Abstract
Most patients with acute myocardial infarction (AMI) experience more than one symptom at onset. Although symptoms are an important early indicator, patients and physicians may have difficulty interpreting symptoms and detecting AMI at an early stage. This study aimed to identify symptom clusters among Korean patients with ST-elevation myocardial infarction (STEMI), to examine the relationship between symptom clusters and patient-related variables, and to investigate the influence of symptom clusters on treatment time delay (decision time [DT], onset-to-balloon time [OTB]). This was a prospective multicenter study with a descriptive design that used face-to-face interviews. A total of 342 patients with STEMI were included in this study. To identify symptom clusters, two-step cluster analysis was performed using SPSS software. Multinomial logistic regression to explore factors related to each cluster and multiple logistic regression to determine the effect of symptom clusters on treatment time delay were conducted. Three symptom clusters were identified: cluster 1 (classic MI; characterized by chest pain); cluster 2 (stress symptoms; sweating and chest pain); and cluster 3 (multiple symptoms; dizziness, sweating, chest pain, weakness, and dyspnea). Compared with patients in clusters 2 and 3, those in cluster 1 were more likely to have diabetes or prior MI. Patients in clusters 2 and 3, who predominantly showed other symptoms in addition to chest pain, had a significantly shorter DT and OTB than those in cluster 1. In conclusion, to decrease treatment time delay, it seems important that patients and clinicians recognize symptom clusters, rather than relying on chest pain alone. Further research is necessary to translate our findings into clinical practice and to improve patient education and public education campaigns.
Keywords: STEMI, symptom cluster, time delay, two-step cluster analysis
1. Introduction
In acute myocardial infarction (AMI), symptoms are an important early indicator for patients to decide when to seek treatment. However, patients can have difficulty interpreting symptoms, and physicians may also have difficulty detecting AMI at an early stage.[1] In a previous study, 35% of patients with AMI experienced only chest pain, whereas 57% experienced other symptoms in addition to chest pain.[2] As many as 87% of patients had at least 1 AMI symptom, and the average number of symptoms patients experienced was 4.75.[2] As a result, some researchers have tried to describe and analyze AMI symptoms as clusters.
Symptom clusters can be defined as 2 or more symptoms that are related and experienced simultaneously.[1] Symptom clusters can be used to analyze patterns, and to identify sociodemographic and clinical characteristics; they can provide useful information for the early detection and diagnosis of diseases.[3] Several investigators have suggested studying the relationships between symptom clusters and major characteristics of patients with ST-elevation myocardial infarction (STEMI). Since patients with STEMI require rapid treatment, they preferentially need to be educated to help in early recognition of the symptoms of AMI onset.[4] Hence, we can expect that identification of symptom clusters among patients with AMI (especially those with STEMI) will enable earlier recognition and diagnosis of AMI, thus reducing delays in treatment.
Treatment time delay is caused by various delays between symptom onset and reperfusion therapy.[5,6] “Patient delay” is defined as the time from symptom onset to the patient's seeking medical attention, that is, the first medical contact.[5,6] “System delay” is the time interval between the first medical contact and reperfusion.[5,6] Finally, “total treatment delay” is defined as the sum of the patient delay and the system delay.[5,6] Since patient delay accounts for most of the prehospital delay[7] and total treatment delay is important for improving clinical outcomes in STEMI,[8] both are good indicators to investigate the association between symptoms and the treatment time delay.
Although symptom clusters have been reported mainly in studies from the US since 2007,[1,2,9–12] there is still insufficient knowledge regarding these clusters. Thus far, few international studies, including few Korean studies, have identified symptom clusters in patients with STEMI[10,13] and investigated the influence of symptom clusters on treatment time delay.[1] Therefore, the present study aimed to identify symptom clusters among Korean patients with STEMI, to examine the relationship between symptom clusters and patient-related variables, and to investigate the influence of symptom clusters on treatment time delay.
2. Methods
2.1. Study setting and population
This was a prospective multicenter study with a descriptive design. The study participants were hospitalized patients with STEMI at 6 percutaneous coronary intervention (PCI)-capable tertiary hospitals throughout Korea between July 2014 and June 2015 (the data collection period at each hospital was different); STEMI teams for primary PCI (PPCI), including a cardiologist, were present on site (partially on call) 24 hours a day, 7 days a week, in all participating hospitals. These hospitals were chosen to provide geographical diversity. Inclusion criteria were as follows: patients who survived and those with a final diagnosis of STEMI who underwent PCI, hospitalization within 72 hours after the onset of symptoms, hemodynamic stability, Korean speaking, and without cognitive impairment. Among patients with STEMI who were consecutively admitted to the hospital during the data collection period, a total of 350 patients met the above criteria. Eight patients who were not clustered due to the missing of clustering variables were excluded from the analysis, resulting in a final sample of 342.
2.2. Ethics statement
The study design and protocol were approved by the Institutional Review Board (IRB) at each hospital before data collection. The present study conformed to the tenets of the Declaration of Helsinki and was approved by the IRB of Seoul National University (IRB No.1502/001-003).
