Abstract
Atrial fibrillation (AF) is known to cause adverse remodeling of left atrium (LA). Radiofrequency catheter ablation (RFCA) of AF is associated with decrease in LA volume. However, the impact of RFCA on left atrial appendage (LAA) volume and hemodynamic function is not fully understood. We analyzed 123 patients who underwent cardiac magnetic resonance imaging (MRI) evaluation before and after RFCA in Korea University Anam Hospital. LA and LAA volume were measured before and after RFCA based on cardiac MRI. Baseline LA volume was 99.5 ± 38.4 cm3 and decreased to 74.6 ± 28.5 cm3 after RFCA (p < 0.001). LA diameter measured with transthoracic echocardiography was also decreased after RFCA (43.3 ± 6.2 mm at baseline and 39.9 ± 5.9 mm at follow up; p < 0.001). However, LAA volume was significantly increased after RFCA (19.4 ± 8.5 cm3 at baseline and 23.7 ± 13.3 cm3 at follow up; p < 0.001). Total ablation time and additional substrate modification was associated with change in LA volume. After RFCA, average LAA velocity measured by transesophageal echocardiography was increased to 51.0 cm/sec from 41.1 cm/sec (p < 0.001). In conclusion, LAA volume was increased after RFCA in contrast to LA volume. Our data raise a concern about worsening hemodynamics of LA and LAA following RFCA and long term clinical significance of enlarged LAA after RFCA needs further evaluation.
Introduction
Radiofrequency catheter ablation (RFCA) has emerged as a treatment of choice for antiarrhythmic drug (AAD) refractory symptomatic atrial fibrillation (AF) patients1. It is evident that RFCA is superior as compared with AAD for restoration and maintenance of sinus rhythm in AF patients2,3. Furthermore, RFCA is associated with significant improvements in quality of life1,4 and recent retrospective studies suggest that RFCA might also reduce ischemic stroke and all-cause mortality5–8.
Studies based on echocardiography and autopsy revealed that left atrial appendage (LAA) is the origin of thrombus formation in more than 90% of patients with non-valvular AF9–12. Thrombus and spontaneous echocontrast (SEC) in LAA and reduced LAA flow velocity are all associated with ischemic stroke in AF patients13–15. According to the SPAF-III study, annual risk of ischemic stroke in patients with dense SEC might reach 18.2% if adequate anticoagulation treatment is not given16. Additionally, LAA flow velocity less than 20 cm/sec was associated with 2.6 times increased risk of ischemic stroke16. Therefore, flow stasis in LAA and its consequences, which is SEC and thrombus formation, are important risk factors for developing clinical ischemic stroke. Recent studies suggested that LAA orifice area and LAA volume are also associated with increased risk of ischemic stroke17,18. Previous studies suggest that RFCA is associated with reverse remodeling of left atrium (LA)19–24. However, recent study performed by Wylie et al.25 showed that RFCA is associated with reduced atrial systolic function despite decreased LA volume which suggests that LA scar formation and consequent stiff LA are the principal mechanism for decreased LA volume following RFCA. Impaired LA function might predispose LAA to higher intraluminal pressure and may cause LAA to dilate similar to a balloon effect. Currently, the impact of RFCA on LAA is not fully revealed. Understanding the hemodynamic and mechanical impact of RFCA on LAA would be important to anticipate future risk of ischemic stroke and to determine anticoagulation strategy in AF patients. We performed this study to evaluate the influence of RFCA on both LA and LAA in AF patients.
Methods
Patients
Patients with AAD resistant AF undergoing first-time RFCA in Korea University Medical Center Anam Hospital were screened for their eligibility. All patients who underwent both baseline (pre-RFCA) and follow up (post-RFCA) cardiac magnetic resonance imaging (MRI) evaluation suitable for LAA size evaluation were enrolled. There was no specific exclusion criteria. The protocols of the current study were consistent with the ethical guidelines of the 2008 Helsinki Declaration. Institutional Review Board of Korea University Medical Center Anam Hospital ensured appropriate ethical and bioethical conduct and specifically approved this study. Written informed consent was waived since the current study is based on retrospective analysis.
Ablation procedure
Ablation procedure in our institution can be summarized as follows. Quadripolar, decapolar, and duo-decapolar catheters were positioned at right ventricle or superior vena cava, high right atrium, and coronary sinus, respectively. Continuous blood pressure monitoring and blood sampling were conducted by left femoral artery line. Double trans-septal punctures were performed using Brockenbrough needle and two SL1 sheaths. After positioning of circular mapping and ablation catheters, 3 dimensional mapping of LA was performed with either EnSite NavX/Velocity (St. Jude Medical, St. Paul, Minnesota) or CARTO (Biosense Webster, Irvine, California) system. Wide antral pulmonary vein isolation was performed in all procedures. In patients with paroxysmal AF, trigger focus evaluation was performed by AF induction with rapid atrial pacing under isoproterenol infusion and subsequent direct current cardioversion. End point of the procedure in paroxysmal AF patients was the absence of trigger focus. If non-pulmonary vein trigger was present, additional ablation was performed to eliminate non-pulmonary vein trigger. In persistent AF, rapid atrial pacing was performed to induce AF without isoproterenol infusion after pulmonary vein isolation. If no sustained AF (lasting for more than 5 minutes) was induced, the procedure was finished. Additional ablation such as complex fractionated atrial electrogram guided ablation or linear ablation were performed on operator’s discretion if sustained AF was induced after pulmonary vein isolation. End point of the procedure was the absence of inducibility. Additional substrate modification was also permitted for paroxysmal AF if the operator considered substrate modification to be more important than trigger point elimination.
