Abstract
Our understanding of how community-level context impacts care of persons living with HIV (PLWH), including antiretroviral therapy (ART) adherence and retention in care, is limited. The objective of this study was to characterize the activity spaces of PLWH from an urban area in Southeastern U.S., where the epidemic is among the nation’s highest, and to examine how such activity spaces are associated with daily mood and health behaviors. In this small, pilot study, 11 participants were tracked with a global positioning system (GPS)-enabled application on their smartphones for 2 weeks. Activity spaces were created by connecting GPS points sequentially and adding buffers. Contextual exposure data (e.g., alcohol outlets) were connected to activity spaces. Participants also completed daily diary entry through texts 3 times per day regarding outcomes of substance use behaviors, mood, and medication adherence. This yielded a total of 18,007 GPS polyline records that we aggregated into 258 person-days that captured discrete occasions of exposure to contextual factors and subjects’ behaviors and moods. On average, the participants spent 19% of their time awake during the 2-week periods in their residential census tract. Exposure to social and built environment factors such as alcohol outlets was greater when participants were outside versus inside their residential census tract. Exposures on daily routes were also significantly associated with ART adherence, alcohol consumption, and mood. Findings suggest substantial differences between activity spaces and residential contexts. Activity spaces are relevant for PLWH and may impact HIV care and behavioral outcomes such as ART adherence and substance use.
Keywords: neighborhoods, HIV, activity space, daily diary, GPS, adherence, alcohol
1. Background
Although antiretroviral therapy (ART) has greatly reduced HIV-related morbidity and mortality (Palella et al., 2006), benefits of therapy require strict adherence, tolerance of side effects, and regular access to primary care (Celum et al., 2013; Lima et al., 2007). Retention in care among PLWH is low in the U.S. (Marks et al., 2010), and 30% or less achieve successful viral suppression (CDC, 2011; Gardner et al., 2011). There is also substantial geographic variability and potential regional contextual differences in retention in care (Rebeiro et al., 2016). Given that a disproportionate burden of HIV is concentrated in socially disenfranchised communities (El-Sadr et al., 2010; Gant et al., 2012; Pellowski et al., 2013), a deeper understanding of the day-to-day experiences of PLWH is paramount if we are to improve clinical outcomes and the HIV care continuum (the steps from the time a person is diagnosed through successful ART to achieve viral suppression) (Auerbach et al., 2011; Watkins-Hayes, 2014).
Social determinants such as poverty, unemployment, or unstable housing play a significant role in successful care, potentially because treatment adherence is difficult when faced with having to manage competing challenging life circumstances (Cornelius et al., 2017; Evans and Strathdee, 2006; Kalichman et al., 2011, 2006; Takahashi et al., 2001). Of the limited neighborhood effect studies among PLWH, most rely on conventional approaches, like utilizing census tract of residence, to measure place-based exposures (Bruce et al., 2015; Eberhart et al., 2015; Willie et al., 2016). However, residential location may not be the most relevant space effecting health outcomes, as individuals are exposed to multiple neighborhood contexts outside of their residential neighborhood (Diez Roux, 2001; Diez Roux and Mair, 2010; Matthews and Yang, 2013). In response to these limitations, the concept of ‘activity space’ has emerged. Activity space research examines all spaces in which daily activities occur, providing a more precise measure of place-based exposures (Kwan, 2009; Vaughan et al., 2017). Methods to capture such activity space often incorporate global positioning systems (GPS), which has been successfully utilized in research among older adults, youth (Byrnes et al., 2015; Wan et al., 2013; Wiehe et al., 2008), and men at risk for HIV (Duncan et al., 2016), among others. GPS can enable more precise measurement of socio-spatial activity but has not, to our knowledge, been used to measure community exposures of PLWH. Furthermore, while daily diary data collection has been used among PLWH to examine daily behavior such as physical activity and alcohol use (Barta et al., 2015; Webel et al., 2015), it has not been coupled with GPS.
Alcohol is frequently abused by PLWH (Hahn and Samet, 2010) and may impact viral suppression through its influence on ART adherence (Samet et al., 2003). In addition to the stress of living in disinvested and violent communities, greater availability of alcohol outlets may lead to greater consumption (Popova et al., 2009; Scribner et al., 2010). Furthermore, the precise mechanisms through which community contexts such as alcohol density or violence act to impact behaviors remains unknown, although daily mood may be one potential route (Fleishman et al., 2000; Janda et al., 2006; Moskowitz, 2003) given the well-known impact of stressful situations on negative mood (Kessler et al., 1985; Pearlin, 1999).