2.3. Questionnaire and data collection
The questionnaire for the present study was developed by the investigator in collaboration with 4 cardiologists. First, the questionnaire was developed by referring to published research articles on cardiovascular populations.[14] Then, the content validity and face validity of the questionnaire were established for the Korean setting through repeated discussions among the 4 cardiologists and pilot testing with patients with STEMI. Data on the following variables were collected using the questionnaire through the interview method: sociodemographic characteristics (gender, age, height, weight, education level, occupation, living alone or not, and residence area); risk factors (smoking, drinking, obesity, and family history of cardiovascular disease); clinical characteristics (hypertension, diabetes, dyslipidemia, medical history of angina, or MI); transport-related items {mode of transport to the study hospital in the case of direct admission or to the first hospital in the case of interhospital transfer for AMI: 119 (the national emergency telephone number in Korea and emergency medical services [EMS]), private vehicle, and other}; and symptoms experienced during the acute phase of STEMI (multiple choice). In the interview, patients were asked about 10 symptoms using a yes/no format: (1) chest pain, (2) radiating pain, (3) dyspnea, (4) sweating, (5) weakness, (6) indigestion, (7) nausea or vomiting, (8) dizziness, (9) palpitations, and (10) other (“other” was an open-ended question). The 10 symptoms were selected based on the previous relevant studies[2–4,11–13,15–17] and the consultation with cardiologists. After the interview, a content analysis was conducted to classify “other” symptoms; some were similar to the 9 symptoms suggested to patients and were added to the existing symptom categories. The symptoms that differed from the 9 symptoms were grouped into the following 4 categories: (10) chills, (11) headache, (12) numbness, and (13) fainting. Finally, the other symptoms that occurred in very few cases and were very different from the 13 categories were grouped into “(14) other.” Ultimately, a total of 14 categories (from “(1) chest pain” to “(14) other”) were used in the cluster analysis.
In this study, treatment time delay was measured by 2 parameters: decision time (DT), representing patient delay or the time interval between symptom onset and when the patient sought medical care, and onset-to-balloon time (OTB), representing the total treatment delay or the time from onset of symptoms to balloon inflation.[5,7] Patient DT was collected as follows: each patient was asked to identify the time at which he/she experienced the symptoms that brought them to the hospital and to estimate the time between symptom onset and the time when they decided to seek medical care. Data on time of ballooning (PCI) were extracted from the medical records. Hospital characteristics were also based on medical records: Killip class on admission was used to assess cardiac risk[18]; left ventricular ejection fraction (LVEF) at admission was used to assess cardiac performance[19]; and final diagnosis. Killip class and LVEF are more precise when used together and are a proxy for disease severity for MI[20]; they were used as risk (severity) adjustment variables in the multiple analysis.
After obtaining written informed consent, patients were interviewed by the study nurse at each hospital. The study nurse conducted the face-to-face questionnaire in the education room, which is a dedicated room for education and counseling for patients and guardians and is located near the cardiac ward. The interview lasted for approximately 20 minutes and was conducted within 3 days of hospital admission.
2.4. Statistical analysis
IBM SPSS Statistics for Windows version 20 (IBM Corp., Armonk, NY) was used for data analysis. Essentially, cluster analysis was performed for symptoms of STEMI. SPSS Statistics provides 3 procedures that can be used to cluster data: hierarchical cluster analysis, k-means cluster, and two-step cluster. Among these, the two-step cluster accommodates categorical as well as continuous variables. In this study, to identify subgroups of patients at risk for specific symptom clusters, 14 symptoms (plus gender, age, prior angina, and prior MI) were analyzed using two-step cluster analysis. Gender, age, prior angina, and prior MI were included because of their established clinical importance in the cluster analysis of symptoms. Age and sex were significant predictors of cluster membership in a previous study.[2] Meanwhile, sex, age, and comorbid conditions were reported to influence the symptoms experienced during acute coronary syndrome (ACS).[10] In another study, it has been reported that age and personal history of heart disease were factors strongly associated with the clusters.[11]
The two-step cluster analysis is performed in 2 phases.[21] The first step of a two-step cluster analysis, called the “precluster,” distributes subjects into small subclusters. During the second step, these subclusters are grouped into a preset number of clusters; if the preferred number of clusters is not given or was unknown, the SPSS two-step cluster component automatically finds the valid number of clusters. In the present study, the log-likelihood distance measure and Bayesian Information Criterion (BIC) were used to determine the best cluster solution, and the number of clusters was not provided in advance.
After the identification of symptom clusters, univariate analysis (using chi-square tests for categorical variables and one-way analysis of variance [ANOVA] models for continuous variables) was performed to compare differences in symptoms and sample characteristics according to the cluster membership. In addition to univariate analysis, a multinomial logistic backward stepwise regression was conducted to explore factors related to each cluster.[11] Next, chi-square tests to examine differences in the treatment time delay (DT, OTB) according to characteristics of patients with STEMI and symptom clusters were performed. Finally, multiple logistic backward stepwise regressions to determine the effect of a symptom cluster on treatment time delay were conducted. DT and OTB were categorized as dichotomous variables (<60 or ≥60 minutes and <180 or ≥180 minutes, respectively). The cutoffs of 60 minutes (DT)[22,23] and 180 minutes (OTB)[5,24] were selected based on the previous literature. Potential confounding variables known to influence treatment time delay were included in the multiple analysis: gender, age, education, occupation, residence, living, smoking, drinking, obesity, family history of cardiovascular disease, hypertension, diabetes, dyslipidemia, prior angina, prior MI, Killip class, LVEF, mode of transport to the first hospital, and symptom cluster. The statistical significance level (α) was set at 0.05.
