Abstract
Background
Although nerve-sparing robot-assisted radical prostatectomy (NS-RALP) is performed, a large number of patients still experience erectile dysfunction (ED) after surgery.
Aim
To evaluate the efficacy and safety of tadalafil 5 mg once daily (OaD) in ED treatment over 2 years and investigate the cause of vascular ED after NS-RARP.
Methods
We retrospectively evaluated 95 men who underwent NS-RARP and had a penile rehabilitation treatment with tadalafil 5 mg OaD. They were classified into 3 groups: tadalafil 5 mg OaD for 2 years (group I), tadalafil 5 mg OaD for 1 year (group II), and no tadalafil (group III). All patients in group I underwent penile color duplex ultrasound to evaluate the cause of vascular ED.
Outcomes
Patients were surveyed using the abridged 5-item International Index of Erectile Function (IIEF-5).
Results
Statistically significant improvements were observed in group I for all IIEF-5 domain scores (P = .000). There was no statistically significant difference in recovery of erectile function (EF) the 2-year follow-up between groups I and II. Sub-analysis based on NS status showed no difference in recovery of EF. However, group I showed better trends in EF improvement. Those with venogenic ED had poor responses compared with those with arteriogenic ED or unremarkable findings with tadalafil 5-mg OaD treatment (14.2% vs 55.0% vs 53.3%). The overall side effects included hot flushing in 9.5%, headache in 7.1%, and dizziness in 2.3% of patients.
Clinical Implications
Long-term usage of tadalafil 5 mg OaD after RARP can be an effective option for penile rehabilitation.
Strengths and Limitations
The present study is a retrospective study with a relatively small sample.
Conclusions
Although the responses of patients with venogenic ED were limited compared with those with arteriogenic ED, tadalafil 5-mg OaD treatment was well tolerated and significantly improved EF up to 2 years after NS-RARP.
Kim S, Sung GT. Efficacy and Safety of Tadalafil 5 mg Once Daily for the Treatment of Erectile Dysfunction After Robot-Assisted Laparoscopic Radical Prostatectomy: A 2-Year Follow-Up. Sex Med 2018;6:108–114.
Key Words: Erectile Dysfunction, Penile Rehabilitation, Phosphodiesterase Type 5 Inhibitor, Robot-Assisted Radical Prostatectomy
Introduction
Radical prostatectomy (RP) has been the primary treatment modality for localized prostate cancer and is considered the best option for improving patient survival compared with conservative management.1, 2 However, RP is associated with a variable loss of urinary continence and erectile function (EF) postoperatively. With an increased rate of RP in young men, a greater emphasis must be placed on the appropriate management of urinary continence and erectile dysfunction (ED) to address patients' quality of life. Recent advances in surgical anatomy and improvements in surgical techniques have yielded satisfactory urinary continence outcomes after RP. Further, the advent of pioneering nerve-sparing (NS) robot-assisted laparoscopic radical prostatectomy (RALP) has significantly increased the potency rate after RP.1, 2, 3 However, although NS-RALP is performed, a large number of patients still experience ED after surgery. After RP, the reported ED incidence rates vary from 30% to 87%.4, 5 Although anatomic NS-RARP promises a high likelihood of postoperative recovery from ED, many men require more than 2 years to satisfactorily return to their baseline function, which can result in absent or decreased EF.6 Several penile rehabilitation (PR) programs have been introduced; however, most have achieved modest outcomes. After its advent in 1998, orally administered phosphodiesterase 5 inhibitors (PDE5-Is) have been increasingly used as the 1st-line management option for ED after RP. A recent literature review showed that PDE5-Is are safe and effective in treating patients with ED after RP. The administration of PDE5-Is once daily (OaD) has proved to have a protective role in ED, and early administration of PDE5-Is helps prevent cavernosal hypoxia, which leads to smooth muscle apoptosis and penile fibrosis.7, 8, 9, 10, 11 Although PDE5-Is are the most frequently recommended treatment for ED after RP, a consensus has not been reached on their use, such as time of initiation, treatment duration, or treatment regimen. Some investigators have recommended starting oral PDE5-Is immediately after an NS procedure to achieve optimal recovery of erections after 2 years, whereas others have reported compliance issues with the regimen, which can pose a significant barrier to an effective treatment. However, patients undergoing NS-RARP could represent a unique cohort who might be more motivated with higher expectations for recovery of potency.
