Abstract
Background
The use of venovenous bypass in liver transplantation has declined over time. Few studies have examined the impact of surgical approach in cases performed exclusively without venovenous bypass. We hypothesized that advances in liver transplant anesthesia and perioperative care have minimized the importance of surgical approach in the modern era.
Methods
Deceased donor liver transplants at the University of Toronto from 2000 to 2015 were reviewed, all performed without venovenous bypass. First, an unadjusted analysis was performed comparing perioperative outcomes and graft/patient survival for 3 different liver transplant techniques (caval interposition, piggyback, side-to-side cavo-cavostomy). Second, a propensity-matched analysis was performed comparing caval interposition to caval-preserving techniques.
Results
One thousand two hundred thirty-three liver transplants were included in the study. On unadjusted analysis, blood loss, transfusion requirement, postoperative complications, and graft/patient survival were equivalent for the 3 different techniques. To account for possible confounding patient variables, propensity matching was performed. Analysis of the propensity-matched cohorts also demonstrated similar outcomes for caval interposition versus caval-preserving approaches.
Conclusions
In the modern era at centers with a multidisciplinary team, the importance of specific liver transplant technique is minimized. Full or partial cross-clamping of the inferior vena cava is feasible without the use of venovenous bypass.
As liver transplantation (LT) was being developed, it was hypothesized that venovenous bypass (VVBP) would improve intraoperative stability during the anhepatic phase of the operation and lead to improved perioperative outcomes.1 As such, VVBP was routinely used at most centers. In the 1990s, however, increased recognition of complications from VVBP and the emergence of the caval-preserving piggyback (PB) implant technique contributed to a decline in the use of VVBP.2-20 In 1998, Chari and colleagues21 published a survey of 50 major North American transplant centers which demonstrated that 42% of centers routinely used VVBP, a significant reduction from 91% in 1987. Since that report, ongoing refinements in intraoperative management have likely led to even further reductions in the use of VVBP, although a contemporary assessment of VVBP practice patterns has not been performed. In the current era, particularly at centers with experienced liver transplant anesthesiologists, LT without VVBP is achievable both with partial or complete cross-clamping of the inferior vena cava (IVC). However, very few studies have examined the impact of surgical approach on outcomes of LT performed without VVBP.
At the University of Toronto, we began performing LT without VVBP in 1993, using a caval interposition (CI) technique. In 1993, 43 of 67 (64%) adult LTs were performed without VVBP. By 1996, 72 (93%) of 77 of adult LTs were performed by CI without VVBP. Since 2000, we have exclusively performed LT without VVBP, and implantation technique is driven purely by surgeon preference. The majority of cases have been performed with the classic CI technique, necessitating full cross-clamp of the IVC. Less frequently, we have used a PB technique in which the recipient IVC is preserved and caval anastomosis performed between donor suprahepatic cava and the confluence of the recipient left and middle hepatic veins. More recently, we have incorporated a third approach, using a side-to-side (SS) caval anastomosis after backtable resection of the caudate lobe.
The purpose of this study is to compare the safety and efficacy of 3 different liver transplant techniques performed without VVBP. In particular, we asked whether surgical approach affects the intraoperative and postoperative course at a high-volume center where patients are managed by a multidisciplinary transplant team.
MATERIALS AND METHODS
The study group consisted of deceased donor LTs performed from 2000 to 2015 at the Toronto General Hospital. Re-transplants and split liver transplants were excluded from the analysis given their added technical complexity. For the SS technique, backtable preparation included mobilization and resection of the caudate lobe with a linear cutting stapler (Figure 1).
FIGURE 1.

Backtable resection of the caudate lobe with a linear cutting stapler.
The following clinical and demographic data were retrospectively extracted from a prospectively collected electronic transplant database (Organ Transplant Tracking Record: Transplant Care Platform 6, Organ Transplant Tracking Record Chronic Care Solutions, Omaha, NE):
(1) Recipient characteristics: age, sex, body mass index (BMI), etiology of liver disease (overlap may be present), acuity at time of transplant (home, inpatient, intensive care unit [ICU]), laboratory values, and model for end-stage liver disease (MELD) score.
(2) Donor characteristics: age, gender, BMI, and graft type.
(3) Operative characteristics: use of antibody induction, cold and warm ischemia times, surgery duration, estimated blood loss, transfusion requirements, intraoperative vasopressor use, and disposition from the OR.
(4) Postoperative outcomes: renal function, liver function tests, length of post-transplant hospitalization, postoperative complications, 90-day graft loss, 90-day patient death, and graft and patient survival.
