Abstract
Objective:
This study aimed to examine a detailed breakdown of costs (absenteeism, presenteeism, and medical/pharmaceutical expenses), of the employees in four pharmaceutical companies in Japan.
Methods:
This is a cross-sectional study. Absenteeism and presenteeism were measured by a self-administered questionnaire for workers, and their costs were estimated using the human capital approach. Presenteeism was evaluated by the degree affected quality and quantity of work. Medical and pharmaceutical expenses were obtained by insurance claims.
Results:
The monetary value due to absenteeism was $520 per person per year (11%), that of presenteeism was $3055 (64%), and medical/pharmaceutical expenses were $1165 (25%). Two of the highest total cost burdens from chronic illness were related to mental (behavioral) health conditions and musculoskeletal disorders.
Conclusion:
A total cost approach can help employers set priorities for occupational health, safety, and population health management initiatives.
Keywords: absenteeism, medical and pharmaceutical expenses, presenteeism
In Japan, the 2016 expenditure on health care was 10.9% of the gross domestic product (GDP). Among the Organization for Economic Co-operation and Development (OECD) countries, the USA had the highest health care expenditures, at 17.2% of GDP—highlighting the fact that rising medical and pharmaceutical expenses are one of the most significant issues in the world.1 Policy makers have been concerned that more than 80% of total health care costs go toward care for people with chronic conditions—with many of those people being retirees.2 Therefore, in order to control this growing burden of chronic illness, it is important to conduct preventive interventions for young to middle-aged persons, with one of the greatest opportunities to make this impact through workplace health initiatives.
In the workplace, the economic burden of poor health from a societal perspective is not only medical and pharmaceutical expenses but also health-related productivity loss due to sick-leave (called “absenteeism”) and reduced performance while at work due to uncontrolled diseases or health risks (called “presenteeism”).3–9 Several studies have revealed that the economic burden due to absenteeism and presenteeism was much greater than medical/pharmacy expenses.10–12 Therefore, understanding a detailed breakdown of total health-related costs (medical and pharmaceutical expenses, monetary value due to absenteeism and presenteeism) is important for policy makers.
Employers also have a strong interest in this topic of health-related productivity loss. In fact, employers are often compelled to make decisions about increasing their investments in workers’ health and safety, when they see an aggregated analysis of the disease-specific burden of illness and related health-related productivity loss in their workforce. The employer studies found the top three medical and pharmacy expenses of diseases or conditions were cancer, back/neck pain, and other chronic pain, and the top three conditions leading to the highest total costs (medical/pharmacy, absenteeism/presenteeism) were depression, obesity, and arthritis.11,12 This information has changed employers’ or health care professionals’ decisions as to which conditions and health care services should be conducted on a priority basis. Furthermore, several past studies in Japan have also revealed the economic impact of the loss of performance due to health-related absenteeism and presenteeism.13,14 However, in Japan, integrating the health-related productivity data with the medical/pharmacy expense data has been lacking.
Japan had made the universal health coverage by establishment of employee-based and community-based social health insurance, and almost everyone came to be insured in 1961.15 Large companies often built the health insurance unions, which insure all employees and their family. In this study, we were able to obtain the complete data of medical and drug expenses of employees by use of health insurance claims except for medical treatment not covered by insurance. The present study aimed to examine a detailed breakdown of expenses (medical and pharmaceutical expenses, and estimated monetary value due to absenteeism and presenteeism) by diseases or symptoms, of the employees in four pharmaceutical companies in Japan.
METHODS
We conducted this study in four pharmaceutical companies and their related health insurance unions. This is a cross-sectional study to calculate total costs due to absenteeism, presenteeism, and medical and pharmaceutical expenses during 1 year (fiscal year 2014). We obtained health data by a self-administered questionnaire for workers once in 2014 to evaluate absenteeism and presenteeism during the past 3 months. Using these data, we estimated costs due to absenteeism and presenteeism for a year. We also analyzed the related claims data from April 1, 2014, to March 31, 2015, from each health insurance union to calculate medical and pharmaceutical expenses in the study populations.
Ethics
The study design was explained to employees and employers through email, intranet homepage, or committee of occupational health and safety in each company and health insurance union. Employees have the freedom to choose whether to participate the study or not. Employers cannot see each answer of self-administered questionnaire.
This study was approved by the ethics committee of University of Occupational and Environmental Health, Kitakyushu, Japan.
Self-administered Questionnaire
The self-administered questionnaire was conducted in four pharmaceutical companies (company A-D). Employees could choose to participate in the survey or not. Only researchers were able to access the results of the questionnaires, and therefore, the study employers and health care staff in those companies were not able to access the questionnaire data. Health care staff in each company sent an email to all employees to inform and encourage to participate in the confidential health survey. Health care staff in company B and D sent an email just once. On the contrary, health care staff in company A and C explained the purpose of the survey to managers before sending an email of information, and send reminder message 2 or 3 weeks later.
Table 1 summarizes sample details. In company A and C, response rate was high (86.5% and 78.6%, respectively); on the contrary, in company B and D not as high (32.7% and 33.4% respectively). The number of the total sample size in the final analysis was 12,350 employees, which was an aggregate average of 58% of the 21,293 total eligible employees across the four employers.
TABLE 1.
