Abstract
Rationale:
Every year, ∼40,000 people suffer burn-related injuries in the United States. Despite recent advances, the odds of dying from exposure to fire, flames, or smoke are one in ∼1500. Smoke inhalation causes injury to the airways via a complex physiological process, and the treatment is mainly supportive. Many recent interventions aim to decrease the formation of fibrin casts, the main cause of airway damage in these patients. Among these, treatment with a combination of nebulized heparin and N-acetylcysteine (NAC) has shown benefit.
Patient concerns:
We describe the case of a 58-year-old man who presented after smoke inhalation during a fire. Soot was found in the nostrils when he was admitted to our hospital, and after he began coughing up carbonaceous material, he was electively intubated and placed on volume assist control ventilation.
Diagnosis:
Bronchoscopy on the first day of intensive care confirmed the injury from smoke inhalation and revealed mucosal edema and soot involving the tracheobronchial tree.
Interventions and outcomes:
Inhaled unfractionated heparin of 10,000 IU in 3 mL of 0.9% normal saline alternating every 2 hours with 3 mL of 20% NAC was started 48 hours after admission and continued for 7 days. Bronchoscopy on the fifth day of intensive care showed significant improvement in airway edema and a resolution of soot.
Lessons:
On the basis of our experience with this case and limited literature, we posit that nebulized heparin and NAC may be of benefit in patients with inhalational smoke-induced lung injury and mild-to-severe lung injury scores.
Keywords: carbon monoxide poisoning, N-acetylcysteine, nebulized heparin, smoke inhalational injury
1. Introduction
Smoke inhalation injury is a major cause of morbidity and mortality in burn patients. Current therapies are mostly supportive, and there is no consensus on standardized management. Because fibrin deposition and the resultant cast formation are pivotal to inhalation lung injuries, various therapies have been used in an attempt to reduce fibrin deposition. One of the therapies that has gained attention is the use of nebulized heparin and N-acetylcysteine (NAC) within 48 hours of injury.[1]
Nebulized heparin exerts a local anticoagulant effect in the lungs without significant systemic effects and can mitigate pulmonary coagulopathy in critically ill patients. NAC helps with mucolysis and decreases inflammation.[2,3] Here, we report the use of nebulized heparin with NAC for the management of a patient with a smoke inhalation injury. In addition to describing the clinical presentation, pathophysiology, and management of this condition, we review the literature involving the use of this treatment.
The publication of a case report is exempted from approval by the Institutional Review Board at Bronx Lebanon Hospital Center. However, patient's consent was obtained for the publication of this manuscript.
2. Case report
A 58-year-old man was admitted to the intensive care unit after accidental smoke inhalation during a fire that occurred at his home. He was trapped in his apartment for an unknown duration and was brought to our emergency room by emergency medical services. His medical comorbidities included hypertension treated with lisinopril and diet-controlled diabetes mellitus. He denied any cigarette smoking or the use of alcohol or illegal drugs.
On examination, he was afebrile, normotensive, and tachypneic with a respiratory rate of 26 breaths/min and a body mass index of 34 kg/m2. An examination of his head and neck revealed bilateral conjunctivitis, soot in the nostrils, and pharyngeal erythema and edema. Bilateral rhonchi and wheezing were heard during the respiratory examination. Cardiovascular and abdominal examinations, as well as an examination of the extremities and skin, were unremarkable. He was coughing blackish sputum with a soot-like material, and he was electively intubated for the protection of his airways. On admission, his carboxyhemoglobin level was 13% and lung injury score (LIS) was 1.25 (alveolar consolidation in 2 quadrants; PO2/FIO2, 245; positive end-expiratory pressure, 8; and respiratory compliance, 60–79 mL/cm H2O). He was placed on volume assist control ventilation with a tidal volume of 7 mL/kg ideal body weight; the initial peak pressure was 45 cm H2O and plateau pressure was 38 cm H2O. Other laboratory parameters, including blood cell counts and renal, hepatic, and acid-base determinations, were normal. Urine toxicology was negative.
