Abstract
Rationale:
Autoimmune encephalitis and Lambert–Eaton myasthenic syndrome are classic paraneoplastic neurological conditions common in patients with small cell lung cancer.
Patient concerns:
The patient complained of tiredness, fluctuating recent memory loss, and inability to find his home. His family members reported a change in character, irritability, and paranoia. One month later, the patient had 1 grand mal seizure lasting 5 minutes.
Diagnosis:
The patient was diagnosed with limbic encephalitis combined with Lambert–Eaton myasthenic syndrome. The gamma-aminobutyric acid B (GABAB) receptor and collapsin response mediator protein 5 (CRMP5, also called CV2) antibody test results were positive. Nine months after the onset of symptoms, the patient was diagnosed with small cell lung cancer.
Interventions:
The patient was administered intravenous immunoglobulin for 5 days. He was then treated with 60 mg prednisone once per day. The prednisone dose was gradually reduced by 1 tablet every 2 weeks. After the diagnosis, the patient underwent 6 courses of chemotherapy with cisplatin combined with sequential chemoradiation therapy.
Outcomes:
The patient was able to take care of himself. Neurological examination revealed a lower limb proximal muscle strength level of 4 and a reduced limb tendon reflex. The patient had deficits in short-term memory, a Mini-Mental State Examination score of 26, Montreal Cognitive Assessment score of 24, Self-rating Depression Scale score of 54 (mild depression), and Self-Rating Anxiety Scale score of 42 (normal).
Lessons:
Autoimmune diseases of the peripheral and central nervous systems can be observed at the same time in patients with small cell lung cancer, even when magnetic resonance imaging findings are negative and immune therapy is effective.
Keywords: anti-CRMP5/CV2 antibody, anti-GABAB receptor antibody, GABAB receptor associated encephalitis, Lambert–Eaton myasthenic syndrome, small cell lung cancer
1. Introduction
Anti-GABAB (γ-aminobutyric acid B) receptor encephalitis or “encephalitis associated with anti-GABAB receptor antibodies” is a type of autoimmune encephalitis associated with anti-neuronal cell surface antibodies, and accounts for approximately 5% of patients with autoimmune synaptic encephalitis.[1] The most characteristic manifestations of this disorder include early and prominent seizures, memory loss, confusion, hallucinations, and personality changes.[2–6] Approximately 50% of patients with this condition have an associated tumor, frequently small cell lung cancer (SCLC), or pulmonary neuroendocrine tumor.[6] Immunotherapy often results in good outcomes and relapse is uncommon.[7]
Anti-collapsin response mediator protein 5 (CRMP5, also called CV2) antibodies, which are paraneoplastic-specific antibodies, react with a 66-kDa brain protein of the Ulip/CRMP family.[8] Patients with anti-CRMP5 antibodies present with different disorders of the central and peripheral nervous systems commonly manifested as cerebellar ataxia, neuropathy, myelopathy, chorea, uveo/retinal symptoms, or myasthenic syndrome, such as Lambert–Eaton myasthenic syndrome (LEMS) and myasthenia gravis.[9] However, anti-CRMP5 antibodies rarely cause autoimmune encephalitis, as the prevalence of CRMP5 autoantibodies is 0.7/100,000 in patients with autoimmune encephalitis. SCLC is the most frequently found tumor in these patients.[10]
Here, we report the case of a patient presenting with muscle weakness, seizure, memory loss, confusion, and personality changes who had anti-CRMP5 and anti-GABAB receptor antibodies effectively treated with immune therapy. Nine months after onset of symptoms, the diagnosis of SCLC was confirmed and the patient underwent tumor treatment. He can now live on his own.
2. Case report
The current study was conducted according to the guidelines of the Ethical Committees of the Affiliated Hospital of Jining Medical University, China. Written informed consent was obtained from the patient.
A 56-year-old male patient was referred to the Affiliated Hospital of Jining Medical University, China in 2016. He complained of tiredness after walking for only 10 meters. He also presented with recent memory loss and could not find his home. The loss of memory occurred several times per day and lasted for 5 to 10 minutes each time. The patient's family members reported changes his character, irritability, and paranoia. One month later, the patient had 1 grand mal seizure lasting for 5 minutes. Four months later, the weakness in the legs had worsened. This symptom fluctuated during the day. Specifically, the patient was able to stand on his own, but could not squat in the morning. He was also tired and had difficulty walking. Neurological examination revealed a lower limb proximal muscle strength level of 3 and a decreased limb tendon reflex. The patient had a Mini-Mental State Examination (MMSE) score of 18, a Montreal Cognitive Assessment (MoCA) score of 16, a Self-Rating Depression Scale score of 54 (mild depression), and Self-Rating Anxiety Scale score of 45 (normal). He had a history of type 2 diabetes for 1 year, and long-term smoking (20/day for 30 years) and alcohol use (500 mL/day for 30 years). The patient's father died of multiple myeloma and his mother died of esophagus cancer.