Aims
This study analyzed the long-term clinical efficacy and safety of PR using tadalafil 5 mg OaD for more than 2 years in the treatment of patients with ED who underwent NS-RARP for clinically localized prostate cancer.
Methods
We retrospectively evaluated the records of 95 patients who underwent NS-RARP by a single experienced surgeon for localized prostate cancer from March 2010 through December 2013. The standard NS-RALP techniques, including bladder neck preservation, interfascial NS, and posterior urethral reconstruction, were performed in all patients. Patients with localized prostate cancer with clinical stage no higher than T2, Gleason score lower than 8, serum prostate-specific antigen level lower than 20 ng/mL, and normal preoperative EF were included in the study. Preoperative EF was assessed by the 5-item International Index of Erectile Function (IIEF-5). We excluded patients who underwent non–NS-RALP and hormonal or radiation therapy and those who received any kind of preoperative ED treatment.
Of the 95 patients, 59 were prescribed with tadalafil and 36 patients were not. In the tadalafil group, all patients were prescribed with tadalafil at a dose of 5 mg OaD; tadalafil was taken 1 hour before bedtime. Oral tadalafil 5-mg OaD treatment was initiated soon after Foley catheter removal within 7 to 10 days after surgery.
The tadalafil group was further stratified based on duration of tadalafil intake: 2-year tadalafil group (group I) and 1-year tadalafil group (group II). Patients who were not prescribed tadalafil were designated as the non-tadalafil group (group III). In groups I and II, all patients were counseled on ED, tadalafil intake, and its side effects at each visit. All 3 groups were followed up for 2 years after surgery. Patient age, clinical stage, Gleason score, comorbidities, and drug side effects were retrospectively reviewed using medical records after receiving approval from the institutional review board. Postoperative EF was assessed through patients' responses to the IIEF-5. Then, each group was classified by NS status: bilateral NS and unilateral NS procedures. Positive responders were those patients whose combined score for question 2 (“When you had erections with sexual stimulation, how often were your erections hard enough for penetration?”) and question 3 (“During sexual intercourse, how often were you able to maintain your erection after you had penetrated your partner?”) on the IIEF-5 was at least 8.
The IIEF-5 was administered before surgery and at 6 months, 1 year, and 2 years after surgery in all patient groups. Outcomes from the tadalafil group and the non-tadalafil group were compared and analyzed according to the NS status based on the patients' IIEF-5 score. In the subgroup analysis, we routinely performed penile color duplex ultrasound (PCDU) using vasoactive intracavernosal injections (ICIs) 1 year after surgery in group I to evaluate the therapeutic responses to tadalafil 5-mg OaD treatment. ED was categorized as arteriogenic, venogenic, or unremarkable depending on the PCDU findings. Arteriogenic ED was defined as the difference in peak systolic velocities greater than 10 cm/s or no greater than 30 cm/s between the 2 cavernosal arteries, and venogenic ED was defined as end-diastolic velocities of the cavernosal artery greater than 5 cm/s. Unremarkable findings were defined as peak systolic velocities and end-diastolic velocities of the 2 cavernosal arteries showing a normal range and spectral waveform.
Categorical variables were presented as frequency and percentage and continuous variables were presented as mean and SD. The Pearson χ2 test or Fisher exact test was used for categorical variables and 1-way analysis of variance or the Kruskal-Wallis test was used for continuous numerical variables. 2-factor analysis of variance was used to test the difference between group and period, and then the Wilcoxon rank sum test or paired t-test was used to test the differences in IIEF-5 domains between time points. 1-way analysis of variance or the Kruskal-Wallis test also was used to test the differences in IIEF-5 domains between groups; Bonferroni correction was applied to determine the significant difference between the 2 groups. The Kaplan-Meier estimates of the cumulative incidence of each end point were conducted for the 2-year and 1-year tadalafil and non-tadalafil groups. The log-rank test was used to investigate the difference in the recovery of erection between groups. Statistical significance was set at an α value equal to 0.05, and all P values were 2-sided. Data manipulation and statistical analyses were conducted using SPSS 19.0 (IBM Corp, Armonk, NY, USA) and Medcalc 11.6.1.0 (Medcalc, Ostend, Belgium).
