Abstract
Background
We sought to understand alcohol behavior change as a process over time by identifying patterns of relapse and remission after outpatient treatment and evaluating how these patterns predict longer-term clinical outcomes.
Method
We conducted latent profile analyses using data from the outpatient arm in Project MATCH. Relapse and remission episodes were defined by the number of consecutive 14-day periods that included any heavy drinking days and no heavy drinking days. Indicators of each profile were: initial 2-week post-treatment remission/relapse status, number of remission/relapse transitions in the first year after treatment, duration of remission episodes, and duration of relapse episodes.
Results
We identified 6 profiles: 1) “remission,” 2) “transition to remission”, 3) “few long transitions,” 4) “many short transitions,” 5) “transition to relapse,” and 6) “relapse.” Profile 1 had the best long-term outcomes. Long-term outcomes were not uniform among individuals with at least some heavy drinking (profiles 2 through 6; ~75% of the sample). Individuals who transitioned back to and sustained periods of remission (profiles 2–4) had better long-term outcomes than those who failed to transition out of relapse (profiles 5–6) following treatment.
Conclusions
Post-treatment change in alcohol use is a process in which individuals variably transition in and out of “relapse” and “remission” statuses. “Any heavy drinking” following treatment is not necessarily a sign of treatment failure. A more nuanced look at the process of AUD change by considering whether individuals are able to transition to and sustain periods of remission seems warranted.
Keywords: alcohol use disorder, treatment outcomes, clinical course, change process, relapse, remission
1. Introduction
The clinical course of alcohol use disorder (AUD) is the progression of change in AUD “symptoms” following the initiation of formal treatment or of self-initiated behavior change (Maisto et al., 2014). Although alcohol consumption per se does not constitute a symptom of AUD according to the DSM-5 or ICD-10, it has been the center of attention among those interested in AUD clinical course. Clinical course is an important topic for AUD treatment providers and researchers because of its relation to the problem of maintenance of change. Recent research on AUD clinical course has shown that post-treatment alcohol consumption is characterized by heterogeneity in drinking patterns among individuals and that change within individuals is discontinuous. For example, Witkiewitz and Masyn’s (2008) analyses of Relapse Replication and Extension Project (RREP) data identified three drinking trajectories following first use of alcohol over the course of one year post-treatment: frequent heavy drinking, frequent drinking following the first lapse and a return to less frequent drinking, and infrequent moderate drinking. These trajectories were essentially replicated in analyses of two additional data sets yielded from Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity; Witkiewitz et al., 2007) and the COMBINE study (Combined Pharmacotherapies and the Behavioral Interventions for Alcohol Dependence; Witkiewitz et al., 2010). Findings such as these have led to the conceptualization that AUD clinical course is a dynamic change process (DiClemente and Crisafulli, 2016; Witkiewitz and Marlatt, 2004).
Two clinical course “change points” (Frank et al., 1991) that have received major attention are remission and relapse. Remission occurs when the initial change response is maintained for at least a specified period of time, and relapse occurs when a period of remission is disrupted by symptom reappearance. In the case of AUD, relapse has been defined in empirical studies most commonly by the occurrence of any alcohol use (also may be called a “lapse” or a “slip,” which, if followed by continued drinking may lead to a full “relapse”) or the occurrence of “heavy” alcohol use (Maisto et al., 2016).
Among the clinical course “change points” (response, remission, relapse, recovery, and recurrence) that Frank et al. (1991) defined, AUD clinicians and researchers have paid most attention to relapse (Maisto et al., 2016). Despite the wide agreement that the broad “change point” concept of AUD relapse is critical, there are divergent views about specifying its definition and whether to view relapse as an outcome or as part of the AUD change course. Traditionally, relapse was considered as an endpoint or as an outcome (of a behavior change episode) in the AUD treatment literature. A different view emerged and gained popularity in the mid-1980s among addictions clinical researchers that relapse is most productively conceptualized as part of the behavior change process (Brownell et al., 1986; Witkiewitz and Marlatt, 2004). This conceptualization of AUD relapse prevails (Hendershot et al., 2011; Maisto et al., 2016) and is consistent with Frank et al.’s (1991) idea of change points, originally developed for the clinical course of depression.
Given empirical evidence (cited earlier) that implies that the clinical course of AUD, as reflected in one’s alcohol consumption, is best viewed as existing on a continuum (also see Miller, 1996a), it is important to justify study of a construct like relapse, which traditionally has been identified as a discrete “state.” In this paper, we still identify discrete states of relapse/remission that patients transition between, but we do not consider relapse as an end point or outcome. The major reasons are both pragmatic and clinical. In this regard, Maisto et al. (2016) noted that the construct of relapse is virtually embedded in the literatures on AUD clinical practice and clinical research, and it is unlikely that use of the term relapse will fade in the near future. In addition, relapse is frequently used in clinical decision-making. Indeed, the construct is often applied as an indicator of treatment prognosis in clinical practice, despite a general lack of empirical evidence suggesting the occurrence of relapse at any given point may predict one’s longer-term functioning, which is the ultimate concern of any treatment.