Cranial magnetic resonance imaging (MRI) revealed no abnormalities. No epileptic discharge was found using electroencephalography. Electromyography revealed myogenic changes in all muscles tested. Repetitive stimulation of the left median and common peroneal nerves revealed significant decreases in compound muscle action potential (CMAP) of 11% and 39%, respectively, at low frequencies (3–5 Hz), and significant increases in CMAP of 11% and 118%, respectively, at high frequencies (10–50 Hz). Post-exercise stimulation of both ulnar nerves revealed a significant increase (118%) in CMAP, which was considered diagnostic of LEMS. Anti-GABAB receptor and anti-CRMP5 antibodies were found in serum (Fig. 1). Whole-body 18F-fludeoxyglucose (PDG) positron emission tomography (PET)/computed tomography (CT) and chest CT revealed no tumor signs.
Figure 1.
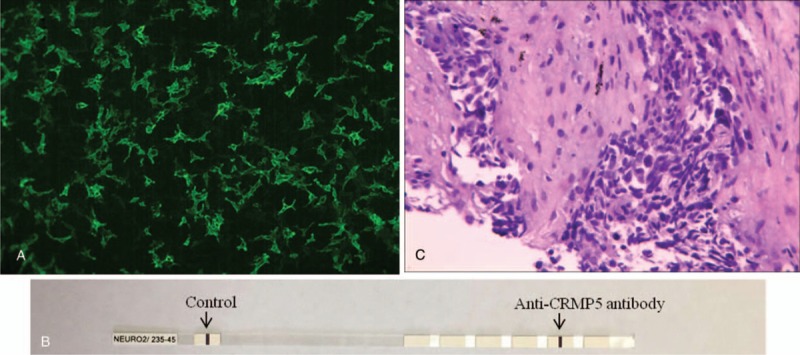
Antibody detection and histological analysis. (A) Anti-GABAB receptor antibody was detected by immunofluorescence. (B) Anti-CRMP5 antibody was detected by immunoblot. (C) small cell lung cancer was detected by hematoxylin-eosin staining.
The patient was diagnosed with limbic encephalitis combined with LEMS. He was treated with intravenous immunoglobulin for 5 days, followed by 60 mg of prednisone once per day. The prednisone dose was gradually reduced by 1 tablet every 2 weeks. The patient's symptoms improved following treatment. He was able to climb the stairs to the third floor and had no more seizures, although the change in character and short-term memory loss persisted.
Nine months after the onset of symptoms, whole-body FDG-PET and chest CT revealed a tumor in the hilus of the right lung. A subsequent bronchoscopic biopsy confirmed the diagnosis of SCLC (Fig. 1). The tumor was treated under the supervision of the oncology department. The patient was treated with 6 courses of chemotherapy with cisplatin and sequential chemoradiation therapy, followed by 1 course of chemotherapy with cisplatin every 3 months. At this time, the lower limb weakness has significantly improved and the patient can cook and take care of his grandchildren, and has returned to normal work. No seizures have occurred. The patient's temper has also improved following his release from the hospital. Neurological examination revealed a lower limb proximal muscle strength of 4 and a reduced limb tendon reflex. The patient has deficits in short-term memory, an MMSE score of 26, a MOCA score of 24, a Self-Rating Depression scale score of 54 (mild depression), and a Self-Rating Anxiety Scale score of 42 (normal).
3. Discussion
This case was unusual as antibodies against GABAB receptor and CRMP5 were observed in a patient with SCLC. Paraneoplastic neurologic disorders (most frequently LEMS, myasthenic syndrome, sensory neuronopathy, and limbic encephalitis) have been reported to be quite prevalent in patients with SCLC.[11] Dogan Onugoren et al[12] and Cho and Wymer[13] have described the concurrent presence of anti-GABAB receptor and anti-P/Q-type voltage-gated calcium channel antibodies in a patient with SCLC. However, the coexistence of anti-CRMP5 and anti-GABAB receptor antibodies in 1 patient with SCLC has never been reported.
