Abstract
Background and objective
Although depression is considered one of the comorbidities of COPD, the clinical characteristics of depression in patients with early COPD remain unknown. We aimed to use national-level data to identify the clinical features and risk factors of depression in patients with early COPD.
Methods
We examined 7,550 subjects who were registered in the Korean National Health and Nutrition Examination Survey database of 2014 because that was the only year in which the Patient Health Questionnaire-9 for depression status was administered. Spirometry was used to identify patients with COPD whose forced expiratory volume in 1 second was 50% or more, and these patients were included in the analysis.
Results
Of the 211 subjects with early COPD, 14.2% also had depression, whereas 85.8% did not. The patients with depression were predominantly living alone and had a greater prevalence of diabetes compared with the patients without depression. The overall quality of life of the subjects with depression was lower than that of those without depression, and only the quality of life index correlated significantly with depression severity. In the multivariate regression analysis, female sex (adjusted OR, 1.79; 95% CI, 1.38–2.31; p<0.01), living alone (adjusted OR, 1.86; 95% CI, 1.37–2.51; p<0.01), and low income (adjusted OR, 2.17; 95% CI, 1.55–3.04; p<0.01) were identified as significant risk factors for depression.
Conclusion
In patients with early COPD, depression was associated with a low quality of life, and female sex, living alone and low income were significant risk factors for depression.
Keywords: early COPD, depression, Patient Health Questionnaire-9, risk factors
Introduction
COPD is a progressive small airway disease that is characterized by chronic respiratory symptoms, such as cough, sputum, and dyspnea. Even though COPD is considered a progressive debilitating disease by itself, several well-known comorbid conditions make patients with COPD difficult to manage.1 Over 50% of patients with COPD have 1–2 comorbid conditions, 15.8% have 3–4, and 6.8% have more than 5.2 Guidelines describe several comorbidities, including hypertension, cardiovascular disease, diabetes mellitus (DM), osteoporosis, and lung cancer.1 Although the mechanisms underlying the association of comorbidities with COPD are not clear, several possible mechanisms, including smoking-related respiratory and systemic inflammation, alveolar microangiopathy, and vascular stiffness, might play a role in the pathogenesis of both the COPD and the comorbidities.3–5
Psychiatric conditions, such as depression and anxiety, are also comorbidities of COPD.1 Comorbid depression in patients with COPD is related to low quality of life (QoL),6,7 high health care resource utilization,8 more frequent exacerbation,9,10 and increased mortality.11 Early identification of these psychiatric conditions and psychological interventions in patients with COPD might improve the depression symptoms and clinical outcomes.12 These observations are mainly evident in patients with symptomatic and overt COPD. Information is lacking on patients with less symptomatic and less severe COPD.
In the present study, we aimed to identify the prevalence, risk factors, and clinical features of depression experienced by patients with early COPD.
Methods
Source of data
The Korean National Health and Nutrition Examination Survey (KNHANES) is a nationwide representative study that is conducted annually to assess the health and nutritional status of people in Korea. Trained interviewers administer questionnaires on diverse health-related data, and subjects self-report their health-related habits, including smoking. Because the KNHANES uses a complex, multistaged probability sample design, the results represent the total noninstitutionalized population of Korea.13,14 We used data from the 2014 KNHANES because that was the only year that the Patient Health questionnaire (PHQ)-9 for assessing depression status was administered.
This study was exempted from the informed consent requirement by the Institutional Review Board Committee of KyungHee University Hospital because of its retrospective nature and widely available public data (IRB No KHUH 2017-11-015). All KNHANES data used in this study were anonymous and did not contain any personally identifiable information.
Definition of early COPD
Subjects over 40 years of age underwent spirometry in the KNHANES design, and COPD was defined as a spirometry-confirmed airflow limitation (forced expiratory volume in 1 second [FEV1]/forced vital capacity [FVC] <0.70). A definition of early COPD has not yet been established. Thus, we used the following inclusion criteria for the patients with early COPD based on the result of a study of the natural course of early COPD in Korean patients:15 1) age ≥40 years, 2) FEV1/FVC <0.70, and 3) FEV1 ≥50%. In order to clarify COPD, only patients with 10 pack-years or more smoking history were included, and patients who were diagnosed with asthma from clinician were excluded.