The current thinking that relapse is part of the AUD change process has been mostly considered in conceptual literature, but unfortunately has not been reflected in the empirical literature. Maisto et al. (2016) reviewed studies published 2010–2015 on AUD relapse in clinical populations and identified 139 unique studies that met inclusion criteria. They found that all studies conceptualized and analyzed relapse as an endpoint or outcome; none modeled relapse as a possibly recurrent event that is part of the AUD change process. This stark lack of correspondence between current conceptualizations and empirical studies likely has slowed progress toward understanding when, how, and why relapse occurs, which is likely to impede progress toward improving the longer-term effectiveness of AUD treatments. Therefore, empirical study of AUD relapse that is aligned with current thinking about AUD clinical course seems to be indicated.
The purpose of this paper was to conduct secondary analyses of Project MATCH data to investigate AUD relapse as part of a process of behavior change. Two-week periods (or “states”) of remission and relapse were defined and identified, and transitions (changes) between these states for each participant were coded. We aimed to model the number of both types of transitions occurring in the first year post-treatment, duration of remission episodes, and duration of relapse episodes. The number of transitions and the duration of relapse/remission episodes were chosen as a way to represent in some detail any change in alcohol consumption over time that happens. We also indexed whether an individual was defined as in remission or relapse in the first 2 weeks post-treatment. Because of the heterogeneity of AUD relapse, we aimed to identify subgroups defined by these four variables (number of transitions, duration of remission episodes, duration of relapse episodes, and remission/relapse status in the first 2 weeks post-treatment), and compare them on alcohol-related and psychosocial outcomes 1- and 3-years post-treatment. This study differs from previous research because it focuses explicitly on the frequency of transitions between remission and relapse states and the duration of those states, rather than remission or relapse outcome itself. Furthermore, this study investigated the relation between shorter-term remission and relapse events to longer-term course at 3 years post-treatment conclusion, which meets the time criterion for “recovery” from AUD in major psychiatric diagnostic systems such as DSM.
It is important to note that this study is considered an initial, descriptive investigation of the process of AUD clinical course over time. As such, the research design includes simplifying features, such as defining remission and relapse only according to alcohol consumption and time. In addition, this study’s aim was not to test whether course of remission and relapse episodes predicts longer-term outcomes independent of other possible predictors such as baseline drinking patterns, but rather to obtain initial empirical evidence of the association between the post-treatment course of relapse and remission episodes and longer-term outcomes. This is essentially clinicians’ aim in alcohol and other drug treatment.
2. Method
2.1. Participants and procedure
We used data from the outpatient arm of Project MATCH (Project MATCH Research Group, 1997), a randomized clinical trial that evaluated the efficacy of three psychosocial treatments for AUD. The treatments were Cognitive Behavioral Therapy (CBT; Kadden, 1995), Motivational Enhancement Therapy (MET; Miller et al., 1992), and Twelve-Step Facilitation (TSF; Nowinski et al., 1992) for AUD. Participants (n=952) were recruited across nine research centers in the U.S. and included individuals who were actively drinking during the 3 months prior to study enrollment and who were seeking outpatient treatment (the aftercare arm of Project MATCH was excluded from the present analysis). Of the 952 outpatients, 877 (92.1%) had drinking data available during the follow-up period and were included in the present analyses. Among patients included in the present study, 28.5% were female, 20.0% were non-White, and the mean age was 38.9 (SD = 10.6).
During the 12-week treatment period, a total of 61.2% of the participants reported consuming at least one drink (Maisto et al.,, 2016). Follow-up measures included in the present study were assessed at baseline and 12 and 36 months post-treatment. For further details refer to Project MATCH Research Group (1997).
2.2. Measures
2.2.1. Alcohol consumption
Alcohol use was measured using the Form-90 (Miller, 1996b), a calendar-based method to obtain retrospective self-reports of alcohol use in the previous 90 days. The Form-90 was administered at each post-treatment assessment. Drinking data were used to quantify periods of relapse and remission, described further later in the Analytic Approach section. The 1- and 3-year post-treatment summary alcohol use variables encompassed the past 30 days and included percent drinking days (PDD), defined as the percentage of days in which any alcohol was consumed,, percent heavy (4/5 drinks in a day for women/men) drinking days (PHDD), and drinks per drinking day (DDD), defined as the average number of drinks on days that an individual reported drinking. Many studies have illustrated the reliability and accuracy of the Form 90 (Witkiewitz et al., 2015b).
2.2.2. Alcohol-related negative consequences
The Drinker Inventory of Consequences (DrInC; Miller et al.,1995) was used to obtain self-reports of alcohol-related negative consequences at 1 and 3 years post-treatment. Patients reported on a 4-point scale (1 = never, 4 = daily or almost daily) the frequency of 45 alcohol-related consequences. Internal consistency of DrInC in this sample ranged from α = 0.93–0.96 at baseline and 12 month follow-up, respectively.
