Abstract
The current investigation extends the findings of previous studies on the effects of simulation and correspondence training for teaching hygiene skills. Two male participants between the ages of 5 and 6 with autism spectrum disorder (ASD) were taught hygiene skills in a clinic setting. Both participants acquired the hygiene routine. Following instruction, the participants’ parents conducted probe sessions to assess generalization to the home environment. Generalization occurred for both participants. Moreover, a 6-month follow-up probe confirmed the maintenance of skills. This article provides utility to practitioners by providing a methodology for teaching hygiene after a bowel movement, demonstrating the generalization of skills from the clinic to the home, and providing a model for parent involvement.
Keywords: Hygiene training, Simulation training, Correspondence training
Many toilet-training protocols have been described in the behavior–analytic literature (Azrin & Foxx, 1971; Hagopian, Fisher, Piazza, & Wierzbicki, 1993; LeBlanc, Carr, Crossett, Bennett, & Detweiler, 2005; Post & Kirkpatrick, 2004). Although the protocols resulted in the acquisition of bladder and bowel control, they did not address a crucial area—for an individual to successfully clean himself or herself following the use of the toilet. Proper hygiene after toilet use is an important skill that is demonstrable, assessable, and identified in many developmental assessments.
Teaching the personal hygiene skills necessary following a bowel movement has been specifically addressed in only one previously published article (Stokes, Cameron, Dorsey, & Fleming, 2004). Stokes and colleagues used chaining and correspondence training (i.e., teaching clients to label whether their toilet paper was “clean” or “dirty” after wiping) to successfully teach three adults with developmental disabilities to wipe themselves effectively after bowel movements. However, that study was published over 12 years ago, and little or no research has been published since then on teaching après-toilette hygiene skills. The lack of current literature surrounding this topic underscores the need for further research targeting the acquisition of essential hygiene skills used following bowel movements.
The purpose of the current investigation was to evaluate the effects of simulation and correspondence training on the acquisition of hygiene skills after a bowel movement. In particular, we taught discrimination skills using a stimulus gradient, naming skills, and simulation performances using simulated feces on a doll to train wiping skills. Finally, we programmed for the generalization of skills and conducted probes to evaluate transference to the home setting.
Method
Participants
Two male participants were selected for this study, ages 5 years 9 months and 6 years 11 months. Both boys received clinic-based services 5 days per week. To qualify to participate, participants had to be bowel and bladder trained, have the ability to raise and lower their pants and underwear, complete at least one behavioral chain, and follow a correspondence training sequence. Both participants required adult support in the bathroom following a bowel movement. Neither of the boys had bowel movements in the context of the clinic setting; rather, bowel movements occurred at home.
The two participants scored at least 12.5 out of 15 on the Verbal Behavior Milestone Assessment and Placement Program (VB–MAPP) in the following relevant domains: mands, tacts, and listener responding.
Setting
Teaching trials took place at one clinic site. All trials for Participants GB and VB took place in cubicles containing a desk, two chairs, and training materials.
Materials
Prior to the start of the study, all parents were surveyed to determine what language would be used when describing the toilet paper (e.g., clean vs. dirty). The natural language preference assessment was conducted to confirm that the participant’s family members would be comfortable with the language used during instruction.
This study consisted of three training components: (a) labeling, (b) receptive identification, and (c) simulation training. The materials for labeling and receptive identification training were identical and consisted of one “clean” card and four different “dirty” cards (SunButter was used to simulate fecal matter). The materials for receptive identification also included a blank distractor card. All picture cards were approximately 8.9 cm wide × 12.7 cm tall and were created by taping two pieces of toilet paper folded into thirds onto a piece of clear laminate. The “dirty” sets varied based on the amount of SunButter (a stimulus gradient was used). SunButter, made from sunflower seeds, was used to ensure that training materials would not pose a risk to children in the clinic with allergies to nuts. The “dirty” cards were made as follows: (a) a 2.54 cm × 5.1 cm smear was made from a quarter teaspoon of SunButter, (b) a 2.54 cm × 1.27 cm smear was made from a pea-sized amount of SunButter, (c) a 2.54 cm × 0.64 cm smear was made with a quarter teaspoon of SunButter, and (d) a small circular smear was the diameter of a pencil eraser.