Sample Details in Four Pharmaceutical Companies
| Company | Number of Eligible Employees | Number of Valid Questionnaire Respondents | Response Rate (%) | Number of Missing Data | Number of Sample in Final Analysis |
| Company A | 6,932 | 5,997 | 86.5 | 369 | 5,628 |
| Company B | 5,159 | 1,688 | 32.7 | 90 | 1,598 |
| Company C | 5,261 | 4,136 | 78.6 | 107 | 4,029 |
| Company D | 3,941 | 1,316 | 33.4 | 221 | 1,095 |
| Total | 21,293 | 13,137 | 61.7 | 787 | 12,350 |
Presenteeism
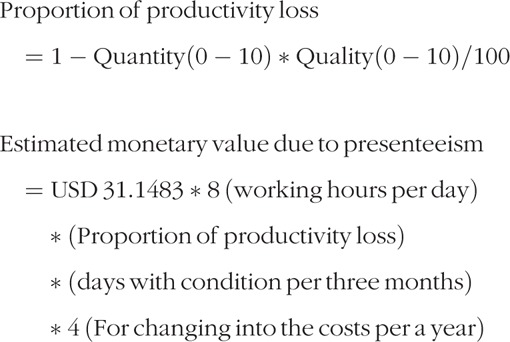
We estimated monetary value due to presenteeism by the following steps from the self-administered questionnaire.
First, we asked they had experienced some health conditions or health risks over the past month. We reviewed as many symptoms as possible that Japanese workers may have through a national database,16 the previous study,11,12 and selected 34 conditions by our researchers’ discussion. The 34 conditions are 1; Respiratory trouble, 2; Liver disease, 3; Diabetes, 4; Dyslipidemia, 5; High blood pressure, 6; Heart disease, 7; Cancer, 8; Anemia, 9; Osteoporosis, 10; Troubled by allergies, 11; Skin disease/Itchiness, 12; Asthma, 13; Cold, influenza, 14; Gastroenteritis, 15; Stomach ulcer, duodenal ulcer, 16; Recurrent diarrhea, constipation, 17; Heartburn, 18; Pain in arm and leg joints, lack of mobility, 19; Back pain, 20; Painful neck or stiff shoulders, 21; Headaches, 22; Tooth trouble, 23; Depression, 24; Anxiety, 25; Insomnia, 26; Insufficient sleep, 27; Menopausal symptoms, 28; Infertility treatment, 29; A sense of weariness or fatigue, 30; Hangover, 31; Deteriorating hearing, 32; Dry eye, glaucoma, etc, 33; Urine-related problems, and 34; Others. If no health problems or conditions, we estimated that productivity loss was nothing. Second, if they had some conditions, we asked which health condition out of 34 they had, and to select the one health condition that they had the biggest effect on their work. We allocated 34 conditions into International Statistical Classification of Diseases and Related Health Problems (ICD) version 10 code. Third, we asked to how many days they had experienced their symptom over the past 3 months. Fourth, we asked the degree of severity how their symptom affected quality and quantity of work, respectively. We asked the quality/quantity of work that they were able to carry out when suffering from their symptom in comparison to when they are not suffering from those conditions or symptoms. The answer was score from 0 (no productivity) to 10 (no productivity loss). We adopted the method that was used in the past study.17,18 The construct validity of this measurement was evaluated in the past study. 18
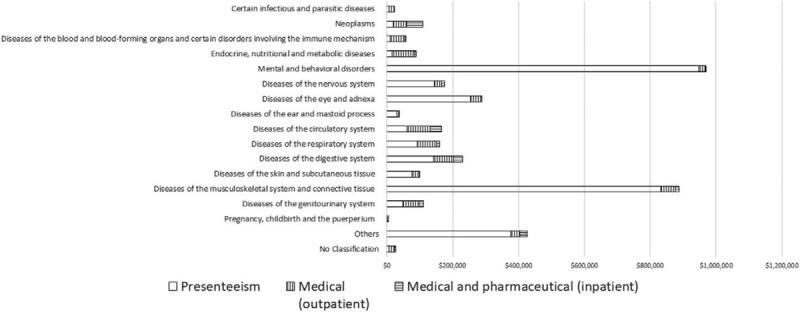
Finally, we calculated proportion of productivity loss and exchanged it for monetary value due to presenteeism by the following formulas.
Average payroll per person per hour was Japanese Yen (JPY) 3300 [that was 31.1483 US Dollar (USD)] in large manufacturing companies in Japan.19 One USD was JPY 105.9448 by average exchange rate in 2014.
 |
Absenteeism
We asked sick-leave days taken over the course of the past 3 months by the self-administered questionnaire.
We estimated monetary value due to absenteeism by following formula.
 |
Medical and Pharmaceutical Expenses
The health insurance unions have the data of medical and pharmaceutical expenses based on compensation claims. We received inpatient claims (including medical and pharmaceutical expenses), outpatient medical claims, and outpatient pharmaceutical claims of all samples from April 1, 2014, to March 31, 2015. These claims do not include dental treatment. Inpatient claims and outpatient medical claims had name of patient, name of illness or injury, and medical or pharmaceutical expenses, so we were able to calculate the expenses by ICD10 code. On the contrary, outpatient pharmaceutical claims did not have the name of the illness or injury, so we just obtained the total outpatient pharmaceutical claims expenses.