Results
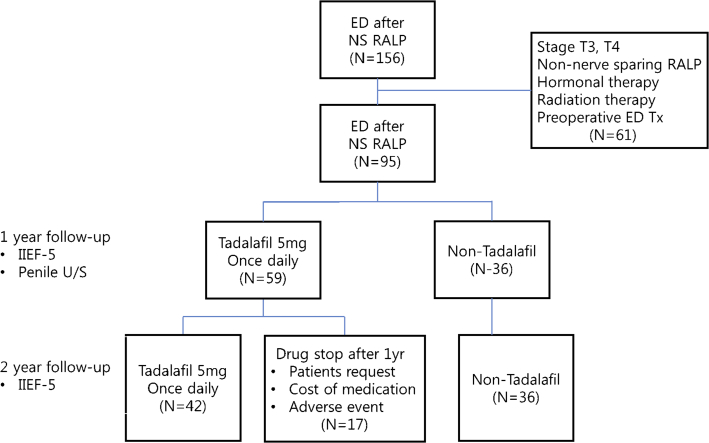
All 95 patients who were followed up for 2 years after surgery were included in the present study. Group I included 42 patients who were prescribed tadalafil 5-mg OaD treatment for 2 years after surgery, and group II included 17 patients who chose to stop taking tadalafil 5 mg OaD 1 year after surgery. Group III included 36 patients who were not on tadalafil 5-mg OaD treatment (Figure 1). The patients' mean age was 67.9 ± 7 years, and their mean prostate-specific antigen level was 9.7 ± 7.3. The pathologic stage for all patients was T2 localized prostate cancer. There was no statistically significant difference in patient characteristics among the 3 groups (Table 1). Patients in groups I and III were subdivided according to NS status. In group I, 30 patients (71.4%) underwent the bilateral NS procedure and 12 patients (28.6%) underwent the unilateral NS procedure. In group III, the bilateral NS procedure was performed in 23 patients (63.9%) and the unilateral NS procedure was performed in 13 patients (36.1%).
Figure 1.
Results of penile color duplex U/S with vasoactive intracavernosal injection analysis. ED = erectile dysfunction; IIEF-5 = 5-item International Index of Erectile Function; NS RALP = nerve-sparing robot-assisted laparoscopic radical prostatectomy; Tx = treatment; U/S = ultrasound.
Table 1.
Baseline patient characteristics
| Variables | Overall | Group I | Group II | Group III | P value |
|---|---|---|---|---|---|
| All patients | 95 (100) | 42 (44.2) | 17 (17.9) | 36 (37.9) | — |
| Age (y) | |||||
| Mean ± SD | 67.9 ± 7 | 66.5 ± 7.6 | 68.7 ± 5.1 | 69.2 ± 7 | .479∗ |
| Median (range) | 69 (46–85) | 68 (46–77) | 69 (58–77) | 69.5 (58–85) | |
| Body mass index | |||||
| Mean ± SD | 24.4 ± 2.7 | 24.6 ± 2.9 | 23.4 ± 2.8 | 24.5 ± 2.3 | .390∗ |
| Median (range) | 24.4 (18.1–32) | 24.5 (19.7–31.1) | 24.1 (18.1–28.4) | 24.3 (20.1–32) | |
| Diabetes mellitus | 15 (15.8) | 10 (23.8) | 2 (11.8) | 3 (8.3) | .154† |
| Hypertension | 42 (44.2) | 20 (47.6) | 6 (35.3) | 16 (44.4) | .688† |
| Tuberculosis | 10 (10.5) | 7 (16.7) | 2 (11.8) | 1 (2.8) | .135† |
| Hepatitis | 4 (4.2) | 3 (7.1) | 0 (0.0) | 1 (2.8) | .401† |
| Prostate-specific antigen | |||||
| Mean ± SD | 9.7 ± 7.3 | 10.6 ± 8.5 | 10 ± 6.4 | 8.4 ± 5.9 | .685∗ |
| Median (range) | 7.6 (0.1–50.8) | 7.7 (3.5–50.8) | 7.7 (4.5–28.2) | 7.6 (0.1–35.3) | |
| Clinical stage | |||||
| T2a | 20 (21.1) | 13 (31.0) | 3 (17.6) | 4 (11.1) | .039† |
| T2b | 2 (2.1) | 2 (4.8) | 0 (0.0) | 0 (0.0) | |
| T2c | 73 (76.8) | 27 (64.3) | 14 (82.4) | 32 (88.9) | |
| Biopsy Gleason score sum | |||||
| 4–6 | 36 (37.9) | 10 (23.8) | 5 (29.4) | 21 (58.3) | .028† |
| 7 | 56 (58.9) | 30 (71.4) | 12 (70.6) | 14 (38.9) | |
| 8 | 2 (2.1) | 1 (2.4) | 0 (0.0) | 1 (2.8) | |
| Nerve sparing | |||||
| Unilateral | 33 (34.7) | 12 (28.6) | 8 (47.1) | 13 (36.1) | .392† |
| Bilateral | 62 (65.3) | 30 (71.4) | 9 (52.9) | 23 (63.9) |
By Kruskal-Wallis test.
