Abstract
Introduction
The glans clitoris is covered by a prepuce that normally moves over the glans surface and can be retracted beyond the corona. Clitoral adhesions, ranging from mild to severe, occur when preputial skin adheres to the glans. Physical examination consistent with clitoral adhesions is based on the inability to visualize the entire glans corona. In this closed compartment, the space underneath the adherent prepuce and clitoris can become irritated, erythematous, or infected and can result in sexual dysfunction.
Aim
To determine the prevalence of clitoral adhesions in a sexual medicine practice and assess risk factors associated with clitoral adhesions.
Methods
This research involved retrospective examinations of vulvoscopy photographs taken from August 2007 to December 2015. Clitoral adhesions were considered absent when preputial retraction enabled full glans corona visualization. The study group consisted of women with mild, moderate, or severe clitoral adhesions based on more than 75%, 25% to 75%, or less than 25% glans clitoris exposure without full corona visualization, respectively. 2 independent reviewers evaluated photographs; a 3rd analyzed study group health record data.
Main Outcome Measure
Prevalence of severity of clitoral adhesions.
Results
Of the 1,261 vulvoscopy photographs, 767 (61%) were determined adequate for assessment and 614 photographs represented individual patients. The study group with clitoral adhesions consisted of 140 women (23%) of whom 44%, 34%, and 22% demonstrated mild, moderate, and severe clitoral adhesions, respectively. In the study group, 14% presented with clitorodynia. Risk factors included a history of sexual pain, yeast infection, urinary tract infection, blunt perineal or genital trauma, lichen sclerosus, low calculated free testosterone, and other sexual dysfunctions including persistent genital arousal disorder.
Conclusion
Women with sexual dysfunction should routinely undergo clitoral physical examination. If the glans corona is not fully visualized, then clitoral adhesions should be suspected. Education, counseling, and/or referral for sexual pain management should be considered.
Aerts L, Rubin RS, Randazzo M, et al. Retrospective Study of the Prevalence and Risk Factors of Clitoral Adhesions: Women's Health Providers Should Routinely Examine the Glans Clitoris. Sex Med 2018;6:115–122.
Key Words: Clitoral Adhesion, Glans Clitoris, Vulvoscopy, Corona, Clitorodynia
Introduction
The glans clitoris is covered by the prepuce that normally moves freely over the surface of the glans and can be retracted beyond the glans corona to the balanopreputial sulcus of the clitoris. This sulcus has its specific moistening system consisting of balanopreputial eccrine glands.1 The size, thickness, and configuration of the prepuce vary greatly among individuals.2 The glans clitoris is very sensitive during sexual activity and this sensitivity can be objectively measured.3
We have observed women presenting to our sexual medicine clinic with clitoral adhesions, documented during physical examination by failure to visualize the entire glans corona and recorded by vulvoscopy with photography. Clitoral adhesions present as preputial skin that physically adheres to the glans clitoris at 1 or more points distal to the balanopreputial sulcus, such that the prepuce is no longer freely retractable over the entire surface of the glans during physical examination. There is a spectrum of clitoral adhesions, ranging from mild to severe, but in all cases of adhesions, there is a closed compartment covering some portion of the glans corona.
The closed compartment space under the clitoral adhesions can prevent adequate drainage of keratinaceous desquamation. Smegma and squamous cells can accumulate underneath the prepuce resulting in smegmatic pseudocysts and/or keratin pearls, in which squamous cells actually form concentric layers and result in several millimeter-sized masses. Thus, the closed compartment between the prepuce and the clitoris can become irritated, erythematous, or infected.4 Any of these changes can be associated with a persistent foreign body sensation (described as similar to grains of sand in the eye), balanitis, discomfort, hypersensitivity, clitorodynia sexual pain disorder, and even persistent genital arousal disorder (PGAD). The exact cause of the clitoral adhesion in a specific patient usually cannot be identified.5, 6
In our sexual medicine clinic, it is expected that patients with sexual health complaints will undergo a detailed genital physical examination including a detailed and systematic examination of the vulva using vulvoscopy magnification and photography.7 Thus, we appeared to be in a unique clinical environment to expand the limited clinical data that exist on the prevalence and risk factors of the specific clitoral pathology of clitoral adhesions. In particular, we wished to know answers to the following questions: What is the prevalence of adhesions of the adjacent prepuce to the glans clitoris in a clinical population? In women with clitoral adhesions, what is the likelihood of clitoral adhesions causing clitoral pain or clitorodynia? What are the risk factors for clitoral adhesions? It was the goal of this retrospective clinical research study to address these questions.