2.2.3. Psychosocial functioning
The Psychosocial Functioning Inventory (PFI; Feragne et al., 1983) was used to measure self-reported psychosocial functioning at 1 and 3 years post-treatment. The PFI has two subscales. The social behavior scale is calculated from 10 items that assess the frequency of engaging in problematic social behavior or experiencing problematic social interactions. Higher scores indicate better psychosocial functioning. The social role performance scale is calculated from 4 items assessing how well one has been doing in various social roles and one item assessing satisfaction with leisure, social, or recreational activities. Higher scores on the social role performance subscale indicate better psychosocial functioning. The PFI has been used in studies among individuals receiving AUD treatment and showed validity as a treatment outcome (Fink et al., 1985), and showed that patterns of alcohol use within treatment (Maisto et al., 2016) and 1-year post treatment (Maisto et al., 2002) predict long-term psychosocial functioning. In this study, internal consistency reliability of the PFI social behavior and social role subscales exceeded α = .80 at the 1- and 3-year follow-ups.
2.2.4. Depression symptoms
The Beck Depression Inventory (BDI; (Beck et al., 1988) is a 21-item self-report scale that measures symptoms of depression. Participants were asked to respond on a 0–3 scale the degree to which each statement best describes the way that he/she has been feeling during the last 2 weeks. Internal consistency reliability in Project MATCH was α == .92 at the 12-month follow-up.
2.3. Analytic approach
Daily drinking data from the post-treatment period (starting 85 days, or 12 weeks, after the start of treatment) were classified as either HDD or days without heavy drinking. “Heavy drinking” was chosen as the alcohol consumption marker indicative of relapse, because as Maisto et al. (2016) showed, it is more likely to be associated with negative consequences than is ‘any drinking.’ From this, we aggregated the data into 26 fourteen-day periods with binary indicators of presence or absence of heavy drinking during each period. Transitions to relapse were defined by having a 14-day period with no heavy drinking that was followed by a 14-day period that included any heavy drinking. Transitions to remission were likewise defined by having a 14-day period with any heavy drinking that was followed by a 14-day period with no heavy drinking. Periods in which no drinking data were available were considered missing; periods with partial data used all available data to classify drinking status. Out of a total of 22,802 possible observations (26 two-week periods within 877 participants), data were available to compute drinking statuses for 21,418 observations (6.07% missing). The binary variables that were created, which indicated transitions into relapse and remission (i.e., not indicators of the relapse status itself), served as the bases for subsequent analyses. Durations of relapse and remission episodes were calculated based on the number of consecutive 14-day periods that occurred between transitioning from relapse to remission or vice versa.
The statistical analyses first aimed to identify and describe differences among individuals in their course of remission and relapse across the one-year follow-up period (0–12 months post-treatment). Given that there is no published precedent of specifying the clinical course of AUD remission and relapse episodes, we chose to use latent profile analysis (LPA) in Mplus v8.0 (Muthén and Muthén, 2012) as a way to identify subgroups (i.e., profiles). These profiles were defined by initial remission/relapse status in the first 2-week period post-treatment, number of transitions in the first year post-treatment, duration of remission episodes, and duration of relapse episodes. An individual’s initial remission/relapse status was indexed because we wanted to model change in the first year following treatment. In this regard, because some individuals were engaging in heavy drinking at the end of treatment, we needed a way to characterize whether individuals began the follow-up engaging in heavy drinking and thus did not relapse following treatment but rather continued a pattern of heavy consumption, or whether they began follow-up in remission and thus could relapse. The number of profiles that provided the best fit to the data was determined by multiple indices of model fit, classification precision, size of the final profile sizes based on latent profile proportions, and interpretability of the final latent profile solution. As measures of model fit, the Lo Mendell Rubin Likelihood Ratio test (LMR), Bayesian Information Criterion (BIC) and sample-size-adjusted BIC (aBIC) were examined. A significant LMR indicates a significantly better fit for a k profile model (e.g., 3 profiles) versus a k-1 profile model (e.g., 2 profiles) and a non-significant LMR indicates that adding an additional profile does not significantly improve model fit (Nylundet al., 2007). In addition, lower BIC and aBIC indicates a better fitting model (Nylund et al., 2007). Classification precision (defined by relative entropy) was used to evaluate how well the final latent profile solution classified individuals into latent profiles. Relative entropy ranges from 0–1, with values closer to 1 indicating greater classification precision and values of entropy greater than .80 indicating good classification precision (Nylund et al., 2007). Once the final latent profile solution was selected, we used distal outcome analysis via a modified approach (Asparouhov and Muthén, 2014; originally described by Bolck et al., 2004; aka the “BCH” method) to examine profile differences in 1- and 3-year post-treatment outcomes. The distal outcome analysis provides differences in mean outcomes across profiles using a Wald chi-square test. Comparisons between profiles derived from the LPA on 1- and 3-year post-treatment outcomes were examined for PDD, PHDD, DDD, DrInC total score, and PFI Social-Behavior and Social Role Performance subscales.