The simulation training materials included SunButter, half and quarter teaspoons for measuring SunButter, a SunButter applicator, toilet paper, a freestanding toilet paper dispenser, a plastic doll, a plastic pretend potty, and a correspondence script and picture schedule flowchart. The correspondence script and picture schedule included the written words for each step (e.g., Get toilet paper) as well as a picture that depicted that step (e.g., a picture of a hand reaching toward a roll of toilet paper).
Identification of Putative Reinforcers
Potential reinforcers were identified for both participants by using a free operant preference assessment conducted under natural conditions.
Instruction, Data Collection, and Mastery Criterion
Baseline
This study comprised a treatment package to train hygiene skills. Participants were not assessed on each component of the treatment package but rather on the final objective: the ability to properly clean oneself following a bowel movement. Because both participants did not have bowel movements while in the clinic setting, the target skills were assessed via parent data collection.
Label Clean Versus Dirty
The labeling procedure involved a four-phase vocal prompt fading sequence. In Phase 1, the experimenter raised one card at a time and presented the SD: “Is it clean or dirty?” The experimenter then provided a full vocal model for the correct response (e.g., “It is clean”). This procedure was repeated for Trial 2. In Trials 3 and 4, the experimenter presented a partial vocal model for the correct response. In Trial 5, there was no vocal model provided, allowing participants the opportunity to respond independently. If a participant made an error on Trial 3 or 4, a full vocal model was used. If a participant made an error on Trial 5, a partial vocal model was provided and then, if necessary, a full vocal model was provided. The sequence for Phase 2 involved the presentation of the SD with a full vocal model on Trial 1. Trials 2 and 3 involved the presentation of the SD with a partial vocal model, and on Trials 4 and 5 the SD was presented with no prompt. The sequence for Phase 3 included a partial vocal model for Trials 1 and 2 and no vocal model for Trials 3, 4, and 5. In Phase 4, all trials were presented without a prompt. Criterion performance for all phases was two consecutive sessions at 90% accuracy. The experimenter rotated between “clean” and “dirty” trials until each card had been presented five times for a total of 10 trials. In order for a response to be considered correct, the participant had to say either “clean” or “dirty” when appropriate. If a participant made an error, the necessary prompt level needed to achieve a correct response was recorded. One session was composed of 10 trials, and sessions were run between one and four times daily. Both correct prompted responses and correct unprompted responses were reinforced.
Receptive Identification of Clean Versus Dirty
Receptive identification was taught using a most-to-least prompting procedure that included a probe trial. In order to ensure that the participants did not receive more assistance than needed, a probe trial was conducted for each target (clean and dirty) to determine the necessary prompt level. Each session started with the experimenter presenting three cards (clean card, dirty card, and clear card) in an array on the desk, stating the SD—“Touch [name of target]”—and allowing the participant 2 to 3 s to respond independently. If the participant made an error or did not respond, then the experimenter would repeat the SD and provide the next (i.e., more restrictive) prompt in the hierarchy. The prompt hierarchy included (a) no prompt, (b) gestural prompt, (c) partial physical prompt, and (d) full physical prompt. If necessary, the experimenter continued up the prompt hierarchy until the participant made a correct response. All correct responses were reinforced whether they were independent or prompted. Following the probe trials, while the materials were on the desk in an array of three, the SD—“Touch [name of target]”—was delivered and the participant was allowed 2 to 3 s to respond. The 2 to 3 s served as a prompt delay and provided an opportunity for the participant to respond independently. If the participant responded incorrectly or did not respond, then the predetermined prompt was provided. A trial was scored as correct when the participant touched the correct card following the SD. If a participant made an error, the necessary prompt level needed to achieve a correct response was recorded. The experimenter rotated between “clean” and “dirty” trials until each target had been presented five times for a total of 10 trials. A complete session was composed of 10 trials, and sessions were run one to four times daily. Both correct prompted responses and correct unprompted responses were reinforced.