Unadjusted Analysis: Comparison of 3 Liver Transplant Techniques
Comparisons were made in unadjusted fashion for the 3 surgical techniques (CI, PB, and SS). For continuous variables, data are reported as mean (standard deviation). Categorical variables are reported as number (percentage). Continuous variables were compared using the Student t test or Mann-Whitney test as dictated by the data distribution. Categorical variables were compared using χ2 or Fischer exact test. Survival analyses were performed using Kaplan-Meier methodology, and comparisons between implant techniques were made using the log-rank test. Graft survival was calculated in uncensored fashion, with failure events including death with a functioning graft and re-transplantation.
Propensity Matched Analysis Comparing CI to Caval-preserving Techniques
To account for possible confounding patient variables, we subsequently performed a propensity score-matched analysis to compare CI to caval-preserving techniques. For this analysis, the PB and SS techniques were combined into a single caval-preserving cohort. A propensity score was generated for each case based on the following recipient variables: recipient age, MELD score, and recipient acuity (home, inpatient, ICU). We chose to use only recipient factors in constructing the propensity match because in centers that use both techniques, recipient status is the primary determinant of which technique is used. A 5:1 nearest-neighbor match (caliper of 0.25) was performed to generate matched cohorts. Perioperative outcomes and graft/patient survival were then compared for CI versus caval preserving implant techniques.
RESULTS
Unadjusted Analysis
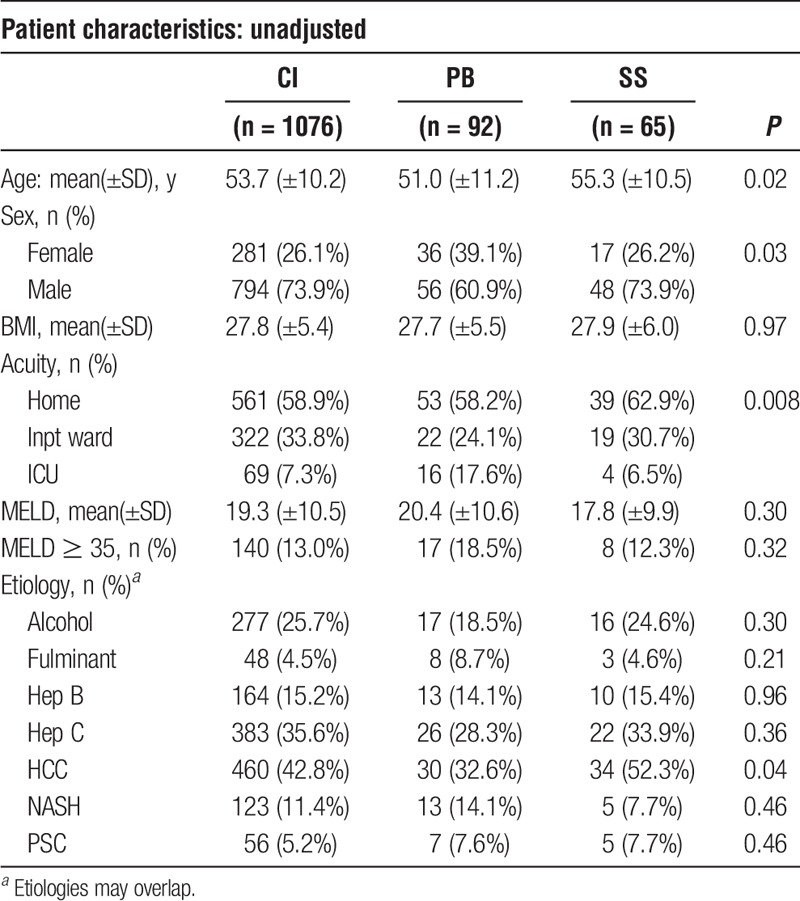
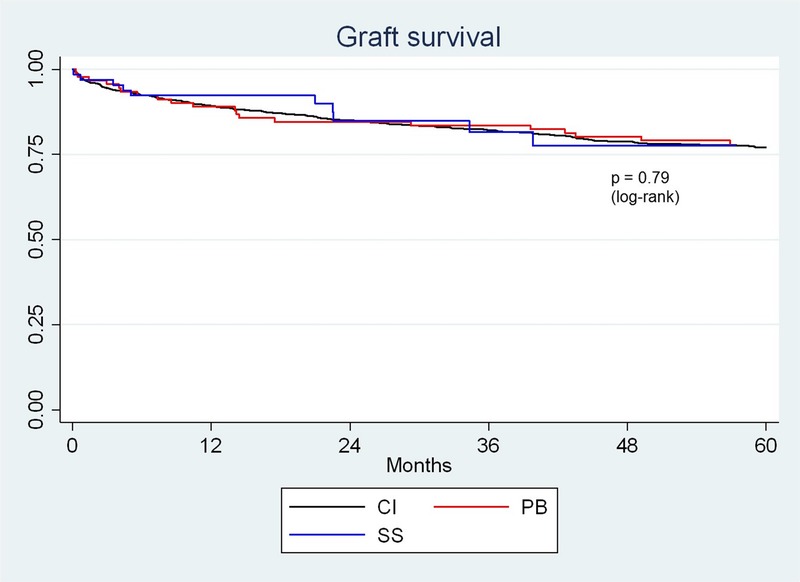
Recipient Characteristics
Recipient characteristics are displayed in Table 1. Recipient age was slightly younger in the PB group compared with the CI and SS groups. There was also a slight preponderance of female patients in the PB group compared with the other 2 groups. Body mass index was similar among the groups. There appeared to be differences among groups with regard to patient acuity, based on patient location before transplant. For example, in the PB group, 17.6% of patients were in the ICU before transplant, compared with only 7.3% and 6.5% in the CI and SS groups, respectively (P = 0.008). However, mean MELD score and the proportion of patients with MELD scores of 35 or greater were similar among groups. The etiology of end-stage liver disease was similar among groups, although there was a higher incidence of hepatocellular carcinoma (HCC) in the SS group compared with the CI and PB groups, respectively (52.3% vs. 42.8% vs. 32.6%, P = 0.04).
