Abstract
Objectives
In 2013, the majority of women lived in states considered hostile to abortion rights, or states with numerous abortion restrictions. By comparison, 31% lived in supportive states. This study examined differences in abortion service delivery according to the policy climate in which clinics must operate.
Methods
Data come from the 2014 Abortion Provider Census, which contains information about all known abortion-providing facilities in the United States. In addition to number and type of facility, we examine several aspects of abortion care: provision of only early medication abortion (EMA-only) whether an advanced practice clinician provided abortions, gestational parameters, and average charge for procedure. All indicators were examined nationally and according to whether the clinic was in a state that was hostile, middle ground, or supportive of abortion rights.
Results
In 2014, hostile and supportive states accounted for the same proportion of all U.S. abortions—44% (each) —although 57% of women age 15 to 44 lived in hostile states. Hostile states had one-half as many abortion-providing facilities as supportive ones. EMA-only facilities accounted for 37% of clinics in supportive states compared with 8% in hostile states. Sixty-five percent of clinics in supportive states reported that advanced practice clinicians provided abortion care, compared with 3% in hostile states. After cost of living adjustments, a first-trimester surgical abortion was most expensive in middle-ground states ($470) and least expensive in supportive states ($402).
Conclusions
The distribution of abortion services, the type of facility in which they are provided, and the amount a facility charges all vary according to the abortion policy climate.
Over the last decade states have passed an unprecedented number of laws regulating abortion. In 2013, 56% of U.S. women lived in a state considered hostile to abortion rights, up from 31% in 2000 (Boonstra & Nash, 2014). During this same time period, the proportion of women living in states considered to be supportive of abortion rights decreased from 40% to 31%.
Between 2011 and 2014, the U.S. abortion rate decreased by 14%, and the number of clinics providing abortion care in the United States decreased by 6% (Jones & Jerman, 2017). Decreases in clinic numbers were greatest in those regions of the United States that passed the most abortion laws (the Midwest and the South); associations between abortion restrictions, number of clinics, and abortion rates were not uniform across states (Jones & Jerman, 2017). The decline in unintended pregnancy also contributed to the decrease in abortion (Finer & Zolna, 2016) and, likely, the decrease in clinic numbers; this may be one reason abortion incidence and number of clinics declined in states that are supportive of abortion rights. But state abortion policies influence more than the number of clinics in a state. Many abortion restrictions are not necessarily meant to close clinics, but to limit service options; these include laws pertaining to health insurance, early medication abortion (EMA), and those designating which health care professionals can provide abortion care. Thus, the types of abortion care offered may vary according to policy climate, because some regulations are specifically intended to impact service delivery.
In 2014, there were 1,671 facilities known to provide abortion care (Jones & Jerman, 2017). Clinics accounted for the largest share, 47%, followed by hospitals and physicians’ offices, at 38% and 15% respectively. Prior research has found that there were fewer hospitals and doctors’ offices providing abortion in the Midwest and the South in 2011, and it is likely that the distribution of abortion-providing facilities also varies across policy climates (Jerman & Jones, 2014). For example, physicians in private practice in hostile states with numerous regulations may not have the resources to meet all these requirements, and there may be fewer of them providing abortions.
The last decade has seen the emergence of a new type of clinic. EMA is offered by the overwhelming majority of clinics providing abortion care and accounted for 31% of abortions in 2014 (Jones & Jerman, 2017). That same year, 23% of nonhospital abortion providers offered only EMA (EMA-only; Jones & Jerman, 2017), although little else is known about these clinics. A majority of states have passed laws intended to make medication abortion more difficult to access. For example, 34 states mandate that only licensed physicians can provide medication abortion, and 19 require that the clinician be physically present when the primary abortion drug is administered (Guttmacher Institute, 2017). In turn, we expect EMA-only facilities will be less common in hostile states.
A majority of states only allow licensed physicians to perform abortions (Guttmacher Institute, 2014a). Many physician-only laws were implemented shortly after abortion was legalized to prevent unlicensed health care providers from performing abortions. However, since that time, nurse practitioners, nurse-midwives, and physician assistants (referred to as advanced practice clinicians [APCs]), have become integrated into the U.S. health care system, including the field of family planning (Auerbach et al., 2012; Fowler, Gable, Wang, & Lasater, 2016). Recent years have seen increased efforts to involve APCs in abortion care (Barry & Rugg, 2015; Weitz et al., 2013; Weitz, Anderson, & Taylor, 2009), and the availability of medication abortion may have bolstered these efforts. Although only five states currently allow APCs to perform surgical abortions, at least 12 additional states allow them to provide medication abortion (Barry & Rugg, 2015; Guttmacher Institute, 2014a). No national study has examined the involvement of APCs in abortion care. Still, because a majority of states mandate that abortion, including medication abortion, can be provided only by a licensed physician, we expect that APC involvement in abortion care will be more common in supportive states.