By χ2 test.
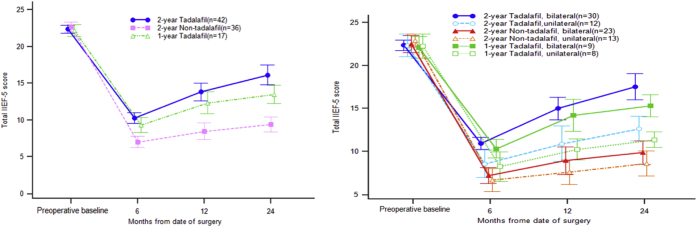
33 patients (34.7%) had a positive response and could achieve a satisfactory erection; group I showed the best EF recovery. At 6 months, 1 year, and 2 years, the IIEF-5 total scores of groups I vs III were 10.3 ± 2.3 vs 7 ± 2.2, 13.8 ± 3.9 vs 8.5 ± 3.3, and 16.1 ± 4.3 vs 9.4 ± 3 (P = .000), respectively. Based on the duration of tadalafil 5-mg OaD treatment, statistically significant improvements (P = .000) in EF were observed in group I for all 5 domains of the IIEF-5 score; group III showed only slight improvement in the IIEF-5 total score at 1-year and 2-year follow-ups (Table 2, Figure 2). When comparing group I with group II, 19 (45.2%) of the 42 patients in group I and 6 (35.3%) of the 17 patients in group II responded positively. However, there was no statistically significant difference in EF recovery at the 2-year follow-up between groups I and II (P = .063). Furthermore, when we analyzed groups based on NS status (bilateral vs unilateral), there was no statistically significant difference between the 2 groups at the 2-year follow-up. However, group I showed a better trend in EF improvement than group II (Figure 2). The improvement in group I was greater than that in group II (1–2 years = 2.3, P = .000, vs 1–2 years = 1.1, P = .024; Table 2).
Table 2.
Mean IIEF-5 scores at baseline and 6-month, 1-year, and 2-year follow-ups
| IIEF-5 total score |
P value∗ |
|||||
|---|---|---|---|---|---|---|
| Preoperative baseline | 6 mo | 1 y | 2 y | 6 mo vs 1 y | 1 vs 2 y | |
| Group I | 22.4 ± 1.7 (18–25) | 10.3 ± 2.3 (5–15) | 13.8 ± 3.9 (5–22) | 16.1 ± 4.3 (10–24) | .000 | .000 |
| Group II | 22.2 ± 1.6 (19–25) | 9.4 ± 2 (7–13) | 12.4 ± 2.8 (8–18) | 13.5 ± 2.5 (9–17) | .001 | .024 |
| Group III | 22.6 ± 2 (16–25) | 7 ± 2.2 (5–13) | 8.5 ± 3.3 (4–15) | 9.4 ± 3 (4–16) | .002 | .000 |
| P value† | 0.439 | 0.000 | 0.000 | 0.000 | ||
| Group I vs II‡ | 0.345 | 0.152 | 0.097 | 0.063 | ||
| Group I vs III‡ | 0.237 | 0.000 | 0.000 | 0.000 | ||
IIEF-5 = 5-item International Index of Erectile Function.
By Wilcoxon rank sum test.
By Kruskal-Wallis test.
By Mann Whitney U-test.
Figure 2.
Comparison of IIEF-5 total scores between nerve-sparing groups after nerve-sparing robot-assisted laparoscopic radical prostatectomy. IIEF-5 = 5-item International Index of Erectile Function.