TABLE 1.
Unadjusted analysis: recipient characteristics
Donor Characteristics
There was a similar proportion of grafts donated after cardiac death (DCD) in each group (Table 2). Donor sex was similar among CI, PB, and SS groups (59% male vs. 49% male vs. 49% male, P = 0.07). Donor age was greater in the SS group compared with the CI and PB groups (55.5 ± 14.8 vs. 46.9 ± 17.4 vs. 48.2 ± 17.5, P = 0.0005). Donor BMI was also slightly higher in the SS group compared with the CI and PB groups (27.4 ± 5.2 vs. 26.4 ± 5.1 vs. 25.3 ± 5.2, P = 0.04).
TABLE 2.
Unadjusted analysis: operative characteristics
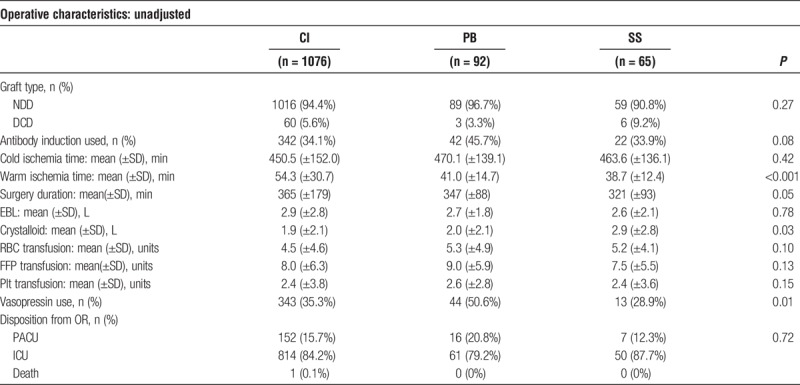
Operative Characteristics
Operative characteristics are displayed in Table 2. The use of induction immunosuppression was similar among groups. Cold ischemic time was similar among groups, but warm ischemic time was significantly longer in the CI group compared with the PB and SS groups, respectively (54.3 min ± 30.7 vs. 41.0 min ± 14.7 vs. 38.7 min ± 12.4, P < 0.001). The operative time was significantly shorter in the SS group compared with the CI and PB groups, respectively (321 ± 93 minutes vs. 365 ± 179 minutes vs. 347 ± 88 minutes, P = 0.05). Estimated blood loss was similar among the groups. There was increased administration of crystalloid in the SS group compared with the CI and PB groups, respectively (2.9 L ± 2.8 vs. 1.9 L ± 2.1 vs. 2.0 L ± 2.1, P = 0.03). Transfusion of red blood cells (RBCs), fresh frozen plasma (FFP), and platelets were similar among the groups. There was significantly less requirement for intraoperative vasopressor agents in the SS group compared with the CI and PB groups, respectively (28.9% vs. 35.3% vs. 50.6%, P = 0.01). The proportion of patients “fast-tracked” postoperatively (extubated and recovered in PACU/stepdown) was similar among groups.
Postoperative Outcomes
Postoperative outcomes are displayed in Table 3. There was a significant reduction in the rise in creatinine on postoperative day 1 in the PB group compared to the CI and SS groups, respectively (2.8% ± 37.0% vs. 13.2% ± 34.8% vs. 9.3% ± 38.7%, P = 0.0005). However, peak creatinine in the first 48 hours was similar among groups. Peak aspartate aminotransferase (AST), alanine aminotransferase (ALT), and internationalized normalized ration (INR) were all similar among groups. Bilirubin on day 7 was also similar among groups. There was an increased ICU and postoperative length of stay in the PB group compared with the other 2 groups. Rates of graft failure (90 days), patient death (90 days), and severe complications (Dindo-Clavien score ≥ 3B) were all similar among groups.