How much women have to pay for abortion care may also be influenced by state policy climate. Restrictions such as waiting periods or ones that require major structural changes to a clinic can result in substantial expenses (Colman & Joyce, 2011; Mercier, Buchbinder, Bryant, & Britton, 2015; Mercier, Buchbinder, & Bryant, 2016), and facilities located in states with numerous restrictions might have to charge more for care to compensate for these costs. Some 75% of patients who obtain abortions are poor or low income (Jones, Jerman, & Onda, 2016). In 2011 and 2012 the average patient paid $480 for a first-trimester surgical procedure (Jerman & Jones, 2014). Because many patients are uninsured or have insurance that does not cover abortion, the majority pay out of pocket (Jones et al., 2016). Women who are unable to come up with this money may not be able to obtain abortions.
Finally, a majority of states, including some considered supportive of abortion rights, have imposed gestational limits on abortion, typically between 20 and 24 weeks (Guttmacher Institute, 2014b). Thus, it is unclear whether we might expect variations in the availability of abortion at later gestations by policy context. At the other end of the spectrum, more providers have been able to offer abortions at very early gestations over the last decade, in part owing to the integration of EMA (Hammond & Chasen, 2009, p. 11; Henshaw, 2009). We might expect greater availability of very early abortion in states with fewer restrictions and greater availability of EMA-only facilities.
This study uses data from all known U.S. abortion-providing facilities to examine several indicators of abortion care according to whether the facility was in a state that was characterized as hostile, middle ground, or supportive on abortion rights. The information from this study expands on the absolute number of clinics as a measure of access, and provides a more nuanced examination of abortion service delivery.
Methods
Data for this cross-sectional study come from the Guttmacher Institute’s 2014 Abortion Provider Census. Since 1973, the census has surveyed the known universe of abortion-providing facilities in the United States, and constitutes the most comprehensive information on abortion incidence. We obtained approval for the census through expedited review by the Guttmacher Institute’s federally registered institutional review board. Detailed information on methodology has been documented elsewhere (Jones & Jerman, 2017), but we provide a brief description.
Paper questionnaires were mailed to all known abortion providing facilities in March 2015. Completed questionnaires were collected through April 2016 via mail and, during nonresponse follow-up, by telephone, fax, and email. Questionnaires included items about the number of abortions provided in 2013 and 2014 (with separate questions for number of medication abortions), the minimum and maximum gestations at which abortions were provided in 2014, and the typical fee schedules for EMA and surgical procedures at 10 and 20 weeks in 2014. For the first time we asked facilities, “In 2014, were any abortions at this facility provided by an APC, such as a physician assistant, nurse practitioner, family nurse practitioner, women’s health nurse practitioner, or certified midwife?” and this measure is included in the current analysis.
Data on number of abortions was provided by 58% of all facilities. Health department data were used to determine abortion caseloads for an additional 20% of facilities, and estimates were made for the remaining 17%. The vast majority of counted abortions—88%—came from information given to us directly by abortion providers.
Although we surveyed all known abortion providing facilities and were able to obtain, or estimate, information on number of abortions for all of them, questionnaires were sometimes incomplete. For some facilities, we were able to obtain additional information over the phone and from facility websites (e.g., fee schedules). We acquired at least some information on gestational limits from 85% of clinics and information on charges from 84% of clinics. We constructed nonresponse weights that accounted for these differences based on facility type and caseload, assuming that nonresponding facilities resembled those that provided the relevant information.
The weight used for amount a facility charged for first-trimester abortions was adjusted for clinic caseload as well as nonresponse. A small number of clinics charge substantially higher prices for abortions (Jerman & Jones, 2014), and these facilities typically serve a small number of clients. The inclusion of facility caseload into the weight prevented these facilities from skewing the amount charged; the measure used in the analysis represents the amount women paid for an abortion. Because abortions at 20 weeks are much less common than those performed at earlier gestations, we did not weight this variable by number of patients; the measure refers to amount charged. Additionally, we applied county-level cost of living adjustments to these amounts (Council for Community and Economic Research, 2016) when comparing across groups of states to account for the fact that some supportive states have a substantially higher cost of living (e.g., New York, California) than states in the Midwest and the South.