Cardiac MRI
Follow up cardiac MRI was recommended during outpatient visit to all patients who had pre-RFCA MRI evaluation. Cardiac MRI was performed using a 3 T MR system (Achieva; Philips Medical Systems, Best, Netherlands) with a 32-element phased-array cardiac coil. Cardiac MRI data were acquired by using contrast-enhanced timing robust angiography sequence without ECG gating after injection of 0.2 mmol/kg of gadolinium contrast agent (Dotarem; Guerbet, S.A., Villepinte, France). The parameters of contrast-enhanced timing robust angiography sequence were as follows: parallel imaging using the sensitivity encoding technique with R = 2; acquisition time = 5 sec; a voxel size = 1 mm × 1 mm × 1.2 mm; TR/TE = 3.9 ms/1.1 ms; flip angle = 25°; bandwidth = 1106.2 Hz/pixel. Contrast media was injected at a rate of 2 ml/s via 18-gauge needle in the left or right arm vein by an automated power injector (Spectris Solaris EP; Medrad, Indianola, PA, USA); this was followed by an injection of a 40 ml normal saline bolus at the same rate. Using a commercially available software (Terarecon iNtuition; TeraRecon, Foster City, CA, USA), cardiac MRI data were evaluated by radiologist who specializes in the field of cardiac MRI (S.H. Hwang). The reviewer was blinded to all of the clinical data and measured the volume of LA and LAA. The LA and LAA cavities completely filled with gadolinium contrast agent were three-dimensionally reformatted. The reviewer traced and determined the endocardial boundaries of LA and LAA on cardiac MRI. The selected endocardial boundaries of LA and LAA excluded the pulmonary veins. Then, the LAA neck as the narrowest portion of LAA at the entrance into the LA was also selected to differentiate between the LA and LAA. Based on manually drawn endocardial boundaries of LA and LAA, the cardiac MRI voxels corresponding to the LA and LAA were selected respectively, and computed to measure the volumes (in mL) of LA and LAA. All measurements were re-evaluated and confirmed by Y.G. Kim and J. Shim and in case of any disagreement, it was resolved by discussion and re-tracing of endocardial boundaries. Representative images for LA and LAA volume measurements are presented in Supplementary Fig. S1.
Transesophageal echocardiography (TEE)
All patients underwent TEE evaluation before RFCA to confirm the absence of thrombus in LA and LAA. Routine views (high esophageal 0°, 45°, 60°, and 120° views) were obtained to evaluate LA, left ventricle (LV), right chambers, and valves. LAA was evaluated using at least three different views (high esophageal 0°, 45°, 60°, or 120° views). Thorough evaluations of LA and LAA were performed to reveal any evidence of SEC or thrombus. SEC was classified into grade 1 (very mild; minimal echogenicity; only detectable transiently; increasing gain setting required for the detection), grade 2 (mild; detectable without increasing gain setting), grade 3 (moderate; dense and swirling echogenic material; echogenic signal is denser in LAA compared to LA), or grade 4 (severe; dense and swirling echogenic material; echogenic signal is equivocal in LAA and LA). Dense SEC was defined as a composite of moderate and severe SEC. During LAA imaging, emptying (forward) and filling (backward) flow velocity of LAA were measured using pulsed wave Doppler analysis. All TEE evaluations were accompanied by transthoracic echocardiography (TTE) evaluations.
Outcome endpoints
The aim of the current study was to evaluate the impact of RFCA on LA and LAA volumes. Post-RFCA LA and LAA volumes measured with MRI were compared with pre-RFCA LA and LAA volumes respectively. LAA to LA volume ratio was defined as [LAA volume/(LA volume + LAA volume)]*100. The influence of clinical and procedural factors on ∆LA and ∆LAA volumes were also evaluated. The impact of AF type, presence of late recurrence, additional substrate modification, anterior line block with consequent delayed activation of LAA, and total ablation time were evaluated. The association between MRI findings and late recurrence, which was defined as any atrial tachyarrhythmia lasting for more than 30 seconds, was examined.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD). Categorical variables are presented as percentile values. Unpaired t-test and one-way ANOVA test were used to compare continuous variables. Paired t-test was performed to compare pre-RFCA LA and LAA volumes with post-RFCA LA and LAA volumes respectively. Categorical variables were compared with chi-square test or Fisher’s exact test as appropriate. Pearson product-moment correlation analysis was performed to examine correlation between two continuous variables. Receiver operating characteristic curve analysis was performed to evaluate predictive value of continuous variables for any specific state variable. Comparison of area under curve (AUC) of two ROC curves was performed by statistical method suggested by Hanley and McNeil26. Subgroup analysis was performed to examine clinical and procedural factors associated with ∆LA and ∆LAA volumes. Cox regression analysis was performed to calculate hazard ratio (HR) of late recurrence for each variable. All significance tests were two-tailed and p values of less than 0.05 were considered statistically significant. All statistical analyses were performed with SPSS version 21.0 (IBM, Armonk, NY, USA).