GABAB receptors are mainly located in the presynaptic and postsynaptic regions of synapses in the hippocampus, thalamus, and cerebellum.[14,15] Mice lacking GABAB receptors develop epilepsy and deficits in memory, learning, and behavior.[2–6] Qiao et al[2] and Cui et al[4] have reported that, in China, patients with anti-GABAB receptor encephalitis are mainly male and have a median age at presentation of 60 years. Seizures, mental and behavioral disorders, and cognitive decline were reported as the most common manifestations, consistent with previous reports. Additional autoantibodies have been identified. About half of the cases of anti-GABAB receptor encephalitis are paraneoplastic in origin, with SCLC being the most commonly identified neoplasm.[2,4] In the elderly, especially those with a history of tobacco smoking, screening for lung cancer is important once the clinical diagnosis of anti-GABAB receptor encephalitis is confirmed.[11] Here, the patient had a long history of smoking and was diagnosed with SCLC 9 months after symptom onset. The central nervous system symptoms of the patient were similar to those in previously reported cases. The anti-GABAB receptor antibody does not have a target at the neuromuscular junction. We therefore speculate that the autoimmune encephalitis was associated with the presence of anti-GABAB receptor antibodies. Unilateral or bilateral medial temporal lobe and hippocampal MRI changes have been previously reported. However, it is accepted that imaging studies do not provide unique or specific information regarding the diagnosis of anti-GABAB receptor encephalitis.[2–4,16] In our patient, MRI findings were normal, which was consistent with previously reported cases. Therefore, negative MRI results do not exclude the possibility of this disease.
Anti-CRMP5 antibody is usually associated with paraneoplastic neurological syndrome and SCLC or thymoma.[9] Patients with anti-CRMP5 antibodies present with different disorders of the central and peripheral nervous systems. These symptoms frequently include cerebellar ataxia, uveo/retinal symptoms, chorea, neuropathy, and myasthenic syndrome, and less frequently include epilepsy.[9] Monstad and Nøstbakken[17] have reported the case of a patient with anti-CRMP5 antibodies with limbic encephalitis and myasthenia gravis. Meyronet et al[18] have reported that CRMP5 might be a specific marker for high-grade lung neuroendocrine carcinoma, although Qvale et al[19] have shown that only 1 of 379 (0.3%) smokers with chronic obstructive pulmonary disease have anti-CRMP5 antibodies. It was also reported that patients with anti-CRMP5 antibodies had better Rankin scores and longer median survival times.[20] Therefore, the role of anti-CRMP5 antibody in our patient was unclear, although it may have caused LE and LEMS.
As cerebrospinal fluid (CSF) from the patient was not available, we were unable to analyze the CSF for anti-GABAB receptor and anti-CRMP5 antibodies. However, the diagnosis of SCLC was confirmed after 9 months of follow-up, and the results obtained using serum support the general concept that specific antibodies predict the presence of an underlying tumor in paraneoplastic conditions.
4. Conclusion
The patient described here had muscle weakness, seizure, memory loss, confusion, and personality changes. He also had anti-CRMP5 and anti-GABAB receptor antibodies, and negative MRI findings. Immune therapy was effective in our patient. Nine months after the onset of symptoms, the diagnosis of SCLC was confirmed. The patient underwent 6 courses of chemotherapy with cisplatin combined with sequential chemoradiation therapy. He recovered well and currently lives on his own.
Acknowledgments
We would like to thank the patient for his participation in this study. We are grateful for Haitao Ren and Yanhuan Zhao from Department of Neurology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, who provided us with the guidance of the experimental technology.
Author contributions
Investigation: Hongfang Li.
Methodology: Aimei Zhang, Hongzhi Guan.
Validation: Yanlei Hao.
Writing – original draft: Zhanyun Lv.
Writing – review & editing: Zhanyun Lv.
Footnotes
Abbreviations: CMAP = compound muscle action potential, CRMP5 = collapsin response mediator protein 5, CSF = cerebrospinal fluid, CT = computed tomography, GABAB = γ-aminobutyric acid B, LEMS = Lambert–Eaton myasthenic syndrome, MMSE = Mini-Mental State Examination, MoCA = Montreal Cognitive Assessment, MRI = magnetic resonance imaging, PDG = 18F-fludeoxyglucose, PET = positron emission tomography, SCLC = small cell lung cancer.
Funding/support: This work was supported by grant 81401064 from the National Natural Science Foundation of China (to Dr. Zhanyun Lv), and grant [2016]56–62 from the Science and Technology Development Project of Jining City, Shandong Province, China (to Dr. Hongfang Li).