We distinguish between four types of abortion facilities: abortion clinics, nonspecialized clinics, hospitals, and physicians’ offices. Abortion clinics are facilities where 50% or more of patient visits in 2014 were for abortion care. Nonspecialized clinics are sites where fewer than 50% of patient visits were for abortion services; these include physicians’ offices that provided 400 or more abortions per year. Facilities that provided fewer than 400 abortions per year and had names suggesting that they were physicians’ private practices were categorized as physicians’ offices.
For this analysis, we also distinguish between EMA-only clinics and those that provided surgical abortion (including those that also provided EMA). Clinics were classified as EMA only when the total number of reported abortions provided in 2014 was equal to the total number of EMAs provided in that year. An additional six clinics were classified as EMA only despite small differences between these two figures (by a count of 4 or less) because they had indicated on the questionnaire that they only provided medication abortion. We assumed the slight discrepancy in the abortion figures was a reporting error.
We rely on analyses from the Guttmacher Institute to categorize states as occupying one of three policy landscapes as it pertains to abortion: supportive, middle ground, or hostile (Gold & Nash, 2012). This categorization scheme is based on 10 categories of major abortion restrictions in 2014. States that enacted restrictions in 1 or fewer of the 10 categories were considered supportive; states that enacted provisions in 2 or 3 of the 10 categories were considered “middle ground”; and states that enacted restrictions in 4 or more of the 10 areas were considered “hostile.” Two states could have the same number of abortion restrictions but considered to be under different policy climates. For example, a state that had in place a parental involvement law that required both notification and consent, but no other abortion restrictions, would be classified as supportive, whereas a state that had only a parental notification law but also required medically inaccurate preabortion counseling would be classified as middle ground. Twenty-seven states were classified as hostile, 12 states as middle ground, and 11 states as supportive (Table 1). The District of Columbia was excluded because it is more comparable to a city than a state.
Table 1.
States by Policy Climate
| Hostile | |
| Alabama | Nebraska |
| Arizona | North Carolina |
| Arkansas | North Dakota |
| Florida | Ohio |
| Georgia | Oklahoma |
| Idaho | Pennsylvania |
| Indiana | Rhode Island |
| Kansas | South Carolina |
| Kentucky | South Dakota |
| Louisiana | Tennessee |
| Michigan | Texas |
| Mississippi | Utah |
| Missouri | Virginia |
| Wisconsin | |
| Middle ground | |
| Alaska | Nevada |
| Colorado | New Hampshire |
| Delaware | West Virginia |
| Illinois | Wyoming |
| Iowa | |
| Massachusetts | |
| Minnesota | |
| Montana | |
| Supportive | |
| California | New Jersey |
| Connecticut | New Mexico |
| Hawaii | New York |
| Maine | Oregon |
| Maryland | Vermont |
| Washington |
Note: District of Columbia is excluded.
We assessed the proportion of women aged 15 to 44 years who were living under each policy climate using data from Census Bureau population data estimates for July 1, 2014 (National Center for Health Statistics, 2015).
We first examine the distribution of abortion-providing facilities and number of abortions, both by provider type and according to abortion policy climate. Because the overwhelming majority of abortions were provided by clinics in all three groups of states, subsequent analyses were restricted to clinic facilities. We next examined the distribution of EMA-only facilities and facilities where APCs provided care, gestational parameters, and average amount paid. All indicators were assessed nationally and according to policy climate. Weights to adjust for nonresponse were used in analysis of EMA, provision by APCs, gestational limits, and cost. Because this is a descriptive study, we did not incorporate significance testing.
Results
Distribution of Abortion-providing Facilities
Hostile and supportive states accounted for approximately the same number and proportion of abortions in 2014 (44%), but supportive states had more than twice as many abortion-providing facilities (Table 2). This was partially due to the fact that there were more hospitals and physicians providing abortions in supportive states. Clinic facilities accounted for 64% of providers in hostile states, compared with 39% in supportive states, but the latter still had more clinic facilities than hostile states (409 vs 271, respectively). Middle-ground states fell in between, and a slight majority of facilities were clinics (52%).
Table 2.