Health Risks
To reveal the characteristics of sample in this study, we evaluated the health risks of the study populations. Edington did significant research establishing 15 health risks of individuals and he revealed that a high-risk category is associated with higher medical expenses.20,21 We used the high-risk definitions of the comparable nine health risks among 15 health risks that have been utilized in many prior studies.20–23 The high-risk definitions are described in Table 2.
TABLE 2.
Health risk definitions and health risk distribution of this study and the past study
| People and Overall Population (12,350) With High Risk in this study | People and Overall Population (7,804) With High Risk in US study | ||||
| Health Risk Definitions (Loeppke et al22) | N | % | N | % | |
| Alcohol | More than 14 drinks per week or binge drinking once or more in past month | 2,392 | 20 | 901 | 12 |
| Blood pressure | Systolic, >139 mm Hg or Diastolic, >89 mm Hg | 1,132 | 10 | 923 | 12 |
| Body mass index | 27.8 (men) 27.3 (women) | 943 | 8 | 3,338 | 43 |
| Cholesterol | Total cholesterol > 239 mg/dL | 1,151 | 10 | 836 | 11 |
| Existing medical problems | Heart problems, cancer, diabetes, or stroke | 751 | 6 | 910 | 12 |
| Fasting blood glucose | Fasting glucose borderline high (≥100 and < 126 mg/dL) or high (≥126 mg/dL) | 2,155 | 18 | 1,616 | 21 |
| HDL cholesterol | HDL cholesterol < 35 mg/dL | 131 | 1 | 328 | 4 |
| Perception of health | Fair or poor | 1,397 | 11 | 842 | 11 |
| Smoking | Current smoker/tobacco user | 2,644 | 22 | 489 | 6 |
Alcohol, existing medical problems, perception of health, and smoking was evaluated by the self-administered questionnaire. Blood pressure, body mass index (BMI), cholesterol, and high-density lipoprotein (HDL) cholesterol was evaluated by health checkup data in 2014. In Japan, employers have to conduct annual health checkup and employees have to get it by legal requirement.24 We took serum total cholesterol (TC) as cholesterol. In the absence of TC data, we took “low density lipoprotein cholesterol + HDL cholesterol + triglyceride (TG)/5” as TC if TG was less than 400 mg/dL.25
We compared the proportion with each health risk in our sample to that in the past study.22
Statistical Analysis
All data analyses were performed using IBM SPSS Statistics 22.0 software (SPSS, Inc., Chicago, Illinois). To reveal workers with symptoms or not by sex, age, and occupation, we used Chi-square tests for sex and occupation and used a Chi-square test for trend to assess a linear trend in proportions across the categories of age. All tests were two-tailed, with differences reported as significant if P value was less than 0.05.
RESULTS
The number of total sample in final analysis was 12,350, 9224 male (75%), and 3126 female (25%). The characteristic in this study is summarized in Table 3. Our sample consisted of 1372 (11%) as 19 to 29 years old, 2779 (23%) as 30 to 39 years old, 4359 (35%) as 40 to 49 years old, 3462 (28%) as 50 to 59 years old, and 378 (3%) as more than 60 years old. Three thousand nine hundred thirty-five (32%) were Sales, 2473 (20%) were Research and Development, 2258 (18%) were Manager, 2215 (18%) were Production line, 1449 (12%) were Clerical and administrative support, and 20 (0.2%) were others.
TABLE 3.
The Sample Characteristic of This Study
| N | % | |
| Gender | ||
| Male | 9,224 | 74.7 |
| Female | 3,126 | 25.3 |
| Age, years | ||
| 19–29 | 1,372 | 11.1 |
| 30–39 | 2,779 | 22.5 |
| 40–49 | 4,359 | 35.3 |
| 50–59 | 3,462 | 28.0 |
| ≥60 | 378 | 3.1 |
| Occupation | ||
| Manager | 2,258 | 18.3 |
| Clerical and administrative support | 1,449 | 11.7 |
| Sales | 3,935 | 31.9 |
| Research and development | 2,473 | 20.0 |
| Production line | 2,215 | 17.9 |
| Others | 20 | 0.2 |
| Total | 12,350 | 100 |
Health risk definitions and health risk distribution of this study is summarized in Table 2. Top three high health risks were smoking (2644 out of 12,262, 22%), alcohol (2392 out of 12,257, 20%), and fasting blood glucose (2155 out of 11,745, 18%).
Demographic distributions with symptoms or not and the degree of the symptoms are described in Table 4. Twenty-five percent of male and 34% female had some symptoms. Fifty to 59-year-old workers had the highest prevalence of symptoms (31%).
TABLE 4.