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
Results
Patient characteristics
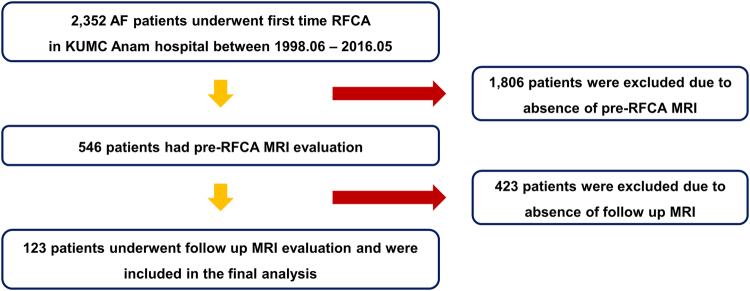
Between June 1998 and May 2016, a total of 2,352 patients with AF underwent first-time RFCA in Korea University Anam hospital. Cardiac MRI was performed just before the procedure in 546 patients. Remaining 1,806 patients who underwent computed tomography evaluation or did not perform any imaging modalities before RFCA were excluded from the current study. Among 546 patients who performed cardiac MRI before RFCA, 312 patients who completed 1 year follow up after first-time RFCA were indicated for follow up MRI and 123 patients who actually underwent follow up MRI were included in the final analysis (Fig. 1).
Figure 1.
Flow diagram of the study.
Baseline characteristics of 123 patients are summarized in Table 1. Mean age was 55.1 ± 10.6 years old and 80.5% of patients were male. Fifty three (43.1%) patients were diagnosed with paroxysmal AF. Mean CHA2DS2-VASc score was 1.2 ± 1.3. During follow up, 78 (63.4%) patients experienced late recurrence.
Table 1.
Baseline characteristics of the study patients.
| N = 123 | |
|---|---|
| Age (years) | 55.1 ± 10.6 |
| Male sex | 99 (80.5%) |
| Paroxysmal | 53 (43.1%) |
| Congestive heart failure | 5 (4.1%) |
| Hypertension | 42 (34.1%) |
| Diabetes mellitus | 10 (8.1%) |
| Cerebrovascular events | 12 (9.8%) |
| Vascular disease | 4 (3.2%) |
| Baseline LA volume (ml) | 101.2 ± 43.3 |
| Baseline LAA volume (ml) | 19.4 ± 8.5 |
| Average LAA flow velocity (cm/sec) | 41.3 ± 20.8 |
| LV ejection fraction (%) | 54.2 ± 6.0 |
| Hemoglobin (g/dl) | 14.9 ± 1.3 |
| WBC (×103/ul) | 6.4 ± 1.5 |
| Platelets (×103/ul) | 200.2 ± 39.6 |
| INR | 1.4 ± 0.6 |
| Creatinine (mg/dl) | 1.0 ± 0.2 |
| CHA2DS2-VASc | 1.2 ± 1.3 |
| Follow up duration (days) | 715.9 ± 227.8 |
| Mean MRI follow up duration (days) | 420.5 ± 171.5 |
| Substrate modification | 46 (37.4%) |
| Ablation time (min) | 108.4 ± 56.6 |
| Late recurrence | 78 (63.4%) |
INR: international normalized ratio; LA: left atrium; LAA: left atrial appendage; LV: left ventricle; MRI: magnetic resonance imaging; WBC: white blood cell count.
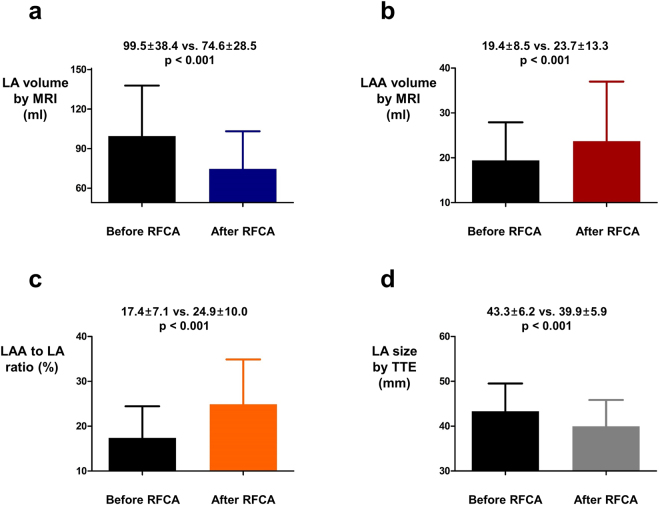
Change in LA and LAA volume after RFCA
After undergoing RFCA, LA volume measured with MRI was significantly decreased (99.5 ± 38.4 ml vs. 74.6 ± 28.5 ml; p < 0.001; Fig. 2a). However, LAA volume (19.4 ± 8.5 ml vs. 23.7 ± 13.3 ml; p < 0.001; Fig. 2b) and LAA to LA volume ratio (17.4 ± 7.1% vs. 24.9 ± 10.0%; p < 0.001; Fig. 2c) measured with MRI were significantly increased following RFCA. LA diameter measured by TTE on parasternal long axis view (43.3 ± 6.2 mm vs. 39.9 ± 5.9 mm; p < 0.001; Fig. 2d) was significantly decreased after RFCA similar to LA volume measured with MRI. ∆LAA and ∆LA volumes of individual patients are depicted in Supplementary Figs S2 and S3 respectively.
Figure 2.