Distribution of Abortion-providing Facilities and Abortions
| Total | Hostile | Middle ground | Supportive | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| N | % | n | % | n | % | n | % | |
| Number and distribution of facilities | 1,662 | 100 | 423 | 25 | 195 | 12 | 1,044 | 63 |
| Facility type | ||||||||
| Abortion clinic | 270 | 16 | 151 | 36 | 36 | 18 | 83 | 8 |
| Nonspecialized clinic | 513 | 31 | 120 | 28 | 67 | 34 | 326 | 31 |
| Hospital | 634 | 38 | 125 | 30 | 59 | 30 | 450 | 43 |
| Physicians’ offices | 245 | 15 | 27 | 6 | 33 | 17 | 185 | 18 |
| Number and distribution of abortions | 920,376 | 100 | 404,374 | 44 | 112,397 | 12 | 403,605 | 44 |
| Facility type | ||||||||
| Abortion clinic | 542,498 | 59 | 304,449 | 75 | 62,130 | 55 | 175,919 | 44 |
| Nonspecialized clinic | 330,917 | 36 | 94,042 | 23 | 44,422 | 40 | 192,453 | 48 |
| Hospital | 34,034 | 4 | 3,547 | 1 | 4,344 | 4 | 26,143 | 7 |
| Physicians’ offices | 12,927 | 1 | 2,336 | 1 | 1,501 | 1 | 9,090 | 2 |
| Percent distribution of all U.S. women 15–44 | 100 | 57 | 13 | 30 | ||||
Similar patterns applied to the number of abortions by facility type, although the differences were much less pronounced. In all three policy climates, the overwhelming majority of abortions were provided by clinics: 98% in hostile, 95% in middle-ground, and 92% in supportive states. However, there were notable differences by clinic type. Clinics specializing in abortion services provided 75% of abortions in hostile states, compared with 55% in middle-ground and 44% in supportive states. The largest share of abortions in supportive states was provided by nonspecialized clinics (48%). Finally, although hostile and supportive states accounted for an equal proportion of all abortions, the majority of U.S. women of reproductive age lived in hostile states (57%) and less than one-third (30%) resided in supportive states.
Given the important role of clinics in all three policy climates, subsequent analyses were limited to these facilities and do not include hospitals or physicians’ offices.
Aspects of Service Delivery
In 2014, 26% of clinic facilities provided only EMA (Table 3). This proportion was highest in supportive states (37%), although nearly one-third of clinics in middle-ground states were EMA only. In hostile states, 8% of clinics were EMA-only facilities. A higher proportion of nonspecialized clinics offered EMA only than abortion clinics, regardless of the policy climate.
Table 3.
Distribution of EMA-only Clinics and Clinics with APCs
| All Clinics | EMA-only Clinics | Some Care Provided by APC | |
|---|---|---|---|
|
|
|
|
|
| N | % | % | |
| Total | 783 | 26 | 40 |
| Abortion clinics | 270 | 2 | 10 |
| Nonspecialized clinics | 513 | 39 | 57 |
| Hostile | 271 | 8 | 3 |
| Abortion clinics | 151 | 2 | 1 |
| Nonspecialized clinics | 120 | 16 | 9 |
| Middle ground | 103 | 32 | 29 |
| Abortion clinics | 36 | 6 | 17 |
| Nonspecialized clinics | 67 | 46 | 35 |
| Supportive | 409 | 37 | 65 |
| Abortion clinics | 83 | 0 | 27 |
| Nonspecialized clinics | 326 | 46 | 74 |
Abbreviations: APCs, advanced practice clinicians; EMA, early medication abortion.
Some 40% of clinic facilities reported that at least some abortions were provided by an APC (Table 3). This was much more common in nonspecialized than abortion clinics, 57% and 10%, respectively. There were notable variations by policy climate. Only 3% of facilities in hostile states had APCs that provided care; this increased to 29% in middle-ground states and 65% in supportive states. In all three policy climates, APCs were more common in nonspecialized clinics.
APC and EMA-only facilities overlapped substantially. The majority of facilities where APCs provided at least some abortion care were EMA-only clinics (57%), and 70% of EMA-only facilities reported that APCs provided at least some abortion care (data not shown). Still, even when EMA-only facilities were excluded, APCs in supportive states provided abortion care in 48% of clinic facilities (that provided surgical and medication abortion or only surgical abortion care).