3. Results
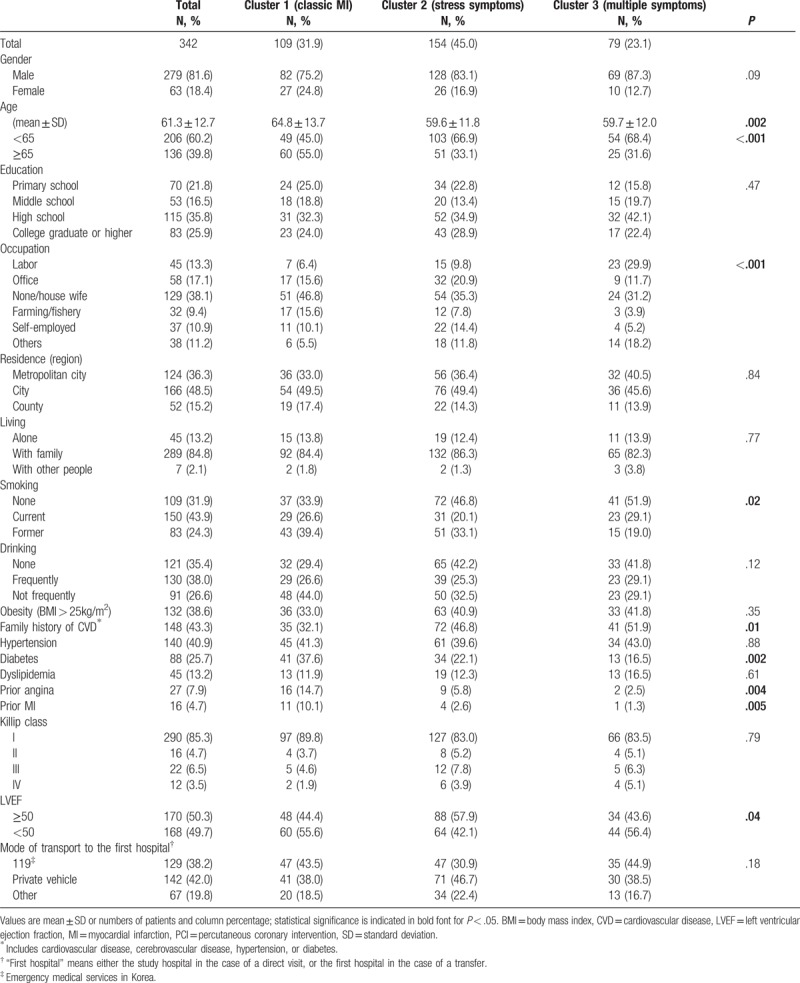
3.1. Baseline characteristics and comparison by cluster group
As shown in Table 1, a total of 342 patients with documented STEMI were included in this study. The patients’ average age was 61.3 ± 12.7 years and 18.4% were female. In terms of risk factors for AMI in the patient's medical history, a history of angina or AMI was reported by 7.9% and 4.7% of patients, respectively. Further sociodemographic and clinical characteristics are detailed in Table 1. Next, 3 symptom clusters were formed after a two-step cluster analysis of total symptoms. Table 1 also shows various characteristics according to symptom cluster. There were more men than women in all 3 clusters, but the difference was not statistically significant (P = .09). The mean age of patients in cluster 1 (64.8 years) was significantly higher than that in cluster 2 (59.6 years) and cluster 3 (59.7 years) (P = .002). In addition, there were differences in occupation (P < .001), smoking (P = .02), and family history (P = .01) among clusters. For medical history, the difference was significant for diabetes (P = .002), prior angina (P = .004), and prior MI (P = .005). There were no differences in Killip classes or mode of transport among the 3 clusters, and a normal range of LVEF (≥50) was most common in cluster 2 at 57.9% (P = .04).
Table 1.
Subjects’ baseline characteristics and comparison of characteristics by cluster group.
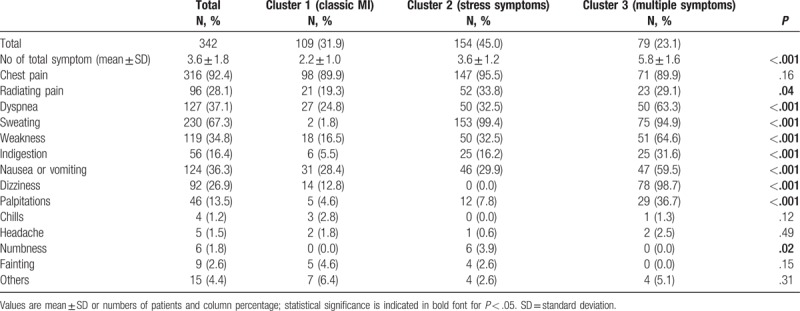
3.2. Comparison of frequency of presenting symptoms by cluster group
Symptoms reported on admission are summarized in Table 2. On average, patients reported 3.6 ± 1.8 symptoms. Most common was chest pain (92.4%), followed by sweating (67.3%). Less frequently reported symptoms were dyspnea (37.1%), nausea or vomiting (36.3%), and weakness (34.8%). Cluster 2 (n = 154, 45.0%) was the largest, followed by cluster 1 (n = 109, 31.9%) and cluster 3 (n = 79, 23.1%). There was a significant difference among the 3 clusters in the number of symptoms (P < .001); patients in cluster 1 had the lowest number of symptoms (2.2 ± 1.0), and those in cluster 3 had the highest (5.8 ± 1.6). Table 2 also shows the frequency of each symptom among the clusters. Among symptoms occurring with a relatively high frequency in cluster 1, chest pain was the most common at 89.9%, followed by nausea or vomiting at 28.4% and dyspnea at 24.8%. In cluster 2, sweating was the most common at 99.4%, followed by chest pain (95.5%) and radiating pain (33.8%). Cluster 3 included many atypical symptoms such as dizziness (98.7%), sweating (94.9%), weakness (64.6%), and dyspnea (63.3%) with greater frequency, in addition to chest pain (89.9%). As for the distribution of total symptoms in each cluster, excluding chest pain, chills, headache, fainting, and others (the 14th item among 14 symptoms), the remaining symptoms (radiating pain [P = .04]; dyspnea, sweating, weakness, indigestion, nausea or vomiting, dizziness, and palpitations [all P < .001]; numbness [P = .02]) showed significant differences between clusters. Considering the distribution, frequency, and number of symptoms, the clusters were named “cluster 1” (classic MI), “cluster 2” (stress symptoms), and “cluster 3” (multiple symptoms).
Table 2.
Comparison of frequency of presenting symptoms by cluster group.