The influence of RFCA on LA and LAA volume. (a) LA volume was significantly decreased after RFCA. (b,c) LAA volume and LAA to LA volume ratio were significantly increased after RFCA. (d) LA diameter measured by TTE was also significantly decreased after RFCA. LA: left atrium; LAA: left atrial appendage; RFCA: radiofrequency catheter ablation; TTE: transthoracic echocardiography.
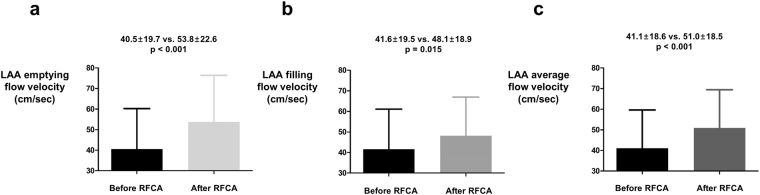
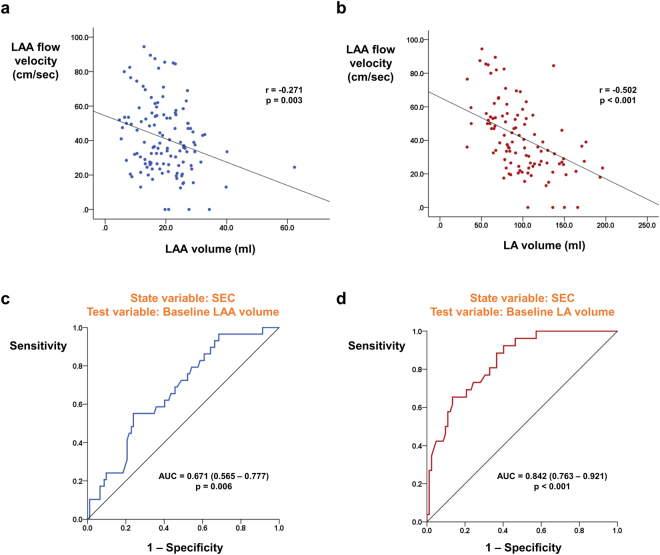
Impact of RFCA on LAA flow velocity and SEC
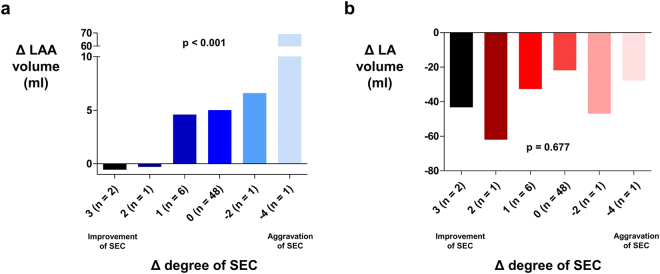
Among 123 patients included in the analysis, 59 patients had both baseline and follow up measurement of LAA flow velocity during TEE examination. The most frequent indication for follow up TEE study was re-do RFCA for recurred AF in 57 patients. Both forward (emptying; 40.5 ± 19.7 cm/sec vs. 53.8 ± 22.6 cm/sec; p < 0.001; Fig. 3a) and backward (filling; 41.6 ± 19.5 cm/sec vs. 48.1 ± 18.9 cm/sec; p = 0.015; Fig. 3b) flow velocity of LAA was significantly increased after RFCA. Average flow velocity of LAA was also improved after RFCA (41.1 ± 18.6 cm/sec vs. 51.0 ± 18.5 cm/sec; p < 0.001; Fig. 3c). Average ∆LAA flow velocity of individual patients are presented in Supplementary Fig. S4. Rhythm status during follow up TEE evaluation was recorded and among 59 patients, 34, 18, and 7 patients had sinus rhythm, atrial tachycardia, and AF respectively. Rhythm status had a significant impact on average LAA flow velocity with sinus rhythm and atrial tachycardia showing significantly higher LAA flow velocity as compared with AF (Supplementary Fig. S5). Sixty patients had both baseline and follow up TEE evaluation for SEC. Although baseline LAA volume showed significant correlation with LAA flow velocity, the degree of correlation was weaker than baseline LA volume (Fig. 4a,b). LA volume also outperformed LAA volume to predict the presence of SEC (AUC: 0.842 vs. 0.671; p < 0.001; Fig. 4c,d). However, ∆LAA volume showed better association with degree of change in SEC grade as compared with ∆LA volume. Nine patients showed improvements in SEC grade after undergoing RFCA. Two patients showed aggravation of SEC and 48 patients did not show any change in SEC grade following RFCA. Degree of improvement or aggravation in SEC grade showed association with ∆LAA volume but not with ∆LA volume (Fig. 5a,b).
Figure 3.
The influence of RFCA on LAA flow dynamics. Emptying (a), filling (b), and its average (c) flow velocities of LAA were significantly improved after RFCA. LA: left atrium; LAA: left atrial appendage; RFCA: radio frequency catheter ablation.
Figure 4.
The association between baseline LA and LAA volume with TEE findings. LA volume showed more close association with both average LAA flow velocity (a,b) and presence of SEC (c,d) as compared with LAA volume. LA: left atrium; LAA: left atrial appendage; SEC: spontaneous echocontrast; TEE: transesophageal echocardiography.
Figure 5.
Relationship between change in SEC grade and ∆LA & ∆LAA volume. Significant difference in ∆LAA volume was present among different groups stratified change in SEC grade (a). However, ∆LA volume showed no such association (b). LA: left atrium; LAA: left atrial appendage; SEC: spontaneous echocontrast.