Psychological well-being is comprised of both positive and negative affect (Bradburn, 1969) or mood, and poor psychological well-being is both a cause of poor outcomes among PLWH (Chida and Vedhara, 2009; Ironson et al., 2015; Pence et al., 2008) as well as an outcome of HIV infection and treatment (Arendt, 2006; Owe-Larsson et al., 2009). Negative mood or generalized mental illness may play a role in adherence to ART, uptake of voluntary testing and counseling, and engagement in secondary prevention (Baum and Nesselhof, 1988). Roughly half of PLWH in care screen positive for at least one psychiatric disorder (Bing et al., 2001), and the prevalence of a depressive disorder ranges from 16–36% compared to 4.9% in the general HIV-negative population. The range is 2–26% for alcohol abuse (Bing et al., 2001; Pence et al., 2006), and the prevalence of PTSD is 10–75% compared to 8% in the general population (Applebaum et al., 2015). Psychiatric co-morbidities have been shown to be an important patient-related barrier to adequate adherence (Applebaum et al., 2015; Gordillo et al., 1999; Haubrich et al., 1999; Paterson et al., 2000), and they have been shown to influence substance use (O’Cleirigh et al., 2015).
GPS tracking promises untapped potential to advance our understanding of these complex and important health phenomena. In this proof of concept paper, we present an innovative approach that uses real-time GPS tracking and short message service (SMS) or text messaging for capturing activity spaces of PLWH. Our objective was to characterize the activity spaces of PLWH from an urban area in Southeastern U.S., where the epidemic is among the nation’s highest (CDC, 2013), and to examine how such activity spaces are associated with daily mood and health behaviors such as alcohol and other drug use as well as ART adherence. If feasible, such an approach will allow us to move beyond our conventional understanding of place-based contextual exposures to one that incorporates the lived experience, allowing for a more precise characterization of context from which to build multilevel and structural interventions.
2. Methods
A parent study was underway in an urban metropolitan region in the Southeast to examine the impact of early life and adult stress on biological and clinical outcomes of PLWH over 2.5 years (N=350). The goal of the parent cohort is to examine the impact of early life and adult stress on biological and clinical outcomes of PLWH over 2.5 years. From October 2015 to October 2017, a small random sample of participants who consented to the parent study were invited to participate in this additional pilot study (N=20) as they attended an appointment at a local HIV clinic; 11 agreed to participate. The random sample included quota sampling in groups of 5 based on sex and level of adherence to ART reported in the parent study (high vs. low). There were no differences between participants in this pilot study and those in the parent study or those who did not agree to participate. The study was approved by the Tulane University Institutional Review Board.
Similar to a protocol utilized in previous activity space work (Byrnes et al., 2015), participants were tracked every 5 minutes over two weeks using ActSoft Comet Tracker (ActSoft Inc., Tampa, FL), which was downloaded as an application on their personal smartphone at the time of enrollment. Over the two weeks, participants were also sent a daily diary survey three times a day (morning—8:00 to 11:00 am, afternoon—1:00 to 4:00 pm, and evening—6:00 to 9:00 pm) using a two-way SMS program that was automated to deliver set messages based on participant responses. The diary took no more than 5 minutes to complete. Participants were required to complete each survey within the specific time period. Those not completed during the window were dropped from the analysis. Connecting sequential GPS points yielded a total of 18,007 polyline segments that we aggregated into 258 person-days that captured discrete occasions of exposure to contextual factors and subjects’ behaviors and moods.
2.1 Daily diary outcome measures
Data collected in the daily diary included measures of positive and negative affect and frequency and quantity of alcohol and other drug use since the previous diary entry, including frequency and type. Questions were formatted for text with short questions surrounding mood and substance use (e.g., “since your last entry, have you used alcohol? Felt angry?”). Poor psychological well-being is both a cause of poor outcomes among PLWH (Chida and Vedhara, 2009; Ironson et al., 2015; Pence et al., 2008) as well as an outcome of HIV infection and treatment (Arendt, 2006; Owe-Larsson et al., 2009). Additional questions were asked once per day, in the evening, regarding medication adherence (i.e., “did you take your prescribed ART medicine today?”), perceived reason for inability to adhere to medication, and perceived social support for medication adherence. One participant was unable to complete the daily diary data collection protocol due to technical difficulties with his cell phone, and therefore the sample with diary data was N=10.