Demographic Distributions With Symptoms or Not, and the Degree of the Symptoms
| With Symptoms | ||||||||||
| No Symptoms | With Symptoms | PL = 0% | 0%<PL≤20% | 20%<PL≤40% | 40%<PL≤60% | 60%<PL≤100% | ||||
| N | % | N | % | P | % | % | % | % | % | |
| Gender | ||||||||||
| Male | 6,950 | 75.3 | 2,274 | 24.7 | <0.001* | 4.4 | 5.6 | 5.3 | 4.3 | 5.0 |
| Female | 2,077 | 66.4 | 1,049 | 33.6 | 6.8 | 8.1 | 7.2 | 4.7 | 6.7 | |
| 0.0 | 0.0 | 0.0 | 0.0 | |||||||
| Age, years | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 19–29 | 1,117 | 81.4 | 255 | 18.6 | <0.001† | 1.7 | 3.2 | 4.2 | 3.6 | 5.8 |
| 30–39 | 2,124 | 76.4 | 655 | 23.6 | 3.6 | 4.7 | 5.3 | 4.4 | 5.6 | |
| 40–49 | 3,131 | 71.8 | 1,228 | 28.2 | 5.2 | 6.7 | 6.2 | 4.5 | 5.5 | |
| 50–59 | 2,374 | 68.6 | 1,088 | 31.4 | 6.8 | 8.0 | 6.6 | 4.9 | 5.3 | |
| ≥60 | 281 | 74.3 | 97 | 25.7 | 8.7 | 8.2 | 3.2 | 2.4 | 3.2 | |
| 0.0 | 0.0 | 0.0 | 0.0 | |||||||
| 0.0 | 0.0 | 0.0 | 0.0 | |||||||
| Occupation | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| Manager | 1,652 | 73.2 | 606 | 26.8 | <0.001* | 5.3 | 7.4 | 6.5 | 4.2 | 3.5 |
| Clerical and administrative support | 1,008 | 69.6 | 441 | 30.4 | 6.0 | 7.8 | 7.5 | 4.1 | 5.1 | |
| Sales | 2,941 | 74.7 | 994 | 25.3 | 4.0 | 5.1 | 5.0 | 4.5 | 6.8 | |
| Research and development | 1,830 | 74.0 | 643 | 26.0 | 4.8 | 6.2 | 6.3 | 4.4 | 4.3 | |
| Production line | 1,583 | 71.5 | 632 | 28.5 | 6.2 | 6.4 | 4.7 | 4.7 | 6.5 | |
| Others | 13 | 65.0 | 7 | 35.0 | 5.0 | 5.0 | 5.0 | 10.0 | 10.0 | |
| 0.0 | 0.0 | 0.0 | 0.0 | |||||||
| Total | 9,027 | 73.1 | 3,323 | 26.9 | 5.0 | 6.3 | 5.8 | 4.4 | 5.4 | |
PL, proportion of productivity loss due to presenteeism.
*Chi-square test.
†Chi-square test for trend.
The monetary value due to presenteeism per person per year was $3055 USD. The symptoms with greater productivity losses were painful neck or stiff shoulders, insufficient sleep, back pain, dry eye, glaucoma, and depression (Table 5).
TABLE 5.
The List of 34 Health Conditions, the Number With Each Symptom, and Estimated Monetary Value Due to Presenteeism per Person per Year by Each Condition With ICD10 Code and Classification Headings
| Health Conditions | ICD10 Code | Classification Headings of ICD10 | N | Monetary Value Due to Presenteeism per Person per Year (USD) |
| Painful neck or stiff shoulders | M00M99 | Diseases of the musculoskeletal system and connective tissue | 420 | $432.92 |
| Insufficient sleep | F00F99 | Mental and behavioral disorders | 266 | $341.58 |
| Back pain | M00M99 | Diseases of the musculoskeletal system and connective tissue | 283 | $264.17 |
| Eyes symptom (Dry eye, etc) | H00H59 | Diseases of the eye and adnexa | 266 | $253.20 |
| Depression | F00F99 | Mental and behavioral disorders | 127 | $247.99 |
| A sense of weariness or fatigue | R00R99 | Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified | 235 | $234.85 |
| Anxiety | F00F99 | Mental and behavioral disorders | 165 | $230.45 |
| Headaches | G00G99 | Diseases of the nervous system | 215 | $143.95 |
| Others | Z00Z99 | Others | 206 | $141.00 |
| Pain in arm and leg joints, lack of mobility | M00M99 | Diseases of the musculoskeletal system and connective tissue | 158 | $136.24 |
| Insomnia | F00F99 | Mental and behavioral disorders | 126 | $128.26 |
| Recurrent diarrhea, constipation | K00K93 | Diseases of the digestive system | 97 | $84.17 |
| Skin disease / Itchiness | L00L99 | Diseases of the skin and subcutaneous tissue | 98 | $77.12 |
| Cold, influenza | J00J99 | Diseases of the respiratory system | 105 | $35.06 |
| Menopausal symptoms | N00N99 | Diseases of the genitourinary system | 70 | $34.28 |
| High blood pressure | I00I99 | Diseases of the circulatory system | 56 | $33.15 |
| Deteriorating hearing | H60H95 | Diseases of the ear and mastoid process | 43 | $31.01 |
| Heart disease | I00I99 | Diseases of the circulatory system | 40 | $28.10 |
| Troubled by allergies | J00J99 | Diseases of the respiratory system | 55 | $23.13 |
| Cancer | C00D48 | Neoplasms | 23 | $19.31 |
| Asthma | J00J99 | Diseases of the respiratory system | 30 | $17.63 |
| Respiratory trouble | J00J99 | Diseases of the respiratory system | 23 | $17.47 |
| Gastroenteritis | K00K93 | Diseases of the digestive system | 36 | $15.70 |
| Diabetes | E00E90 | Endocrine, nutritional, and metabolic diseases | 29 | $13.58 |
| Stomach ulcer, duodenal ulcer | K00K93 | Diseases of the digestive system | 24 | $12.18 |
| Anemia | D50D89 | Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 16 | $11.07 |
| Heartburn | K00K93 | Diseases of the digestive system | 23 | $10.58 |
| Tooth trouble | K00K93 | Diseases of the digestive system | 26 | $10.44 |
| Liver disease | K00K93 | Diseases of the digestive system | 15 | $9.74 |
| Urine-related problems | N00N99 | Diseases of the genitourinary system | 20 | $8.46 |
| Infertility treatment | N00N99 | Diseases of the genitourinary system | 6 | $5.32 |
| Dyslipidemia | E00E90 | Endocrine, nutritional, and metabolic diseases | 16 | $2.15 |
| Hangover | R00R99 | Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | 5 | $0.45 |
| Osteoporosis | M00M99 | Diseases of the musculoskeletal system and connective tissue | 0 | $0.00 |
| Total | 3323 | $3,054.71 |
ICD, International Statistical Classification of Diseases and Related Health Problems.