3. Results
We conducted LPA to examine different patterns of AUD clinical course based on the number of transitions between relapse and remission, heavy drinking status in the first two weeks following treatment, duration of relapse episodes, and duration of remission episodes. Individuals who were non-heavy drinkers during the first two weeks following treatment and who never transitioned to heavy drinking during the 1-year follow-up were considered to be in remission. Individuals who were heavy drinkers during the first two weeks following treatment and who never transitioned to non-heavy drinking were considered relapsed. These remission and relapse profiles were known (individuals who were in remission or relapsed) and constraints were placed on the data to ensure these two profiles were part of the final latent profile solution. Additional profiles were estimated from the data based on heavy drinking during the first two weeks post-treatment, number of transitions between relapse and remission, and duration of relapse/remission episodes.
Results of the LPA indicated that a 6-profile model provided the best balance of parsimony and model fit, with significantly better fit and lower BIC/aBIC than the 5-profile model. The 7-profile model did not fit significantly better than the 6-profile model. The 6-profile model also provided the highest entropy (0.96) and yielded interpretable latent profiles.
The 6-profile model was characterized by the following profiles of drinking behavior over the 1-year period following treatment: (1) continuous remission (≈25.5%); (2) approximately one transition to remission and staying in remission after this transition (≈9.6%); (3) few transitions with each remission/relapse episode lasting approximately 2 months on average (≈33.7%); (4) numerous transitions with each remission/relapse episode lasting approximately 1 month on average (≈13.6%); (5) approximately one transition to relapse and staying in relapse after this transition (≈ 7.1%); and (6) continuous relapse (≈10.5%). By definition, none of the individuals in profile 1 were drinking heavily in the first two weeks post-treatment, and all of the individuals in profile 6 were drinking heavily. It is important to emphasize for interpretation of these profiles that each one represents a combination of probabilities associated with each of the four defining criteria (post-treatment heavy drinking, number of transitions, duration of remission episodes, and duration of relapse episodes, respectively). For example, individuals “assigned” to profile 1 by definition began with no heavy drinking in the first two weeks post-treatment, and were highly unlikely to transition (essentially had 0 transitions as a group) to relapse. Similarly, by definition, individuals assigned to profile 6 engaged in heavy drinking in the first two weeks and were very unlikely to transition to remission. For profiles 1 and 6, the duration of remission and relapse episodes were fixed at 0 due to a lack of transition between relapse and remission states.
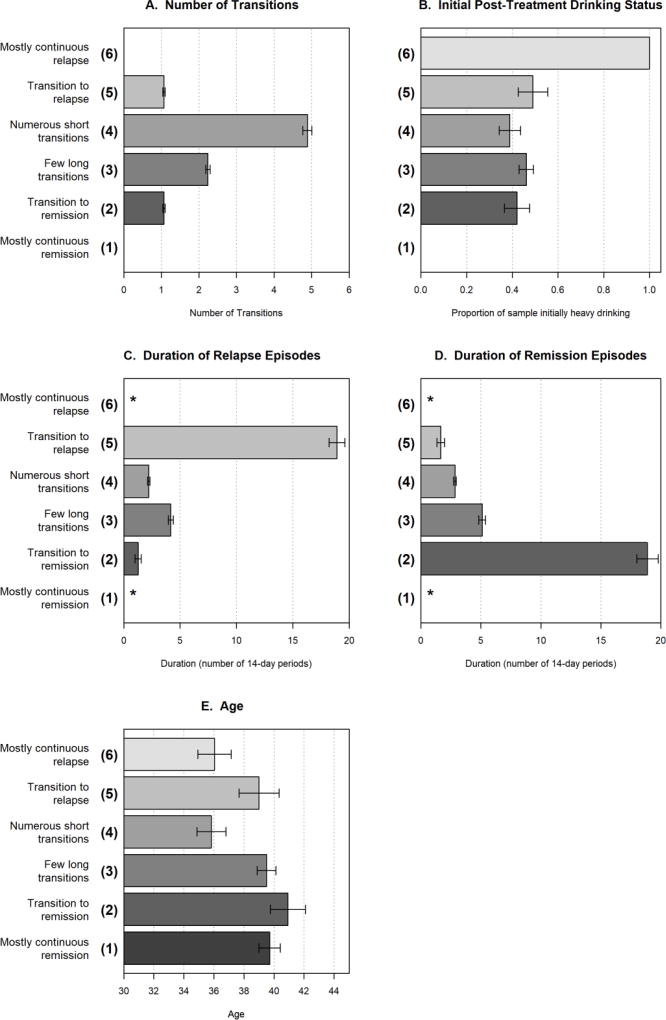
Figure 1 displays modeled profile means for the number of transitions (panel A), proportions of participants initially in heavy drinking at the start of post-treatment (panel B), and durations of relapse and remission episodes (panels C and D) for each latent profile. As noted earlier, for the duration data (panels C and D), the values on the x-axis represent the mean number of consecutive 14-day intervals for each episode (e.g., the mean relapse duration of 18.92 fourteen-day periods for profile 5 corresponds to an average relapse duration of about 265 days).
Figure 1.
Mean number of transitions, initial post-treatment drinking status, mean duration (in 2-week intervals) of relapse and remission episodes, respectively, and mean age for the latent profiles. Number of transitions reflects the sum of transitions to relapse and to remission; these two component parts were combined in the analytic model due to their high correlation (r = 0.94).
Figure note. Whiskers indicate ± SE. * = duration could not be computed.