2.2 Community-level measures
Three community-level exposures were used in this pilot study to link to GPS routes, utilizing a method identical to that in Byrnes and colleagues’ work (Byrnes et al., 2015). These community-level exposures included areal data on concentrated disadvantage (Sampson et al., 1997) and point data on alcohol outlets and violent crime events. Concentrated disadvantage was calculated with items obtained from the U.S. Census American Community Survey (ACS) 5-year estimates 2008–2012, based on Sampson and colleague’s index (Sampson et al., 2008), for each census tract in the region using the 2010 Census TIGER/Line Shapefile for tract boundaries. Geocoded alcohol outlet locations were obtained from the city and state’s Department of Alcohol and Tobacco Control data for 2015–2016. Numbers of active alcohol outlets by both census tract and along the GPS route over the 2-week period were tabulated for off-premise (e.g., liquor stores) and on-premise (e.g., bars) establishments. Geocoded data on violent crime events (i.e., assaults and homicides) were obtained from local police department data 2015–2016 and counts of events tabulated in an equivalent manner.
Alcohol and crime environments were considered primary exposures, while concentrated disadvantage was utilized for mapping purposes and testing of areal data linkage to GPS data in this feasibility study.
2.3 Analysis
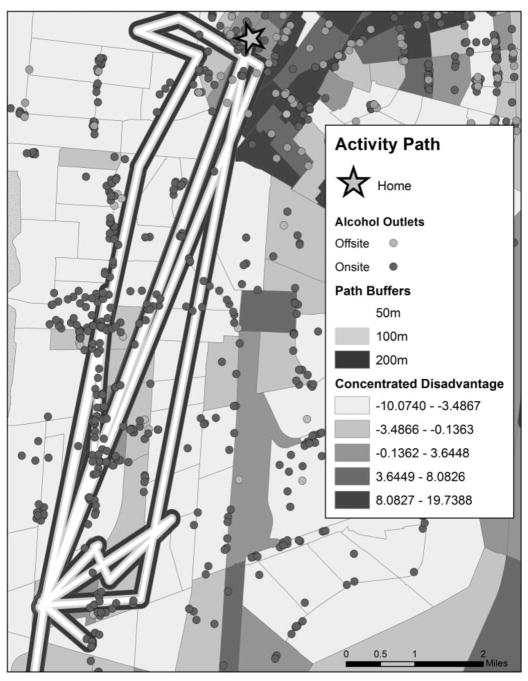
Activity spaces were calculated in ArcGIS® by first connecting GPS points in time order to create an aggregated polyline route representing the two-week activity path for each individual. Buffers at 50, 100, and 200 meters were created for each participant’s activity path. Second, community-level data layers were appended by latitude and longitude location (for point data) or census tract concentrated disadvantage to each minute-to-minute point of each participant’s activity path over their 14-day period, thereby providing precise estimates of exposures that they experienced throughout the course of activities. These data were also aggregated by time of day (i.e., morning, afternoon, and evening routes) over the 14-day period and then merged with daily diary data.
Daily diaries were also summarized by aggregating affirmative responses to questions asked three times per day to a daily value. For example, if respondents reported using alcohol at any of the three time points, they were classified as having used alcohol that day. Likewise, if they reported feeling mad, happy, excited, or sad in at least one of the three survey time points, they were classified as having the affect that day (not mutually exclusive). Responses for each participant were summarized as percentages of the total number of days in which they responded to the question (missing responses were removed from the denominator). Percentage of participants responding were slightly higher during week 1: mean percentage of participants responding to texts from morning 1 through evening 7 was 65% compared to 61% in week 2 (morning 8 through evening 14). Response rates were highest to morning and evening texts (both 71%) and lower in the afternoon (48%).
Descriptive statistics were utilized to examine activity patterns and daily diary responses, and repeated measures correlation (Bakdash and Marusich, 2017) was employed to explore the relation between activity space exposures and daily substance use, mood, and adherence.
3. Results
Almost half (45%) of participants in this small pilot study (N=11) were female, and 90% identified as Black. On average, the participants spent 19% of their time awake during the 2-week periods in their residential census tract. Participants traversed an average of 23 census tracts over this period. They were exposed to neighborhood violent crime rates that varied from 1 to 28 per 1,000 population and off-site alcohol density rates of 0 to 22 per 1,000 depending on the census tract. The average number of alcohol outlets within a 200-meter radius of participant’s daily paths was 5.6, with greater exposure on weekend days (average of 7.3 outlets) than weekdays (4.1 outlets), and on average 41% of their time was spent within a 200-meter proximity to an alcohol outlet. Results were similar, albeit slightly lower, for exposure within 100- and 50-meter radii. Details of exposure along their activity path are presented in Table 1, Section A. An example portion of one participant’s 2-week activity path is shown in Figure 1.