PHQ-9 for assessing depression
The PHQ-9, which is based on the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), assesses the patients for feelings of no pleasure, depression, sleep changes, fatigue, changes in appetite, guilt feelings, no sense of worth, loss of concentration, feelings of being stuck, and suicidal ideation over the previous 2 weeks. Each item is scored from 0 (not at all) to 3 (almost daily), with a score of 27 overall, which reflects more severe depression.16,17 PHQ-9 is used to not only screening but also for diagnosing depressive disorder because all DSM-IV criteria of a depressive episode are included.18 A PHQ-9 scores of 5 or more indicates depression,17 and a PHQ-9 score of ≥10 has been found to have 91% sensitivity and 89% specificity for a diagnosis of major depression in stroke patients.19 The PHQ-9 was validated in both a medical setting and in a general population.16,20,21 Furthermore, we used Korean version of PHQ-9 depression scale, which also has been validated.22 We defined the PHQ score of ≥5 as depression in this study.
Clinical measurements
The KNHANES provides researchers information on various demographic factors, including age, sex, body mass index (BMI), level of education, self-perceived degree of income, spirometry results, and disease status for patients either previously diagnosed or currently under treatment. EuroQol-5 dimensions questionnaire (EQ-5D), a simple health-related QoL instrument consisting of 5 health dimension (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), was used to measure QoL status.23 For each dimension, subjects are asked to mark between 1: “no problem” to 5: “unable to/extreme problems,” and these responses are combined to produce a 5-digit number and consequently converted to EQ-5D index score from full health status 1 to death 0. The EQ-5D is a valid instrument for measuring self-perceived health-related QoL status in both general and COPD patients.24 The Korean version of the EQ-5D scale was used in the KNHANES.25
Statistical analysis
The differences between patient groups (COPD vs non-COPD, with depression vs without depression) were assessed using χ2 tests for categorical variables, with the results expressed as numbers and percentages, and Student’s t-tests for continuous variables, with the results presented as mean and SD. The KNHANES provides population weights. When comorbid conditions were compared between subjects with COPD and those without COPD, survey analyses weighted for spirometry were examined and expressed as percentages to result in estimates that were representative of the noninstitutionalized population. Spearman rank correlation analyses were performed to identify correlations between the PHQ scores and other factors, such as BMI and FEV1. Then, to identify factors that were related to depression in the subjects with early COPD, stepwise logistic regression analyses were conducted. Only factors with P-value <0.1 in the univariate analysis were used in the multivariate analysis.
P-values <0.05 were considered significant. All analyses were conducted using Stata (version 14.2; StataCorp LC, College Station, TX, USA).
Results
Subject characteristics
Among the 2,885 subjects over 40 years of age who underwent spirometry, 211 were patients with early COPD who had PHQ-9 questionnaire results available (Figure 1).
Figure 1.
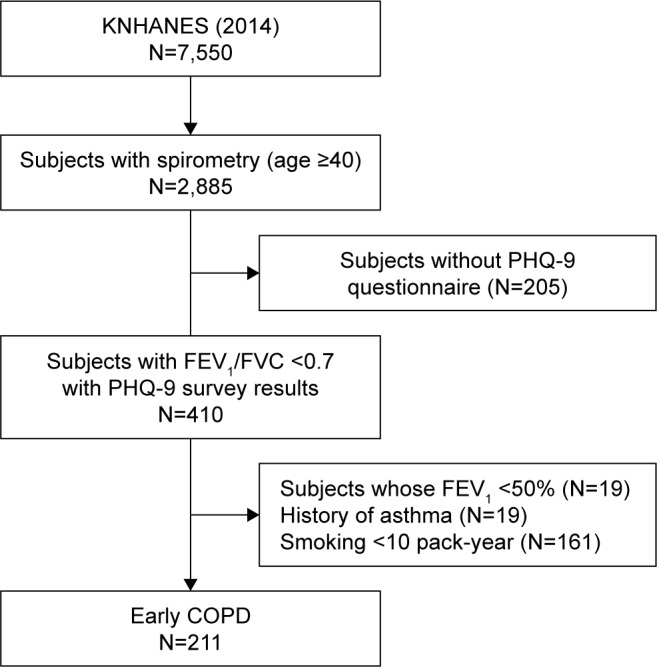
Flow diagram of the study participants.
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; KNHANES, Korean National Health and Nutritional Examination Survey; PHQ-9, Patient Health Questionnaire-9.