42 patients in group I underwent PCDU with a vasoactive ICI. Arteriogenic and venogenic cases of ED were observed in 20 patients (47.6%) and 7 patients (16.6%), respectively. 15 patients (35.7%) showed unremarkable findings. Patients with venogenic ED had poor responses to tadalafil 5-mg OaD treatment (14.2%). However, those with arteriogenic ED or unremarkable findings had significantly improved EF with tadalafil 5-mg OaD treatment (55% and 53.3%; Table 3).
Table 3.
Results of PCDU with vasoactive intracavernosal injection analysis
| PCDU | Patients, n (%) | Positive response, n (%) |
|---|---|---|
| Total | 42 (100) | 19 (42.2) |
| Arteriogenic | 20 (47.6) | 11 (55.0) |
| Venogenic | 7 (16.6) | 1 (14.2) |
| Unremarkable | 15 (35.7) | 8 (53.3) |
PCDU = penile color duplex ultrasound.
There was no serious treatment-related adverse event in this study. The total complication rate was 19%, and the most common side effects were flushing (9.5%, n = 4), headache (7.1%, n = 3), and dizziness (2.3%, n = 1). All side effects were controlled using conservative management (Table 4).
Table 4.
Adverse events
| Adverse events | Patients, n (%) |
|---|---|
| Hot flushing | 4 (9.5) |
| Headache | 3 (7.1) |
| Dizziness | 1 (2.3) |
| Backache | 0 |
| Indigestion | 0 |
| Total | 8 (19) |
Discussion
ED is one of the most common sequelae after RP. Recently, several pathophysiologic theories have been proposed for ED after RP, including nerve and vascular injuries.12, 13, 14 The most reliable pathophysiology of ED after RP is that of neurapraxia, which leads to temporarily decreased oxygenation and subsequent structural changes in the penile tissue. During neurapraxia, the penile tissue is in a constant state of low oxygen supply, which can lead to smooth muscle apoptosis and fibrosis.15 This also is related to veno-occlusive dysfunction.16 PR was introduced to block this process. PR is defined as “the use of any drug or device after RP to maximize ED recovery.”17 This PR concept was 1st introduced by Montorsi et al18 who showed in a small cohort of patients that the early postoperative intracavernous administration of alprostadil improved EF recovery rates after RP in 1997. Since then, numerous studies have reported that a PR program is useful in improving EF, particularly after NS-RP.14 However, there are several ongoing debates on the efficacy of PR in the recovery of postoperative EF. Furthermore, the ideal form or component of PR programs does not exist. According to the International Society for Sexual Medicine, 87% of urologists use some kind of PR and commonly use PDE5-Is.19 The current medical literature suggests that PDE5-Is are the 1st-line treatment modality for ED after RP. PDE5-Is are effective and easy to use with minimal side effects. As the 2ndline treatment, ICI or a vacuum erection device (VED) was recommended. Penile prostheses can be used as a last option for patients who do not respond to such treatments or for those who want a permanent solution.20
In the REACTT study, the effect of tadalafil after RP was tested by comparing tadalafil 5 mg OaD, tadalafil 20 mg on demand, and placebo after NS-RP. At the end of the study, significant improvement was found only in the OaD tadalafil group. The investigators concluded that although tadalafil did not improve drug-unassisted EF recovery after RP, OaD treatment could protect against penile structural changes.21 Moncada et al22 reported that the administration of tadalafil OaD significantly shortened the time to EF recovery during a 9-month course of treatment. Conversely, a recent randomized trial evaluating patients who underwent bilateral NS-RARP failed to show statistically significant differences in patients receiving sildenafil OaD vs on demand at 13-month follow-up.23 However, these results are limited by the small number of patients evaluated (N = 100), the lack of a placebo group, and the relatively short follow-up period. In the present study, we treated patients with ED after NS-RALP with tadalafil 5 mg OaD more than 2 years after surgery. In a previous study, tadalafil 5-mg OaD treatment for patients with ED after NS-RALP was well tolerated at 1-year follow-up and significantly improved EF compared with treatment for the non-tadalafil group.24 Interestingly, EF continuously improved up to 2 years after surgery in the present study. Although group III showed gradual improvements in EF, such outcomes were significantly inferior to those of group I. Furthermore, when we compared groups I and II, there was no statistically significant difference (P = .266). However, group I showed a better trend toward clinical EF improvement. These clinical results showed more patients in group I had a superior response to PDE5-Is compared with group II (1–2 years = 2.3 vs 1.1; Table 2).