Methods
This retrospective research study was approved by the institutional review board. For women who present for assessment of their female sexual dysfunction, it is routine in our multidisciplinary sexual medicine practice to obtain consent to perform a detailed sexual history and administer a battery of patient questionnaires, including the Female Sexual Function Index (FSFI), the Sexual Distress Scale–Revised, the Perceived Stress Scale, the Personal Health Questionnaire, the McGill Genital Pain Questionnaire, and the Vulvar Pain Questionnaire (V-Q). In addition, blood tests are performed, including total testosterone, sex hormone binding globulin, estradiol, and calculated free testosterone.
It also is routine in our practice to perform a standardized optically magnified vulvoscopy examination with photography. We use Wallach ZoomScope vulvoscopy (Wallach Surgical Devices, Trumbull, CT, USA) with an attached foot-pedal–controlled Cannon EOS XSi Digital SLR camera (Canon, Shimomaruko Ota-Ku, Japan), which links to a light-emitting diode monitor so the patient and her partner can observe the vulvoscopy findings in real time.7 At the end of each day, the images are transferred to a file in an encrypted computer in our office. The only photo identification is the date and time the photos were taken.
During the vulvoscopy examination, a standard operating procedure is followed. Physical examination is performed of the (i) skin overlying the right and left labia majora, right and left labia minora, and the sulcus between the 2 labia; (ii) the glans clitoris and prepuce; (iii) the urethral meatus; (iv) the vestibule between the Hart line and hymen, especially the vestibular glands at the 1:00 and 11:00 o'clock positions; and (v) the vagina, especially the anterior vaginal wall and cervix, and assessment for the presence or absence of vaginal rugae. During vulvoscopy, the clitoral glans is specifically assessed using gentle bilateral cephalad preputial retraction. The clitoris and preputial region are examined for the (i) size of the glans clitoris compared with the cotton swab, (ii) presence or absence of the corona of the glans, (iii) presence of clitoral adhesions with underlying keratin pearls and/or smegma, and (iv) presence of clitoral pain, hypersensitivity, or discomfort.
The primary goal of this study was to determine the prevalence of glans clitoral adhesions in a single sexual medicine practice. To achieve this, we examined our large collection of vulvoscopy photos, taken over an 8-year 6-month period from August 2007 to December 2015. The criteria for inclusion of each vulvoscopy photograph were (i) good photographic focus of the glans clitoris and (ii) the presence of appropriate manual cephalad preputial retraction that allowed for full visualization of the glans corona.
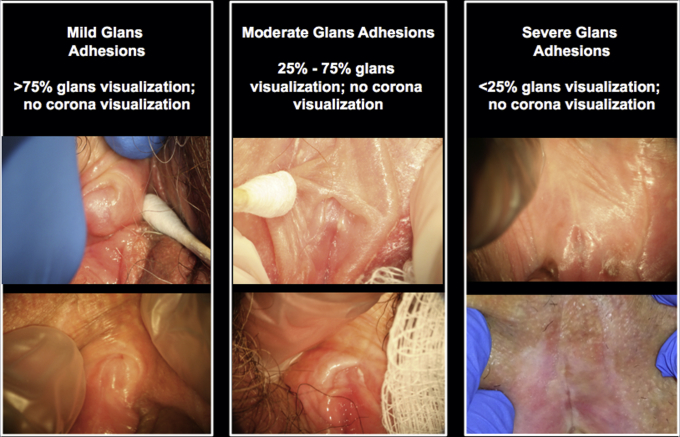
Clitoral adhesions were recorded as absent when the prepuce could be retracted to the balanopreputial sulcus and the full corona was visualized (Figure 1). In contrast, when the vulvoscopy photograph showed an inability to fully expose the glans clitoris, the woman was identified as having clitoral adhesions and thereby entered into the study group. The following classification was used to estimate the degree of clitoral adhesion: (i) mild clitoral adhesions were defined as more than 75% of the surface of the glans clitoris exposed and the corona was not visualized; (ii) moderate clitoral adhesions were defined as 25% to 75% of the surface of the glans clitoris exposed and the corona was not visualized; and (iii) severe clitoral adhesions were defined as less than 25% of the surface of the glans clitoris exposed and the corona was not visualized (Figure 2).
Figure 1.