A chest roentgenogram revealed patchy infiltrates in the lower lobes and possible infiltrates in the upper lobes of the lungs. The endotracheal tube (ETT) was high in the trachea and required repositioning (Fig. 1). A bronchoscopy was performed with a flexible fiberoptic bronchoscope (FFB) on the first day of admission, and airway damage was graded as 2 using bronchoscopic mucosal scoring.[4] The bronchoscopy revealed significant subglottic and diffuse airway edema and erythema throughout the tracheobronchial tree, with blackish lesions suggestive of injury from the recent inhalation of smoke and soot (Fig. 2). The fluid from a bronchoalveolar lavage performed from the right middle lobe was greyish black in color. Due to the airway edema, the ETT could not be advanced further. The patient underwent a tracheostomy to secure the airway on the second day of admission. Treatment with antibiotics was started for suspected aspiration pneumonia. The bronchodilators albuterol and ipratropium and systemic steroids were added to the treatment to manage the bronchoconstriction and edema. A regimen of 10,000 IU of inhaled unfractionated heparin (Sagent Pharmaceuticals, Schaumburg, IL) diluted in 3 mL of 0.9% normal saline alternating every 2 hours with 3 mL of 20% NAC (Fresenius Kabi, Lake Zurich, IL) was started 48 hours after admission and continued for 7 days. A second bronchoscopy with an FFB on the fifth day after admission showed a significant improvement in the airway edema and a resolution of the soot (Fig. 2). The patient did not experience any adverse events, such as bleeding or bronchospasm, from the therapy. Daily monitoring of platelets revealed no changes from baseline, which ranged between 175 and 205 k/μL. The patient's clinical status improved and he was taken off the ventilator, and he was later decannulated on the ninth day of admission and subsequently discharged from the hospital.
Figure 1.
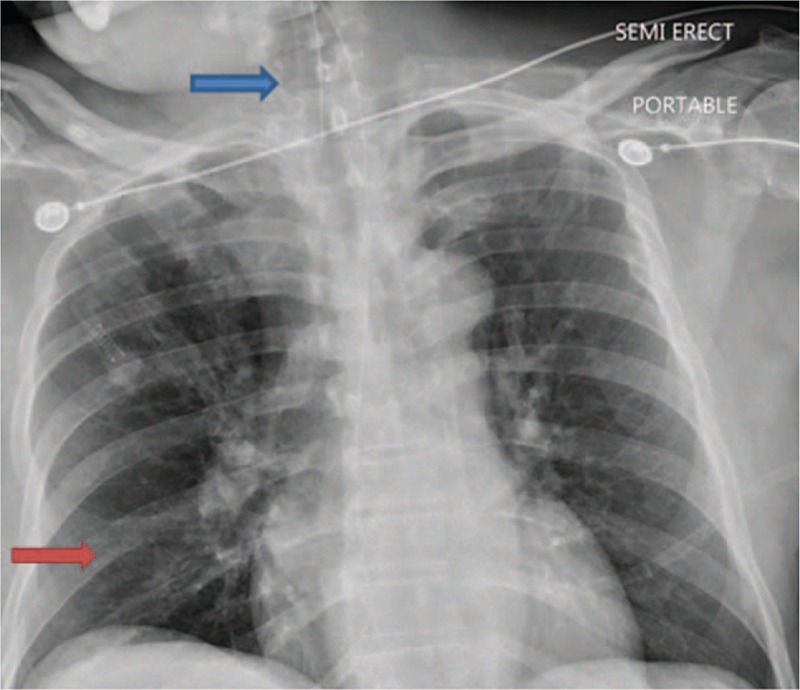
Chest roentgenogram on admission showing ETT high in the trachea (blue arrow), ill-defined infiltrates in right lower lobe (red arrow), and possible infiltrates in the right upper lobe.
Figure 2.