Mean participant ages are also shown in Figure 1 (panel E): participants with profiles 6 (relapse) and 4 (numerous short transitions) were significantly younger than participants with profiles 1 (remission), 2 (long duration remission), and 3 (few long transitions). Profiles did not have significantly different proportions of participants who were male, χ2(df=5) = 4.70, p=.45, or who were racial minorities, χ2(df=5) = 3.77, p=.58.
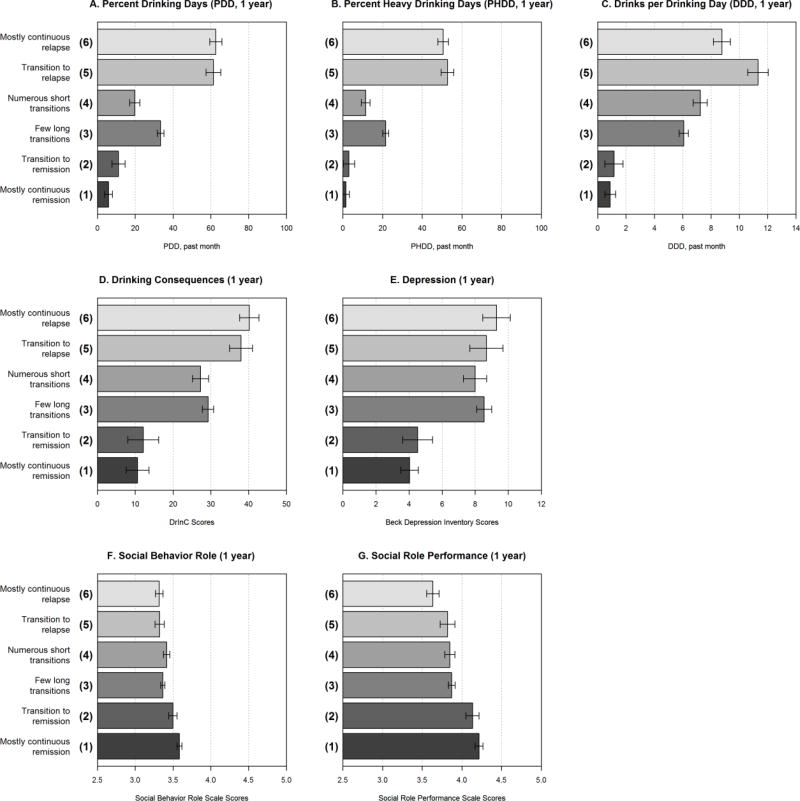
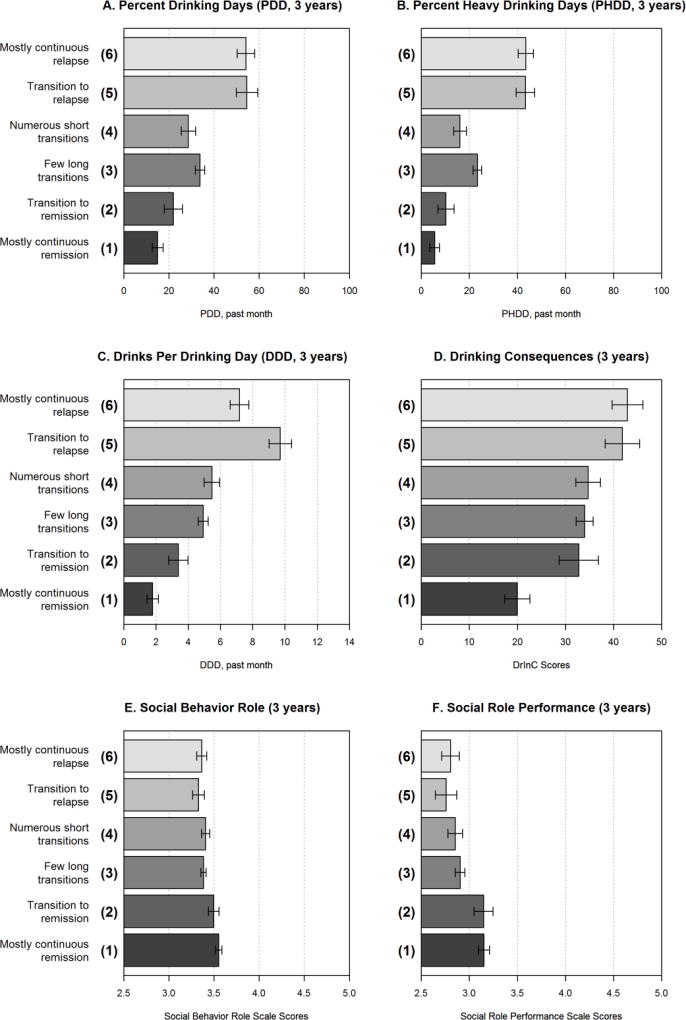
Distal outcome analyses using the BCH method in Mplus indicated significant differences between profiles on drinking outcomes and psychosocial functioning measures at 1 and 3 years post-treatment (Figures 2 and 3, respectively). Profiles 1 (remission) and 2 (transition to remission) had the best outcomes and were not significantly different from each other on any outcomes at 1 year post-treatment. Individuals in profile 2 had significantly greater DDD and consequences at 3 years post-treatment, as compared to profile 1. Profiles 6 (relapse) and 5 (transition to relapse) had the worst outcomes and were not significantly different from each other on any outcomes at 3 years post-treatment. Profiles 4 (numerous shorter transitions) and 3 (fewer longer transitions) did not differ on psychosocial functioning and DDD, but profile 3 was drinking more frequently than profile 4 at 1- and 3-year post-treatment. Profiles 3 and 4 had significantly better outcomes than profiles 6 and 5, and significantly worse outcomes than profiles 1 and 2 on most outcomes.1
Figure 2.