Absent clitoral glans adhesions when the prepuce was retracted to the balanopreputial sulcus and the full corona was visualized.
Figure 2.
Mild, moderate, and severe clitoral adhesion.
2 independent reviewers, at different times, evaluated the vulvoscopy photographs: one was a gynecologist (L.A.) and the other was a sexual medicine fellow (R.R.). For any discrepancy between the 2 reviewers for the absence or degree of clitoral adhesions, the photograph was re-evaluated until a consensus was reached.
The secondary objective of this retrospective study was to assess the risk factors associated with clitoral adhesions by examining the clinical data of the study group. We further subdivided the study group by menopausal status and by degree of clitoral adhesion severity. To achieve this goal, a 3rd independent reviewer (M.R.) who had not seen the vulvoscopy photographs analyzed the health record data of the study group (Tables 1 and 2).
Table 1.
Results of validated instruments, history, and physical findings analyzed by severity of clitoral of adhesions
| Degree of phimosis |
|||
|---|---|---|---|
| Mild (n = 62) | Moderate (n = 48) | Severe (n = 30) | |
| Age (y), median | 46.5 | 46 | 39.5 |
| Duration of sexual dysfunction (y), median | 7 | 5 | 5 |
| FSFI scores, median | 15.7 | 15.4 | 14.8 |
| Desire | 2.4 | 2.4 | 2.4 |
| Arousal | 2.55 | 2.55 | 2.7 |
| Lubrication | 1.65 | 3 | 2.1 |
| Orgasm | 2.8 | 2 | 2 |
| Pain | 1.2 | 1.4 | 1.2 |
| Satisfaction | 2 | 2.6 | 2.8 |
| SDS-R score, median | 32 | 32.5 | 26 |
| PSS score, median | 20 | 23 | 20 |
| PHQ scores, median | 7 | 6.5 | 4 |
| Sensory | 9 | 5 | 6 |
| Affective | 2 | 2.5 | 0 |
| PPI score, median | 3 | 3 | 2 |
| V-Q score, median | 9 | 4.5 | 6 |
| Total T, median | 28 | 22.6 | 20 |
| SHBG, median | 76.6 | 77 | 83 |
| Calculated free T, median | 0.2855 | 0.238 | 0.22 |
| Clitoral pain, n (%) | 7 (11.3) | 5 (10.4) | 8 (27) |
| PGAD, n (%) | 6 (9.7) | 3 (6.3) | 2 (6.7) |
| Yeast infection Hx, n (%) | 38 (61.3) | 38 (79.2) | 21 (70) |
| UTI Hx, n (%) | 35 (56.5) | 30 (62.5) | 13 (43.3) |
| Perineal trauma Hx, n (%) | 15 (24.2) | 11 (22.9) | 5 (16.7) |
| Lichen sclerosus Hx, n (%) | 3 (4.8) | 2 (4.2) | 3 (10) |
| Lysis of adhesions, n (%) | 4 (6.5) | 1 (2.1) | 1 (3.3) |
FSFI = Female Sexual Function Index; Hx = history; PGAD = persistent genital arousal disorder; PHQ = Personal Health Questionnaire; PPI = Present Pain Intensity; PSS = Perceived Stress Scale; SDS-R = Sexual Distress Scale–Revised; SHBG = sex hormone binding globulin; T = testosterone; UTI = urinary tract infection; V-Q = Vulvar Pain Questionnaire.
Table 2.