TABLE 3.
Unadjusted analysis: postoperative outcomes
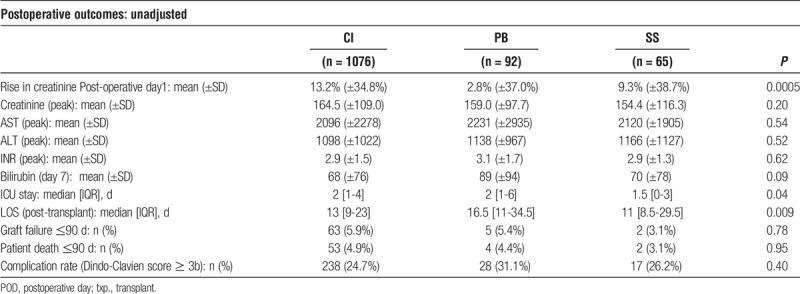
Graft and Patient Survivals
Graft survival is displayed in Figure 2. There was no difference in graft survival among groups (P = 0.79, log-rank). Graft survival at 1 year for CI, PB, and SS groups was 89.3%, 89.0%, and 92.3%, respectively. Graft survival at 5 years for CI, PB, and SS groups was 77.1%, 78.0%, and 77.5%, respectively. Patient survival is displayed in Figure 3. There was no difference in patient survival among groups (P = 0.64, log-rank). Patient survival at 1 year for CI, PB, and SS groups was 90.5%, 90.2%, and 92.3%, respectively. Patient survival at 5 years for CI, PB, and SS groups was 78.2%, 80.4%, and 81.6%, respectively.
FIGURE 2.
Unadjusted analysis: graft survival.
FIGURE 3.
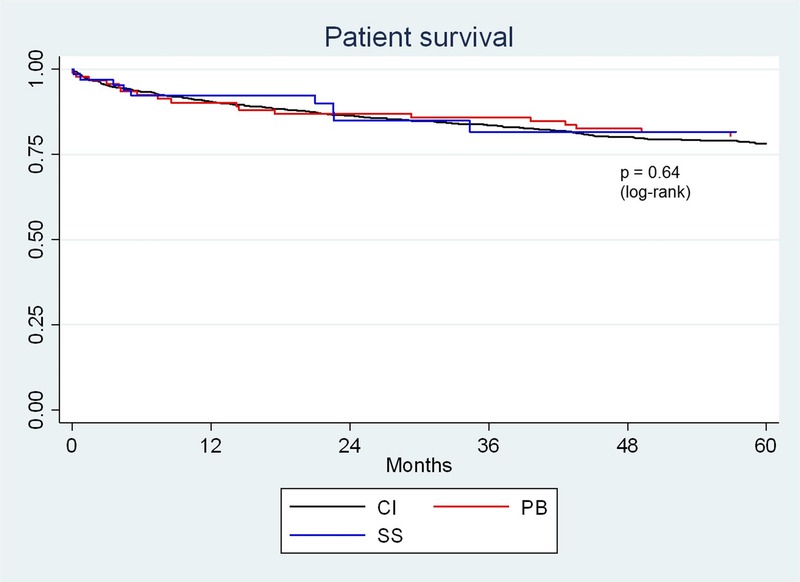
Unadjusted analysis: patient survival.
Propensity Matched Cohort Analysis
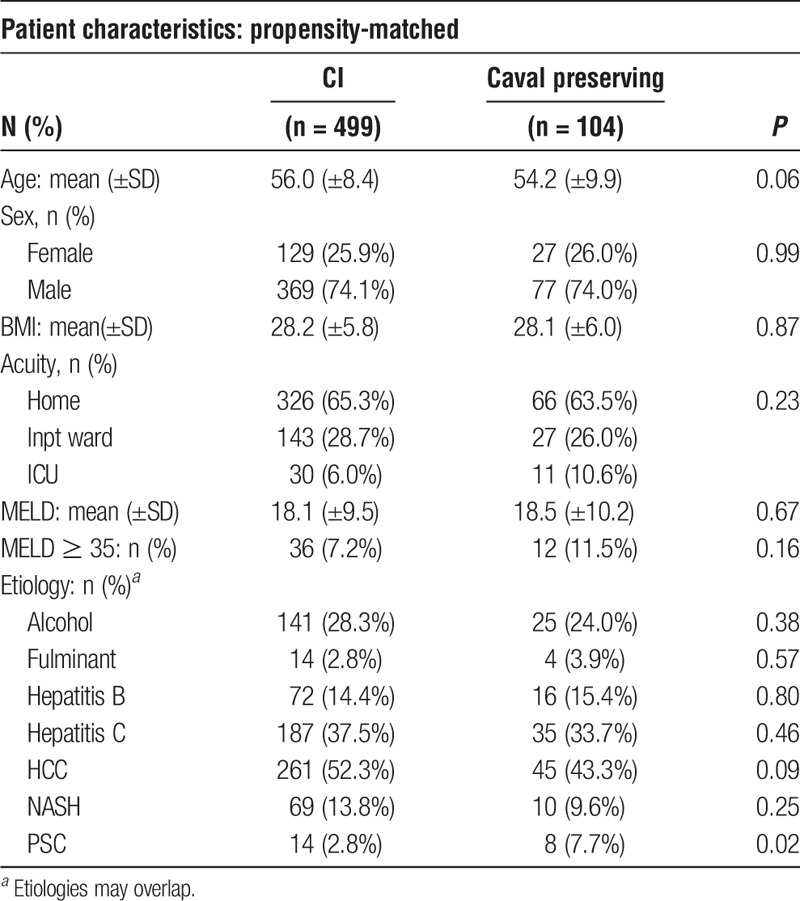
Recipient Characteristics
After propensity-score matching, patients were well balanced between the CI and caval sparing cohorts (Table 4). There were no significant differences in age, sex, BMI, patient acuity, or MELD score between cohorts.