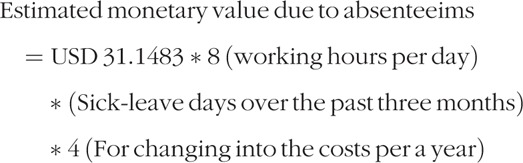
In total costs, the monetary value due to absenteeism was $520 USD per person per year (11%), that due to presenteeism was $3055 USD (64%), medical (outpatient) expenses were $607 USD (13%), pharmaceutical (outpatient) expenses were $357 USD (8%), and medical and pharmaceutical expenses (inpatient) were $201 USD (4%) in Fig. 1.
FIGURE 1.
The $USD costs per person per year of absenteeism, presenteeism, and medical (outpatient), pharmaceutical (outpatient) and medical and pharmaceutical inpatient) expenses, and the proportion in total.
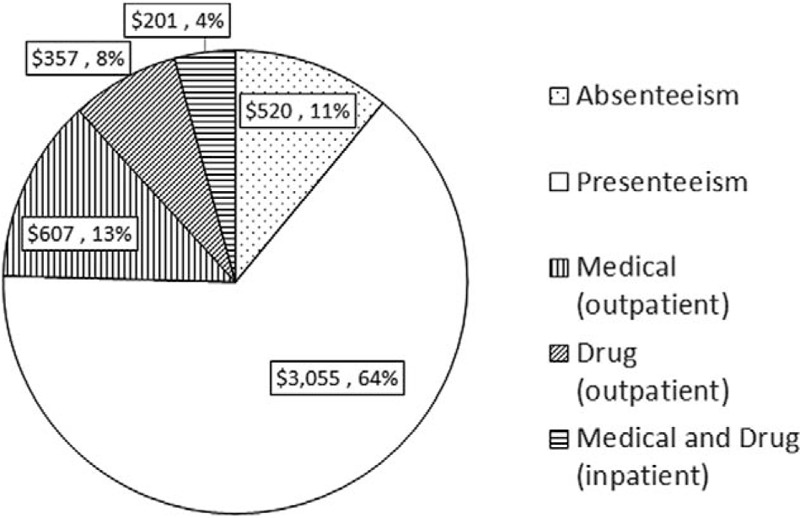
In total health-related costs, the two health conditions with the largest burden were Mental and behavioral disorders, and Diseases of the musculoskeletal system and connective tissue, with a large portion of the cost burden being due to presenteeism, as noted in Fig. 2. In mental and behavioral disorders, costs of presenteeism were $ 948,276 USD per 1000 full-time equivalent per year, medical (outpatient) expenses were $19,569 USD, and medical and pharmaceutical expenses (inpatient) were $1683 USD, and in Diseases of the musculoskeletal system and connective tissue, costs of presenteeism were $ 833,327 USD per 1000 full-time equivalent per year, medical (outpatient) expenses were $43,935 USD, and medical and pharmaceutical expenses (inpatient) were $10,228 USD.
FIGURE 2.
The $USD costs per 1,000 full-time equivalent per year of presenteeism, medical (outpatient), and medical and pharmaceutical (inpatient) expenses classified by International Statistical Classification of Diseases and Related Health Problems version 10 code (ICD 10).
DISCUSSION
We revealed total burden of absenteeism, presenteeism, and medical and pharmaceutical expenses in four pharmaceutical companies in Japan. The monetary value due to presenteeism was a relatively large burden to employers, especially in mental/behavioral and musculoskeletal conditions.