Results of validated instruments, history, and physical findings analyzed by menopausal status
| All patients (N = 140) | Premenopausal (n = 70) | Menopausal (n = 70) | |
|---|---|---|---|
| Age (range = 18–77 y), median | 45 | 31 | 58 |
| Duration of sexual dysfunction (y), median | 6 | 6 | 6 |
| FSFI scores, median | 15.4 | 15.2 | 15.8 |
| Desire | 2.4 | 2.4 | 2.4 |
| Arousal | 2.7 | 2.4 | 3 |
| Lubrication | 2.4 | 2.4 | 2.3 |
| Orgasm | 2.4 | 1.6 | 3.2 |
| Pain | 1.2 | 1.2 | 1.6 |
| Satisfaction | 2.4 | 2.2 | 2.8 |
| SDS-R score, median | 31 | 35 | 25 |
| PSS score, median | 21 | 22 | 21 |
| PHQ scores, median | 6 | 7 | 5 |
| Sensory | 7 | 11 | 3 |
| Affective | 2 | 3.5 | 0 |
| PPI score, median | 3 | 3 | 2 |
| V-Q score, median | 6.5 | 8.5 | 3 |
| Total T, median | 23 | 23 | 22.1 |
| SHBG, median | 78 | 85 | 77 |
| Calculated free T, median | 0.245 | 0.240 | 0.249 |
| Clitoral pain, n (%) | 20 (14.3) | 13 (18.6) | 7 (10) |
| PGAD, n (%) | 11 (7.9) | 4 (5.7) | 7 (10) |
| Yeast infection Hx, n (%) | 99 (70.7) | 49 (70.0) | 50 (71.4) |
| UTI Hx, n (%) | 79 (56.4) | 40 (57.1) | 39 (55.7) |
| Perineal trauma Hx, n (%) | 33 (23.6) | 22 (31.4) | 11 (15.7) |
| Lichen sclerosus Hx, n (%) | 8 (5.7) | 5 (7.1) | 3 (4.3) |
| Lysis of adhesions, n (%) | 6 (4.3) | 3 (4.3) | 3 (4.3) |
FSFI = Female Sexual Function Index; Hx = history; PGAD = persistent genital arousal disorder; PHQ = Personal Health Questionnaire; PPI = Present Pain Intensity; PSS = Perceived Stress Scale; SDS-R = Sexual Distress Scale–Revised; SHBG = sex hormone binding globulin; T = testosterone; UTI = urinary tract infection; V-Q = Vulvar Pain Questionnaire.
Results
Figure 3 shows a flowchart that summarizes the process of the vulvoscopy photographic examination used in this retrospective clinical study. 1,261 vulvoscopy photographs were examined over an 8-year 6-month period from August 2007 to December 2015. Given the criteria for inclusion of good optical focus and adequate preputial retraction, 767 photographs of the glans clitoris were determined adequate for assessment, whereas 494 photos were not. Of the 767 adequate photographs, 614 represented individual patients and 153 represented follow-up studies. 140 (23%) of the 614 individual patients demonstrated clitoral adhesions and formed the study group. Of these 140 photographs, 44% (62 of 140) were considered mild, 34% (48 of 140) were considered moderate, and 22% (30 of 140) were considered severe clitoral adhesions (Figure 3).
Figure 3.
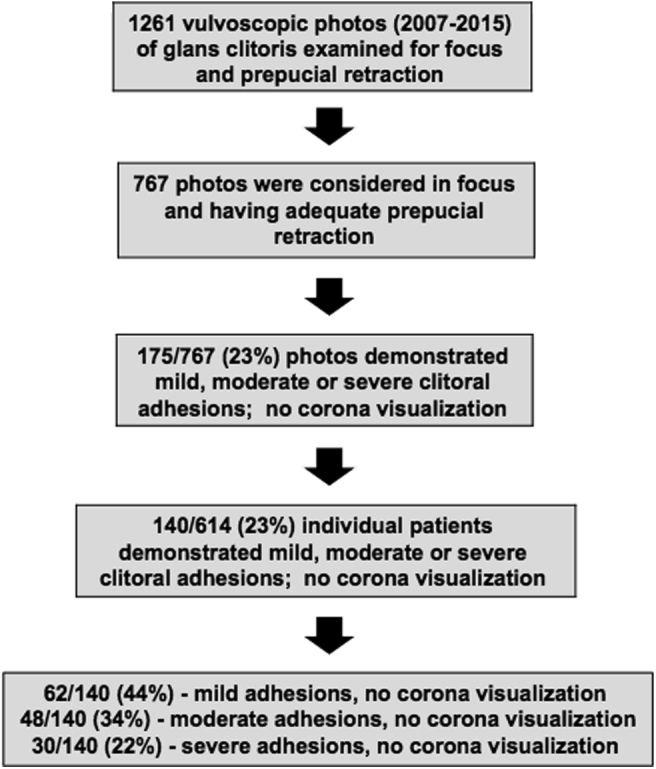
Determination of study population.