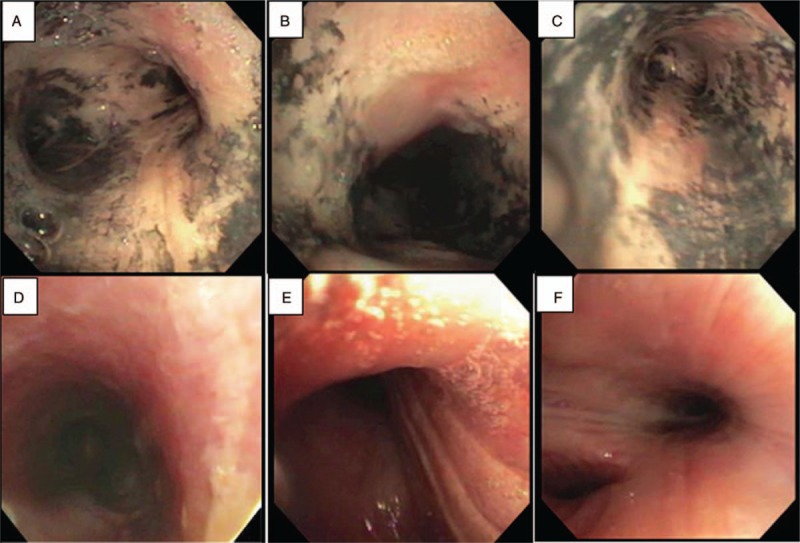
Bronchoscopy with an FFB showing the airway on admission (A–C) with extensive carbonaceous material and airway edema. (D–F) Pictures of the same airway 5 days later. A and D, carina; B and E, right main bronchus; C and F, left main bronchus.
3. Discussion
Inhalation injuries are found in 10% to 20% of burn patients and increase overall morbidity and mortality.[5] Other factors associated with an increased mortality of these patients include the burn surface area, advanced age, and a low PaO2/FiO2 ratio.[6,7] However, a significant airway injury may exist even in the absence of cutaneous burns.[8]
Among the culprits for lung injury secondary to inhalation are insults from thermal energy or chemical irritants. Heat or thermal injury is usually restricted to supraglottic structures, as the larger area of distribution nullifies the high degree of heat other than in cases of steam jet injury. Heat injury results in massive swelling of the upper airway, resulting in airway compromise.[9,10] Chemical injury to the lower airway occurs as a result of toxins generated from the burning of substances such as rubber, plastics, cotton, and laminated furniture. These toxins cause damage to epithelial and capillary endothelial cells of the airway, resulting in the destruction of mucociliary transport and surfactant loss. Moreover, the leakage of plasma into the airway causes intra-airway coagulation and fibrin deposition. The cellular debris, mucin, and fibrin mixture develops into airway casts, resulting in a perfusion-ventilation mismatch and an increase in dead space.[9]
A devastating complication in burn patients is systemic toxicity from the products of combustion, including carbon monoxide and cyanide. Carbon monoxide is an odorless and colorless gas and is one of the most prevalent etiologies for early morbidity in burn-injured patients.[9] Incremental increases in systemic concentrations of carboxyhemoglobins are associated with a spectrum of clinical presentations. Levels of 10% to 30% are associated with headaches, levels of 30% to 40% cause fatigue, nausea, and impaired cognition, and levels of 40% to 60% can result in combativeness, hallucinations, shock, and unconsciousness. Levels higher than 60% cause respiratory and cardiac depression and are fatal in more than half of patients. Hydrogen cyanide is produced during the combustion of numerous household materials. It inhibits the cytochrome oxidase system and can also act synergistically with carbon monoxide to prolong tissue hypoxia, induce refractory acidosis, and decrease cerebral oxygen consumption.[10,11]
The diagnosis of compromised airways involves primarily a high index of suspicion together with clinical evaluation and direct visualization of the airways. A detailed history pertaining to the type and duration of exposure, the quality of inhaled irritants (house fire or industrial), and unconsciousness should be obtained. Physical examination should focus on the presence of facial injuries, stridor, hoarseness, singed nasal hairs, soot in the naso-oropharynx, carbonaceous material in the sputum, or respiratory distress. Bronchoscopy can confirm an inhalational injury and show mucosal edema, erythema, erosions, necrosis, and the presence of soot or carbonaceous material in the airway.[9–11]
It is often difficult to predict the severity and extent of airway involvement. Proximal injuries observed by bronchoscopy typically exceed those of the peripheral pulmonary parenchyma, and thus, bronchoscopic grading schemes inconsistently predict the severity of the condition.[9,10,12] The measurement of bronchial wall thickness by chest computed tomography is a promising technique for evaluating the severity of the injury and determining the clinical course.[13]