TABLE 4.
Propensity-matched analysis: recipient characteristics
Donor Characteristics
There was a similar proportion of grafts donated after cardiac death (DCD) in each cohort (Table 5). Donor sex was similar between CI and caval preserving cohorts (61.2% male vs. 51.5% male, P = 0.07). Donor age was slightly younger in the CI cohort compared with the caval preserving cohort (47.7 ± 17.5 vs. 51.5 ± 17.4, P = 0.04). Donor BMI was similar between cohorts (26.5 ± 5.0 vs. 26.1 ± 5.2, P = 0.55).
TABLE 5.
Propensity-matched analysis: operative characteristics
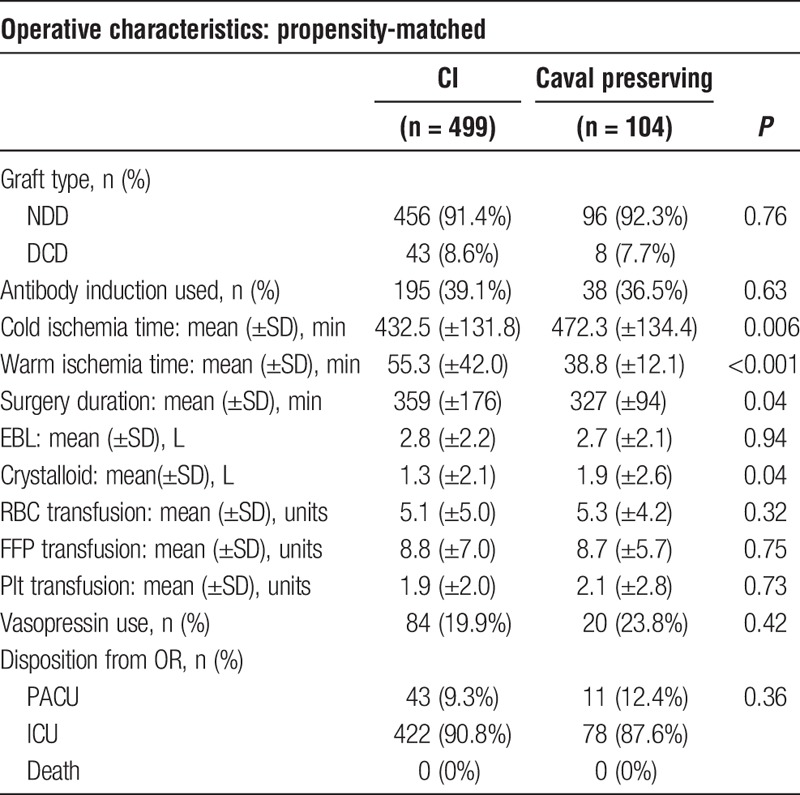
Operative Characteristics
Operative characteristics for the propensity-matched cohorts are displayed in Table 5. The use of induction immunosuppression was similar. Cold ischemic time was slightly shorter in the CI cohort (432.5 ± 131.8 minutes vs. 472.3 ± 134.4 minutes, P = 0.006). As expected, warm ischemic time was significantly longer in the CI cohort compared with the caval preserving cohort, owing to an additional caval anastomosis (55.3 ± 42.0 minutes vs. 38.8 ± 12.1 minutes, P < 0.001). The operative time was also significantly longer in the CI cohort (359 ± 176 minutes vs. 327 ± 94 minutes, P = 0.04). Estimated blood loss, blood product transfusion, and requirement for intraoperative vasopressor agents were similar between cohorts. The proportion of patients “fast-tracked” postoperatively (extubated and recovered in PACU/stepdown) was also similar between cohorts.