Compared with non-COPD patients (n=2,224), patients with COPD (n=211) were older, predominantly male, and had a greater history of smoking. Education levels differed significantly between the non-COPD and COPD groups, with the COPD group having lower levels of education. The data for the prevalence of the comorbid conditions, which are presented in percentages (%) by applying the survey analysis, showed that DM, hypertension, ischemic heart disease, and cerebrovascular accident are more common in the COPD group than in the non-COPD group. The PHQ-9 scores was higher in non-COPD group (2.5±3.5 vs 2.0±3.1 for non-COPD and early COPD group, respectively; p=0.04). But, prevalence of moderate-to-severe depression was not different between the 2 groups (27.8% vs 20.0%; p=0.36) (Table 1). The scores for each item on the PHQ-9 for the COPD and non-COPD subjects are presented in Table S1.
Table 1.
Baseline characteristics of patients with non-COPD and early COPD
| Variables | Non-COPDa (N=2,224) | Early COPDa (N=211) | P-value |
|---|---|---|---|
| Age, years | 56.1±10.2 | 64.7±9.0 | <0.01 |
| Sex, male (%) | 852 (38.3) | 208 (98.6) | <0.01 |
| BMI (kg/m2) | 24.0±3.1 | 24.1±2.9 | 0.83 |
| Ever smokerb | 782 (35.5) | 211 (100.0) | <0.01 |
| Smoking, pack-year | 7.1±13.8 | 34.7±22.7 | <0.01 |
| Living style, live alone | 300 (13.8) | 15 (7.2) | 0.01 |
| Income, low vs high | 485 (21.9) vs 595 (26.8) | 52 (24.8) vs 53 (25.2) | 0.61 |
| Level of education | |||
| Primary level | 562 (25.3) | 67 (31.7) | 0.02 |
| Secondary level | 1,069 (48.1) | 104 (49.3) | |
| University level | 592 (26.6) | 40 (19.0) | |
| Comorbidities (%) | |||
| DM | 13.2 | 25.3 | <0.01 |
| HTN | 33.0 | 46.6 | <0.01 |
| Ischemic heart disease | 1.8 | 4.8 | 0.01 |
| CKD | 0.3 | 0 | 0.48 |
| CVA | 1.4 | 3.2 | 0.03 |
| History of PTB | 3.9 | 6.5 | 0.12 |
| History of cancer | 4.9 | 3.6 | 0.37 |
| Lung function | |||
| FEV1, % predicted | 95.5±12.0 | 79.8±13.1 | <0.01 |
| FEV1/FVC (%) | 79.4±4.8 | 63.5±5.5 | <0.01 |
| Index of QoL | |||
| EQ-5D | 0.9±0.1 | 0.9±0.1 | 0.77 |
| PHQ-9 | |||
| Total score | 2.5±3.5 | 2.0±3.1 | 0.04 |
| Moderate to severe depression | 109 (27.8) | 6 (20.0) | 0.36 |
Notes:
Data are presented as number (%) or mean ± SD.
Ever smoker includes current or ex-smoker.
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; CVA, cerebrovascular accident; DM, diabetes mellitus; EQ-5D, EuroQol-5 dimensions questionnaire; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HTN, hypertension; PHQ-9, Patient Health Questionnaire-9; PTB, pulmonary tuberculosis; QoL, quality of life.
Clinical characteristics of the patients with early COPD according to depression
Table 2 shows the clinical features of the patients with early COPD with and without depression. Patients with early COPD and depression at the same time were more likely to live alone in low QoL status than those early COPD patients without depression. With regard to the comorbidities, patients with early COPD and depression had a significantly higher prevalence of DM than those without depression. The results of the comparative analyses of each item of the PHQ-9 for the subjects with and those without depression are presented in Table S2.
Table 2.