Simulation Training
When a participant met mastery criteria for labeling clean versus dirty and receptive identification of clean versus dirty, which were set at three consecutive sessions at 90% or better, simulation training was initiated. Simulation training involved preparing a doll with the protocol-specified amount of SunButter for “dirty” trials or no SunButter for “clean” trials. Once the doll was prepared, the participant was presented with a correspondence training script and a picture schedule flowchart with all steps of the hygiene protocol chain delineated. In the initial phase, the experimenter read the script to the participant while pointing to the corresponding picture. The participant was required to complete each step. If prompting was necessary, the experimenter followed a prompt hierarchy until a correct response was achieved. In the second phase, the correspondence script and picture schedule flowchart were made available to the participant. The experimenter no longer read the text or pointed to pictures unless the participant did not respond or responded incorrectly. Praise was delivered after each step of the behavior chain, and a small edible was presented following the entire chain even if the learner required prompting. Scoring of correct versus incorrect trials was relative to each response in the entire chain. For example, one step included looking to see if the toilet paper was dirty after wiping the doll. If the participant did not engage in an orienting response to the toilet paper, this trial would be incorrect and a prompt would be provided until the orienting response occurred. Mastery criterion for simulation training was set at five consecutive sessions at 100% accuracy, which was higher than that for labeling or receptive identification. The rationale for this increase was that the simulation training was a series of responses in a chain, and any step not completed in the chain would result in the hygiene routine not being completed properly.
Generalization Probe Sessions
After the participants met mastery criterion in the simulation training, parents were asked to conduct generalization probes when the participants had a bowel movement at home. Parents were given a copy of the hygiene protocol and duplicate copies of data collection sheets for simultaneous data collection. Scoring of correct versus incorrect trials was relative to each response in the entire chain, just as it was in simulation training.
Interobserver Agreement
Interobserver agreement was collected for VB during 24% of labeling trials, 39% of receptive identification trials, and 64% of simulation training trials. For GB, 43% of labeling sessions, 50% of receptive identification sessions, and 67% of simulation training trials involved interobserver agreement data collection. The interobserver agreement for all of GB’s and VB’s sessions was 100%.
Results
GB
GB acquired the ability to label clean versus dirty in 35 sessions and met the mastery criterion for receptive identification of clean versus dirty in 12 sessions (Table 1). Following the acquisition of both labeling and receptive identification, simulation training was implemented, and GB achieved mastery performance within 30 sessions (Table 1).
Table 1.
Number of Sessions to Mastery
| Participant | Label clean versus dirty | Receptive identification of clean versus dirty | Simulation training (not including parent probes) |
|---|---|---|---|
| VB | 34 | 15 | 55 |
| GB | 35 | 12 | 26 |
Following simulation training trials, the parents of the participants were given modified data sheets and the hygiene protocol in order to collect generalization data at home. During in situ trials, two adults collected data on identical data sheets. Parents provided no instructions to the participants unless a prompt was needed, and participants were not provided with the script or flowchart. Five probe sessions were conducted for GB. On average, he responded with 87.5% accuracy with a range of 75% to 100% (Fig. 1). The sessions that scored below 100% were due to the participant not flushing the toilet. All other parts of the behavior chain were demonstrated during 100% of probe sessions for both participants. At a 6-month follow-up probe, GB responded with 100% accuracy (Fig. 1).
Fig. 1.