Impact of substrate modification on LA and LAA volume
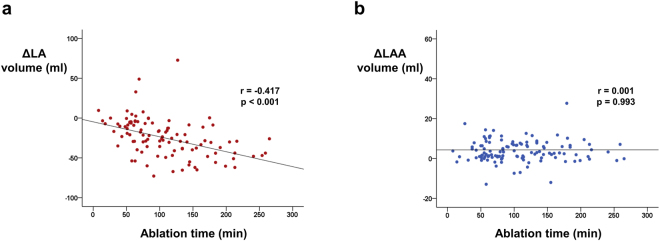
Patient with (n = 78) or without (n = 45) late recurrence showed no difference in ∆LA volume (−25.6 ± 29.2 ml vs. −23.7 ± 19.5 ml; p = 0.716; Table 2) and ∆LAA volume (5.0 ± 9.2 ml vs. 3.1 ± 5.4 ml; p = 0.218; Table 2). Non-paroxysmal AF (n = 70) as compared with paroxysmal AF (n = 53), showed larger baseline LA volume (114.9 ± 44.3 ml vs. 83.7 ± 35.3 ml; p < 0.001; Table 2) and greater decline in LA volume after RFCA (−29.6 ± 23.8 ml vs. −18.9 ± 27.5 ml; p = 0.034; Table 2). However, ∆LAA volume did not differ between the two groups (5.0 ± 9.6 ml vs. 3.4 ± 5.3 ml; p = 0.254; Table 2). Substrate modification in addition to pulmonary vein isolation (n = 77) was significantly associated with greater LA volume shrinkage after RFCA (−33.5 ± 26.3 ml vs. −12.1 ± 19.3 ml; p < 0.001; Table 2). In contrast, LAA volume was not affected by additional substrate modification (4.7 ± 9.2 ml vs. 3.6 ± 5.5 ml; p = 0.459; Table 2). Delayed activation of LAA results in simultaneous contraction of LAA and LV and therefore, might predispose LAA to higher intraluminal pressure. Successful block of anterior line (n = 31), confirmed by delayed activation of LAA, was associated with significant decrease in LA volume (−39.1 ± 28.1 ml vs. −20.8 ± 23.9 ml; p = 0.002; Table 2; see Supplementary Fig. S6 for representative intracardiac electrogram of delayed activation of LAA occurring simultaneously or after QRS complex). ∆LAA volume was numerically larger in anterior line block group (6.2 ± 12.8 ml vs. 3.7 ± 5.6 ml; p = 0.127; Table 2), but without statistical significance. Decrease in LA volume and increase in LAA volume after RFCA were consistent throughout all subgroups (Table 2). Total time for ablation was significantly associated with ∆LA volume with longer ablation time associated with greater shrinkage of LA (r = −0.417; p < 0.001; Fig. 6a), but not with ∆LAA volume (r = 0.001; p = 0.993; Fig. 6b).
Table 2.
Impact of clinical parameters on LA and LAA size.
| No late recurrence (n = 45) | Late recurrence (n = 78) | p value (between group) | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | p value (pre and post) | Mean | SD | p value (pre and post) | ||
| Baseline LA | 93.4 | 31.7 | 105.7 | 48.4 | 0.153 | ||
| F/U LA | 69.6 | 25.2 | 77.0 | 29.6 | 0.166 | ||
| ∆ LA | −23.7 | 19.5 | <0.001 | −25.6 | 29.2 | <0.001 | 0.716 |
| Baseline LAA | 20.4 | 6.7 | 18.9 | 9.3 | 0.336 | ||
| F/U LAA | 23.6 | 8.4 | 23.8 | 15.4 | 0.921 | ||
| ∆ LAA | 3.1 | 5.4 | <0.001 | 5.0 | 9.2 | <0.001 | 0.218 |
| Paroxysmal (n = 53) | Non-paroxysmal (n = 70) | ||||||
| Baseline LA | 83.7 | 35.3 | 114.9 | 44.3 | <0.001 | ||
| F/U LA | 66.0 | 23.1 | 80.4 | 30.2 | 0.004 | ||
| ∆ LA | −18.9 | 27.5 | <0.001 | −29.6 | 23.8 | <0.001 | 0.034 |
| Baseline LAA | 19.3 | 6.3 | 19.6 | 9.9 | 0.834 | ||
| F/U LAA | 22.6 | 7.7 | 24.5 | 16.4 | 0.433 | ||
| ∆ LAA | 3.4 | 5.3 | <0.001 | 5.0 | 9.6 | <0.001 | 0.254 |
| PVI only (n = 46) | PVI + Substrate modification (n = 77) | ||||||
| Baseline LA | 77.8 | 23.6 | 117.0 | 46.5 | <0.001 | ||
| F/U LA | 65.0 | 24.5 | 79.7 | 28.9 | 0.005 | ||
| ∆ LA | −12.1 | 19.3 | <0.001 | −33.5 | 26.3 | <0.001 | <0.001 |
| Baseline LAA | 20.2 | 6.5 | 19.0 | 9.5 | 0.420 | ||
| F/U LAA | 23.8 | 8.3 | 23.7 | 15.6 | 0.957 | ||
| ∆ LAA | 3.6 | 5.5 | <0.001 | 4.7 | 9.2 | <0.001 | 0.459 |
| No anterior line block (n = 92) | Anterior line block (n = 31) | ||||||
| Baseline LA | 97.6 | 42.3 | 113.7 | 45.2 | 0.108 | ||
| F/U LA | 74.7 | 28.2 | 73.0 | 28.6 | 0.780 | ||
| ∆ LA | −20.8 | 23.9 | <0.001 | −39.1 | 28.1 | <0.001 | 0.002 |
| Baseline LAA | 19.9 | 7.3 | 18.0 | 11.3 | 0.380 | ||
| F/U LAA | 23.5 | 8.5 | 24.2 | 22.4 | 0.873 | ||
| ∆ LAA | 3.7 | 5.6 | <0.001 | 6.2 | 12.8 | 0.012 | 0.127 |
F/U: follow up; LA: left atrium; LAA: left atrial appendage; PVI: pulmonary vein isolation; SD: standard deviation.