Postoperative Outcomes
Postoperative outcomes are displayed in Table 6. There was a greater rise in creatinine on postoperative day 1 for the CI cohort compared with the caval preserving cohort (14.3% ± 34.9% vs. 7.3% ± 41.3%, P = 0.003). However, this effect appeared to be transient, as peak creatinine in the first 48 hours was similar between cohorts. Peak AST, ALT, INR, and day 7 bilirubin were all similar between cohorts. Length of ICU stay and posttransplant length of stay were similar between groups. Rates of graft failure (90 days), patient death (90 days), and severe complications (Dindo-Clavien score ≥ 3B) were all similar between groups.
TABLE 6.
Propensity-matched analysis: postoperative outcomes
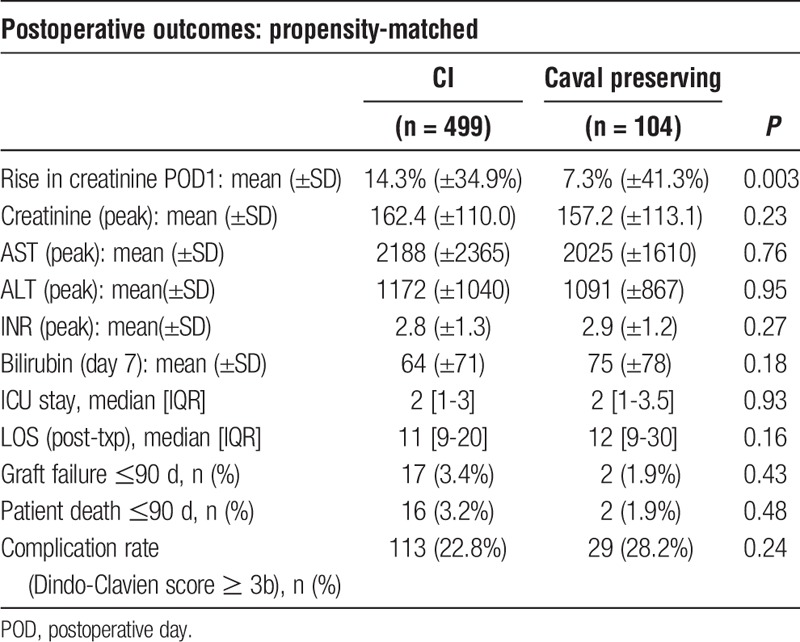
Graft and Patient Survivals
Graft survival is displayed in Figure 4. There was no difference in graft survival between cohorts (P = 0.34, log-rank). Graft survival at 1 year for the CI cohort was 91.1% versus 92.2% for the caval preserving cohort. Graft survival at 5 years for the CI cohort was 79.4% versus 82.0% for the caval preserving cohort. Patient survival is displayed in Figure 5. There was no difference in patient survival between cohorts (P = 0.24, log-rank). Patient survival at 1 year for the CI cohort was 91.7% versus 92.3% for the caval preserving cohort. Patient survival at 5 years for the CI cohort was 79.3% versus 83.8% for the caval preserving cohort.
FIGURE 4.
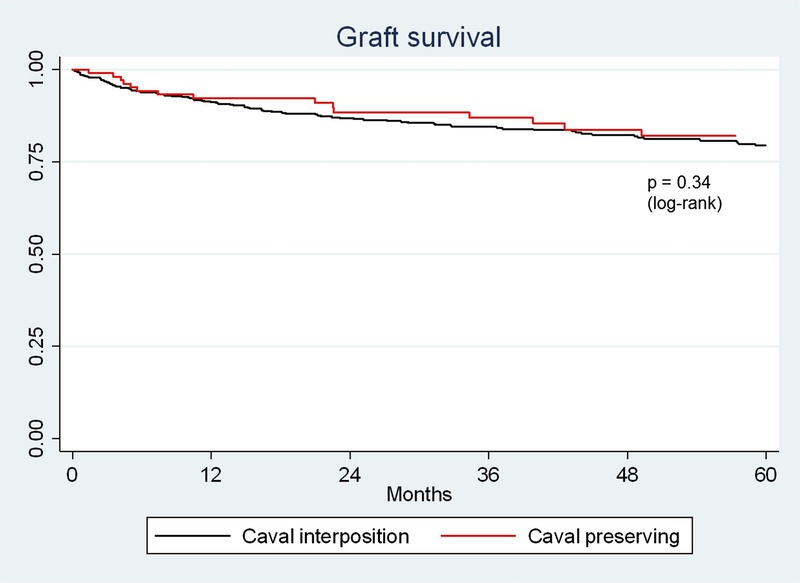
Propensity-matched analysis: graft survival.
FIGURE 5.