The management of smoke-induced acute lung injury is mainly supportive and depends on the presenting condition. Endotracheal intubation is warranted if airway patency is threatened. However, the security of the ETT should be closely monitored, because upper airway edema makes reintubation difficult. In addition, a larger ETT is recommended in anticipation of the increased amount of secretions and debris. An immediate tracheostomy is rarely required, but early tracheostomy requires less sedation, results in higher airway security, and has been shown to provide better patient comfort and ventilation.[11] Prophylactic antibiotics and empirical glucocorticoids are typically not recommended.[9,10]
Various adjunct therapies have been used to decrease the formation of fibrin casts, thus limiting airway obstruction and improving oxygenation. Although therapies such as inhaled tissue plasminogen activator, danaparoid, activated protein C, antithrombin, and tissue factor pathway inhibitor have only been researched in animal models and with variable success, the combination of nebulized heparin and NAC has shown efficacy in animal and human studies.[2,8] Nebulized heparin inhibits fibrin clot formation and NAC promotes mucolysis and provides antioxidant and anti-inflammatory properties. The use of nebulized heparin and NAC gained popularity after a study by Desai et al. [1] showed decreased mortality, reintubation rate, and incidence of pneumonia in children with inhalation injuries treated with low doses of heparin (5000 IU) and 3 mL of a 20% solution of aerosolized NAC. The dose of nebulized heparin was 10,000 IU in our patient. A therapy consisting of alternating treatment with nebulized heparin, NAC, and albuterol in adult patients with smoke inhalation injuries decreased the mortality and improved the LIS in 1 retrospective study [14] and reduced the duration of mechanical ventilation in another.[15] However, another retrospective study by Holt et al [16] showed no significant difference in mortality, duration of mechanical ventilation, length of stay, or incidence of pneumonia in patients treated with inhaled heparin and NAC.
Retrospective studies showing beneficial effects of nebulized heparin and NAC used either a high-dose (10,000 IU) [14] or low-dose (5000 IU) [1,15] nebulized heparin regimen. However, a recent prospective randomized study comparing different doses of nebulized heparin in 29 patients with smoke inhalation concluded that the higher dose of 10,000 IU decreased the LIS and duration of mechanical ventilation compared with that in patients treated with a lower dose of 5000 IU.[4] A retrospective analysis with historical controls by Yip et al [17] showed the safety of nebulized heparin and NAC, which is consistent with the results of the prospective study mentioned previously.[4]
4. Conclusion
The case we report here highlights several aspects of the challenging management of patients with inhalation injury. The most important aspects involve the early recognition of airway compromise; anticipation of a difficult airway, especially in a patient with obesity; close monitoring of the position of the ETT; and medication and ventilator management. The decision to perform a tracheotomy should be made on an individual basis. On the basis of our experience with this patient, we postulate that a regimen of nebulized heparin and NAC may be safe and beneficial in patients with mild-to-severe inhalation injuries. This regimen should be initiated as soon as possible. Lung protective techniques should be used for patients on mechanical ventilation.
Author contributions
Writing – original draft and literature review: Umair Ashraf, Bharat Bajantri, and Gabriella Roa-Gomez.
Writing – review & editing: Amanda Cantin, Sindhaghatta Venkatram, Gilda Diaz-Fuentes
Footnotes
Abbreviations: ETT = endotracheal tube, FFB = flexible fiberoptic bronchoscope, LIS = lung injury score, NAC = N-acetylcysteine.