Figure 6.
Impact of total ablation time on change in LA and LAA volume. Longer ablation time was associated with greater decrease in LA volume (a). However, no association was found between total ablation time and ∆LAA volume (b). LA: left atrium; LAA: left atrial appendage.
MRI findings and risk of late recurrence
Both baseline and follow up MRI findings were not associated with the risk of late recurrence. In Cox regression analysis, HR was 1.002 (p = 0.421), 1.006 (p = 0.182), and 1.002 (p = 0.712) for baseline LA, follow up LA, and ∆LA volume respectively. LAA volume also was not associated with late recurrence: HR = 0.979 (p = 0.121) for baseline LAA; HR = 0.996 (p = 0.605) for follow up LAA, and HR = 1.007 (p = 0.528) for ∆LAA.
Discussion
The findings of the current study can be summarized as follows: (i) RFCA is associated with decreased LA volume (ii) However, LAA volume is increased after RFCA (iii) additional substrate modification and total ablation time are associated with greater decrease in LA volume (iv) LAA volume was increased after RFCA irrespective of presence of late recurrence, type of AF, procedure type, and ablation time (v) flow velocity of LAA is increased even in patients with late recurrence. Previous studies focused on the impact of RFCA on LA but not on LAA. However, it is LAA which have more profound impact on ischemic stroke in AF patients and therefore, influence of RFCA on LAA deserves more attention. The current study evaluated LA and LAA simultaneously using MRI and TEE in AF patients undergoing RFCA.
Decreased LA volume and increased LAA volume after RFCA
Previous studies consistently reported decreased size (or volume) of LA after RFCA in AF patients27. However, in contrast to LA size or volume, LA ejection fraction is not improved after RFCA25,27. In the study performed by John and his colleagues, LA end-systolic volume was decreased after RFCA but LA ejection fraction was also reduced25. Furthermore, reduced LA volume and systolic function was closely associated with the volume of LA scar related to RFCA25. Therefore, LA volume reduction after RFCA might not be a result of improved hemodynamics in LA but rather due to LA scar formation and shrinkage of LA which is often called ‘stiff LA syndrome’28. Our results support this concept. Patients who underwent additional substrate modification and longer duration of radiofrequency energy delivery showed greater decline in LA volume as compared with patients with pulmonary vein isolation only. Furthermore, the amount of LA and LAA volume change did not differ between patients with successful ablation and those who experienced late recurrence indicating that the change in LA and LAA volume is not the result of successful restoration of sinus rhythm but consequences of scar created by radiofrequency energy.
Increased LAA volume after RFCA also deserves further attention. LAA volume, area, and orifice area are known risk factors for ischemic stroke in patients with AF17,18. The current study demonstrated that LAA volume is increased after RFCA in AF patients. Furthermore, enlargement of LAA volume was independent from the presence of late recurrence, AF type, procedure type, and ablation time. The mechanism of increased LAA volume after RFCA is uncertain. Ablation scar might result in stiff LA wall which will not dilate sufficiently to receive incoming blood from pulmonary veins. As a consequence, LA pressure will rise and relatively compliant LAA might dilate in response to increased pressure in LA which is similar to a balloon effect. After RFCA, ∆LA volume did not show any association with ∆degree of SEC but ∆LAA volume revealed a significant association with ∆degree of SEC with increased LAA volume correlated with aggravation of SEC. Whether this increased LAA volume will actually lead to ischemic stroke in AF patients undergoing RFCA needs further investigation. Previous studies demonstrated that low LA compliance, represented by elevated LA pressure and decreased LA pulse pressure, is associated with electroanatomical remodeling of the LA and increased risk of late recurrence after AF ablation29,30. Whether RFCA, especially extensive ablation including LA substrate modification, actually leads to elevated LA pressure is not directly demonstrated in our study. However, increase in LAA volume in contrast to decreased LA volume raise a concern about adverse hemodynamic effect of RFCA on LA and LAA. Future studies should measure pre- and post-RFCA LA pressure to better understand the effect of RFCA on LA hemodynamics.
