urban hoster (eg, high proportion of gbMSM in very close proximity).
A larger explanatory study is needed to determine the generalizability/transferability of our archetype findings; better define and characterize the archetypes, for instance, by personality, attachment style, and emotional development; assess how well the archetypes resonate with participants themselves; and further explore how each archetype may impact STI transmission and intervention. Our findings suggest a potential role for tailoring STI interventions and prevention strategies to reach hosters, rovers, and geoflexibles, especially if they can serve as sensors for selective monitoring.27,28 Online testing programs like GetCheckedOnline have increased access to sexual health messaging and testing outside core areas,29 which is especially promising for men who use the internet to find sexual partners,30 such as hosters.
Supplementary Material
Footnotes
Source of Funding: Funded in part by Canadian Institutes of Health Research funding reference number 492948.
Conflict of Interest: None declared.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
REFERENCES
- 1.Gesink D, Wang S, Norwood T, et al. Spatial epidemiology of the syphilis epidemic in Toronto, Canada. Sex Transm Dis 2014; 41:637–648. [DOI] [PubMed] [Google Scholar]
- 2.Solomon MM, Mayer KH. Evolution of the syphilis epidemic among men who have sex with men. Sex Health 2015; 12:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis DA. The role of core groups in the emergence and dissemination of antimicrobial-resistant N gonorrhoeae. Sex Transm Infect 2013; 89(Suppl 4):iv47–iv51. [DOI] [PubMed] [Google Scholar]
- 4.Stenger MR, Pathela P, Anschuetz G, et al. Increases in the rate of Neisseria gonorrhoeae among gay, bisexual and other men who have sex with men—findings from the Sexually Transmitted Disease Surveillance Network 2010–2015. Sex Transm Dis 2017; 44:393–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothenberg R. Maintenance of endemicity in urban environments: a hypothesis linking risk, network structure and geography. Sex Transm Infect 2007; 83:10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gindi RM, Sifakis F, Sherman SG, et al. The geography of heterosexual partnerships in Baltimore city adults. Sex Transm Dis 2011; 38:260–266. [DOI] [PubMed] [Google Scholar]
- 7.Logan JJ, Jolly AM, Blanford JI. The Sociospatial Network: risk and the role of place in the transmission of infectious diseases. PLoS One 2016; 11:e0146915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mustanski B, Birkett M, Kuhns LM, et al. The role of geographic and network factors in racial disparities in HIV among young men who have sex with men: an Egocentric Network Study. AIDS Behav 2015; 19:1037–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poletto C, Tizzoni M, Colizza V. Heterogeneous length of stay of hosts' movements and spatial epidemic spread. Sci Rep 2012; 2:476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaughan AS, Kramer MR, Cooper HL, et al. Activity spaces of men who have sex with men: an initial exploration of geographic variation in locations of routine, potential sexual risk, and prevention behaviors. Soc Sci Med 2017; 175:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mason M, Mennis J, Way T, et al. Young adolescents' perceived activity space risk, peer networks, and substance use. Health Place 2015; 34:143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kretzschmar M. Sexual network structure and sexually transmitted disease prevention: a modeling perspective. Sex Transm Dis 2000; 27:627–635. [DOI] [PubMed] [Google Scholar]
- 13.Rocha LE, Liljeros F, Holme P. Simulated epidemics in an empirical spatiotemporal network of 50,185 sexual contacts. PLoS Comput Biol 2011; 7:e1001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rocha LE, Liljeros F, Holme P. Information dynamics shape the sexual networks of Internet-mediated prostitution. Proc Natl Acad Sci U S A 2010; 107:5706–5711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lorimer K, Flowers P, Davis M, et al. Young men who have sex with men's use of social and sexual media and sex-risk associations: cross-sectional, online survey across four countries. Sex Transm Infect 2016; 92:371–6. [DOI] [PubMed] [Google Scholar]
- 16.Beymer MR, Weiss RE, Bolan RK, et al. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect 2014; 90:567–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Castro FG, Kellison JG, Boyd SJ, et al. A methodology for conducting integrative mixed methods research and data analyses. J Mix Methods Res 2010; 4:342–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toronto Public H. Sexually Transmitted Bloodborne Infections: Communicable Diseases in Toronto, 2015. In. http://www1.toronto.ca/City Of Toronto/Toronto Public Health/Communicable Disease Control/Communicable Disease Surveillance/Annual Reports/Files/pdf/2/STIwHeps_AnnualReport_eng_2015_v2.pdf; 2016.
- 19.Howarth RJ. Sources for a history of the ternary diagram. Br J Hist Sci 1996; 29:337–356. [Google Scholar]
- 20.Alirol E, Wi TE, Bala M, et al. Multidrug-resistant gonorrhea: a research and development roadmap to discover new medicines. PLoS Med 2017; 14:e1002366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yorke JA, Hethcote HW, Nold A. Dynamics and control of the transmission of gonorrhea. Sex Transm Dis 1978; 5:51–56. [DOI] [PubMed] [Google Scholar]
- 22.Thomas JC, Tucker MJ. The development and use of the concept of a sexually transmitted disease core. J Infect Dis 1996; 174(Suppl 2):S134–S143. [DOI] [PubMed] [Google Scholar]
- 23.Gesink DC, Sullivan AB, Miller WC, et al. Sexually transmitted disease core theory: roles of person, place, and time. Am J Epidemiol 2011; 174:81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doherty IA, Serre ML, Gesink D, et al. Sexual networks, surveillance, and geographical space during syphilis outbreaks in rural North Carolina. Epidemiology 2012; 23:845–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holme P. Information content of contact-pattern representations and predictability of epidemic outbreaks. Sci Rep 2015; 5:14462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karsai M, Perra N, Vespignani A. Time varying networks and the weakness of strong ties. Sci Rep 2014; 4:4001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herrera JL, Srinivasan R, Brownstein JS, et al. Disease Surveillance on Complex Social Networks. PLoS Comput Biol 2016; 12:e1004928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bai Y, Yang B, Lin L, et al. Optimizing sentinel surveillance in temporal network epidemiology. Sci Rep 2017; 7:4804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert M, Haag D, Hottes TS, et al. Get checked… Where? The Development of a comprehensive, integrated internet-based testing program for sexually transmitted and blood-borne infections in British Columbia, Canada. JMIR Res Protoc 2016; 5:e186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brennan DJ, Lachowsky NJ, Georgievski G, et al. Online outreach services among men who use the internet to seek sex with other men (MISM) in Ontario, Canada: an online survey. J Med Internet Res 2015; 17:e277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