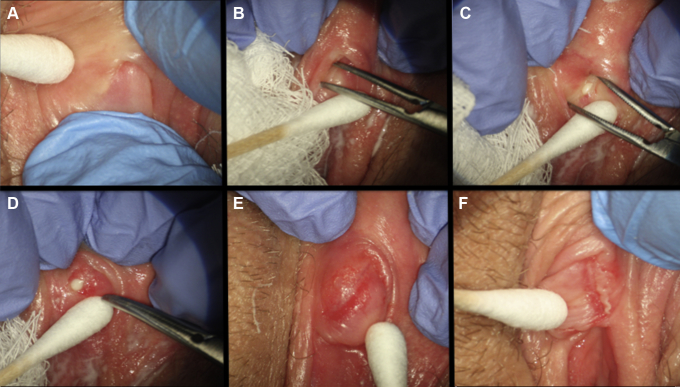
20 women (14%) in the study group actually presented to the sexual medicine clinic with specific clitoral pain or clitorodynia. Of those with clitorodynia, 6 (4%) underwent a surgical procedure for lysis of clitoral adhesions (Figure 4).
Figure 4.
In-office lysis of clitoral adhesions. Panel A shows skin adhesions. Panel B shows lysis with fine Jacobsen mosquito forceps after topical application of anesthetics. Panels C and D show keratin pearls. Panels E and F show visualization of corona.
The 140 women composing the study group had the following characteristics. They reported sexual dysfunction for a median of 6 years before presentation (median FSFI score = 15.35 of 36). Of the 6 domains of the FSFI, the lowest score was for sexual pain (median score = 1.2 of 6). A low score on the FSFI is consistent with more sexual pain complaints. Sexual pain on the FSFI was calculated from the following 3 questions: (i) Over the past 4 weeks, how often did you experience discomfort or pain during vaginal penetration? (ii) Over the past 4 weeks, how often did you experience discomfort or pain after vaginal penetration? (iii) Over the past 4 weeks, how would you rate your level (degree) of discomfort or pain during or after vaginal penetration? Of the remaining sexual function domains, the median scores were equally low for desire (2.4 of 6), arousal (2.7 of 6), lubrication (2.4 of 6), orgasm (2.4 of 6), and intercourse satisfaction (2.4 of 6).
The Sexual Distress Scale–Revised score was quite high (median score = 31 of 52).
Sexual pain also was assessed in the study group using the McGill Genital Pain Score in which a higher score is associated with more pain. The study group had a median sensory score of 7 of 45 and a median overall intensity of pain score of 3 of 5, considered distressing pain.
Sexual pain was further assessed in the study group using the V-Q, in which a higher score is associated with more pain. The study group had a median V-Q score of 6.5 of 33.
The medical history characteristics of the 140 women of the study group were as follows. The median age was 45 years (range = 18–77 years). The most common associations identified, in order of prevalence, were a history of yeast infection in 99 (71%), urinary tract infection in 79 (56%), trauma to the perineum, including habitual bicycle or horseback riding in 33 (24%), and lichen sclerosus in 8 (6%). The median scores for total testosterone, sex hormone binding globulin, and calculated free testosterone were 23 ng/dL, 78 nmol/L, and 0.245 ng/dL, respectively. The calculated free testosterone values are consistent with lower than ideal values of 0.6 to 0.8 ng/dL.
The study group was further subdivided by severity of clitoral adhesions: mild (n = 62, 44%; median age = 46.5 years), moderate (n = 48, 34%; median age = 46 years), and severe (n = 30, 22%; median age = 39.4 years). Concerning FSFI domain scores, the score for sexual pain was lowest compared with the remaining 5 FSFI domains in all 3 subgroups of clitoral adhesions. Of note, in the sexual pain assessment using the V-Q, in which a higher score is associated with more pain, the highest median sexual pain score was noted in the subgroup with mild clitoral adhesions. The mild subgroup had a median V-Q score of 9 of 33 compared with median V-Q scores of 4.5 and 6 of 33, respectively, for the moderate and severe clitoral adhesion subgroups. There were no differences in the 3 subgroups of clitoral adhesions for calculated free testosterone values (Table 1).
The study group was subsequently subdivided into premenopausal (n = 70, 50%; median age = 31 years) and menopausal (n = 70, 50%; median age = 58 years). The median FSFI domain score for pain was lower in the premenopausal subgroup (1.2 of 6) compared with the menopausal subgroup (1.6 of 6). The median FSFI domain score for orgasm was much lower in the premenopausal subgroup (1.6 of 6) compared with the menopausal subgroup (3.2 of 6). The median FSFI domain score for arousal was lower in the premenopausal subgroup (2.4 of 6) compared with the menopausal subgroup (3 of 6). There were no differences between the premenopausal and menopausal subgroups for calculated free testosterone values (Table 2).