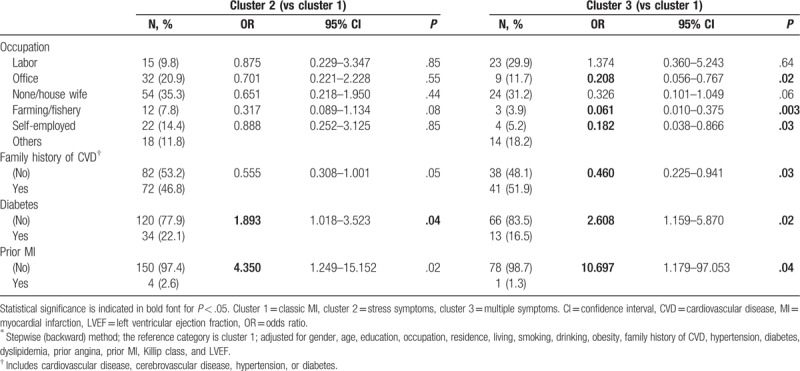
3.3. Factors related to each cluster
As a result of a multinomial logistic regression analysis, Table 3 shows factors related to clusters 2 and 3 compared to cluster 1; the reference category is cluster 1. Compared with patients in cluster 1, patients without diabetes or prior MI were significantly more likely to belong to clusters 2 or 3; patients in cluster 2 were less likely to have diabetes or prior MI (odds ratio [OR] 1.893; 95% confidence interval [CI], 1.018–3.523 and OR 4.350; 95% CI, 1.249–15.152, respectively). Similarly, the OR of belonging to cluster 3 was 2.608 (95% CI, 1.159–5.870) in patients without diabetes and 10.697 (95% CI, 1.179–97.053) in those without prior MI.
Table 3.
Multinomial logistic regression analysis∗: factors related to each cluster.
3.4. Characteristics of patients with STEM stratified according to treatment time delay
DT of <60 minutes was seen in 85.7% of patients who were college graduates or higher (P = .01), and patients without dyslipidemia or with prior angina had a significantly shorter DT. There were no gender or age differences in DT. On the other hand, patients who used 119 (83.9%, P = .01) were significantly more likely to have a DT of less than 60 minutes than those who used a private vehicle (69.5%) or other mode of transport (67.2%) to the first hospital (Table 4).
Table 4.
Characteristics of patients with ST-elevation myocardial infarction stratified according to treatment time delay (decision time, onset-to-balloon time).
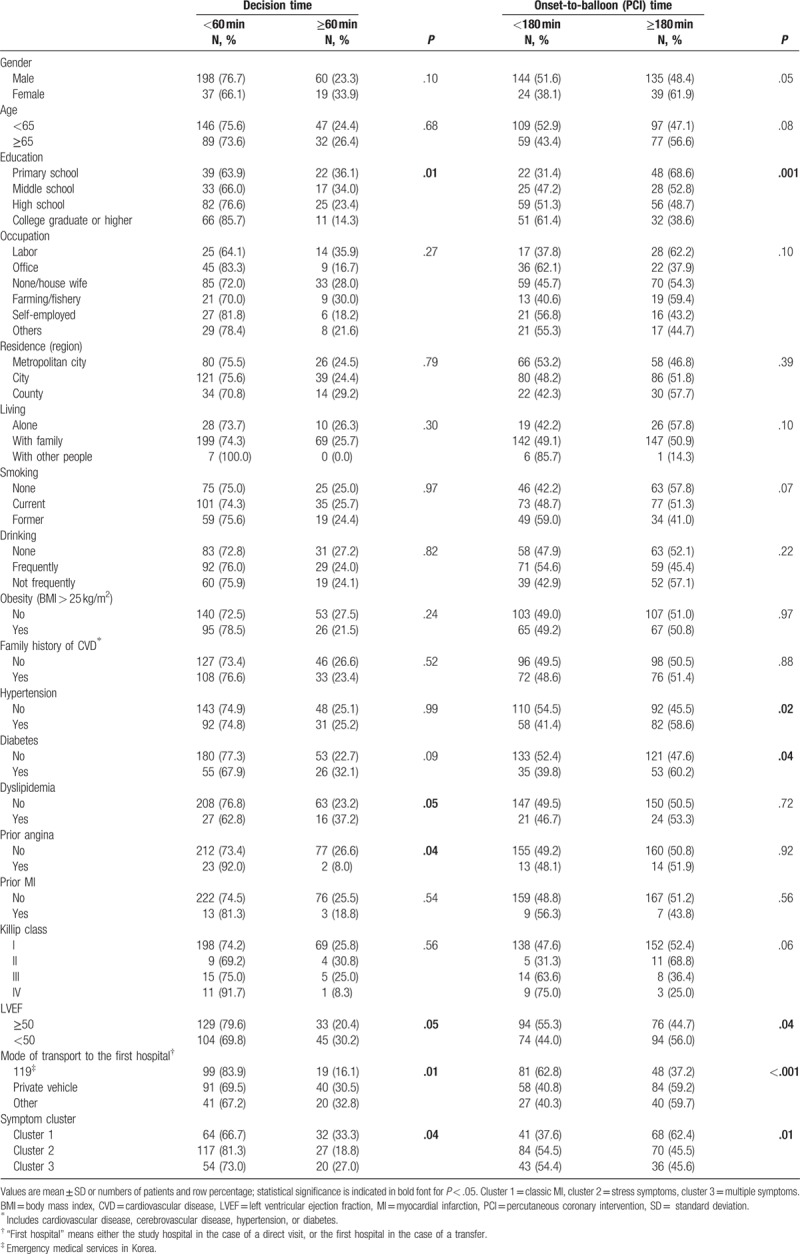
Concerning OTB, patients who were college graduates or higher (61.4%) and those without hypertension or diabetes (54.5% and 52.4%, respectively) were significantly more likely to have an OTB of less than 180 minutes. Among those with an OTB of less than 180 minutes, significantly more patients used 119 (62.8%, P < .001) than those who used a private vehicle or other mode of transport to the first hospital. Patients with a normal LVEF (55.8%) belonged significantly more often to this group (P = .04). Regarding treatment time delay according to symptom cluster, patients with a DT of less than 60 minutes most commonly (81.3%) belonged to cluster 2 (P = .04), and those with an OTB of more than 180 minutes most commonly (62.4%) belonged to cluster 1 (P = .01) (Table 4).