Means of outcomes measured at 1 year for latent profiles. Time reference for alcohol consumption is last 30 days, alcohol related consequences is last 90 days, depression is last 2 weeks, and the PFI scales are last 30 days.
Figure note. Whiskers indicate ± SE.
Figure 3.
Means of outcomes measured at 3 years for latent profiles. Time reference for alcohol consumption is last 30 days, alcohol related consequences is last 90 days, depression is last 2 weeks, and the PFI scales are last 30 days.
Figure note. Whiskers indicate ± SE.
4. Discussion
The results of this study reaffirm the importance of viewing AUD “relapse” as a process rather than an outcome. About 65 percent of the sample transitioned between relapse and remission at least once during the first year after outpatient treatment. The data also reaffirm the heterogeneity of AUD clinical course when it is defined by alcohol consumption, as the analyses identified six subgroups based on participants’ initial remission/relapse status and number of transitions between and duration of relapse-remission episodes during the one-year period following treatment. Examination of the data presented in Figures 1 and 2 further suggests that time spent in “remission” or “relapse” status was the important variable in predicting outcomes. Number of transitions per se, however, seemed to have less impact, although that is difficult to determine, because in this context there is some degree of dependence between number of transitions and duration of remission and relapse episodes. Therefore, from a clinical standpoint, it seems most important to prevent heavy drinking from occurring, but, if it does, to then intervene in order to keep periods of heavy drinking as brief as possible. One way clinicians might intervene is by educating clients about research-based data on the process of change in alcohol use patterns and that transition to remission predicts reductions in alcohol craving and negative affect following such transitions (Hallgren et al., 2016; Hallgren et al., 2017) as well as better longer-term drinking-related and psychosocial related outcomes several years after treatment (as found here). In other words, research-based data may bolster clinician efforts in helping clients reframe negative beliefs (e.g., I am a failure) after a relapse and in encouraging clients to work hard to “get back on their feet” once, or even several times, following one or more relapse episodes.
From the perspective of establishing metrics of AUD treatment outcomes, it would seem important to move toward an index that incorporates a pattern of heavy drinking and non-heavy drinking over time (including abstinence) in conjunction with psychosocial and health-related outcomes. Considering any of these dimensions in isolation likely would provide a less sensitive index of treatment effects and may not fully distinguish different clinical outcomes. Our LPA provides a few examples of this distinction, with different profiles having distinct post-treatment clinical courses despite some similarities in profiles (e.g., profiles 1 and 2 more strongly reflecting remission, profiles 5 and 6 more strongly reflecting relapse, and profiles 3 and 4 more strongly reflecting transitions between relapse and remission). Moreover, the distinctions between profiles 2–6 would be lost if the occurrence of heavy drinking (i.e., any relapse) was modeled as the primary outcome. Although statistical fit indices supported the six-profile solution, future work may aim to test whether similar profiles are replicated in different samples.
Altogether, our findings indicate that change in alcohol use is a heterogeneous process that unfolds over time, in which individuals commonly transition between “relapse” and “remission” statuses. Accordingly, clinicians and researchers should refrain from deeming “any heavy drinking” following treatment as a sign of treatment failure, but rather should take a more nuanced look at the process of AUD change by considering whether individuals are able to transition out of relapse episodes and subsequently sustain periods of remission. While frontline AUD treatment providers in the U.S. commonly view non-abstinence as an unacceptable treatment outcome (Davis and Rosenberg, 2013), there may be clinical value for providers to focus on helping patients who relapse minimize the durations of relapse episodes. In regards to clinical research trials of alcohol treatments, our findings suggest that evaluating “any heavy drinking” and “time to first heavy drinking episode” as the only endpoints may not adequately capture the process of alcohol behavior change over time. For example, these endpoints based on single events can incorrectly categorize individuals as treatment failures, given they do not consider the heterogeneity that exists with respect to how well individuals are able to transition to and sustain remission (e.g., no heavy drinking) following a relapse. Our study findings are consistent with a recent study by Wilson et al. (2016), which showed that the group of clients reporting any heavy drinking following treatment (so called “failures”) was actually a heterogeneous group, and that a large portion of this group exhibited similarly good long-term psychosocial outcomes as compared to those who reported no heavy drinking during follow-up.
It might be argued that finding differences among the profiles in 1-year alcohol consumption outcomes is difficult to interpret, because part of the data that define the outcomes also were part of the basis of profile classification. However, the outcome differences among profiles identified at one year generally held at three years post-treatment. Furthermore, the profile classification variable was associated with psychosocial variables, which were not part of profile classification.