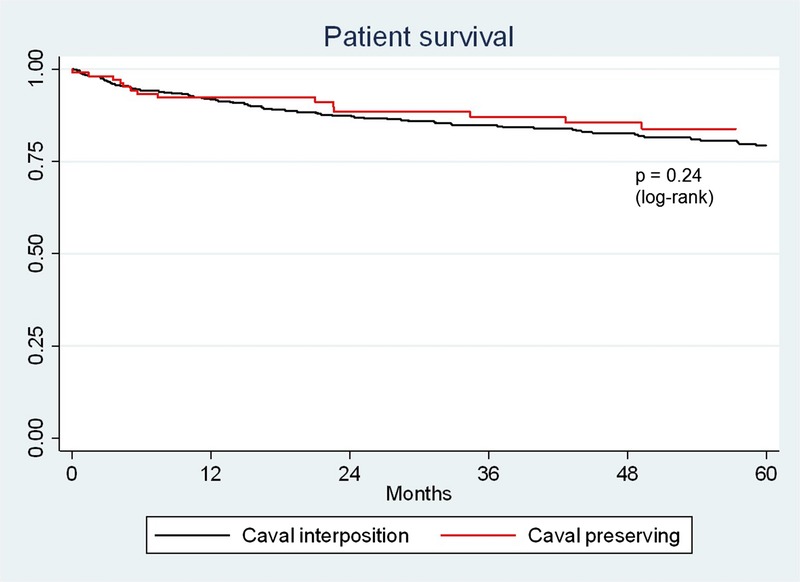
Propensity-matched analysis: patient survival.
DISCUSSION
Historically, the choice of surgical technique and use of VVBP in LT were closely linked. Several studies from the late 1990s and early 2000s suggested superiority of the PB technique without VVBP compared with the classic CI technique with VVBP.2,6,7 However, very few studies have analyzed the effect of surgical techniques when LT is performed exclusively without VVBP.22 Thus, the purpose of the present study was to compare 3 different liver transplant techniques used exclusively without VVBP. We hypothesized that the impact of specific surgical technique would be relatively minimal at an experienced center with a dedicated multidisciplinary LT team. This study represents one of the largest series of LT performed without VVBP in the literature, and to our knowledge includes the largest series of transplants performed by CI without VVBP.
The unadjusted analysis of the 3 implant techniques did not demonstrate any clear trends in favor of a particular technique. Blood loss, transfusion requirements, post-operative complication rates, and graft/patient survival were all similar. However, we observed some potentially confounding differences in patient characteristics (age, gender, and patient acuity). To account for these potential confounders, we performed a propensity-matched analysis based on patient age, MELD, and acuity. Matched cohorts were generated and comparisons then made by surgical approach (CI versus caval preserving).
After propensity score matching, patient cohorts were well balanced. With respect to the effect of surgical approach, there were some notable differences observed between cohorts, but again, no pattern to suggest a clear advantage. For example, there was a longer warm ischemic time and operative time for the CI technique compared with caval preservation, but no difference in blood loss, transfusion requirement, or need for vasopressor agents. Caval preservation appeared to have a transient benefit in terms of renal function (reduced rise in creatinine on postoperative day 1), but this benefit did not manifest in a reduction in peak creatinine. Postoperative complication rate, ICU stay, posttransplant length of stay, and graft/patient survival were also similar between matched cohorts.
There are limitations of this study that must be acknowledged. First, this is a retrospective, single-institution study and is thus subject to the biases associated with our practice environment. In particular, differences in patient demographics and organ availability in Canada have facilitated transplantation at a lower average MELD score than many centers in the United States and Europe. This has contributed to our center's ability to eliminate the use of VVBP, which may not be achievable in other settings with higher patient acuity. Another limitation of our study is the relatively small sample size for the caval-preserving techniques relative to CI, which is the dominant technique in Toronto. While most clinically relevant outcomes appear to be similar, our study may be underpowered to detect small differences between groups.
In conclusion, this report highlights a substantial experience with LT performed exclusively without VVBP, including the largest series of CI done in this fashion. Because of the predominance of the CI technique at our center, surgical and anesthesia teams have become accustomed to routinely managing the hemodynamic alterations during this period. In such an environment, both CI and caval-preserving approaches appear to be similarly safe and effective, and the importance of specific surgical technique is minimized even without VVBP.
Footnotes
Published online 24 April, 2018.
The authors declare no funding or conflicts of interest.
A.B., N.G., M.D., D.A., M.C., A.G., P.G., D.G., G.S., M.S., S.M., I.M. participated in the research design. A.B., J.L., M.M., I.M. participated in the performance of research. A.B., M.M., I.M. participated in the data analysis. A.B. participated in the drafting of the article. N.G., M.D., D.A., M.C., A.G., P.G., D.G., G.S., M.S., S.M., I.M. participated in the critical review.