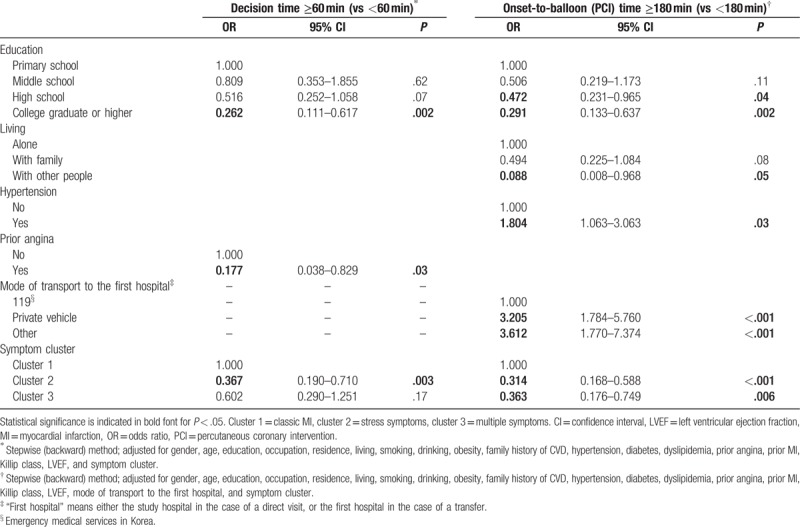
3.5. Factors associated with treatment time delay
Table 5 shows the independent factors influencing treatment time delay. The delay in DT was significantly shorter in patients who were college graduates or higher (P = .002), and in patients with prior angina (P = .03). OTB was significantly shorter in those with high school or college graduate/higher education than in those with primary school education, and in those living with other people (who are not a family member) than in those living alone. Patients with hypertension showed a longer OTB than those without (P = .03). The OTB in patients using a private vehicle or other modes of transport to the first hospital was significantly longer than in those using 119 (P < .001). As for symptom cluster, cluster 2 remained associated with a shorter DT (P = .003), and clusters 2 and 3 were also associated with a shorter OTB compared to cluster 1 (P < .001 and P = .006, respectively), after adjusting for several relevant factors.
Table 5.
Factors significantly associated with treatment time delay (decision time, onset-to-balloon time).
4. Discussion
Of all ACS types, patients with STEMI have the most urgent need for the blocked blood vessels to be reopened. In order to develop intervention strategies to reduce treatment time delay in Korean patients with STEMI, this study identified symptom clusters, examined the relationship between symptom clusters and patient-related variables, and investigated the influence of symptom clusters on treatment time delay. Using a two-step cluster analysis, 3 symptom clusters were identified: cluster 1 (classic MI), cluster 2 (stress symptoms), and cluster 3 (multiple symptoms). Among these, clusters 2 and 3, which comprised of markedly other symptoms in addition to chest pain, related with significantly shorter DT and OTB than cluster 1.
Patients most frequently reported chest pain, sweating, dyspnea, nausea or vomiting, weakness, and radiating pain, in the order named. The symptoms identified in this study are mostly similar to those listed by the American Heart Association. The American Heart Association identifies heart attack symptoms as chest discomfort, discomfort in the arms, back, neck, jaw, or stomach, shortness of breath, cold sweat, nausea, or lightheadedness.[25] Meanwhile, 1 study on patients with AMI in Korea[3] noted that we need to highlight “sweating” as one of the representative symptoms in any future public health campaigns and education to improve awareness of AMI symptoms in Korea. The importance of sweating is highlighted through the fact that it was a major component of clusters 2 and 3. This finding is very meaningful in Korea, because there is no standard set of AMI symptoms, and no report has validated the symptoms used in campaigns or in the education of physicians, patients, or the public.
In this study, only 7.6% of patients did not report chest pain as the presenting symptom on admission in this study. Some studies in Korea reported atypical symptoms in 9.4%[26] to 28.3%[27] of patients with STEMI; on the other hand, international studies have reported atypical symptoms in 16.6%[2] to 27.1%[28] of patients with AMI. Thus, being aware of chest pain alone is insufficient to enable patients to seek medical care and for clinicians to provide proper treatment for AMI. The different incidences of atypical symptoms reported in these studies may be in part due to different inclusion criteria or due to differences in research methods; nevertheless, most patients with STEMI in Korea seem to experience chest pain.
In our study, the average number of symptoms experienced was 3.6. This is similar to prior studies of patients with AMI that reported 3.6 symptoms[29] to 4.75 symptoms[30] on average and a study of patients with ACS reporting 3.14 symptoms.[31] Meanwhile, we identified 3 symptom clusters in this study. The number of clusters has varied from 3 to 5 in previous studies,[1–3,9,13] and there were also differences and similarities in the type of symptom clusters among these studies. In the present study, chest pain was predominant in cluster 1, or classic MI. Cluster 1 is similar to the “typical chest pain symptom” and the average age (about 64 years) in the study by Hwang et al[13] and to the “Classic ACS” reported by Riegel et al (although this group included only chest pain).[1] Cluster 1 in our study is also similar to the “Chest Pain Only,”[9] and “Chest Symptoms Only”[10] clusters of other studies[9,10] in the sense that patients in these clusters had the highest average age among the clusters identified in each study (67.53 and 65.4 years, respectively). In cluster 2 (stress symptoms), sweating and chest pain were predominant. This is similar to the “multiple symptoms” and the ages (59.6 and 58.1 years, respectively) reported in the study by Hwang et al.[13] However, the “multiple symptoms” reported by Hwang et al[13] were more characterized by chest pain than sweating, whereas the reverse was true in this study. Cluster 2 is also partly similar to the “Stress Symptoms” reported by Riegel et al,[1] although “sweating” and “nausea” were the major components in the study by Riegel et al.[1] The dominant characteristic of cluster 3 (multiple symptoms) was the highest rate of dizziness. One explanation for this seems to be the difference in occupation; patients in cluster 3 reported the highest percentage of “labor” (manual) workers among the 3 clusters, and labor workers reported significantly more “dizziness” in the univariate analysis (data not shown, P < .001). The characteristics of cluster 3 are in part similar to the “Younger, minority, multiple distressing symptom,”[11] the “atypical symptom” group,[13] “Cluster 3,”[2] and “Heavy Symptom Burden”[9,10] reported in previous studies; the last cluster (Heavy Symptom Burden) had the youngest average age in both studies (56.97[9] and 54.8 years,[10] respectively).