Comparison of demographic and clinical characteristics among patients with early COPD with or without depressiona
| Variables | Early COPD
|
P-value | |
|---|---|---|---|
| Without depression | With depression | ||
| Subjects | 181 (85.8) | 30 (14.2) | |
| Age, years | 64.9±8.9 | 64.0±9.5 | 0.65 |
| Sex, male (%) | 179 (98.9) | 29 (96.7) | 0.34 |
| BMI (kg/m2) | 24.2±2.9 | 23.4±2.9 | 0.20 |
| Smoking, pack-year | 35.1±23.9 | 32.6±13.3 | 0.57 |
| Living style, live alone | 8 (4.5) | 7 (23.3) | <0.01 |
| Income, low vs high | 43 (23.8) vs 46 (25.4) | 9 (31.0) vs 7 (24.1) | 0.69 |
| Level of education | |||
| Primary level | 57 (31.5) | 10 (33.3) | 0.42 |
| Secondary level | 92 (50.8) | 12 (40.0) | |
| University level | 32 (17.7) | 8 (26.7) | |
| PHQ-9 score | 1.0±1.3 | 7.9±4.0 | <0.01 |
| Comorbidities | |||
| DM | 35 (20.2) | 10 (41.7) | 0.02 |
| HTN | 88 (48.6) | 19 (63.3) | 0.14 |
| Ischemic heart disease | 10 (5.5) | 1 (3.3) | 0.62 |
| CKD | NA | NA | |
| CVA | 9 (5.0) | 1 (3.3) | 0.70 |
| Obesity, underweight vs obesity | 3 (1.7) vs 117 (64.6) | 1 (3.3) vs 16 (53.3) | 0.45 |
| History of PTB | 12 (6.6) | 1 (3.3) | 0.49 |
| History of cancer | 10 (5.5) | 1 (3.3) | 0.62 |
| Lung function | |||
| FEV1, % predicted | 80.1±13.2 | 77.7±12.8 | 0.35 |
| FEV1/FVC | 63.6±0.1 | 62.9±0.1 | 0.49 |
| Index of QoL | |||
| EQ-5D | 1.0±0.1 | 0.8±0.2 | <0.01 |
Note:
Data are presented as number (%) or mean ± SD.
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; CVA, cerebrovascular accident; DM, diabetes mellitus; EQ-5D, EuroQol-5 dimensions questionnaire; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HTN, hypertension; NA, not applicable; PHQ-9, Patient Health Questionnaire-9; PTB, pulmonary tuberculosis; QoL, quality of life.
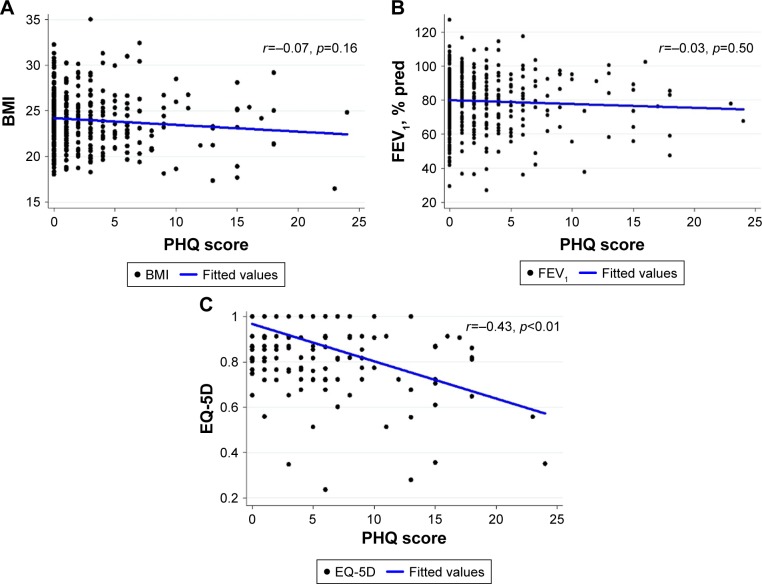
There was no significant difference in BMI between the groups, nor was there any difference in the analysis according to the degree of obesity according to Asian Pacific guidelines for obesity.26 Lung function did not differ between the groups. QoL was significantly lower in the depressed group (EQ-5D: early COPD without depression, 1.0±0.1; early COPD with depression, 0.8±0.2; p<0.01). Among the possible relevant factors (Figure 2), only the EQ-5D was significantly and negatively correlated with PHQ-9 scores (Spearman rank correlation coefficient, −0.43; p<0.01; Figure 2C).
Figure 2.
Correlation between PHQ score and (A) BMI; (B) FEV1; and (C) EQ-5D.
Abbreviations: BMI, body mass index; EQ-5D, EuroQol-5 dimensions questionnaire; FEV1, forced expiratory volume in 1 second; PHQ, Patient Health Questionnaire; pred, predicted.