Table 1.
Daily Diary and GPS Observations and GPS-Diary Trends
| Section A. Two-week GPS data (N=11 participants, 18,007 observations) | ||
|---|---|---|
| Mean (STD) | Range | |
| Mean off-premise alcohol outlet density in residential census tract | 2.10 (1.25) | 0–6 |
| Total number of census tracts traversed (n) | 23.5 (13.6) | 4–44 |
| Mean off-premise alcohol outlets per 1,000 in tracts along path | 6.4 (6.2) | 0–22 |
| Mean violent crime rate per 1,000 in tracts along path | 14.5 (7.4) | 1–28 |
| Exposure within path buffers | ||
| Mean number of off-premise alcohol outlets in 50-meters along path | 2.0 (2.6) | 0–8 |
| Mean number of off-premise alcohol outlets in 100-meters along path | 4.1 (4.7) | 0–15 |
| Mean number of off-premise alcohol outlets in 200-meters along path | 5.6 (8.6) | 0–33 |
| Mean number of off-premise alcohol outlets in 200-meters along path during weekdays (Monday morning to Friday evening) | 4.1 (7.8) | 0–25 |
| Mean number of off-premise alcohol outlets in 200-meters along path during over weekend days (Friday evening to Monday morning) | 7.3 (11.6) | 0–33 |
| Mean % of time exposed to an off-premise outlet within 200-meters | 41.0 (35.1) | 1–100 |
| Section B. Two-week daily diary responses (N=10 participants, 281 observations)a | ||
|---|---|---|
| Mean (STD) | Range | |
| Total days responded to at least 1 text (n) | 12.5 (1.8) | 8–14 |
| Substance Use | ||
| Days reported alcohol use (%) | 46.5 (37.0) | 0–100 |
| Days reported marijuana use (%) | 43.5 (39.4) | 0–100 |
| Days reported other drug use (%) | 10.3 (19.4) | 0–61.5 |
| Medication adherence | ||
| Days reported taking medication (%) | 90.7 (11.3) | 66.7–100 |
| Days reported not taking medication because too busy (%) | 8.0 (12.3) | 0–33.3 |
| Days reported not taking medication because not feeling well (%) | 9.2 (16.9) | 0–50.0 |
| Days reported not taking medication because of being too drunk or too high (%) | 3.1 (6.5) | 0–16.7 |
| Section C. GPS-Diary Trends: Impact of Alcohol Exposure in 100 Meters of Pathway (N=10 participants, 258 observations) | ||
|---|---|---|
| Correlation | p-value | |
| Taking ART as prescribed | −0.365 | 0.005 |
| Alcohol use | 0.519 | 0.041 |
| Marijuana use | 0.381 | 0.001 |
| Felt mad | 0.203 | 0.009 |
| Did not take meds because high or drunk | 0.258 | 0.048 |
One participant was unable to complete the daily diary data collection protocol due to technical difficulties with his cell phone.
Figure 1.
Example of GPS record of one participant’s activity space overlaid on census tracts, alcohol outlets, and concentrated disadvantage.
The crime and alcohol density rate participants were exposed to on their activity path was substantially different from the rates in their residential tract. There were on average 6.4 off-premise outlets per 1,000 in the tracts through which respondents traversed, and approximately 4 of these were on weekdays and 7 on weekends, as discussed above. There were on average 2 off-premise outlets per 1,000 in their residential tract. However, this did vary by respondent, and some were exposed to much more on their daily path (e.g., one participant had an average of 1 outlet per 1,000 in their residential tract compared to 22 per 1,000 in tracts through which they spent time on their activity path), while some were exposed to less risky environments (e.g., 10 off-premise outlets per 1,000 in their residential tract compared to an average of 1 per 1,000 in tracts in their daily activity path).
Responses to daily diaries are summarized in Table 1, Section B. On average, participants responded to at least one of the three daily diaries for 12.5 of the possible 14 days (range 8–14). Participants reported alcohol use about half the time, on average, across survey response days. Reponses varied across individuals; some reported alcohol or marijuana at every diary response day, and others never reported alcohol or marijuana use. While not presented in Table 1, participants were happy at least once for most (81%) of their response days, sad on 44% of response days, and mad on 33% of response days. On average, participants reported having taken their medication 90% of the days they responded to the survey, and this ranged from two thirds (67%) to every day.