PCDU also was performed in group I to evaluate the penile vascular status of patients with tadalafil 5-mg OaD treatment. Although 55% of patients (11 of 20) with arteriogenic ED responded to tadalafil, only 1 patient (14.2%) with venogenic ED responded to treatment. These results suggest that arterial insufficiency is improved by PDE5-Is; however, in patients with venogenic ED, PDE5-Is were ineffective. Thus, if the patient does not respond to PDE-5Is over 1 year, PCDU should be considered to evaluate the vascular status of ED for an optimal treatment. For patients with venogenic ED, treatment modalities other than PDE5-Is alone might need to be considered.
ICIs showed positive results for EF recovery. Non-randomized studies have supported the efficacy of ICIs in the recovery of EF after surgery, even after initial administrations of sildenafil.25, 26, 27 However, when considering this approach, patient compliance and minimizing dropout rates are important.25 Yiou et al28 reported that up to 11% of patients who received ICIs of alprostadil 2.5 μg for ED discontinued treatment because the pain scores negatively affected the IIEF scores at 6-month follow-up. Thus, ICI is insufficient for clinicians to routinely recommend to patients as a treatment modality. However, ICI might be effective in patients who previously tried oral agents but did not respond and who have high compliance.29
Another treatment modality is the use of VEDs for PR after RP. In a preclinical study, VED therapy was very effective for the preservation of endothelial and smooth muscle integrity by increasing arterial flow and supplying oxygen to the corpus cavernosum.30 Raina et al31 found that the early use of VED facilitated early recovery of EF. More recently, Basal et al32 assessed the recovery rates of EF among 4 groups: VEDs, PDE5-Is alone, VEDs and PDE5-Is, or placebo in patients after RARP. In the study, only patients with PDE5-Is alone and those with VEDs and PDE5-Is showed significant improvements. Thus, VED alone or in combination with PDE5-Is might represent a treatment option for PR in patients who have undergone NS-RP. Despite these findings, there is still no clinical evidence for supporting the efficacy of this approach.
There are several limitations of the present study, including the fact that it was a retrospective study with a relatively small sample and no placebo group. Furthermore, there was a selection bias. Apparently, the patients who were included in the tadalafil group usually had sexual partners and had stronger intentions of recovering from ED than patients in the non-tadalafil group. However, despite these limitations, the present study is the first long-term follow-up study that evaluated the efficacy and safety of tadalafil 5-mg OaD treatment in patients with ED after NS-RALP and showed continuous improvements in EF up to 2 years of follow-up. Further larger, multi-institutional prospective studies will help to establish PR by tadalafil 5-mg OaD treatment. This new information could be an important finding for physicians when counseling patients who are undergoing NS-RARP and interested in optimal EF recovery.
Conclusion
In patients with ED after NS-RALP, tadalafil 5-mg OaD treatment was well tolerated and significantly improved EF up to 2 years after surgery compared with treatment in patients in the non-tadalafil group. However, the effect of tadalafil 5-mg OaD treatment on EF recovery in patients with venogenic ED was relatively limited compared with that in the patients with arteriogenic ED in group I.
Statement of authorship
Category 1
-
(a)Conception and Design
- Gyung Tak Sung
-
(b)Acquisition of Data
- Soodong Kim; Gyung Tak Sung
-
(c)Analysis and Interpretation of Data
- Soodong Kim
Category 2
-
(a)Drafting the Article
- Soodong Kim; Gyung Tak Sung
-
(b)Revising It for Intellectual Content
- Soodong Kim; Gyung Tak Sung
Category 3
-
(a)Final Approval of the Completed Article
- Soodong Kim; Gyung Tak Sung
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Funding: None.