Discussion
The objectives of this study were 3-fold. By retrospectively evaluating vulvoscopy photographic data of women visiting a multidisciplinary sexual medicine facility during the previous 8.5 years, we could (i) study the prevalence of adhesions of the adjacent skin to the glans clitoris; (ii) study the likelihood of these adhesions causing clitorodynia; and (iii) assess the risk factors associated with clitoral adhesions.
Our study showed that the prevalence of clitoral adhesions in our select sexual dysfunctional population is slightly higher than 1 of 5 women, with more than half showing moderate to severe adhesions. We defined clitoral adhesions as an abnormal physical finding, in which preputial skin physically adheres to the glans clitoris at 1 or more points distal to the balanopreputial sulcus, such that the prepuce is no longer freely retractable over the entire surface of the glans during physical examination. This creates a closed compartment covering some portion of the glans corona.
We reviewed the literature and found 2 studies that looked at the prevalence of the abnormal physical finding of clitoral adhesions. One study in 2002 looked at a similar sexual dysfunction population8; however, vulvoscopy photographic documentation was not performed in that study. The conclusion of that study was that the prevalence rate of clitoral adhesions and phimosis was 22%.8 The other study looked at a group of 589 college-age students seen in a student health clinic. They found the rate of clitoral adhesions to be 33%. Of those with adhesions, 58% were considered mild.9 We conclude that the abnormal physical finding of clitoral adhesions in a sexually dysfunctional population is sufficiently common to warrant routine clitoral examination in all women with sexual dysfunction.
This study further showed that 80% of women with clitoral adhesions did not present to the sexual medicine clinic specifically for complaints of clitoral pain. In assessing the characteristics of our study group, we used 3 validated measures of sexual pain, the FSFI, the McGill Genital Pain Questionnaire, and the V-Q. In all these measures, we observed that for our study group sexual pain was the most substantial area of sexual dysfunction compared with the other sexual domains, including desire, arousal, lubrication, orgasm, and intercourse satisfaction. The sexual pain in our study group was considered distressing on the McGill Genital Pain Questionnaire, and the V-Q score indicated significant sexual pain. How can this discrepancy of a few women presenting to the sexual medicine clinic with complaints of sexual pain but scores on validated instruments showing substantial sexual pain be explained?
One theory is that clitoral pain is greatly underdiagnosed and seriously undertreated. Gordon5 called clitoral pain the “great unexplored pain” in women. In our practice we have seen numerous patients who accept their symptoms of clitoral hypersensitivity, clitoral discomfort, and even clitoral pain precluding their ability to wear tight clothing, who do not self-examine their clitoris or seek assessment from a health care provider. Some women presenting with clitoral pathology who sought medical diagnosis and treatment were told by at least 1 previous health care provider that “we do not examine the clitoris” or “we do not see anything abnormal on physical examination” although there was obvious clitoral phimosis with underlying balanitis tenderness on vulvoscopy examination in our office. Pukall10 noted that clitoral pain can be a presenting sign of vestibulodynia.
Based on our data (Tables 1 and 2), we postulate there are risk factors that can increase the prevalence of clitoral adhesions by changing the glans clitoral and preputial skin health. Factors found in this study that appear to be implicated in the formation of clitoral adhesions include blunt perineal or genital trauma, genital fungal or bacterial infections, genital dermatologic conditions such as lichen sclerosus, and insufficient sex steroid hormones. Future research will need to determine whether these risk factors are causally related.
Concerning the recent increase in basic science and clinical publications concerning clitoral physiology, these publications appear to relate to a diversity of topics including clitoral anatomy, neurophysiology, endocrinology, smooth muscle, and vascular physiology. When using the key word clitoris in PubMed for the 40-year period from 1961 to 2000, the average number of articles was only 25 ± 11 per year. However, this number has dramatically increased to 73 ± 8 per year in PubMed when using the key word clitoris for the 5-year period from 2012 through 2016.
There appears to be a discrepancy between the increasing scientific interest concerning clitoral physiology and pathophysiology and limited educational opportunities for provider training on how to perform a physical examination of the clitoris. For example, urology residency programs universally teach physical examination of the male homologue (the penis) but do not regularly teach how to examine the clitoris. Disorders of the homologue glans and prepuce fall within the purview of urology, but clinical management of parallel pathologies in women generally does not. In gynecology training programs and clinical practice, physical examination of the clitoris is uncommon and not routinely taught.