Comparison With the Past Studies
Japanese national survey named Comprehensive Survey of Living Conditions has been conducted every year to research basic subjects of living conditions such as health, medical care, and other factors.16 As for the Large-scale survey 2013, the Health questionnaire covered whole households (234,383 households) in Japan who were randomly sampled in 5440 districts from the National Census in 2005. The survey revealed that the proportion of persons with symptoms was 27.7% in male and 34.5% in female, and that rises with age (16.9% in 20s, 21.4% in 30s, 23.4% in 40s, and 27.1% in 50s for males, 25.8% in 20s, 30.1% in 30s, 32.6% in 40's, and 36.6% in 50s for females) in the Japanese general population. The proportion in our study was almost the same: 24.7% for male and 33.6% for female in working population. Our study also revealed that the top four health conditions are first: Painful neck or stiff shoulders, second: Back pain, third: Insufficient sleep, and fourth: Eye symptom (Dry eye, etc) for male, and first: Painful neck or stiff shoulders, second: Headaches, third: Eye symptom (Dry eye, etc), and fourth: A sense of weariness or fatigue for female. That denoted almost the same tendency of the national survey: top three health conditions was first: back pain, second: stiff shoulders, and third: nasal discharge and congestion for male, and first: stiff shoulders, second: back pain, and third: pain in arm and leg joints for female. However, our study had much persons with eye symptoms and insufficient sleep. That may be related to workers in our study populations spent a significant amount of their working time using computers, with long working hours that could have shortened their sleeping hours.
In regard to the economic impact of loss of performance due to presenteeism, the top five health conditions in our study were painful neck or stiff shoulders, insufficient sleep, back pain, eyes symptom (dry eye, etc), and depression. After we sorted health conditions into ICD10 code, a large part of the burden (38.3%) was caused by “Mental and behavioral disorders” and “Diseases of the musculoskeletal system and connective tissue.” That coincided with the Japanese past study, which concluded the burden of presenteeism of “depression, anxiety, or emotional disorders” and “back or neck disorders” were biggest.13
From the national database,26 estimates of national medical care expenditure per person for all age and sex was $ 3031 USD in 2014, which was composed of 37.4% medical and pharmaceutical expenses (inpatient), 34.3% medical expenses (outpatient), 17.9% pharmaceutical expenses (outpatient), 6.8% dental expenses, and others. All expenditures were increasing with age. Average medical expenses (outpatient) per person per year were $ 292 USD in aged 20 to 24 years, $ 429 USD in 30 to 34 years, $ 556 USD in 40 to 44 years, $ 850 USD in 50 to 54 years, and $ 1314 USD in 60 to 64 years. With our sample, the expenses were $ 607 USD, and were equivalent to the average expenses in 40 to 49 years. Average pharmaceutical expenses (outpatient) per person per year in Japan were $ 127 USD in aged 20 to 24 years, $ 199 USD in 30 to 34 years, $ 274 USD in 40 to 44 years, $ 413 USD in 50 to 54 years, and $ 640 USD in 60 to 64 years. With our sample, the expenses were $ 357 USD, and were equivalent to the average expenses in 45 to 54 years. In contrast, average medical and pharmaceutical expenses (inpatient) per person per year were $ 193 USD in aged 20 to 24 years, $ 328 USD in 30 to 34 years, $ 389 USD in 40 to 44 years, $ 681 USD in 50 to 54 years, $ 1274 USD in 60 to 64 years. With our sample, the expenses were $ 201 USD, and were equivalent to the average expenses in 20 to 29 years old. Lower medical and pharmaceutical expenses of inpatient may have been due to healthy worker effect.27
The past study in the USA revealed that the top 10 health conditions by costs (medical and pharmaceutical expenses, absenteeism and presenteeism) were depression, obesity, arthritis, back/neck pain, anxiety, GERD (gastroesophageal reflux disease), allergy, cancers (other than skin), other chronic pain, and hypertension in descending order.11 It was difficult to compare it to our study because the specific categories of health conditions were somewhat different, but the results were similar, especially related to mental health conditions showing a high burden of total cost—with very high proportion of presenteeism. In our sample of pharmaceutical companies, the mental health status of workers might have affected the intellectual nature of their work, especially among research and development workers as well as in communication with customers. The total cost of musculoskeletal disorders such as back and neck pain was huge in both countries, but the breakdown of the cost was somewhat different. While in USA almost half of the costs was composed of medical expenses, in Japan, almost all the cost was due to presenteeism.
It is notable that the ratio of health-related productivity costs (absenteeism and presenteeism) to medical/pharmaceutical costs is 3 to 1 in this study of Japan employers/employees and is similar to the 2.3 to 1 ratio revealed in the past study of U.S. employers/employees.11
The health risk factor comparison between the USA and Japan reveals some differences, especially among BMI and smoking, as summarized in Table 2.
In fact, the prevalence rates of the top three individual health risk factors, which were high risk in our study, were as follows: smoking (22%), alcohol (20%), and fasting blood glucose (18%)—and those compared with prevalence rates of high risks in smoking (6%), alcohol (12%), and fasting blood glucose (21%) found in the past study.22
One of the major differences between this Japan study and the prior U.S. study on total health-related costs was with obesity. National Health and Nutrition Survey of Japan in 2014 revealed that the proportion whose BMI was more than 25 kg/m2 was 28.8% in males and 21.3% in females.28 In our sample, overweight high risk workers by the Edington health risk criteria (BMI of >27.8 for males and >27.3 for females) was just 8.0%. In spite of the lower proportion of obesity, diabetes mellitus was still one of big issues in Japan. Those who are highly suspected to have diabetes (those who have hemoglobin Alc level of 6.1% or more, or those who answered “to be on medication of diabetes” in a questionnaire) was 15.5% in male and 9.8% in female. Therefore, there should be a high priority on nutrition and exercise interventions for workers in Japan.