In the present study, differences in the symptoms comprising each cluster were not striking when compared with the previous literature. This is because most subjects had experienced chest pain as a chief complaint; even in cluster 3 with a high rate of atypical symptoms, chest pain was reported in 89.9% of patients. This may be attributed to the fact that we enrolled only patients with STEMI in this study. This is consistent with a recent study demonstrating that among patients presenting to the emergency department with potential ACS, patients with STEMI are more likely to be included in the 2 symptom clusters characterized prominently by chest pain or discomfort.[10]
No gender differences were seen among the clusters in this study, which is similar to the results of previous studies.[1,13] Among the patients, those in cluster 1 had the highest average age; in addition, the proportion of patients with diabetes, prior angina, or prior MI was significantly higher in this cluster. Concerning the symptoms and subjects’ characteristics, this result is different from some previous literature suggesting that atypical symptoms are more commonly seen in elderly or diabetic patients,[13,32] and that older adults experience milder and more diffuse symptom clusters that include less classic symptoms of ACS.[12] Nevertheless, cluster 1 in the present study, and “Chest Pain Only”[9] and “Chest Symptom Only”[10] in previous studies, which included chest pain as a major component and are relatively recent studies, were the oldest groups. It is controversial whether symptoms and prehospital delay times differ in patients with diabetes and those without.[33] On one hand, some studies reported silent ischemia in patients with diabetes[32]; however, some reports showed no difference in the pattern of the cardiac-related symptoms experienced by patients with and without diabetes who visited the emergency room.[33] According to the latest literature,[33] patients with and without diabetes commonly reported chest pain; this did not change after adjusting for age and gender. Additionally, chest pain, sweating, pain, or discomfort in the arms/hands, and fatigue were the most frequent symptoms in patients without diabetes.[33] As shown by the multinomial logistic regression analysis, patients belonging to cluster 1 had a higher probability of prior MI compared to those in clusters 2 and 3. This result is similar to that in previous literature,[34] and it can be assumed that patients with prior MI experience chest pain more commonly than those without.
Concerning the number of symptoms, although we have to consider the difference in criteria for “younger” and “older” patients in each study, our results are similar to those of previous research showing that older patients with ACS often report fewer symptoms.[10] Furthermore, it is also consistent with the prior finding that older patients are more prone to experience clusters composed of the least number of symptoms.[9,10,12] One explanation for this tendency is that the elderly may have difficulty recognizing symptoms, which can be in part due to poor interoception (sensitivity to stimuli originating inside of the body).[35]
The symptom groups and the number of clusters in this study are similar to those seen in previous literature. However, a few differences exist between them. This can be partly attributed to the differences in target population (ACS, AMI, STEMI), inclusion criteria, the symptoms included in each instrument, and clustering methods.[12]
Some findings in this study are consistent with the literature showing that higher education level and living with a colleague/companion or someone who is not a family member are associated with a shorter delay at ACS symptom onset.[36] One possible explanation for the association between education and delays is that education level could affect patients’ knowledge/awareness about the disease and its symptoms.[37,38] Another possible explanation is that education level might just be a proxy for socioeconomic status, which has been known to be a factor influencing prehospital delay.[24,39,40] Ultimately, since education impacts one's ability to collect and interpret information and to solve problems on many levels and may play an important role in both choosing lifestyle and health behaviors and searching health care,[41] the DT and the OTB might be affected by different choices in the process of decision-making and seeking medical care. On the other hand, in contrast to some previous literature reporting that prehospital delay did not differ among symptom clusters,[1,13] in the present study, treatment time delay (DT, OTB) differed significantly among the symptom cluster groups in both univariate and multiple analyses. Although patients in cluster 1 had chest pain as the only dominant symptom, the percentage of patients with an OTB of more than 180 minutes was the greatest in this cluster. Regarding OTB, various factors influence OTB, including patients’ personal characteristics and system-related characteristics (quality of hospital care, EMS in the prehospital phase).[42,43] Meanwhile, the system delay may have multiple paths,[8,44] but all external factors relevant to these paths were not considered in this study. For example, the EMS system is one of the most important factors in these paths. Moreover, it is composed of various systematic factors that affect the performance of the EMS system, including the appropriateness of the prehospital care (preliminary medical care on scene and during transport), prehospital time, prehospital transport, hospital care, and interhospital transfer. Despite the fact that this study did not measure the intensity of symptoms or exclude the possibility of residual confounding by other variables associated with treatment time delay, it appears that DT and OTB decrease when several symptoms rather than a single symptom are prominent. This result is supported by previous literature; individuals evaluate or validate an illness based on multiple symptoms (clusters or groups), using 1 symptom as a trigger.[2] Thus, to decrease treatment time delay, it seems to be important that patients and clinicians recognize symptom clusters rather than rely on chest pain alone.
4.1. Strengths and limitations
The major strengths of this study are the study design and data collection methods. The study had a prospective, multicenter design, and used face-to-face interviews and a structured questionnaire. These elements can contribute to increased accuracy of data and the representativeness of the study compared to previous research that was based on medical records or used data from only 1 hospital. Prior reports have demonstrated that symptom data obtained by interviews are more accurate and complete than data extracted from medical records.[2,45] Finally, to the best of our knowledge, this study was the first to identify symptom clusters in Korean patients with STEMI.