This could explain in part why there is so much patient acceptance of distressing clitoral pain and why health care providers in general neither know how to examine nor feel comfortable examining the clitoris. This would explain the paucity of clinical data on the prevalence of the various recognized clitoral pathologies, including clitoral adhesions, and how clitoral adhesions can relate to female sexual dysfunctions.
Chronic sexual pain problems involving the female reproductive system, such as clitorodynia, are major health concerns in women of all ages adversely affecting women's psychosocial well-being and disrupting all aspects of sexual function.5, 6 Despite significant advances, sexual pain, especially clitorodynia, is still poorly understood. The causes of clitorodynia are, in general, considered multifactorial, involving psychosexual and biomedical factors.5, 6 In some women with clitorodynia, a localized type of vulvodynia, the skin adhesions to the glans clitoris can give rise to a closed compartment syndrome with accumulation of skin secretions and initiation of a glans balanitis, leading to chronic vulvar pain. A potential treatment of this condition is the minimally invasive, typically office-based surgical lysis of the adhesions with a fine Jacobsen mosquito forceps and removal of the particulate skin secretions, such as keratin pearls (Figure 4). In some cases, in which the adhesions are recurrent, a more invasive solution could involve a dorsal slit surgical procedure.11
In addition, this study showed that there were several risk factors associated with clitoral adhesions. Our study identified a history of sexual pain, yeast infection, urinary tract infection, blunt perineal or genital trauma, lichen sclerosus, and low calculated free testosterone as relevant risk factors. Of note, the 2002 prevalence study suggested that the pathophysiology of clitoral adhesions and phimosis was likely skin health concerns that caused secondary changes to preputial elasticity.8
This study supports that conclusion. Dermatologic health of the glans clitoris and the prepuce can be adversely affected by such factors as lichen sclerosus, recurrent yeast infections, and blunt trauma. The function of the balanopreputial eccrine glands of the prepuce can be adversely affected by a low testosterone state. Low calculated free testosterone states are associated with hormonal-based contraceptives.12 Recurrent urinary tract infections can be manifestations of a more broad urogenital atrophy, including atrophy of the genital glans and preputial skin, especially associated with menopausal estrogen deficiency or hormonally related contraception.13 An unusual explanation could be the use of panty liners used to absorb light menstrual flow, vaginal discharge, or urine leakage or to maintain a clean, dry feeling. Panty liners can trap heat and moisture to promote vulvovaginal candidiasis or promote colonization by microbes that contribute to urinary tract infections and changes in local genital skin health, although more research is needed.
Our study further showed that other bothersome sexual dysfunctions can be associated with clitoral adhesions, in particular PGAD, which is characterized by persistent or recurrent, unwanted or intrusive, distressing feelings of genital arousal or being on the verge of orgasm (genital dysesthesia), not associated with concomitant sexual interest, thoughts, or fantasies for a minimum of 6 months.14 Clinical conditions observed in women with PGAD can include peripheral genital pathologies such as clitorodynia from clitoral adhesions, with an underlying balanitis related to the closed compartment syndrome.15 Some women with PGAD and clitoral adhesions might respond favorably to local clitoral treatment.
There are limitations to this single-center retrospective study. The study population is biased and consists exclusively of women visiting a sexual medicine practice. The ideal study group would be women in the general population, although it would be unclear how to motivate such a broad population to allow vulvoscopy photographic examinations. Ideally a control comparison group also would be studied. Another limitation is the isolated interpretation that the distressing sexual pain experienced by women in the study group was related to their clitoral adhesion. The women could have had other types of sexual pain such as hormonally mediated vestibulodynia or genitourinary syndrome of menopause. A prospective study would allow for more clarity regarding the real basis of their sexual pain.
In summary, this study showed that vulvoscopy photographs of more than 1 in 5 women showed clitoral adhesions on a standardized method of optically magnified vulvoscopy examination with photography. The diagnosis of clitoral adhesions is based on an inability to visualize the corona on physical examination in the presence of cephalad preputial retraction. The benefits of magnification cannot be overstated because the anatomy becomes significantly clearer than with the naked eye alone. This information is medically relevant to the patient and the health care provider. Education and counseling should be provided concerning the pathophysiology of clitoral adhesions occurring secondary to conditions that adversely interfere with the health of the skin of the glans and the prepuce. Understanding the management of these risks factors can affect the clitoral adhesion condition, but more research is needed. Follow-up optically magnified vulvoscopy examinations with photography to compare baseline with follow-up data are recommended to assess for disease progression.