Linkage of the GPS and daily diary data revealed numerous trends. As shown in Table 1, Section C, participants with greater exposure to off-premise alcohol outlets within 100 meters of their daily paths were significantly less likely to take medication as prescribed and were more likely to report drinking, marijuana use, feelings of anger, and difficulty taking medication because they were drunk or high. Results were similar when considering exposure within 50- or 200-meters of their daily paths.
4. Discussion
This study fits within a broader effort in the study of health and place to document the multiple contexts that individuals inhabit and the ways they move across contexts throughout the day. Results demonstrate the feasibility of this methodology (GPS coupled with a daily diary captured via SMS messaging) among PLWH. Furthermore, as demonstrated in previous studies (Byrnes et al., 2015), there were meaningful differences in exposure context comparing activity space to residential contexts. Similar GPS-tracking approaches have been shown to be feasible among other populations (Byrnes et al., 2015; Duncan et al., 2016; Wan et al., 2013; Wiehe et al., 2008), and this study demonstrates feasibility among PLWH.
Limitations of the study include the limited number of participants who were also drawn from a convenience sample, lessening both power as well as generalizability. However, a diverse selection of participants was invited to participate, based on sex and level of adherence, to better reflect the larger community of PLWH. Furthermore, sampling from a local HIV clinic may miss those not engaged in care. We expect, however, that exposure to stressful community contexts and behavioral outcomes may be just as high or higher for those not engaged in care; there may be a potentially greater impact of environment and differences in activity space versus residential exposure if these patients were included. There were also limitations with GPS signal and satellite when indoors, which created some gaps in the GPS data, but this was primarily at respondent’s homes and not on their activity path outside the home. Finally, observing individuals in a 2-week time frame may not fully capture their daily activity space.
Additional contexts in the community that are amenable to structural interventions—such as the community alcohol environment—have not been examined in relation to adherence or substance use among PLWH. These contexts, however, may impact substance use behavior as well as overall stress and violence exposure, and all of these may play a role in HIV care behavior and retention in care. Given the often-differential community contexts across race in the U.S. (LaVeist, 2003) and potentially different lived experiences of PLWH based on race, sex, or gender (Watkins-Hayes, 2014), deeper exploration of spatial context coupled with daily behavior may explain some of the intractable racial disparities in HIV care outcomes observed (Nunn et al., 2015; Underwood et al., 2014). Use of spatial data coupled with behavioral data using such an approach may provide a detailed picture of not only social but spatial risks in the daily lives of PLWH, allowing for new and potentially more impactful environmental prevention strategies to improve the continuum of care.
Highlights.
GPS data may reveal differences in community exposure to risk environments.
Exposure to alcohol and crime environments was greater in activity spaces.
Activity space exposures were associated with behavioral outcomes.
GPS and daily diary data collection approaches were feasible among people living with HIV (PLWH).
Acknowledgments
This study was supported by the National Institutes on Alcohol Abuse and Alcoholism (NIAAA) (P60AA009803). This study was approved by two university Institutional Review Boards. The authors thank all of the participants who agreed to take part in this study.
Footnotes
Contributors
KPT and DJW conceptualized the study. EFK and XZ conducted data collection. Data analysis was conducted by EFK, MW, CM, and KPT. KPT wrote the manuscript with feedback provided by all co-authors. All authors have contributed to and approved the final manuscript
Conflict of Interest
There are no conflicts of interest to report.