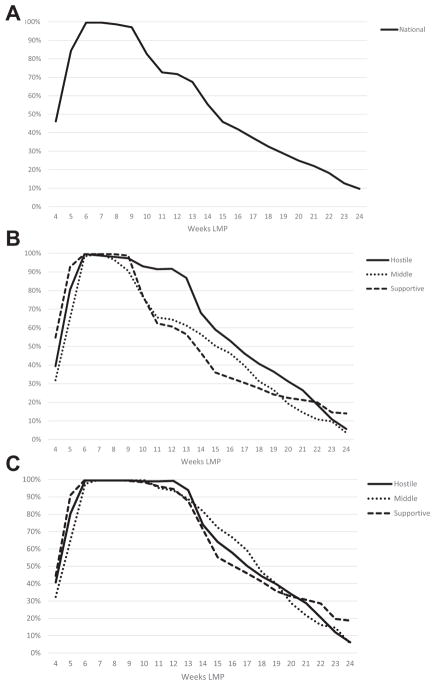
Virtually all clinics provided abortions at 6 to 8 weeks gestation, and 84% offered them at 5 weeks (Figure 1A). Provision started gradually decreasing at 10 weeks (83%), and only 25% of clinics offered abortions at 20 weeks gestation.
Figure 1.
(A) Percentage of clinics performing abortions, by gestational age at which abortions were performed in 2014. (B) Percentage of clinics performing abortions, by gestational age at which abortions were performed, according to policy climate, 2014. (C) Percentage of clinics (excluding early medication abortion-only facilities) performing abortions, by gestational age at which abortions were performed, according to policy climate, 2014. Abbreviation: LMP, last menstrual period.
Patterns of abortion provision by gestational parameters were variable by policy climate (Figure 1B). Very early abortions, or those at 4 or 5 weeks gestation, were offered by a higher proportion of clinics in supportive states than in middle-ground or hostile ones. Although virtually all clinic facilities in all three policy climates offered abortions at 6 to 9 weeks gestation, patterns diverged at 10 weeks. In particular, compared with supportive and middle-ground states, a higher proportion of clinics in hostile states offered abortion care at 10 to 22 weeks. A slightly higher proportion of clinics in supportive states offered abortions after 22 weeks.
We anticipated that the skewed distribution in hostile states was due to the higher number of EMA-only facilities in supportive states. When these facilities were excluded, the proportion of clinics providing abortions at the earliest gestations and between 10 and 22 weeks was much more similar across the three groups (Figure 1C).
In 2014, abortion patients paid an average of $508 for a surgical abortion at 10 weeks gestation, and there were notable differences according to policy climate (Table 4). The unadjusted figures suggest that women in supportive states paid more for a first-trimester surgical procedure than women in hostile states. However, the pattern was reversed when the cost of living adjustment was applied: women paid $40 more in hostile ($442) than in supportive ($402) states. Women in middle-ground states paid the most, regardless of which figure was used.
Table 4.
Average Amount Patients Paid for Surgical Abortion at 10 Weeks Gestation and for EMA
| Paid, Mean (range) | ||||
|---|---|---|---|---|
|
| ||||
| Total | Hostile | Middle ground | Supportive | |
| Surgical abortion at 10 weeks | 508 (75–2500) | 473 (250–750) | 551 (75–2500) | 533 (295–1600) |
| With cost of living adjustment | 442 | 470 | 402 | |
| EMA at 10 weeks | 535 (75–1633) | 514 (165–825) | 531 (75–1633) | 557 (100–1500) |
| With cost of living adjustment | 479 | 457 | 419 | |
| EMA-only facilities | 562 (300–1633) | 515 (400–700) | 522 (315–1633) | 577 (300–1500) |
| With cost of living adjustment | 488 | 487 | 454 | |
Abbreviation: EMA, early medication abortion.
Women paid an average of $535 for an EMA in 2014, $27 more than a first-trimester surgical procedure. According to figures adjusted for cost of living, this procedure cost most in hostile states ($479) and least in supportive ones ($419). On average, women paid $27 more for medication abortion at EMA-only facilities than at facilities that also offered surgical abortion. This pattern was consistent across the three policy climates, ranging from $9 more in hostile states to $35 more in supportive ones (according to the adjusted figures).
Abortions at later gestational lengths require greater technical skills and resources, and, in turn, cost more (Hammond & Chasen, 2009, p. 11). In 2014, the median charge for an abortion at 20 weeks gestation was $1,195 (data not shown). Clinics in hostile states charged the most, at $1,350 (adjusted for cost of living), and clinics in supportive states charged the least, at $964; clinics in middle-ground states charged slightly less than hostile states at $1,158.