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- [1].Lancaster E, Martinez-Hernandez E. Encephalitis and antibodies to synaptic and neuronal cell surface proteins. Neurology 2011;77:179–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Qiao S, Zhang YX, Zhang BJ, et al. Clinical, imaging, and follow-up observations of patients with anti-GABAB receptor encephalitis. Int J Neurosci 2017;127:379–85. [DOI] [PubMed] [Google Scholar]
- [3].Chen X, Liu F, Li JM, et al. Encephalitis with antibodies against the GABAB receptor: seizures as the most common presentation at admission. Neurol Res 2017;39:973–80. [DOI] [PubMed] [Google Scholar]
- [4].Cui J, Bu H, He J, et al. The gamma-aminobutyric acid-B receptor (GABAB) encephalitis: clinical manifestations and response to immunotherapy. Int J Neurosci 2017;1–7. [DOI] [PubMed] [Google Scholar]
- [5].Graus F, Saiz A, Dalmau J. Antibodies and neuronal autoimmune disorders of the CNS. J Neurol 2010;257:509–17. [DOI] [PubMed] [Google Scholar]
- [6].Gozzard P, Woodhall M, Chapman C, et al. Paraneoplastic neurologic disorders in small cell lung carcinoma: a prospective study. Neurology 2015;85:235–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Höftberger R, Titulaer MJ, Sabater L, et al. Encephalitis and GABAB receptor antibodies: novel findings in a new case series of 20 patients. Neurology 2013;81:1500–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Fukada M, Watakabe I, Yuasa-Kawada J, et al. Molecular characterization of CRMP5, a novel member of the collapsin response mediator protein family. J Biol Chem 2000;275:37957–65. [DOI] [PubMed] [Google Scholar]
- [9].Dubey D, Lennon VA, Gadoth A, et al. Autoimmune CRMP5 neuropathy phenotype and outcome defined from 105 cases. Neurology 2018;90:e103–10. [DOI] [PubMed] [Google Scholar]
- [10].Dubey D, Pittock SJ, Kelly CR, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol 2018;83:166–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 2016;15:391–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dogan Onugoren M, Rauschka H, Bien CG. Conjoint occurrence of GABAB receptor antibodies in Lambert-Eaton myasthenic syndrome with antibodies to the voltage gated calcium channel. J Neuroimmunol 2014;273:115–6. [DOI] [PubMed] [Google Scholar]
- [13].Cho JJ, Wymer JP. Paraneoplastic Lambert-Eaton Myasthenic syndrome with limbic encephalitis: clinical correlation with the coexistence of anti-VGCC and anti-GABAB receptor antibodies. J Clin Neuromuscul Dis 2017;19:84–8. [DOI] [PubMed] [Google Scholar]
- [14].Wu XH, Song JJ, Faull RLM, et al. GABAA and GABAB receptor subunit localization on neurochemically identified neurons of the human subthalamic nucleus. J Comp Neurol 2018;526:803–23. [DOI] [PubMed] [Google Scholar]
- [15].Sheilabi MA, Battacharyya D, Caetano L, et al. Quantitative expression and localization of GABAB receptor protein subunits in hippocampi from patients with refractory temporal lobe epilepsy. Neuropharmacology 2017;pii: S0028-3908(17)30368-4. [DOI] [PubMed] [Google Scholar]
- [16].Su M, Xu D, Tian R. (18)F-FDG PET/CT and MRI findings in a patient with anti-GABA(B) receptor encephalitis. Clin Nucl Med 2015;40:515–7. [DOI] [PubMed] [Google Scholar]
- [17].Monstad SE, Nøstbakken JK. CRMP5 antibodies found in a patient with limbic encephalitis and myasthenia gravis. J Neurol Neurosurg Psychiatry 2009;80:241–2. [DOI] [PubMed] [Google Scholar]
- [18].Meyronet D, Massoma P, Thivolet F, et al. Extensive expression of collapsin response mediator protein 5 (CRMP5) is a specific marker of high-grade lung neuroendocrine carcinoma. Am J Surg Pathol 2008;32:1699–708. [DOI] [PubMed] [Google Scholar]
- [19].Qvale TH, Storstein A, Mazengia K, et al. Paraneoplastic Hu and CRMP5 antibodies are present in smokers without cancer or neurological disease. Respirology 2014;19:730–4. [DOI] [PubMed] [Google Scholar]
- [20].Honnorat J, Cartalat-Carel S, Ricard D, et al. Onco-neural antibodies and tumour type determine survival and neurological symptoms in paraneoplastic neurological syndromes with Hu or CV2/CRMP5 antibodies. J Neurol Neurosurg Psychiatry 2009;80:412–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