Role of Funding Source
No form of payment was given to anyone to produce the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Applebaum A, Richardson M, Brady S, Brief D, Keane T. Gender and other psychosocial factors as predictors of adherence to Highly Active Antiretroviral Therapy (HAART) in adults with comorbid HIV/AIDS, psychiatric and substance-related disorder. AIDS Behav. 2009;13:60–65. doi: 10.1007/s10461-008-9441-x. [DOI] [PubMed] [Google Scholar]
- Applebaum AJ, Bedoya CA, Hendriksen ES, Wilkinson JL, Safren SA, O’Cleirigh C. Future directions for interventions targeting PTSD in HIV-infected adults. J Assoc Nurses AIDS Care. 2015;26:127–138. doi: 10.1016/j.jana.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arendt G. Affective disorders in patients with HIV infection. CNS Drugs. 2006;20:507–518. doi: 10.2165/00023210-200620060-00005. [DOI] [PubMed] [Google Scholar]
- Auerbach JD, Parkhurst JO, Cáceres CF. Addressing social drivers of HIV/AIDS for the long-term response: Conceptual and methodological considerations. Glob Public Health. 2011;6:S293–S309. doi: 10.1080/17441692.2011.594451. [DOI] [PubMed] [Google Scholar]
- Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;8:456. doi: 10.3389/fpsyg.2017.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barta W, Portnoy D, Kiene S, Tennen H, Abu-Hasaballah K, Ferrer R. A daily process investigation of alcohol-involved sexual risk behavior among economically disadvantaged problem drinkers living with HIV/AIDS. AIDS Behav. 2015;12:729–740. doi: 10.1007/s10461-007-9342-4. [DOI] [PubMed] [Google Scholar]
- Baum A, Nesselhof SE. Psychological research and the prevention, etiology, and treatment of AIDS. Am Psychol. 1988;43:900–906. doi: 10.1037//0003-066x.43.11.900. [DOI] [PubMed] [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Turner BJ, Eggan F, Beckman R, Vitiello B. Psychiatric disorders and drug use among human immunodeficiency virus–infected adults in the United States. Arch Gen Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Bradburn NM. The structure of psychological well-being. Aldine; Oxford: 1969. [Google Scholar]
- Bruce D, Kahana SY, Bauermeister JA, Nichols SL, Hightow-Weidman LB, Heinze JE, Shea J, Fernández MI. Neighborhood-level and individual-level correlates of cannabis use among young persons living with HIV/AIDS. Drug Alcohol Depend. 2015;151:173–180. doi: 10.1016/j.drugalcdep.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes HF, Miller BA, Wiebe DJ, Morrison CN, Remer LG, Wiehe SE. Tracking adolescents with Global Positioning System-enabled cell phones to study contextual exposures and alcohol and marijuana use: A pilot study. J Adolesc Health. 2015;57:245–247. doi: 10.1016/j.jadohealth.2015.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Vital signs: HIV prevention through care and treatment—United States. MMWR Morb Mortal Wkly Rep. 2011;60:1618. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV/AIDS Surveillance Report. Year-end 2011 Edition. Centers for Disease Control and Prevention; Atlanta: 2013. [Google Scholar]
- Celum C, Hallett TB, Baeten JM. HIV-1 prevention with ART and PrEP: Mathematical modeling insights into resistance, effectiveness, and public health impact. J Infect Dis. 2013;208:189–191. doi: 10.1093/infdis/jit154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Vedhara K. Adverse psychosocial factors predict poorer prognosis in HIV disease: A meta-analytic review of prospective investigations. Brain Behav Immun. 2009;23:434–445. doi: 10.1016/j.bbi.2009.01.013. [DOI] [PubMed] [Google Scholar]
- Cornelius T, Jones M, Merly C, Welles B, Kalichman MO, Kalichman SC. Impact of food, housing, and transportation insecurity on ART adherence: A hierarchical resources approach. AIDS Care. 2017;29:449–457. doi: 10.1080/09540121.2016.1258451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, Regan SD, Goedel WC, Levy MD, Barton SC, Friedman SR, Halkitis PN. Feasibility and acceptability of global positioning system (GPS) methods to study the spatial contexts of substance use and sexual risk behaviors among young men who have sex with men in New York City: A p18 cohort sub-study. PLoS One. 2016;11:e0147520. doi: 10.1371/journal.pone.0147520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhart MG, Yehia BR, Hillier A, Voytek CD, Fiore DJ, Blank M, Frank I, Metzger DS, Brady KA. Individual and community factors associated with geographic clusters of poor HIV care retention and poor viral suppression. J Acquir Immune Defic Syndr. 2015;69:S37–S43. doi: 10.1097/QAI.0000000000000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sadr WM, Mayer KH, Hodder SL. AIDS in America—Forgotten but not gone. New Engl J Med. 2010;362:967–970. doi: 10.1056/NEJMp1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans L, Strathdee SA. A roof is not enough: Unstable housing, vulnerability to HIV infection and the plight of the SRO. Int J Drug Policy. 2006;17:115–117. [Google Scholar]