There are several limitations of this study that should be considered in interpretation of its findings. The data are primarily descriptive and show the association between profile membership defined by course of remission and relapse episodes 1-year post-treatment and alcohol use/consequences and psychosocial outcomes at 1 and 3 years post-treatment. Moreover, the profiles are probabilistic and some misclassification does occur. Nonetheless, the results of the LPA suggest heterogeneity of AUD clinical course and the importance of viewing AUD remission and relapse as part of the change process rather than as endpoints. Importantly the results of the current study do not advance an explanation of those phenomena. Future work may help advance such explanations, for example, by examining how time-varying psychosocial constructs associated with relapse and remission change concurrently during the AUD clinical course. Unfortunately, the Project MATCH data were limited to assessments of psychosocial constructs at three-month intervals, and thus a more fine-grained account of time-varying predictors of relapse and remission episodes was not possible.
Another limitation is that the definitions of “remission” and “relapse” were, to some degree, arbitrary and involved only two factors (time and alcohol consumption). The interval period of 14 days was based on earlier empirical studies of AUD relapse (e.g., Maisto et al., 1995) and continues to be used for identifying within-treatment drinking transitions (e.g., Hallgren et al., 2016). Although alcohol consumption is the predominant factor considered both clinically and in clinical research when defining AUD relapse and remission, a strong case may be made for considering other factors as well, particularly those related to an individual’s psychosocial functioning (Miller, 1996a). Such a broad definition of remission or relapse could yield findings that differ from those reported in this paper.
Another limitation to consider is that this study consisted of secondary data analyses and thus is restricted to the content of a data set that was not originally designed to answer questions posed in this study. Nevertheless, the MATCH data have been extremely productive in advancing knowledge about AUD treatment and clinical course for over two decades. Finally, the data in this study were obtained via self-reports and thus are subject to the frailties of that method of data collection. Any associated concerns are ameliorated, however, by the use of psychometrically established measures. Nevertheless, replication of this study’s findings by use of multiple methods, such as the use of biomarkers to measure acute or chronic alcohol consumption, would increase confidence in the reliability of the results.
5. Conclusion
In conclusion, the results of this study reaffirm the heterogeneity of AUD clinical course and the validity of and utility in studying AUD remission and relapse as part of the change process rather than as outcomes. The most fundamental step for future research is to replicate the AUD clinical course profiles identified in this study. The profiles can be extended by including biopsychosocial variables as components of definitions of remission and relapse, which would provide the empirical base needed to consider the profiles more reliable and more generalizable. Consistent conceptually with Litten et al.’s (2015) Alcohol Addiction Research Domain Criteria, and Kwako et al.’s (2016) Addiction Neuroclinical Assessment, such research would increase knowledge about the biopsychosocial factors that may underlie profile differences and ultimately lead to more patient-centered AUD treatment.
Highlights.
Post-treatment change in alcohol use is a heterogeneous process.
Individuals variably transition in and out of “relapse” and “remission” statuses.
“Any heavy drinking” following treatment (tx) is not necessarily a sign of tx failure.
Preventing heavy drinking and intervening quickly if it occurs seems most crucial.
Evaluating “time to first heavy drinking episode” may not capture behavior change.
Acknowledgments
Role of Funding Source
Preparation of this manuscript was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism [R01 AA022328, R01 AA025539, K05 AA016928, and K01 AA024796]. The funding source was not involved in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
To place the results of these analyses in a broader context, we tested the profiles for differences in alcohol consumption and psychosocial variables at baseline. The analyses showed that the profiles differed on frequency of consumption, as Profile 4 drank on significantly (p < .05) fewer occasions and drank heavily less frequently than Profiles 5 and 6. However, the results of models testing predictions of profile differences at 1 and 3 years did not change substantively when baseline alcohol consumption variables were entered into the models.
Contributors
All authors conceptualized the present study and contributed to writing the manuscript’s first draft and to editing subsequent drafts. SAM and KAH conducted the background literature review and contributed to the interpretation of the findings. KAH and KW conducted statistical analyses. All authors contributed to and approved the final manuscript.
Conflicts of Interest
None declared.