Discussion
Some of the restrictions used to categorize whether states were supportive or hostile toward abortion were intended to directly impact some of the indicators examined in this study. So it is not surprising, for example, that APCs provided abortions at a greater proportion of clinics in supportive states. However, this is the first study to document several of the outcomes examined this study, including differences by policy climate.
Number of and type of abortion-providing facilities and service delivery varied substantially by state policy climate. Hostile and supportive states each accounted for 44% of abortions in 2014, but a substantially larger proportion of women of reproductive age lived in hostile states. Hostile states had one-half as many abortion-providing facilities as supportive states, including fewer clinic facilities. That a smaller number of clinics had to serve a larger number of patients means that some women in these states had to travel further to access care (Bearak, Burke, & Jones, 2017).
Compared with supportive and middle-ground states, a greater proportion of abortion providing facilities in hostile states were accounted for by clinics specializing in abortion care; these facilities also accounted for three-quarters of abortions in hostile states. The concentration of abortion services in hostile states make these facilities more vulnerable to legislation that interferes with a clinic’s ability to operate. For example, if a clinic in a hostile state closes because of a new law requiring admitting privileges, this change will likely have a greater impact than the closure of a clinic in a supportive state.
The type of abortion services available differed by policy climate. We found more than one-third of clinics in supportive states provided only EMA, compared with 8% in hostile states. Indeed, without these EMA-only facilities, supportive states would have had slightly fewer clinics than hostile states. However, we cannot assume EMA-only facilities increase access to care for all women. Women who would prefer a surgical abortion, or are too late in the pregnancy for a medication abortion, would be unable to obtain services at EMA-only facilities. This factor could pose an obstacle if a surgical provider is not nearby.
APCs’ involvement in abortion care differed by policy climate. Nationally, 40% of clinics reported that APCs provided at least some abortions. APCs were involved in abortion care in approximately two-thirds of clinics in supportive states, compared with 3% in hostile ones, and this pattern corresponds with a recent study finding that APC provision of medication abortion was substantially higher in the Eastern and Western United States than in the South and Midwest (Jones et al., 2017). These patterns are likely a direct consequence of abortion restrictions combined with the impact of state practice regulations. A majority of hostile (and middle-ground) states have laws mandating that abortions can only be provided by a licensed physician (Guttmacher Institute, 2014a). By contrast, states that have granted APCs the authority to provide abortions, particularly early medication procedures, are disproportionately ones with supportive policy climates (Barry & Rugg, 2015). We found that APCs were concentrated in EMA-only clinics, and most EMA-only facilities had APCs who provided at least some abortion care. These patterns suggest that the legal ability of APCs to provide EMA in some nonhostile states contributes to the greater number of EMA-only facilities in those states. We also found that APCs provide abortions in nearly one-half of clinics in supportive states that also provide surgical abortions. Thus, they may increase access to abortion care in general, for example, by allowing facilities to add more abortion service days.
A lesser proportion, and smaller number, of clinics in hostile and middle-ground states provided abortions after 22 weeks gestation compared with supportive ones. The majority of hostile states had laws that banned abortions after 20 weeks post-fertilization (akin to 22 weeks gestation; Guttmacher Institute, 2014b). This restriction means that women seeking later abortions in these states were only able to access care if they traveled to another state. It is also worth noting that, even in supportive states, only 20% of clinics offered abortions after 22 weeks gestation, and women needing later abortions may have had to travel substantial distances even in these states.
On average, abortion patients had to pay $508 for a first-trimester surgical procedure and $535 for an EMA; these amounts were comparable with those paid by patients in 2012, after adjusting for inflation (Jerman & Jones, 2014). It first seemed that women paid less for first-trimester surgical and medication abortion in hostile states than in middle-ground or supportive ones. However, once we adjusted for cost of living differences, the patterns were reversed; regardless of procedure type, abortion cost less in supportive than in hostile states. Meeting state abortion requirements such as providing in-person counseling and converting to Ambulatory Surgical Centers can be expensive (Colman & Joyce, 2011; Mercier et al., 2015; Mercier et al., 2016), and presumably some of these costs are passed on to patients in hostile states. Moreover, a greater reliance on APCs in supportive states may reduce the cost of care compared with facilities that relied almost exclusively on physicians. More research is needed to better understand the dynamics that influence how much clinics charge for abortions and why this is so variable, even among clinics operating within the same policy climate.