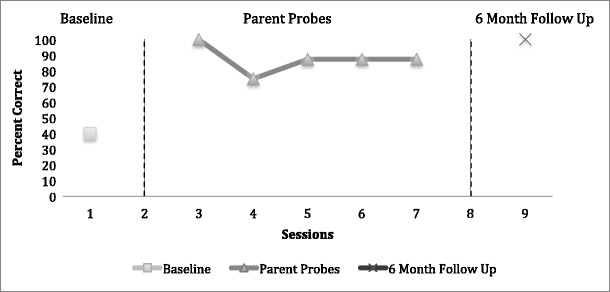
In vivo hygiene routine for GB
VB
The results of the acquisition trials for labeling and receptive identification were similar for VB, as he met mastery criterion for labeling clean versus dirty in 34 sessions and mastery criterion for receptive identification of clean versus dirty in 15 sessions. However, 55 training sessions were conducted, which was almost double those of the other participant (Table 1). The protocol for simulation training contained two training phases with a criterion of five consecutive sessions at 100%. It was also intended that the initial phase only be implemented with the first set of SunButter and toilet paper. However, due to experimenter error, the initial phase was run with all three sets of materials, which resulted in 10 additional sessions. Also, in addition to the first two phases, an additional mastery phase was implemented with each set of SunButter and toilet paper materials, which added 15 sessions for a total of 25 extra training sessions. After the initial teaching phase, the range of responding was 87.5% to 100% for the remaining sessions. It cannot be said with certainty if those extra training sessions were necessary; however, due to the high rates of accurate responding, it is likely that VB could have mastered this skill more quickly. Nevertheless, following the labeling and receptive identification trials, the objective of the simulation training trials was acquired.
Generalization probes for VB were also conducted. Data from six probe sessions were collected for VB, and on average he responded with 95.8% accuracy with a range of 87.5% to 100%. The sessions that scored below 100% were due to the participant not flushing the toilet (Fig. 2). During a 6-month follow-up probe, he responded with 100% accuracy (Fig. 2).
Fig. 2.

In vivo hygiene routine for VB
Discussion
The outcome of the current study was the acquisition of an essential behavioral repertoire across both learners and the verified generalization of skills for the two participants. Upon completion of the generalization probes, the family members reported quality of life changes involving their child’s independence, the alleviation of parental assistance centered on toilet use, and their child’s commendable hygiene and personal development. The interventions outlined in this study had the desired outcome, and the current study extends previous research by teaching post–bowel movement wiping skills using a doll simulation.
In the spirit of research honesty, the current investigation brought forward some of the challenges of applied research—specifically, the addition of unwarranted training trials rendered instruction inefficient. Fortunately, the excess training trials did not involve errors, were reinforced, and supported the experimenters’ end goal. The current study highlights the need for close, continuous monitoring of every phase of an applied research project. Another area of concern is the lack of a sound experimental design. Future research should be designed with a multiple baseline or multiple probes across participants. Additionally, the participants in this study possessed strong foundational verbal and motor skills. Thus, the profiles of the participants differ from those of other children with autism spectrum disorder (ASD) who are more severely affected. Therefore, the external validity of the current treatment package should be evaluated in future research.
The current study provides a serviceable guide to clinicians and caregivers interested in teaching hygiene skills to individuals with ASD. In conclusion, by establishing personal hygiene skills for after a bowel movement, this study addresses a skill that all people need but that has been the subject of very little previous research.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human Studies
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Azrin NH, Foxx RM. A rapid method of toilet training of the institutionalized retarded. Journal of Applied Behavior Analysis. 1971;4:89–99. doi: 10.1901/jaba.1971.4-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Fisher W, Piazza CC, Wierzbicki JJ. A water-prompting procedure for the treatment of urinary incontinence. Journal of Applied Behavior Analysis. 1993;26:473–474. doi: 10.1901/jaba.1993.26-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBlanc LA, Carr JE, Crossett SE, Bennett CM, Detweiler DD. Intensive outpatient behavioral treatment of primary urinary incontinence of children with autism. Focus on Autism and Other Developmental Disabilities. 2005;20:98–105. doi: 10.1177/10883576050200020601. [DOI] [Google Scholar]
- Post R, Kirkpatrick MA. Toilet training for a young boy with pervasive developmental disorder. Behavioral Interventions. 2004;19:45–50. doi: 10.1002/bin.149. [DOI] [Google Scholar]
- Stokes JV, Cameron MJ, Dorsey MF, Fleming E. Task analysis, correspondence training, and general case instruction for teaching personal hygiene skills. Behavioral Interventions. 2004;19:121–135. doi: 10.1002/bin.153. [DOI] [Google Scholar]