REFERENCES
- 1.Shaw BW, Jr, Martin DJ, Marquez JM, et al. Venous bypass in clinical liver transplantation. . 1984;200:524–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jovine E, Mazziotti A, Grazi GL, et al. Piggy-back versus conventional technique in liver transplantation: report of a randomized trial. . 1997;10:109–112. [DOI] [PubMed] [Google Scholar]
- 3.Navarro F, Le Moine MC, Fabre JM, et al. Specific vascular complications of orthotopic liver transplantation with preservation of the retrohepatic vena cava: review of 1361 cases. . 1999;68:646–650. [DOI] [PubMed] [Google Scholar]
- 4.Parrilla P, Sanchez-Bueno F, Figueras J, et al. Analysis of the complications of the piggy-back technique in 1,112 liver transplants. . 1999;67:1214–1217. [DOI] [PubMed] [Google Scholar]
- 5.Gerber DA, Passannante A, Zacks S, et al. Modified piggyback technique for adult orthotopic liver transplantation. . 2000;191:585–589. [DOI] [PubMed] [Google Scholar]
- 6.Reddy KS, Johnston TD, Putnam LA, et al. Piggyback technique and selective use of veno-venous bypass in adult orthotopic liver transplantation. . 2000;14:370–374. [DOI] [PubMed] [Google Scholar]
- 7.Hosein Shokouh-Amiri M, Osama Gaber A, Bagous WA, et al. Choice of surgical technique influences perioperative outcomes in liver transplantation. . 2000;231:814–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belghiti J, Ettorre GM, Durand F, et al. Feasibility and limits of caval-flow preservation during liver transplantation. . 2001;7:983–987. [DOI] [PubMed] [Google Scholar]
- 9.Moreno-Gonzalez E, Meneu-Diaz JG, Fundora Y, et al. Advantages of the piggy back technique on intraoperative transfusion, fluid compsumption, and vasoactive drugs requirements in liver transplantation: a comparative study. . 2003;35:1918–1919. [DOI] [PubMed] [Google Scholar]
- 10.Miyamoto S, Polak WG, Geuken E, et al. Liver transplantation with preservation of the inferior vena cava. A comparison of conventional and piggyback techniques in adults. . 2004;18:686–693. [DOI] [PubMed] [Google Scholar]
- 11.Nishida S, Nakamura N, Vaidya A, et al. Piggyback technique in adult orthotopic liver transplantation: an analysis of 1067 liver transplants at a single center. . 2006;8:182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan S, Silva MA, Tan YM, et al. Conventional versus piggyback technique of caval implantation; without extra-corporeal veno-venous bypass. A comparative study. . 2006;19:795–801. [DOI] [PubMed] [Google Scholar]
- 13.Mangus RS, Fridell JA, Vianna RM, et al. Use of the piggyback hepatectomy technique in liver transplant recipients with hepatocellular carcinoma. . 2008;85:1496–1499. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann K, Weigand MA, Hillebrand N, et al. Is veno-venous bypass still needed during liver transplantation? A review of the literature. . 2009;23:1–8. [DOI] [PubMed] [Google Scholar]
- 15.Sakai T, Matsusaki T, Marsh JW, et al. Comparison of surgical methods in liver transplantation: retrohepatic caval resection with venovenous bypass (VVB) versus piggyback (PB) with VVB versus PB without VVB. . 2010;23:1247–1258. [DOI] [PubMed] [Google Scholar]
- 16.Lai Q, Nudo F, Molinaro A, et al. Does caval reconstruction technique affect early graft function after liver transplantation? A preliminary analysis. . 2011;43:1103–1106. [DOI] [PubMed] [Google Scholar]
- 17.Mehrabi A, Mood ZA, Fonouni H, et al. A single-center experience of 500 liver transplants using the modified piggyback technique by Belghiti. . 2009;15:466–474. [DOI] [PubMed] [Google Scholar]
- 18.Gurusamy KS, Koti R, Pamecha V, et al. Veno-venous bypass versus none for liver transplantation. . 2011:CD007712. [DOI] [PubMed] [Google Scholar]
- 19.Levi DM, Pararas N, Tzakis AG, et al. Liver transplantation with preservation of the inferior vena cava: lessons learned through 2,000 cases. . 2012;214:691–698; discussion 698–699. [DOI] [PubMed] [Google Scholar]
- 20.Brescia MD, Massarollo PC, Imakuma ES, et al. Prospective randomized trial comparing hepatic venous outflow and renal function after conventional versus piggyback liver transplantation. . 2015;10:e0129923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chari RS, Gan TJ, Robertson KM, et al. Venovenous bypass in adult orthotopic liver transplantation: routine or selective use? . 1998;186:683–690. [DOI] [PubMed] [Google Scholar]
- 22.Vieira de Melo PS, Miranda LE, Batista LL, et al. Orthotopic liver transplantation without venovenous bypass using the conventional and piggyback techniques. . 2011;43:1327–1333. [DOI] [PubMed] [Google Scholar]