- Fleishman J, Sherbourne C, Crystal S, Collins R, Marshall G, Kelly M, Bozzette S, Shapiro M, Hays R. Coping, conflictual social interactions, social support, and mood among HIV-infected persons. Am J Community Psychol. 2000;28:421–453. doi: 10.1023/a:1005132430171. [DOI] [PubMed] [Google Scholar]
- Gant Z, Lomotey M, Hall HI, Hu X, Guo X, Song R. A county-level examination of the relationship between HIV and social determinants of health: 40 states, 2006–2008. Open AIDS J. 2012;6:1–7. doi: 10.2174/1874613601206010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52:793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordillo V, del Amo J, Soriano V, González-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 1999;13:1763–1769. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- Hahn JA, Samet JH. Alcohol and HIV disease progression: Weighing the evidence. Curr HIV/AIDS Rep. 2010;7:226–233. doi: 10.1007/s11904-010-0060-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haubrich RH, Little SJ, Currier JS, Forthal DN, Kemper CA, Beall GN, Johnson D, Dubé MP, Hwanga JY, McCutchan JA. The value of patient-reported adherence to antiretroviral therapy in predicting virologic and immunologic response. AIDS. 1999;13:1099–1107. doi: 10.1097/00002030-199906180-00014. [DOI] [PubMed] [Google Scholar]
- Ironson G, O’Cleirigh C, Kumar M, Kaplan L, Balbin E, Kelsch C, Fletcher M, Schneiderman N. Psychosocial and neurohormonal predictors of HIV disease progression (CD4 cells and viral load): A 4 year prospective study. AIDS Behav. 2015:1–10. doi: 10.1007/s10461-014-0877-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janda LH, Markowski E, Derlega VJ, Nezlek J, McCain N. Daily events and mood state among individuals living with HIV: Examination of the within-persons approach to data collection using daily diary methodology. J Nurs Meas. 2006;14:116–128. doi: 10.1891/jnm-v14i2a004. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Pellowski J, Kalichman M, Cherry C, Detorio M, Caliendo A, Schinazi R. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prev Sci. 2011;12:324–332. doi: 10.1007/s11121-011-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kagee A, Toefy Y, Jooste S, Cain D, Cherry C. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med. 2006;62:1641–1649. doi: 10.1016/j.socscimed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: Stress, social support, and coping processes. Annu Rev Psychol. 1985;36:531–572. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- Kwan MP. From place-based to people-based exposure measures. Soc Sci Med. 2009;69:1311–1313. doi: 10.1016/j.socscimed.2009.07.013. [DOI] [PubMed] [Google Scholar]
- LaVeist TA. Racial segregation and longevity among African Americans: An individual-level analysis. Health Serv Res. 2003;38:1719–1734. doi: 10.1111/j.1475-6773.2003.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima VD, Hogg RS, Harrigan PR, Moore D, Yip B, Wood E, Montaner JSG. Continued improvement in survival among HIV-infected individuals with newer forms of highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2007;21:685–692. doi: 10.1097/QAD.0b013e32802ef30c. [DOI] [PubMed] [Google Scholar]
- Marks G, Gardner LI, Craw J, Crepaz N. Entry and retention in medical care among HIV-diagnosed persons: A meta-analysis. J Acquir Immune Defic Syndr. 2010;24:2665–2678. doi: 10.1097/QAD.0b013e32833f4b1b. [DOI] [PubMed] [Google Scholar]
- Matthews SA, Yang TC. Spatial polygamy and contextual exposures (SPACEs): Promoting activity space approaches in research on place and health. Am Behav Sci. 2013;57:1057–1081. doi: 10.1177/0002764213487345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT. Positive affect predicts lower risk of AIDS mortality. Psychosom Med. 2003;65:620–626. doi: 10.1097/01.psy.0000073873.74829.23. [DOI] [PubMed] [Google Scholar]
- Nunn A, Sanders J, Carson L, Thomas G, Cornwall A, Towey C, Lee H, Tasco M, Shabazz-El W, Yolken A, Smith T, Bell G, Feller S, Smith E, James G, Shelton Dunston B, Green D. African American community leaders’ policy recommendations for reducing racial disparities in HIV infection, treatment, and care. Health Promot Pr. 2015;16:91–100. doi: 10.1177/1524839914534855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cleirigh C, Valentine S, Pinkston M, Herman D, Bedoya C, Gordon J, Safren S. The unique challenges facing HIV-positive patients who smoke cigarettes: HIV viremia, art adherence, engagement in HIV care, and concurrent substance use. AIDS Behav. 2015;19:178–185. doi: 10.1007/s10461-014-0762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owe-Larsson MB, Säll L, Salamon E, Allgulander C. HIV infection and psychiatric illness. Afr J Psychiatry. 2009;12:115–128. doi: 10.4314/ajpsy.v12i2.43729. [DOI] [PubMed] [Google Scholar]