References
- 1.Bill-Axelson A., Holmberg L., Garmo H. Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med. 2014;370:932–942. doi: 10.1056/NEJMoa1311593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heidenreich A., Bastian P.J., Bellmunt J. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65:124–137. doi: 10.1016/j.eururo.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 3.Zippe C.D., Pahlajani G. Penile rehabilitation following radical prostatectomy: role of early intervention and chronic therapy. Urol Clin North Am. 2007;34:601–618. doi: 10.1016/j.ucl.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Tal R., Alphs H.H., Krebs P. Erectile function recovery rate after radical prostatectomy: a meta-analysis. J Sex Med. 2009;6:2538–2546. doi: 10.1111/j.1743-6109.2009.01351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alemozaffar M., Regan M.M., Cooperberg M.R. Prediction of erectile function following treatment for prostate cancer. JAMA. 2011;306:1205–1214. doi: 10.1001/jama.2011.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rabbani F., Schiff J., Piecuch M. Time course of recovery of erectile function after radical retropubic prostatectomy: does anyone recover after 2 years? J Sex Med. 2010;7:3984–3990. doi: 10.1111/j.1743-6109.2010.01969.x. [DOI] [PubMed] [Google Scholar]
- 7.User H.M., Hairston J.H., Zelner D.J. Penile weight and cell subtype specific changes in a post-radical prostatectomy model of erectile dysfunction. J Urol. 2003;169:1175–1179. doi: 10.1097/01.ju.0000048974.47461.50. [DOI] [PubMed] [Google Scholar]
- 8.Gratzke C., Strong T.D., Gebska M.A. Activated RhoA/Rho kinase impairs erectile function after cavernous nerve injury in rats. J Urol. 2010;184:2197–2204. doi: 10.1016/j.juro.2010.06.094. [DOI] [PubMed] [Google Scholar]
- 9.Leungwattanakij S., Bivalacqua T.J., Usta M.F. Cavernous neurotomy causes hypoxia and fibrosis in rat corpus cavernosum. J Androl. 2003;24:239–245. doi: 10.1002/j.1939-4640.2003.tb02668.x. [DOI] [PubMed] [Google Scholar]
- 10.Lysiak J.J., Yang S.K., Klausner A.P. Tadalafil increases Akt and extracellular signal-regulated kinase 1/2 activation, and prevents apoptotic cell death in the penis following denervation. J Urol. 2008;179:779–785. doi: 10.1016/j.juro.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 11.Mullerad M., Donohue J.F., Li P.S. Functional sequelae of cavernous nerve injury in the rat: is there model dependency. J Sex Med. 2006;3:77–83. doi: 10.1111/j.1743-6109.2005.00158.x. [DOI] [PubMed] [Google Scholar]
- 12.Chung E., Brock G. Sexual rehabilitation and cancer survivor-ship: a state of art review of current literature and management strategies in male sexual dysfunction among prostate cancer survivors. J Sex Med. 2013;10:102–111. doi: 10.1111/j.1743-6109.2012.03005.x. [DOI] [PubMed] [Google Scholar]
- 13.Salonia A., Burnett A.L., Graefen M. Prevention and management of post-prostatectomy sexual dysfunctions. Part 1: choosing the right patient at the right time for the right surgery. Eur Urol. 2012;62:261–272. doi: 10.1016/j.eururo.2012.04.046. [DOI] [PubMed] [Google Scholar]
- 14.Mulhall J.P., Bella A.J., Briganti A. Erectile function rehabilitation in the radical prostatectomy patient. J Sex Med. 2010;7:1687–1698. doi: 10.1111/j.1743-6109.2010.01804.x. [DOI] [PubMed] [Google Scholar]
- 15.Moreland R.B. Is there a role of hypoxemia in penile fibrosis: a viewpoint presented to the Society for the Study of Impotence. Int J Impot Res. 1998;10:113–120. doi: 10.1038/sj.ijir.3900328. [DOI] [PubMed] [Google Scholar]
- 16.Fode M., Ohl D.A., Ralph D. Penile rehabilitation after radical prostatectomy: what the evidence really says. BJU Int. 2013;112:998–1008. doi: 10.1111/bju.12228. [DOI] [PubMed] [Google Scholar]
- 17.Mulhall J.P. Penile rehabilitation following radical prostatectomy. Curr Opin Urol. 2008;18:613–620. doi: 10.1097/MOU.0b013e3283136462. [DOI] [PubMed] [Google Scholar]