Implications to Practice
These data of the total health-related cost burden of health conditions can help employers set priorities on population health management and develop effective workplace health and human capital investment strategies. In Japan, mental health is a critical issue and various measures have been implemented. Absenteeism has been drawing attention in Japan and the guidance for helping workers return to work due to mental health problems was published in 2004.29 Our study revealed that health-related productivity loss for mental health problems was huge, and this fact indicates that occupational health staff should take care not only of sick-leave workers but also of workers with symptoms of depression, anxiety, and sleep. However, the typical countermeasures for sleep disorders (such as insufficient sleep and insomnia) do not adequately address the broader mental/behavioral health disorders such as depression, anxiety substance abuse, and other common mental health conditions. In addition to that, the typical countermeasures to address neck and back pain have been insufficient. To support employers in setting workplace health priorities and strategies, it would be beneficial to analyze the cost-effectiveness and/or the cost benefits of workplace health initiatives from a total (productivity and medical/pharmaceutical) cost perspective. In prior articles, cost estimation tools for occupational health services30 and calculated costs of each occupational health activity in Japanese manufacturing companies were described.31 To compare the effectiveness of workplace health initiatives, assessing an employer's total cost burden of health conditions and health risks would provide the baseline information for a pre-post impact analysis.
Furthermore, this study confirms the importance of occupational health professionals considering these total health-related costs to employers when considering not only the return on investment (ROI) but also the broader value of the investment (VOI)32 in occupational health, safety, and population health management initiatives for employers.
Strengths and Limitations
This is the first study in Japan to reveal total burden of medical and pharmaceutical expenses, and monetary value due to absenteeism and presenteeism by health conditions. Our study has several strengths. First, we used complete medical and pharmaceutical claims by the national health insurance system in Japan, so medical and pharmaceutical expenses were mutually exclusive and collectively exhaustive. Second, we estimated the monetary value due to presenteeism to meet the actual situation. In the calculating formula of productivity loss, we used duration of health problems or symptoms. With recall bias in mind, we asked workers how many days they had experienced their symptom over the past 3 months. Third, our sample size was large (12,350) and the overall response rate was high (61.7%). All workers were in pharmaceutical companies, so this result was easily interpreted.
Our study has several limitations. First, medical and pharmaceutical claims do not contain dental claims. The dental expenses were just 6.8% in total medical care expenditure,26 so total burden was not influenced a great deal by lack of dental expenses. In addition to that, pharmaceutical claims were based on the prescription of doctors, so the expenses of over-the-counter drugs were not included. Second, we conducted self-administer questionnaire just once. Chronic health conditions were not greatly affected; however, seasonal conditions such as allergy to pollen, influenza, and so on depend on the season of the survey. In actual, the survey was conducted in summer, so hay fever and influenza were at a low prevalence rate. This should be considered in interpretation of the result. Third, the absenteeism and presenteeism measure were self-reported with possibility of recall bias. To minimize the influence, we had asked the situation of the past three months. We set 3 months as recall period because we thought 6 months were too long to recall the situation, and 1 month was too short to represent the situation of 1 year. Fourth, the response rate was different among the four companies in the study. The response rate was high in company A (86.5%) and company C (78.6%), whereas it was not as high in company B (32.7%) and company D (33.4%). We described the cause in Methods section. In company B and D, health-minded workers might answer self-administered questionnaire. In order to verify this, we had analyzed health checkup data and compared smoking rate of respondents of questionnaire to that of nonrespondents. In company B, smoking rate of respondents was 21.5%, whereas that of nonrespondents was 23.2% (P = 0.195). In company D, the rate was 27.2% and 24.3% in turn (P = 0.066). Sampling bias appears to have little to no impact on the result. Fifth, those who had been absent themselves from work due to health conditions during the survey period might not have been able to participate in the study survey. However, we set long survey period (about 1 month) to reduce that influence. The four companies involved in the study were all large-scale pharmaceutical companies, so our results may not accurately represent small- and medium-scale companies or other categories of business. Further study would be needed to verify the generalizability.
CONCLUSION
The monetary value due to absenteeism was $520 per person per year (11%), that of presenteeism was $3055 (64%), and medical/pharmaceutical expenses were $1165 (25%) [which included outpatient medical expenses of $607 (13%), outpatient pharmaceutical expenses of $357 (8%), and inpatient medical and pharmaceutical expenses of $201 (4%)]. Two of the highest total cost burdens of chronic illness were mental (behavioral) health conditions and musculoskeletal disorders.
It is notable that the ratio of health-related productivity costs (absenteeism and presenteeism) to medical/pharmaceutical costs is 3 to 1 in this study of employers/employees in Japan and is similar to the 2.3 to 1 ratio revealed in the past study of U.S. employers/employees.11
This study further confirms the importance of considering these total health-related costs to employers when considering not only the ROI but also the broader VOI31 in occupational health, safety, and population health management initiatives for employers.
Footnotes
This study was funded by the Collabo-Health Study Group.
The authors have no competing interests.