Risk factors for depression in patients with early COPD
To identify the factors that contribute to depression in patients with early COPD, univariate and stepwise multivariate logistic regression analyses were conducted, and the results, which are presented in Table 3, showed that female sex (adjusted OR, 1.79; 95% CI, 1.38–2.31; p<0.01), living alone (adjusted OR, 1.86; 95% CI, 1.37–2.51; p<0.01), and low income (adjusted OR, 2.17; 95% CI, 1.55–3.04; p<0.01) were related to the development of depression in patients with early COPD. The EQ-5D was also significant in the logistic regression analysis, but it was not included as a single variable considering the ambiguity of the causal relationship with depression.
Table 3.
Factors associated with depression in patients with early COPD
| Variables | Univariate analysis
|
Multivariate analysisa
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Age | 0.99 | 0.95–1.03 | 0.64 | 0.99 | 0.98–1.01 | 0.45 |
| Sex, female | 3.09 | 0.27–35.14 | 0.36 | 1.79 | 1.38–2.31 | <0.01 |
| Living style, live alone | 6.51 | 2.16–19.62 | <0.01 | 1.86 | 1.37–2.51 | <0.01 |
| Income | ||||||
| Low vs high | 0.73 | 0.25–2.12 | 0.56 | 2.17 | 1.55–3.04 | <0.01 |
| Level of education | ||||||
| Primary vs university level | 1.43 | 0.51–3.97 | 0.50 | 0.75 | 0.50–1.11 | 0.15 |
| DM | 2.82 | 1.15–6.87 | 0.02 | 1.23 | 0.88–1.72 | 0.22 |
| FEV1, % predicted | 0.99 | 0.96–1.02 | 0.35 | |||
| FEV1/FVC | 0.10 | 0–72.72 | 0.49 | |||
Note:
Adjusted for age, sex, BMI, living style, level of income, level of education and comorbid DM.
Abbreviations: BMI, body mass index; DM, diabetes mellitus; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
Discussion
The present study showed that subjects with early COPD and depression simultaneously were more often females living alone in low socioeconomic status compared with subjects without depression. The most notable aspect of our study was that depression was assessed by using a valid and objective tool. Besides, studies on early COPD are rare. There is a lack of data on the clinical features of early COPD because it is extremely difficult to enroll patients in clinical trials or cohort studies because of the mild, asymptomatic symptoms rarely requiring a visit to the hospital. However, we can evaluate these patients through the national health checkup project. This is another noteworthy point in this study.
Like patients with other chronic disease, patients with COPD have a higher prevalence of depression than the general population does, and the relative risk of developing depression was highest in patients with severe COPD.27 The key pathophysiological mechanisms underlying the association between COPD and depression are not fully understood. However, because of several common contributing factors related to the development and progression of each disease, depression is considered one of the comorbid conditions of COPD. A number of mechanisms might underlie the association of depression with COPD. First, smokers tend to be depressed. Hamalainem et al,28 found a 2.24-fold increased risk of depression in current smokers compared with nonsmokers. This result might have been related to smoke-induced inflammation29 or nicotinic acetylcholine receptor activation.30 Second, because COPD is a chronic inflammatory disease, depression might occur as part of the systemic inflammatory response. Although systemic inflammatory markers, such as tumor necrosis factor-α31 and soluble tumor necrosis factor receptor-1,32 have been reported to positively correlate with depression in patients with COPD. Third, hypoxia might affect the development of depression as 57% and 18% of patients with severe COPD requiring long-term oxygen therapy had depression and severe depression, respectively.33 However, in the present study, depression defined by PHQ-9 was not prevalent in COPD subjects compared to non-COPD subjects. This result was probably due to the nature of our data, in that our study did not include patients with severe COPD but only patients with early COPD who were receiving routine checkups.
In this study, the risk factors associated with depression in early COPD patients were female sex, living alone, and low income. Because we only analyzed patients with early COPD whose respiratory symptoms were not severe, results consistent with the known risk factors of depression in the general population were identified.34,35 The female gender is one of the most significant predictors of depression in early COPD as in the general population. Globally, the depression prevalence is higher in females than in males, and this suggests that the differential risk may have resulted from biological differences and depends less on cultural and socioeconomic factors.36 There is no clear evidence of gender difference on depression, but several possible relating factors are reported such as the tendency to internalize emotions or the occurrence of illness associated with depression, such as premenstrual emotional disorder, postpartum depression, and anxiety.37,38 However, this gender difference of risk of depression decreases with age and is similar at ages older than 65 years.39 Given the fact that the mean age of female subjects in this study is over 65 years of age and female gender is a risk factor for depression in early COPD subjects, this suggests that there may be a difference in gender perception or response to COPD disease itself.