- 18.Montorsi F., Guazzoni G., Strambi L.F. Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injections of alprostadil: results of a prospective, randomized trial. J Urol. 1997;158:1408–1410. [PubMed] [Google Scholar]
- 19.Teloken P., Mesquita G., Montorsi F. Post-radical prostatectomy pharmacological penile rehabilitation: practice patterns among the international society for sexual medicine practitioners. J Sex Med. 2009;6:2032–2038. doi: 10.1111/j.1743-6109.2009.01269.x. [DOI] [PubMed] [Google Scholar]
- 20.Hatzichristou D., Eardley I., Giuliano F. European Association of Urology; Arnhem, Netherlands: 2014. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. [DOI] [PubMed] [Google Scholar]
- 21.Montorsi F., Brock G., Stolzenburg J.U. Effects of tadalafil treatment on erectile function recovery following bilateral nerve-sparing radical prostatectomy: a randomised placebo-controlled study (REACTT) Eur Urol. 2014;65:587–596. doi: 10.1016/j.eururo.2013.09.051. [DOI] [PubMed] [Google Scholar]
- 22.Moncada I., de Bethencourt F.R., Lledó-García E. Effects of tadalafil once daily or on demand versus placebo on time to recovery of erectile function in patients after bilateral nerve-sparing radical prostatectomy. World J Urol. 2015;33:1031–1038. doi: 10.1007/s00345-014-1377-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pavlovich C.P., Levinson A.W., Su L.M. Nightly vs on-demand sildenafil for penile rehabilitation after minimally invasive nerve-sparing radical prostatectomy: results of a randomized double-blind trial with placebo. BJU Int. 2013;112:844–851. doi: 10.1111/bju.12253. [DOI] [PubMed] [Google Scholar]
- 24.Seo Y.E., Kim S.D., Kim T.H. The efficacy and safety of tadalafil 5 mg once daily in the treatment of erectile dysfunction after robot-assisted laparoscopic radical prostatectomy: 1-year follow-up. Korean J Urol. 2014;55:112–119. doi: 10.4111/kju.2014.55.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polito M., d'Anzeo G., Conti A. Erectile rehabilitation with intracavernosal prostadil after radical prostatectomy: refusal and dropout rates. BJU Int. 2012;110:E954–E957. doi: 10.1111/j.1464-410X.2012.11484.x. [DOI] [PubMed] [Google Scholar]
- 26.Mulhall J., Land S., Parker M. The use of an erectogenic pharmacotherapy regimen following radical prostatectomy improves recovery of spontaneous erectile function. J Sex Med. 2005;2:532–540. doi: 10.1111/j.1743-6109.2005.00081_1.x. discussion 540–542. [DOI] [PubMed] [Google Scholar]
- 27.Nandipati K., Raina R., Agarwal A. Early combination therapy: intracavernosal injections and sildenafil following radical prostatectomy increases sexual activity and the return of natural erections. Int J Impot Res. 2006;18:446–451. doi: 10.1038/sj.ijir.3901448. [DOI] [PubMed] [Google Scholar]
- 28.Yiou R., Cunin P., de la Taille A. Sexual rehabilitation and penile pain associated with intracavernosal prostadil after radical prostatectomy. J Sex Med. 2011;8:575–582. doi: 10.1111/j.1743-6109.2010.02002.x. [DOI] [PubMed] [Google Scholar]
- 29.Salonia A., Burnett A.L., Graefen M. Prevention and management of postprostatectomy sexual dysfunctions part 2: recovery and preservation of erectile function, sexual desire, and orgasmic function. Eur Urol. 2012;62:273–286. doi: 10.1016/j.eururo.2012.04.047. [DOI] [PubMed] [Google Scholar]
- 30.Broderick G.A., McGahan J.P., Stone A.R. The hemodynamics of vacuum constriction erections: assessment by color Doppler ultrasound. J Urol. 1992;147:57–61. doi: 10.1016/s0022-5347(17)37132-x. [DOI] [PubMed] [Google Scholar]
- 31.Raina R., Agarwal A., Ausmundson S. Early use of vacuum constriction device following radical prostatectomy facilitates early sexual activity and potentially earlier return of erectile function. Int J Impot Res. 2006;18:77–81. doi: 10.1038/sj.ijir.3901380. [DOI] [PubMed] [Google Scholar]
- 32.Basal S., Wambi C., Acikel C. Optimal strategy for penile rehabilitation after robot-assisted radical prostatectomy based on preoperative erectile function. BJU Int. 2013;111:658–665. doi: 10.1111/j.1464-410X.2012.11487.x. [DOI] [PubMed] [Google Scholar]