References
- Asparouhov T, Muthén BO. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary second model (No. 21) Muthén and Muthén; Los Angeles, CA: 2014. [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. [Google Scholar]
- Bolck A, Croon M, Hagenaars J. Estimating latent structure models with categorical variables: One-step versus three-step estimators. Polit. Anal. 2004;12:3–27. doi: 10.1093/pan/mph001. [DOI] [Google Scholar]
- Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. Am. Psychol. 1986;41:765–782. doi: 10.1037//0003-066x.41.7.765. [DOI] [PubMed] [Google Scholar]
- Davis AK, Rosenberg H. Acceptance of non-abstinence goals by addiction professionals in the United States. Psychol. Addict. Behav. 2013;27:1102. doi: 10.1037/a0030563. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Crisafulli MA. Alcohol relapse and change needs a broader view than counting drinks. Alcohol. Clin. Exp. Res. 2016;41:266–269. doi: 10.1111/acer.13288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feragne MA, Longabaugh R, Stevenson JF. The psychosocial functioning inventory. Eval. Health Prof. 1983;6:25–48. doi: 10.1177/016327878300600102. [DOI] [PubMed] [Google Scholar]
- Fink EB, Longabaugh R, McCrady BM, Stout RL, Beattie M, Ruggieri-Authelet A, McNeil D. Effectiveness of alcoholism treatment in partial versus inpatient settings: Twenty-four month outcomes. Addic. Behav. 1985;10:235–248. doi: 10.1016/0306-4603(85)90004-8. [DOI] [PubMed] [Google Scholar]
- Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush JA, Weissman MM. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: Remission, recovery, relapse, and recurrence. Arch. Gen. Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Hallgren KA, Delker BC, Simpson TL. Effects of initiating abstinence from alcohol on daily craving and negative affect: Results from a pharmacotherapy clinical trial. Alcohol. Clin. Exp. Res. 2017;42:634–645. doi: 10.1111/acer.13591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren KA, McCrady BS, Epstein EE. Trajectories of drinking urges and the initiation of abstinence during cognitive–behavioral alcohol treatment. Addiction. 2016;111:854–865. doi: 10.1111/add.13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevention for addictive behaviors. Subst. Abuse Treat. Prev. Policy. 2011;6:1–17. doi: 10.1186/1747-597X-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden R, editor. Cognitive-behavioral coping skills therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (No. 94) National Institute on Alcohol Abuse and Alcoholism; Bethesda MD: 1995. [Google Scholar]
- Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: A neuroscience-based framework for addictive disorders. Biol. Psychiatry. 2016;80:179–189. doi: 10.1016/j.biopsych.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litten RZ, Ryan ML, Falk DE, Reilly M, Fertig JB, Koob GF. Heterogeneity of alcohol use disorder: understanding mechanisms to advance personalized treatment. Alcohol. Clin. Exp. Res. 2015;39:579–584. doi: 10.1111/acer.12669. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Longabaugh R, Beattie M. The relationship between abstinence for one year following pretreatment assessment and alcohol use and other functioning at two years in individuals presenting for alcohol treatment. J. Stud. Alcohol. 2002;63:397–403. doi: 10.15288/jsa.2002.63.397. [DOI] [PubMed] [Google Scholar]
- Maisto SA, McKay JR, O'Farrell TJ. Relapse precipitants and behavioral marital therapy. Addict. Behav. 1995;20:383–393. doi: 10.1016/0306-4603(94)00079-e. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Roos CR, Hallgren KA, Moskal D, Wilson AD, Witkiewitz K. Do alcohol relapse episodes during treatment predict long-term outcomes? Investigating the validity of existing definitions of alcohol use disorder relapse. Alcohol. Clin. Exp. Res. 2016;40:2180–2189. doi: 10.1111/acer.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Witkiewitz K, Moskal D, Wilson AD. Is the construct of relapse heuristic, and does it advance alcohol use disorder clinical practice? J. Stud. Alcohol Drugs. 2016;77:849–858. doi: 10.15288/jsad.2016.77.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. What is a relapse? Fifty ways to leave the wagon. Addiction. 1996a;91:15–28. [PubMed] [Google Scholar]
- Miller WR. Form 90: A structured assessment interview for drinking and related behaviors: Test manual (NIH Publication No. 96-4004) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1996b. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse (NIH Publication No. 95-3911) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1995. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. (Project MATCH Monograph Series) National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide (Version 8) Muthén and Muthén; Los Angeles: 2017. [Google Scholar]
- Nowinski J, Baker S, Carroll KM. Twelve step facilitation therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence(Vol. 1) US Dept. of Health and Human Services, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct. Equ. Modeling. 2007;14:535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project match posttreatment drinking outcomes. J. Stud. Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K. Finding success in failure: Using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction. 2016;111:2145–2154. doi: 10.1111/add.13518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, Kranzler HR. Guidelines for the reporting of treatment trials for alcohol use disorders. Alcohol. Clin. Exp. Res. 2015a;39:1571–1581. doi: 10.1111/acer.12797. http://doi.org/10.1111/acer.12797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, Kranzler HR. Recommendations for the design and analysis of treatment trials for alcohol use disorders. Alcohol. Clin. Exp. Res. 2015b;39:1557–1570. doi: 10.1111/acer.12800. http://doi.org/10.1111/acer.12800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Maisto SA, Donovan D. A comparison of methods for estimating change in drinking following alcohol treatment. Alcohol. Clin. Exp. Res. 2010;34:2116–2125. doi: 10.1111/j.1530-0277.2010.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. Am. Psychol. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Masyn KE. Drinking trajectories following an initial lapse. Psychol. Addict. Behav. 2008;22:157–167. doi: 10.1037/0893-164X.22.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, van der Maas HJ, Hufford MR, Marlatt GA. Non-normality and divergence in post-treatment alcohol use: Re-examining the Project MATCH data “another way”. J. Abnorm. Psychol. 2007;116:378–394. doi: 10.1037/0021-843X.116.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]