REFERENCES
- 1.Organisation for Economic Co-operation and Development. OECD.Stat: Health Expenditure and Financing 2016. Available at: http://stats.oecd.org/index.aspx?DataSetCode=SHA Accessed January 12, 2018. [Google Scholar]
- 2.Partnership for Solutions National Program Office. Chronic Conditions: Making the Case for Ongoing Care. September 2004 Update. Baltimore, MD: Partnership for Solutions, John Hopkins University; 2004. [Google Scholar]
- 3.Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. 2000; 54:502–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dew K, Keefe V, Small K. ‘Choosing’ to work when sick: workplace presenteeism. 2005; 60:2273–2282. [DOI] [PubMed] [Google Scholar]
- 5.Loeppke R, Hymel P. Health and productivity enhancement, Chapter 16. In: Moser R, Jr, editor. Effective Management of Health and Safety Programs: a Practical Guide, 3rd Edition. Beverly Farm, MA; 2008; pp. 265–290. [Google Scholar]
- 6.Hymel P, Loeppke R, Baase C, et al. Establishing a research agenda in health and productivity. 2004; 46:518–520. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Ames M, Hymel PA, et al. Using the WHO Health and Work Performance Questionnaire to evaluate the indirect workplace costs of illness. 2004; 46:S23–S37. [DOI] [PubMed] [Google Scholar]
- 8.Loeppke R, Hymel PA, Lofland JH, et al. Health-related workplace productivity measurement: general and migraine specific recommendations from the ACOEM Expert Panel. 2003; 45:349–359. [DOI] [PubMed] [Google Scholar]
- 9.Johns G. Presenteeism in the workplace: a review and research agenda. 2009; 31:519–542. [Google Scholar]
- 10.Brady W, Bass J, Moser R, Anstadt GW, Loeppke R, Leopold R. Total corporate health costs. 1997; 39:224–231. [DOI] [PubMed] [Google Scholar]
- 11.Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: a multiemployer study. 2009; 51:411–428. [DOI] [PubMed] [Google Scholar]
- 12.Loeppke R, Taitel M, Richling D, et al. Health and productivity as a business strategy. 2007; 49:712–721. [DOI] [PubMed] [Google Scholar]
- 13.Wada K, Arakida M, Watanabe R, Negishi M, Sato J, Tsutsumi A. The economic impact of loss of performance due to absenteeism and presenteeism caused by depressive symptoms and comorbid health conditions among Japanese workers. 2013; 51:482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wada K, Moriyama M, Narai R, et al. The effect of chronic health conditions on work performance in Japanese companies. 2007; 49:103–109. [DOI] [PubMed] [Google Scholar]
- 15.Ikegami N, Yoo BK, Hashimoto H, et al. Japanese universal health coverage: evolution, achievements, and challenges. 2011; 378:1106–1115. [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Health, Labour and Welfare, Japan. Comprehensive Survey of Living Conditions. Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan; 2013. [Google Scholar]
- 17.Hoeijenbos M, Bekkering T, Lamers L, Hendriks E, van Tulder M, Koopmanschap M. Cost-effectiveness of an active implementation strategy for the Dutch physiotherapy guideline for low back pain. 2005; 75:85–98. [DOI] [PubMed] [Google Scholar]
- 18.Brouwer WB, Koopmanschap MA, Rutten FF. Productivity losses without absence: measurement validation and empirical evidence. 1999; 48:13–27. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health, Labour and Welfare, Japan. Basic Survey on Wage Structure. 2013; Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan, Available at: http://www.mhlw.go.jp/toukei/list/chinginkouzou.html. Accessed January 12, 2018. [Google Scholar]
- 20.Edington DW. Emerging research: a view from one research center. 2001; 15:341–349. [DOI] [PubMed] [Google Scholar]
- 21.Edington DW. Zero Trends: Health as a Serious Economic Strategy. Ann Arbor, MI: Health Management Research Center, University of Michigan; 2009. [Google Scholar]
- 22.Loeppke R, Edington D, Bender J, Reynolds A. The association of technology in a workplace wellness program with health risk factor reduction. 2013; 55:259–264. [DOI] [PubMed] [Google Scholar]
- 23.Loeppke R, Edington DW, Beg S. Impact of the prevention plan on employee health risk reduction. 2010; 13:275–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ministry of Health, Labour and Welfare, Japan. Industrial Safety and Health Act, Article 66. Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan; 1972. [Google Scholar]
- 25.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. 1972; 18:499–502. [PubMed] [Google Scholar]
- 26.Ministry of Health, Labour and Welfare, Japan. Estimates of National Medical Care Expenditure. Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan; 2014. [Google Scholar]
- 27.Shah D. Healthy worker effect phenomenon. 2009; 13:77–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health, Labour and Welfare, Japan. National Health and Nutrition Survey. Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan; 2014. [Google Scholar]
- 29.Ministry of Health, Labour and Welfare, Japan. ‘The guidance for helping workers return to work due to mental health problems’ (in Japanese). Tokyo, Japan: Ministry of Health, Labour and Welfare, Japan; 2004. Available at: http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000186066.html Accessed January 12, 2018. [Google Scholar]
- 30.Nagata T, Mori K, Aratake Y, et al. Development of cost estimation tools for total occupational safety and health activities and occupational health services: cost estimation from a corporate perspective. 2014; 56:215–224. [DOI] [PubMed] [Google Scholar]
- 31.Nagata T, Mori K, Aratake Y, et al. Establishment of reference costs for occupational health services and implementation of cost management in Japanese manufacturing companies. 2016; 58:323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loeppke R. The value of health and the power of prevention. 2008; 1:95–108. [Google Scholar]