Studies on clinical features of early COPD patients are rare, as those patients generally do not experience symptoms to induce hospital visits. However, we benefitted from the use of the KNHANES to identify these groups of patients. It remains unclear whether knowing the clinical feature and treating asymptomatic early COPD could be beneficial with regard to the aspect of delaying disease progression and changing the clinical outcome. But considering the pathogenesis and continuum of disease progression suggests that identifying and treating these patients might influence the course of disease. In fact, EQ-5D scores in early COPD patients were almost normal, but EQ-5D was significantly lower in patients with depression. Except for the severity of COPD, depression may have an impact on overall QoL. This suggests that early detection of depressive symptom in early COPD patients and conducting an appropriate intervention may affect the patient’s clinical course.
There are several limitations to consider. First, COPD was defined by spirometry-confirmed airflow obstruction, but only prebronchodilator spirometry results were available in the KNHANES protocol. However, the prebronchodilator and postbronchodilator results were shown to be interchangeable in a large cohort study,40,41 and defining COPD patients not only by spirometry but smoking status as well might help clearly define the COPD patients. Second, we assessed depression using a valid questionnaire, but the gold standard for the diagnosis of depression is the DSM-IV, which was not available in the KNHANES dataset. Third, among the depressed patients with early COPD, 24 of 30 (80%) were mildly depressed. Therefore, an analysis of the severity of depression was not applicable. Finally, because all study participants were Korean, this study lacked racial diversity, which results in restrictions when it comes to generalizing of our results to all patients with early COPD.
Conclusion
In the present study, we focused on early COPD and found that the female sex, living alone, and low income were the factors related to the development of depression. The risk factors for depression in patients with early COPD were similar to those of well-known risk factors for depression in the general population. Since the KNHANES survey is conducted every 2 years, longitudinal studies regarding depression in early COPD are expected in the future.
Supplementary materials
Table S1.
Comparison of each PHQ-9 item in patients with COPD and non-COPDa
| PHQ-9 items | Non-COPD (N=2,224) | COPD (N=211) | P-value |
|---|---|---|---|
| PHQ1 (little interest or pleasure in doing things) | 0.30±0.70 | 0.24±0.64 | 0.21 |
| PHQ2 (feeling down, depressed, or hopeless) | 0.26±0.62 | 0.16±0.47 | 0.02 |
| PHQ3 (trouble falling or staying asleep, or sleeping too much) | 0.53±0.90 | 0.43±0.84 | 0.10 |
| PHQ4 (feeling tired or having little energy) | 0.63±0.91 | 0.49±0.85 | 0.04 |
| PHQ5 (poor appetite or overeating) | 0.26±0.65 | 0.19±0.60 | 0.18 |
| PHQ6 (feeling bad about yourself, or that you are a failure or have let yourself or your family down) | 0.18±0.54 | 0.21±0.60 | 0.54 |
| PHQ7 (trouble concentrating on things, such as reading the newspaper or watching television) | 0.12±0.47 | 0.12±0.46 | 0.98 |
| PHQ8 (moving or speaking so slowly that other people could have noticed, or the opposite, being so fidgety or restless that you have been moving around a lot more than usual) | 0.08±0.38 | 0.06±0.30 | 0.44 |
| PHQ9 (thoughts that you would be better off dead or hurting yourself in some way) | 0.10±0.41 | 0.06±0.31 | 0.21 |
| Total score | 2.46±3.50 | 1.95±3.07 | 0.04 |
Note:
Data are presented as mean ± SD.
Abbreviation: PHQ-9, Patient Health Questionnaire-9.
Table S2.