Increased flow velocity of LAA after RFCA
The mechanism of ischemic stroke in AF patients is still not conclusive. However, it is generally accepted that blood stasis caused by AF, especially in LAA, makes a suitable place for the development of fibrin-rich red thrombus14,31,32. The underlying pathophysiology of thrombus formation is significantly different from acute coronary syndrome in which platelets play a major role. Since the activation of coagulation cascade triggered by flow stasis is one of the main mechanism of thrombus formation and consequent ischemic stroke in AF patients, anticoagulants show significantly better efficacy compared to antiplatelets in terms of stroke prevention33,34. LAA, especially when blood stasis is accompanied, is the major source of thrombus formation and consequent cardio-embolic stroke. Therefore, it is not surprising that the flow velocity of LAA measured with TEE is a significant predictor of future ischemic stroke in AF patients16. Maintaining adequate emptying and filling velocity of LAA will have a significant benefit in terms of stroke prevention. According to our analysis, emptying, filling, and its average flow velocity of LAA were improved after RFCA. The results are in contrast to our previous analysis regarding LAA volume since RFCA was associated with increased LAA volume. The reason for this discrepancy is not clear, but we assume that LAA flow velocity was improved after RFCA since substantial number of patients were in atrial tachycardia, rather than atrial fibrillation, at the time of late recurrence (43 and 35 patient recurred as AF and AT respectively). The clinical importance of increased LAA flow velocity associated with RFCA is currently not determined and needs further evaluation.
Limitations
The current study have several limitations. First, this was a retrospective study. Our analyses are not free from intrinsic limitations of retrospective analysis. Second, follow up TEE evaluation was usually performed in patients with late recurrence. Follow up MRI was also preferentially performed in patients who experienced late recurrence.
Conclusions
In conclusion, LA volume is decreased after RFCA which is probably due to stiff LA related to scar formation. LAA volume, in contrast to LA, is increased after RFCA. Clinical significance of increased LAA volume after RFCA needs further evaluation in future trials.
Electronic supplementary material
Author Contributions
J. Shim had full access to all data in this study and takes responsibility for data integrity and analytical accuracy. Y.G. Kim, J. Shim, and Y.H. Kim were responsible for study design. Y.G. Kim and S.K. Oh were responsible for data collection. Y.G. Kim, H.S. Park, K.N. Lee, J.I. Choi and Y.H. Kim interpreted and analyzed the data. S.H. Hwang conducted imaging analysis. Y.G. Kim and J. Shim conducted the statistical analysis. Y.G. Kim drafted the manuscript. All authors contributed to the editing and final approval of the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-26212-y.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kim YG, Shim J, Choi JI, Kim YH. Radiofrequency Catheter Ablation Improves the Quality of Life Measured with a Short Form-36 Questionnaire in Atrial Fibrillation Patients: A Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0163755. doi: 10.1371/journal.pone.0163755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilber DJ, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303:333–340. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 3.Stabile G, et al. Catheter ablation treatment in patients with drug-refractory atrial fibrillation: a prospective, multi-centre, randomized, controlled study (Catheter Ablation For The Cure Of Atrial Fibrillation Study) Eur Heart J. 2006;27:216–221. doi: 10.1093/eurheartj/ehi583. [DOI] [PubMed] [Google Scholar]
- 4.Jais P, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation. 2008;118:2498–2505. doi: 10.1161/CIRCULATIONAHA.108.772582. [DOI] [PubMed] [Google Scholar]
- 5.Friberg L, Tabrizi F, Englund A. Catheter ablation for atrial fibrillation is associated with lower incidence of stroke and death: data from Swedish health registries. Eur Heart J. 2016;37:2478–2487. doi: 10.1093/eurheartj/ehw087. [DOI] [PubMed] [Google Scholar]
- 6.Karasoy D, et al. Oral anticoagulation therapy after radiofrequency ablation of atrial fibrillation and the risk of thromboembolism and serious bleeding: long-term follow-up in nationwide cohort of Denmark. Eur Heart J. 2015;36:307–314a. doi: 10.1093/eurheartj/ehu421. [DOI] [PubMed] [Google Scholar]
- 7.Sjalander S, et al. Assessment of Use vs Discontinuation of Oral Anticoagulation After Pulmonary Vein Isolation in Patients With Atrial Fibrillation. JAMA Cardiol. 2017;2:146–152. doi: 10.1001/jamacardio.2016.4179. [DOI] [PubMed] [Google Scholar]
- 8.Marrouche NF, et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N Engl J Med. 2018;378:417–427. doi: 10.1056/NEJMoa1707855. [DOI] [PubMed] [Google Scholar]
- 9.Holmes DR, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009;374:534–542. doi: 10.1016/S0140-6736(09)61343-X. [DOI] [PubMed] [Google Scholar]
- 10.Blackshear JL, Odell JA. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61:755–759. doi: 10.1016/0003-4975(95)00887-X. [DOI] [PubMed] [Google Scholar]
- 11.Stoddard MF, Dawkins PR, Prince CR, Ammash NM. Left atrial appendage thrombus is not uncommon in patients with acute atrial fibrillation and a recent embolic event: a transesophageal echocardiographic study. J Am Coll Cardiol. 1995;25:452–459. doi: 10.1016/0735-1097(94)00396-8. [DOI] [PubMed] [Google Scholar]