The authors of this manuscript did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare no conflict of interest.
References
- [1].Desai MH, Mlcak R, Richardson J, et al. Reduction in mortality in pediatric patients with inhalation injury with aerosolized heparin/N-acetylcystine [correction of acetylcystine] therapy. J Burn Care Rehabil 1998;19:210–2. [DOI] [PubMed] [Google Scholar]
- [2].Juschten J, Tuinman PR, Juffermans NP, et al. Nebulized anticoagulants in lung injury in critically ill patients: an updated systematic review of preclinical and clinical studies. Ann Transl Med 2017;5:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Glas GJ, Serpa Neto A, Horn J, et al. Nebulized heparin for patients under mechanical ventilation: an individual patient data meta-analysis. Ann Intensive Care 2016;6:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Elsharnouby NM, Eid HE, Abou Elezz NF, et al. Heparin/N-acetylcysteine: an adjuvant in the management of burn inhalation injury: a study of different doses. J Crit Care 2014;29:182.e1-e4. [DOI] [PubMed] [Google Scholar]
- [5].Walker PF, Buehner MF, Wood LA, et al. Diagnosis and management of inhalation injury: an updated review. Crit Care 2015;19:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].El-Helbawy RH, Ghareeb FM. Inhalation injury as a prognostic factor for mortality in burn patients. Ann Burns Fire Disasters 2011;24:82–8. [PMC free article] [PubMed] [Google Scholar]
- [7].Hassan Z, Wong JK, Bush J, et al. Assessing the severity of inhalation injuries in adults. Burns 2010;36:212–6. [DOI] [PubMed] [Google Scholar]
- [8].Miller AC, Elamin EM, Suffredini AF. Inhaled anticoagulation regimens for the treatment of smoke inhalation-associated acute lung injury: a systematic review. Crit Care Med 2014;42:413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Sheridan RL. Fire-related inhalation injury. N Engl J Med 2016;375:464–9. [DOI] [PubMed] [Google Scholar]
- [10].Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med 2013;21:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Palmieri TL, Gamelli RL. Jeschke MG, Kamolz L-P, Sjöberg F, Wolf SE. Diagnosis and management of inhalation injury. Handbook of Burns: Acute Burn Care Volume 1. Vienna: Springer Vienna; 2012. 163–72. [Google Scholar]
- [12].Spano S, Hanna S, Li Z, et al. Does bronchoscopic evaluation of inhalation injury severity predict outcome? J Burn Care Res 2016;37:1–1. [DOI] [PubMed] [Google Scholar]
- [13].Yamamura H, Morioka T, Hagawa N, et al. Computed tomographic assessment of airflow obstruction in smoke inhalation injury: relationship with the development of pneumonia and injury severity. Burns 2015;41:1428–34. [DOI] [PubMed] [Google Scholar]
- [14].Miller AC, Rivero A, Ziad S, et al. Influence of nebulized unfractionated heparin and N-acetylcysteine in acute lung injury after smoke inhalation injury. J Burn Care Res 2009;30:249–56. [DOI] [PubMed] [Google Scholar]
- [15].McGinn KA, Weigartz K, Lintner A, et al. Nebulized heparin with N-acetylcysteine and albuterol reduces duration of mechanical ventilation in patients with inhalation injury. J Pharm Pract 2017;0897190017747143s. [DOI] [PubMed] [Google Scholar]
- [16].Holt J, Saffle JR, Morris SE, et al. Use of inhaled heparin/N-acetylcystine in inhalation injury: does it help? J Burn Care Res 2008;29:192–5. [DOI] [PubMed] [Google Scholar]
- [17].Yip LY, Lim YF, Chan HN. Safety and potential anticoagulant effects of nebulised heparin in burns patients with inhalational injury at Singapore General Hospital Burns Centre. Burns 2011;37:1154–60. [DOI] [PubMed] [Google Scholar]