We recommend that clitoral physical examination be taught in medical schools and in urology and gynecology residency programs. Attention should be given to bothersome and distressing clitoral pathologic conditions such as clitoral adhesions.
Statement of authorship
Category 1
-
(a)Conception and Design
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
-
(b)Acquisition of Data
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
-
(c)Analysis and Interpretation of Data
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
Category 2
-
(a)Drafting the Article
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
-
(b)Revising It for Intellectual Content
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
Category 3
-
(a)Final Approval of the Completed Article
- Leen Aerts; Rachel S. Rubin; Michael Randazzo; Sue W. Goldstein; Irwin Goldstein
Footnotes
Conflicts of Interest: None.
Funding: None.
References
- 1.Cold C.J., Taylor J.R. The prepuce. BJU Int. 1999;83(Suppl 1):34–44. doi: 10.1046/j.1464-410x.1999.0830s1034.x. [DOI] [PubMed] [Google Scholar]
- 2.Sherfey M.J. The evolution and nature of female sexuality in relation to psychoanalytic theory. J Am Psychoanal Assoc. 1966;14:28–128. doi: 10.1177/000306516601400103. [DOI] [PubMed] [Google Scholar]
- 3.Burke Y.Z., Lowenstein L. Value of quantitative sensory testing in the evaluation of genital sensation: its application to female sexual dysfunction. Sex Med Rev. 2016;4:121–125. doi: 10.1016/j.sxmr.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Wabrek A.J., Wabrek C.J. Dyspareunia. J Sex Marital Ther. 1975;1:234–241. doi: 10.1080/00926237508405293. [DOI] [PubMed] [Google Scholar]
- 5.Parada M., D'Amours T., Amsel R. Clitorodynia: a descriptive study of clitoral pain. J Sex Med. 2015;12:1772–1780. doi: 10.1111/jsm.12934. [DOI] [PubMed] [Google Scholar]
- 6.Gordon A.S. Clitoral pain: the great unexplored pain in women. J Sex Marital Ther. 2002;28:S123–S128. doi: 10.1080/00926230252851249. [DOI] [PubMed] [Google Scholar]
- 7.Kottmel A., Goldstein I. Vulvoscopy. J Sex Med. 2012;9:2990–2993. [Google Scholar]
- 8.Munarriz R., Talakoub L., Kuohung W. The prevalence of phimosis of the clitoris in women presenting to the sexual dysfunction clinic: lack of correlation to disorders of desire, arousal and orgasm. J Sex Marital Ther. 2002;28:S181–S185. doi: 10.1080/00926230252851302. [DOI] [PubMed] [Google Scholar]
- 9.Wiesmeier E., Masongsong E.V., Wiley D.J. The prevalence of examiner-diagnosed clitoral hood adhesions in a population of college-aged women. J Lower Genit Tract Dis. 2008;12:307–310. doi: 10.1097/LGT.0b013e31817f36e8. [DOI] [PubMed] [Google Scholar]
- 10.Pukall C.F. Primary and secondary provoked vestibulodynia: a review of overlapping and distinct factors. Sex Med Rev. 2016;4:36–44. doi: 10.1016/j.sxmr.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 11.Goldstein A.T., Burrows L.J. Surgical treatment of clitoral phimosis caused by lichen sclerosus. Am J Obstet Gynecol. 2007;196:126.e1–126.e4. doi: 10.1016/j.ajog.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Burrows L.J., Goldstein A.T. The treatment of vestibulodynia with topical estradiol and testosterone. Sex Med. 2013;1:30–33. doi: 10.1002/sm2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu K.K., Boyko E.J., Scholes D. Risk factors for urinary tract infections in postmenopausal women. Arch Intern Med. 2004;164:989–993. doi: 10.1001/archinte.164.9.989. [DOI] [PubMed] [Google Scholar]
- 14.Parish S.J., Goldstein A.T., Goldstein S.W. Toward a more evidence-based nosology and nomenclature for female sexual dysfunctions—part II. J Sex Med. 2016;13:1888–1906. doi: 10.1016/j.jsxm.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 15.Jackowich R.A., Pink L., Gordon A. Persistent genital arousal disorder: a review of its conceptualizations, potential origins, impact, and treatment. Sex Med Rev. 2016;4:329–342. doi: 10.1016/j.sxmr.2016.06.003. [DOI] [PubMed] [Google Scholar]