This study has several shortcomings. The number of abortions was measured according to state of occurrence. Some women in hostile states may have obtained abortions in supportive states to avoid regulations such as waiting periods or because the out-of-state clinic was closer. However, many women in hostile states who go out of state obtain abortions in neighboring states that are also hostile (Jatlaoui et al., 2016), and we do not anticipate that data by state of residence would substantially alter the findings. We did not obtain data on gestational limits or cost of care from 15% to 16% of clinic facilities. Weights were constructed to adjust for nonresponse, but these figures may still be inaccurate if nonresponding facilities were substantially different on these characteristics. We applied a county-level cost of living adjustment to account for the fact that urban areas in supportive states have a higher cost of living. However, this adjustment assumes that abortion pricing responds and adheres to the same market dynamics as other goods and services. Prior research suggests that this may not be the case (Dennis, Blanchard, & Córdova, 2011; Kimport & Rowland, 2017). Although the survey attempted to identify all abortion-providing facilities, it is expected that some hospitals and physicians’ offices were not captured (Jones & Jerman, 2017). If these providers were concentrated in one of the groups of states examined in this study—for example, if physicians’ offices and hospitals in hostile states were unwilling to acknowledge they provided abortion care—this could alter our findings. (Table 1). Finally, data are for abortion services in 2014, and it is possible that the indicators and measures used in the analysis are out of date. Still, we expect that the patterns by policy landscape are still applicable.
Implications for Policy and/or Practice
This study revealed some of the ways that state abortion restrictions directly and indirectly influence service delivery. The findings suggest that EMA still has the potential to increase access to abortion care in the United States. Developments such as the integration of nurse practitioners, midwives, and physician assistants into abortion care; the increase in EMA-only facilities; and the provision of medication abortion by telemedicine all have the potential to allow more women to access abortion earlier. However, it is unlikely these strategies will be pursued in the states where they are most needed, and hostile ones in particular, until restrictive laws are removed.
Acknowledgments
The authors thank Elizabeth Nash for assistance with state policy documentation, and Megan Donovan, Lawrence B. Finer, Rachel Benson Gold, Kathryn Kost, and Elizabeth Nash for reviewing early versions of this article. The data analysis and summary were supported by a grant from the Susan Thompson Buffett Foundation.
References
- Auerbach DI, Pearson ML, Taylor D, Battistelli M, Sussell J, Hunter LE, Schneider EC. Nurse Practitioners and Sexual and Reproductive Health Services. Santa Monica, CA: RAND Corporation; 2012. [Accessed: January 3, 2018]. Available: https://www.rand.org/pubs/technical_reports/TR1224.html. [PMC free article] [PubMed] [Google Scholar]
- Barry D, Rugg J. Improving abortion access by expanding those who provide care. Washington, DC: Center for American Progress; 2015. [Accessed: January 3, 2018]. Available: https://www.americanprogress.org/issues/women/reports/2015/03/26/109745/improving-abortion-access-by-expanding-those-who-provide-care/ [Google Scholar]
- Bearak JM, Burke KL, Jones RK. Disparities and change over time in distance women would need to travel to have an abortion in the USA: A spatial analysis. Lancet Public Health. 2017;2(11):e493–e500. doi: 10.1016/S2468-2667(17)30158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boonstra HD, Nash E. A surge of state abortion restrictions puts providers—And the women they serve—In the crosshairs. Guttmacher Policy Review. 2014;17(1):1–7. [Google Scholar]
- Colman S, Joyce T. Regulating abortion: Impact on patients and providers in Texas. Journal of Policy Analysis and Management. 2011;30(4):775–797. [Google Scholar]
- Council for Community and Economic Research. [Accessed: September 19, 2017];Cost of living index. 2016 Available: http://coli.org/about/
- Dennis A, Blanchard K, Córdova D. Strategies for securing funding for abortion under the Hyde Amendment: A Multistate study of abortion providers’ experiences managing Medicaid. American Journal of Public Health. 2011;101(11):2124–2129. doi: 10.2105/AJPH.2011.300212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. New England Journal of Medicine. 2016;374(9):843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler C, Gable J, Wang J, Lasater B. Family planning annual report: 2015 National summary. Research Triangle Park, NC: RTI International; 2016. [Google Scholar]