This study has several limitations. First, recall bias attributed to survey methodology (patient interview) cannot be excluded, but to minimize this bias, we tried to complete the interview within 3 days of hospital admission. However, it has been shown that people have accurate memories of experiences surrounding strong life events.[11] Second, we mainly analyzed variables related to patients’ personal characteristics, while other factors that could influence treatment time delay, particularly system characteristics were beyond the scope of this study. Another limitation is that this study cannot be generalized to all patients with STEMI; we were not able to include the patients who died shortly after arrival at the hospital since they could not be surveyed because their condition was too severe. Finally, we could not collect and analyze health outcomes according to symptom cluster, such as major adverse cardiac events, because of the limited survey duration. Thus, a further longitudinal study is necessary to verify and assess the differences in long-term outcomes among symptom cluster groups.
5. Conclusions
Identifying symptom clusters of AMI is intended to help patients recognize the symptoms and for clinicians to accurately triage and diagnose in the emergency room when patients describe these symptoms. The finding that age and medical history were statistically different among the clusters is crucial in predicting cluster membership. Based on this finding, the association between patient characteristics and symptom cluster could be used to determine cluster membership. In conclusion, to decrease treatment time delay, it seems important that patients and clinicians recognize symptom clusters, rather than relying on chest pain alone. Further research is necessary to confirm symptom clusters that can be generalized in patients with STEMI and to translate the findings into clinical practice and improve patient education and public education campaigns.
Author contributions
Conceptualization: Hee-Sook Kim, Sang Jun Eun, Kun-Sei Lee, Sung-il Cho.
Data curation: Sang Jun Eun.
Formal analysis: Hee-Sook Kim, Sang Jun Eun.
Funding acquisition: Kun-Sei Lee.
Investigation: Jin Yong Hwang, Kun-Sei Lee.
Methodology: Hee-Sook Kim, Sang Jun Eun, Jin Yong Hwang, Kun-Sei Lee, Sung-il Cho.
Project administration: Hee-Sook Kim, Jin Yong Hwang, Kun-Sei Lee.
Supervision: Sung-il Cho.
Writing – original draft: Hee-Sook Kim.
Writing – review & editing: Sung-il Cho.
Footnotes
Abbreviations: ACS = acute coronary syndrome, AMI = acute myocardial infarction, DT = decision time, EMS = emergency medical services, LVEF = left ventricular ejection fraction, OTB = onset-to-balloon time, PCI = percutaneous coronary intervention, STEMI = ST-elevation myocardial infarction.
Funding/support: This study was supported by funding from the Ministry of Health and Welfare.
The authors have no conflicts of interest to disclose.
References
- [1].Riegel B, Hanlon AL, McKinley S, et al. Differences in mortality in acute coronary syndrome symptom clusters. Am Heart J 2010;159:392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ryan CJ, DeVon HA, Horne R, et al. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res 2007;56:72–81. [DOI] [PubMed] [Google Scholar]
- [3].Park E, Lee J. Symptom clusters in Korean patients with acute myocardial infarction. J Korean Acad Nurs 2015;45:378–87. [DOI] [PubMed] [Google Scholar]
- [4].Hwang SY, Zerwic JJ, Jeong MH. Impact of prodromal symptoms on prehospital delay in patients with first-time acute myocardial infarction in Korea. J Cardiovasc Nurs 2011;26:194–201. [DOI] [PubMed] [Google Scholar]
- [5].Rollando D, Puggioni E, Robotti S, et al. Symptom onset-to-balloon time and mortality in the first seven years after STEMI treated with primary percutaneous coronary intervention. Heart 2012;98:1738–42. [DOI] [PubMed] [Google Scholar]
- [6].Ho AFW, Pek PP, Fook-Chong S, et al. Prehospital system delay in patients with ST-segment elevation myocardial infarction in Singapore. World J Emerg Med 2015;6:277–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Finn JC, Bett JHN, Shilton TR, et al. Patient delay in responding to symptoms of possible heart attack: can we reduce time to care? Med J Aust 2007;187:293–8. [DOI] [PubMed] [Google Scholar]
- [8].Higuma T, Hanada H, Okumura K, et al. and better clinical outcome in ST-segment elevation myocardial infarction. Circ J 2015;79:1897–9. [DOI] [PubMed] [Google Scholar]
- [9].DeVon HA, Ryan CJ, Rankin SH, et al. Classifying subgroups of patients with symptoms of acute coronary syndromes: a cluster analysis. Res Nurs Health 2010;33:386–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Rosenfeld AG, Knight EP, Steffen A, et al. Symptom clusters in patients presenting to the emergency department with possible acute coronary syndrome differ by sex, age, and discharge diagnosis. Heart Lung 2015;44:368–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].McSweeney JC, Cleves MA, Zhao W, et al. Cluster analysis of women's prodromal and acute myocardial infarction symptoms by race and other characteristics. J Cardiovasc Nurs 2010;25:311–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].DeVon HA, Vuckovic K, Ryan CJ, et al. Systematic review of symptom clusters in cardiovascular disease. Eur J Cardiovasc Nurs 2017;16:6–17. [DOI] [PubMed] [Google Scholar]
- [13].Hwang SY, Ahn YG, Jeong MH. Atypical symptom cluster predicts a higher mortality in patients with first-time acute myocardial infarction. Korean Circ J 2012;42:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zimmerman L, Pozehl B, Vuckovic K, et al. Selecting symptom instruments for cardiovascular populations. Heart Lung 2016;45:475–96. [DOI] [PubMed] [Google Scholar]
- [15].McSweeney JC, Cody M, O'Sullivan P, et al. Women's early warning symptoms of acute myocardial infarction. Circulation 2003;108:2619–23. [DOI] [PubMed] [Google Scholar]
- [16].Zerwic JJ. Symptoms of acute myocardial infarction: expectations of a community sample. Heart Lung 1998;27:75–81. [DOI] [PubMed] [Google Scholar]