- 12.Aberg H. Atrial fibrillation. I. A study of atrial thrombosis and systemic embolism in a necropsy material. Acta Med Scand. 1969;185:373–379. doi: 10.1111/j.0954-6820.1969.tb07351.x. [DOI] [PubMed] [Google Scholar]
- 13.Patel SV, Flaker G. Is early cardioversion for atrial fibrillation safe in patients with spontaneous echocardiographic contrast? Clin Cardiol. 2008;31:148–152. doi: 10.1002/clc.20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Black IW. Spontaneous echo contrast: where there’s smoke there’s fire. Echocardiography. 2000;17:373–382. doi: 10.1111/j.1540-8175.2000.tb01153.x. [DOI] [PubMed] [Google Scholar]
- 15.Bernhardt P, Schmidt H, Hammerstingl C, Luderitz B, Omran H. Patients with atrial fibrillation and dense spontaneous echo contrast at high risk a prospective and serial follow-up over 12 months with transesophageal echocardiography and cerebral magnetic resonance imaging. J Am Coll Cardiol. 2005;45:1807–1812. doi: 10.1016/j.jacc.2004.11.071. [DOI] [PubMed] [Google Scholar]
- 16.Transesophageal echocardiographic correlates of thromboembolism in high-risk patients with nonvalvular atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators Committee on Echocardiography. Ann Intern Med 128, 639–647 (1998). [DOI] [PubMed]
- 17.Lee JM, et al. Impact of increased orifice size and decreased flow velocity of left atrial appendage on stroke in nonvalvular atrial fibrillation. Am J Cardiol. 2014;113:963–969. doi: 10.1016/j.amjcard.2013.11.058. [DOI] [PubMed] [Google Scholar]
- 18.Lee JM, et al. Additional value of left atrial appendage geometry and hemodynamics when considering anticoagulation strategy in patients with atrial fibrillation with low CHA2DS2-VASc scores. Heart Rhythm. 2017;14:1297–1301. doi: 10.1016/j.hrthm.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 19.Bax JJ, Marsan NA, Delgado V. Non-invasive imaging in atrial fibrillation: focus on prognosis and catheter ablation. Heart. 2015;101:94–100. doi: 10.1136/heartjnl-2013-305150. [DOI] [PubMed] [Google Scholar]
- 20.Delgado V, et al. Fate of left atrial function as determined by real-time three-dimensional echocardiography study after radiofrequency catheter ablation for the treatment of atrial fibrillation. Am J Cardiol. 2008;101:1285–1290. doi: 10.1016/j.amjcard.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 21.Marsan NA, et al. Comparison of left atrial volumes and function by real-time three-dimensional echocardiography in patients having catheter ablation for atrial fibrillation with persistence of sinus rhythm versus recurrent atrial fibrillation three months later. Am J Cardiol. 2008;102:847–853. doi: 10.1016/j.amjcard.2008.05.048. [DOI] [PubMed] [Google Scholar]
- 22.Hof IE, et al. Pulmonary vein antrum isolation leads to a significant decrease of left atrial size. Europace. 2011;13:371–375. doi: 10.1093/europace/euq464. [DOI] [PubMed] [Google Scholar]
- 23.Jayam VK, et al. Atrial volume reduction following catheter ablation of atrial fibrillation and relation to reduction in pulmonary vein size: an evaluation using magnetic resonance angiography. J Interv Card Electrophysiol. 2005;13:107–114. doi: 10.1007/s10840-005-0215-3. [DOI] [PubMed] [Google Scholar]
- 24.Tsao HM, et al. Morphologic remodeling of pulmonary veins and left atrium after catheter ablation of atrial fibrillation: insight from long-term follow-up of three-dimensional magnetic resonance imaging. J Cardiovasc Electrophysiol. 2005;16:7–12. doi: 10.1046/j.1540-8167.2005.04407.x. [DOI] [PubMed] [Google Scholar]
- 25.Wylie JV, Jr., et al. Left atrial function and scar after catheter ablation of atrial fibrillation. Heart Rhythm. 2008;5:656–662. doi: 10.1016/j.hrthm.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 27.Xiong B, et al. The Effect of Catheter Ablation on Left Atrial Size and Function for Patients with Atrial Fibrillation: An Updated Meta-Analysis. PLoS One. 2015;10:e0129274. doi: 10.1371/journal.pone.0129274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gibson DN, et al. Stiff left atrial syndrome after catheter ablation for atrial fibrillation: clinical characterization, prevalence, and predictors. Heart Rhythm. 2011;8:1364–1371. doi: 10.1016/j.hrthm.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 29.Park J, et al. High left atrial pressures are associated with advanced electroanatomical remodeling of left atrium and independent predictors for clinical recurrence of atrial fibrillation after catheter ablation. Heart Rhythm. 2014;11:953–960. doi: 10.1016/j.hrthm.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 30.Park J, et al. Low Left Atrial Compliance Contributes to the Clinical Recurrence of Atrial Fibrillation after Catheter Ablation in Patients with Structurally and Functionally Normal Heart. PLoS One. 2015;10:e0143853. doi: 10.1371/journal.pone.0143853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merino A, et al. Echocardiographic “smoke” is produced by an interaction of erythrocytes and plasma proteins modulated by shear forces. J Am Coll Cardiol. 1992;20:1661–1668. doi: 10.1016/0735-1097(92)90463-W. [DOI] [PubMed] [Google Scholar]
- 32.Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet. 2009;373:155–166. doi: 10.1016/S0140-6736(09)60040-4. [DOI] [PubMed] [Google Scholar]
- 33.van Walraven C, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002;288:2441–2448. doi: 10.1001/jama.288.19.2441. [DOI] [PubMed] [Google Scholar]
- 34.Connolly SJ, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364:806–817. doi: 10.1056/NEJMoa1007432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).