- Gold RB, Nash E. Troubling trend: More states hostile to abortion rights as middle ground shrinks. Guttmacher Policy Review. 2012;15(1):1–6. [Google Scholar]
- Guttmacher Institute. State policies in brief: An overview of abortion laws. Washington, DC: Guttmacher Institute; 2014a. pp. 1–4. [Google Scholar]
- Guttmacher Institute. State policies in brief: State policies on later abortions. Washington, DC: Guttmacher Institute; 2014b. pp. 1–4. [Google Scholar]
- Guttmacher Institute. State policies in brief: Medication abortion. Washington, DC: Guttmacher Institute; 2017. pp. 1–3. [Google Scholar]
- Hammond C, Chasen S. Dilation and evacuation. In: Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD, editors. Management of unintended and abnormal pregnancy: Comprehensive abortion care. Oxford, UK: Blackwell Publishing Ltd; 2009. [Accessed: January 3, 2018]. Available: http://onlinelibrary.wiley.com/doi/10.1002/9781444313031.ch11/summary. [Google Scholar]
- Henshaw SK. Unintended pregnancy and abortion in the USA: Epidemiology and public health impact. In: Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD, editors. Management of unintended and abnormal pregnancy: Comprehensive abortion care. Oxford, UK: Blackwell Publishing Ltd; 2009. [Accessed: January 3, 2018]. Available: http://onlinelibrary.wiley.com/doi/10.1002/9781444313031.ch3/summary. [Google Scholar]
- Jatlaoui TC, Ewing A, Mandel MG, Simmons KB, Suchdev DB, Jamieson DJ, Pazol K. Abortion surveillance — United States, 2013. MMWR Surveillance Summaries. 2016;65(12):1–44. doi: 10.15585/mmwr.ss6512a1. [DOI] [PubMed] [Google Scholar]
- Jerman J, Jones RK. Secondary Measures of access to abortion services in the United States, 2011 and 2012: Gestational age limits, cost, and harassment. Women’s Health Issues. 2014;24(4):e419–e424. doi: 10.1016/j.whi.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones HE, O’Connell White K, Norman WV, Guilbert E, Lichtenberg ES, Paul M. First trimester medication abortion practice in the United States and Canada. PloS One. 2017;12(10):e0186487. doi: 10.1371/journal.pone.0186487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RK, Jerman J. Abortion incidence and service availability in the United States, 2014. Perspectives on Sexual and Reproductive Health. 2017;49(1):17–27. doi: 10.1363/psrh.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones RK, Jerman J, Onda T. Characteristics of U.S. Abortion patients in 2014 and changes since 2008. New York: Guttmacher Institute; 2016. [Accessed: January 3, 2018]. pp. 1–29. Available: https://www.guttmacher.org/sites/default/files/report_pdf/characteristics-us-abortion-patients-2014.pdf. [Google Scholar]
- Kimport K, Rowland B. Health and Health Care Concerns Among Women and Racial and Ethnic Minorities. Vol. 35. Bingley, UK: Emerald Publishing Limited; 2017. Taking insurance in abortion care: Policy, practices, and the role of poverty; pp. 39–57. [Google Scholar]
- Mercier R, Buchbinder M, Bryant A, Britton L. The experiences and adaptations of abortion providers practicing under a new TRAP law: A qualitative study. Contraception. 2015;91(6):507–512. doi: 10.1016/j.contraception.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercier RJ, Buchbinder M, Bryant A. TRAP laws and the invisible labor of US abortion providers. Critical Public Health. 2016;26(1):77–87. doi: 10.1080/09581596.2015.1077205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Vintage 2014 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010–July 1, 2014), by year, county, single-year of age (0, 1, 2, …, 85 years and over), bridged race, Hispanic origin, and sex. [Accessed: January 3, 2018];2015 :1–22. Prepared under a collaborative arrangement with the U.S. Census Bureau. Available: https://www.cdc.gov/nchs/nvss/bridged_race.htm.
- Weitz TA, Taylor D, Desai S, Upadhyay UD, Waldman J, Battistelli MF, Drey EA. Safety of aspiration abortion performed by nurse practitioners, certified nurse midwives, and physician assistants under a California legal waiver. American Journal of Public Health. 2013;103(3):454–461. doi: 10.2105/AJPH.2012.301159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitz T, Anderson P, Taylor D. Advancing scope of practice for advanced practice clinicians: more than a matter of access. Contraception. 2009;80(2):105–107. doi: 10.1016/j.contraception.2009.04.013. [DOI] [PubMed] [Google Scholar]