- Palella, Frank J, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, Holmberg SD. Mortality in the highly active antiretroviral therapy era: Changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43:27–34. doi: 10.1097/01.qai.0000233310.90484.16. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Pearlin LI. Handbook of the Sociology of Mental Health. New York: Springer; 1999. The stress process revisited; pp. 395–415. [Google Scholar]
- Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: Social disadvantage and the US HIV epidemic. Am Psychol. 2013;68:197–209. doi: 10.1037/a0032694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Whetten K, Eron JJ, Gaynes BN. Prevalence of DSM-IV-defined mood, anxiety, and substance use disorders in an HIV clinic in the Southeastern United States. J Acquir Immune Defic Syndr. 2006;42:298–306. doi: 10.1097/01.qai.0000219773.82055.aa. [DOI] [PubMed] [Google Scholar]
- Pence BW, Ostermann J, Kumar V, Whetten K, Thielman N, Mugavero MJ. The influence of psychosocial characteristics and race/ethnicity on the use, duration, and success of antiretroviral therapy. J Acquir Immune Defic Syndr. 2008;47:194–201. doi: 10.1097/QAI.0b013e31815ace7e. [DOI] [PubMed] [Google Scholar]
- Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: Impacts on alcohol consumption and damage: A systematic review. Alcohol Alcohol. 2009;44:500–516. doi: 10.1093/alcalc/agp054. [DOI] [PubMed] [Google Scholar]
- Rebeiro PF, Gange SJ, Horberg MA, Abraham AG, Napravnik S, Samji H, Yehia BR, Althoff KN, Moore RD, Kitahata MM. Geographic variations in retention in care among HIV-infected adults in the United States. PLoS One. 2016;11:e0146119. doi: 10.1371/journal.pone.0146119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Horton NJ, Traphagen ET, Lyon SM, Freedberg KA. Alcohol consumption and HIV disease progression: Are they related? Alcohol Clin Exp Res. 2003;27:862–867. doi: 10.1097/01.ALC.0000065438.80967.56. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci. 2008;105:845–852. doi: 10.1073/pnas.0710189104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner R, Theall KP, Simonsen N, Robinson W. HIV risk and the alcohol environment: Advancing an ecological epidemiology for HIV/AIDS. Alcohol Res Health. 2010;33:179. [PMC free article] [PubMed] [Google Scholar]
- Takahashi LM, Wiebe D, Rodriguez R. Navigating the time–space context of HIV and AIDS: Daily routines and access to care. Soc Sci Med. 2001;53:845–863. doi: 10.1016/s0277-9536(00)00363-4. [DOI] [PubMed] [Google Scholar]
- Underwood C, Hendrickson Z, Van Lith LM, Kunda J, ECM Role of community-level factors across the treatment cascade: A critical review. J Acquir Immune Defic Syndr. 2014;66:s311–s318. doi: 10.1097/QAI.0000000000000234. [DOI] [PubMed] [Google Scholar]
- Vaughan AS, Kramer MR, Cooper HL, Rosenberg ES, Sullivan PS. Activity spaces of men who have sex with men: An initial exploration of geographic variation in locations of routine, potential sexual risk, and prevention behaviors. Soc Sci Med. 2017;175:1–10. doi: 10.1016/j.socscimed.2016.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan N, Qu W, Whittington J, Witbrodt BC, Henderson MP, Goulding EH, Schenk AK, Bonasera SJ, Lin G. Assessing smart phones for generating life-space indicators. Env Plann B Plann Des. 2013;40:350–361. doi: 10.1068/b38200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins-Hayes C. Intersectionality and the sociology of HIV/AIDS: Past, present, and future research directions. Annu Rev Sociol. 2014;40:431–457. [Google Scholar]
- Webel AR, Barkley J, Longenecker CT, Mittelsteadt A, Gripshover B, Salata RA. A cross-sectional description of age and gender differences in exercise patterns in adults living with HIV. J Assoc Nurses AIDS Care. 2015;26:176–186. doi: 10.1016/j.jana.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiehe SE, Carroll AE, Liu GC, Haberkorn KL, Hoch SC, Wilson JS, Fortenberry JD. Using GPS-enabled cell phones to track the travel patterns of adolescents. Int J Health Geogr. 2008;7:22. doi: 10.1186/1476-072X-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie TC, Overstreet NM, Sullivan TP, Sikkema KJ, Hansen NB. Barriers to HIV medication adherence: Examining distinct anxiety and depression symptoms among women living with HIV who experienced childhood sexual abuse. Behav Med. 2016;42:120–127. doi: 10.1080/08964289.2015.1045823. [DOI] [PMC free article] [PubMed] [Google Scholar]