- [17].DeVon HA, Rosenfeld A, Steffen AD, et al. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J Am Heart Assoc 2014;3:e000586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].El-Menyar A, Zubaid M, AlMahmeed W, et al. Killip classification in patients with acute coronary syndrome: insight from a multicenter registry. Am J Emerg Med 2012;30:97–103. [DOI] [PubMed] [Google Scholar]
- [19].Konstam MA, Kramer DG, Patel AR, et al. Left ventricular remodeling in heart failure: current concepts in clinical significance and assessment. JACC Cardiovasc Imaging 2011;4:98–108. [DOI] [PubMed] [Google Scholar]
- [20].Parakh K, Thombs BD, Bhat U, et al. Long-term significance of Killip class and left ventricular systolic dysfunction. Am J Med 2008;121:1015–8. [DOI] [PubMed] [Google Scholar]
- [21].Bermudez V, Rojas J, Salazar J, et al. Sensitivity and specificity improvement in abdominal obesity diagnosis using cluster analysis during waist circumference cut-off point selection. J Diabetes Res 2015;2015:750265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Herlitz J, Wireklintsundstrom B, Bang A, et al. Early identification and delay to treatment in myocardial infarction and stroke: differences and similarities. Scand J Trauma Resusc Emerg Med 2010;18:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Herlitz J, Thuresson M, Svensson L, et al. Factors of importance for patients’ decision time in acute coronary syndrome. Int J Cardiol 2010;141:236–42. [DOI] [PubMed] [Google Scholar]
- [24].Park YH, Kang GH, Song BG, et al. Factors related to prehospital time delay in acute ST-segment elevation myocardial infarction. J Korean Med Sci 2012;27:864–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].American Heart Association. Warning Signs of a Heart Attack. 2015. Available from: http://www.heart.org/HEARTORG/Conditions/HeartAttack/WarningSignsofaHeartAttack/Warning-Signs-of-a-Heart-Attack_UCM_002039_Article.jsp. Accessed October 6, 2015. [Google Scholar]
- [26].Park YK, Jeong J-O, Park JH, et al. Clinical impact of time delay on 1-year mortality in patients with ST-segment elevation myocardial infarction. Korean J Med 2011;81:199–207. [Google Scholar]
- [27].Kim JA, Jeong JO, Ahn KT, et al. Causative factors for time delays in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean J Med 2010;78:586–94. [Google Scholar]
- [28].Canto AJ, Kiefe CI, Goldberg RJ, et al. Differences in symptom presentation and hospital mortality according to type of acute myocardial infarction. Am Heart J 2012;163:572–9. [DOI] [PubMed] [Google Scholar]
- [29].Gao Y, Zhang HJ. The effect of symptoms on prehospital delay time in patients with acute myocardial infarction. J Int Med Res 2013;41:1724–31. [DOI] [PubMed] [Google Scholar]
- [30].Horne R, James D, Petrie K, et al. Patients’ interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart 2000;83:388–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].O’Donnell S, McKee G, O’Brien F, et al. Gendered symptom presentation in acute coronary syndrome: a cross sectional analysis. Int J Nurs Stud 2012;49:1325–32. [DOI] [PubMed] [Google Scholar]
- [32].DeVon HA, Penckofer S, Larimer K. The association of diabetes and older age with the absence of chest pain during acute coronary syndromes. West J Nurs Res 2008;30:130–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Ängerud KH, Thylén I, Lawesson SS, et al. Symptoms and delay times during myocardial infarction in 694 patients with and without diabetes; an explorative cross-sectional study. BMC Cardiovasc Disord 2016;16:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Dracup K, Alonzo AA, Atkins JM, et al. The physician's role in minimizing prehospital delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Ann Intern Med 1997;126:645–51. [DOI] [PubMed] [Google Scholar]
- [35].Riegel B, Dickson VV, Cameron J, et al. Symptom recognition in elders with heart failure. J Nurs Scholarsh 2010;42:92–100. [DOI] [PubMed] [Google Scholar]
- [36].Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke a scientific statement from the American heart association council on cardiovascular nursing and stroke council. Circulation 2006;114:168–82. [DOI] [PubMed] [Google Scholar]
- [37].Ghazawy ER, Seedhom AE, Mahfouz EM. Predictors of delay in seeking health care among myocardial infarction patients, Minia District, Egypt. Adv Prev Med 2015;2015:342361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Choudhary R, Sharma S, Kumar V, et al. An Observational study of prehospital and hospital delay in reperfusion for acute myocardial infarction at a University Hospital in India. J Pract Cardiovasc Sci 2016;2:163–8. [Google Scholar]
- [39].Henriksson C, Larsson M, Arnetz J, et al. Knowledge and attitudes toward seeking medical care for AMI-symptoms. Int J Cardiol 2011;147:224–7. [DOI] [PubMed] [Google Scholar]
- [40].Peng YG, Feng JJ, Guo LF, et al. Factors associated with prehospital delay in patients with ST-segment elevation acute myocardial infarction in China. Am J Emerg Med 2014;32:349–55. [DOI] [PubMed] [Google Scholar]
- [41].Zimmerman EB, Woolf SH, Haley A. Understanding the Relationship Between Education and Health: A Review of the Evidence and an Examination of Community Perspectives. 2015. Available from: https://www.ahrq.gov/professionals/education/curriculum-tools/population-health/zimmerman.html. Accessed June 11, 2017. [Google Scholar]
- [42].Ministry of Health and Welfare. Emergency Medical Services Plan 2013–2017. Seoul: Ministry of Health and Welfare; 2013. [Google Scholar]
- [43].Kim Y. Future agenda for emergency medical service in Korea: from silos to systems. J Korean Med Assoc 2015;58:776–9. [Google Scholar]
- [44].Fujii T, Masuda N, Suzuki T, et al. Impact of transport pathways on the time from symptom onset of ST-segment elevation myocardial infarction to door of coronary intervention facility. J Cardiol 2014;64:11–8. [DOI] [PubMed] [Google Scholar]
- [45].Davis LL. Determining time of symptom onset in patients with acute coronary syndromes: agreement between medical record and interview data. Dimens Crit Care Nurs 2015;34:222–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