Comparison of each PHQ-9 items in early COPD subjects with or without depressiona
| PHQ-9 items | Without depression (N=181) | With depression (N=30) | P-value |
|---|---|---|---|
| PHQ1 (little interest or pleasure in doing things) | 0.11±0.42 | 1.0±1.1 | <0.01 |
| PHQ2 (feeling down, depressed, or hopeless) | 0.77±0.90 | 0.06±0.23 | <0.01 |
| PHQ3 (trouble falling or staying asleep, or sleeping too much) | 0.23±0.59 | 1.6±1.16 | <0.01 |
| PHQ4 (feeling tired or having little energy) | 0.29±0.61 | 1.7±1.06 | <0.01 |
| PHQ5 (poor appetite or overeating) | 0.11±0.46 | 0.70±0.99 | <0.01 |
| PHQ6 (feeling bad about yourself, or that you are a failure or have let yourself or your family down) | 0.07±0.32 | 1.03±1.07 | <0.01 |
| PHQ7 (trouble concentrating on things, such as reading the newspaper or watching television) | 0.07±0.29 | 0.43±0.94 | <0.01 |
| PHQ8 (moving or speaking so slowly that other people could have noticed, or the opposite, being so fidgety or restless that you have been moving around a lot more than usual) | 0.02±0.17 | 0.30±0.65 | <0.01 |
| PHQ9 (thoughts that you would be better off dead or hurting yourself in some way) | 0.01±0.10 | 0.37±0.72 | <0.01 |
| Total score | 0.97±1.25 | 7.90±3.96 | <0.01 |
Note:
Data are presented as mean ± SD.
Abbreviation: PHQ-9, Patient Health Questionnaire-9.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2017) [Accessed October 20, 2017]. Availabel from: http://www.goldcopd.org/
- 2.Cavailles A, Brinchault-Rabin G, Dixmier A, et al. Comorbidities of COPD. Eur Respir Rev. 2013;22(130):454–475. doi: 10.1183/09059180.00008612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li H, Srinivasan SR, Berenson GS. Comparison of the measures of pulsatile arterial function between asymptomatic younger adult smokers and former smokers: the Bogalusa Heart Study. Am J Hypertens. 2006;19(9):897–901. doi: 10.1016/j.amjhyper.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165–1185. doi: 10.1183/09031936.00128008. [DOI] [PubMed] [Google Scholar]
- 5.Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005;2(1):8–11. doi: 10.1513/pats.200404-032MS. [DOI] [PubMed] [Google Scholar]
- 6.Balcells E, Gea J, Ferrer J, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8:108. doi: 10.1186/1477-7525-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwon HY, Kim E. Factors contributing to quality of life in COPD patients in South Korea. Int J Chron Obstruct Pulmon Dis. 2016;11:103–109. doi: 10.2147/COPD.S90566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Polo C, Alcazar-Navarrete B, Ruiz-Iturriaga LA, et al. Factors associated with high healthcare resource utilisation among COPD patients. Respir Med. 2012;106(12):1734–1742. doi: 10.1016/j.rmed.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Papaioannou AI, Bartziokas K, Tsikrika S, et al. The impact of depressive symptoms on recovery and outcome of hospitalised COPD exacerbations. Eur Respir J. 2013;41(4):815–823. doi: 10.1183/09031936.00013112. [DOI] [PubMed] [Google Scholar]
- 10.Xu W, Collet JP, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178(9):913–920. doi: 10.1164/rccm.200804-619OC. [DOI] [PubMed] [Google Scholar]
- 11.de Voogd JN, Wempe JB, Koeter GH, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009;135(3):619–625. doi: 10.1378/chest.08-0078. [DOI] [PubMed] [Google Scholar]
- 12.Jordan N, Lee TA, Valenstein M, Pirraglia PA, Weiss KB. Effect of depression care on outcomes in COPD patients with depression. Chest. 2009;135(3):626–632. doi: 10.1378/chest.08-0839. [DOI] [PubMed] [Google Scholar]
- 13.The fifth Korean National Health and Nutrition Survey (KNHANES VI) [Internet] [Accessed November 18, 2017]. Available from: https://knhanes.cdc.go.kr/
- 14.Kim Y. The Korea National Health and Nutrition Examination Survey (KNHANES): current status and challenges. Epidemiol Health. 2014;36:e2014002. doi: 10.4178/epih/e2014002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rhee CK, Kim K, Yoon HK, et al. Natural course of early COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:663–668. doi: 10.2147/COPD.S122989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowe B, Spitzer RL, Grafe K, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004;78(2):131–140. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 19.Williams LS, Brizendine EJ, Plue L, et al. Performance of the PHQ-9 as a screening tool for depression after stroke. Stroke. 2005;36(3):635–638. doi: 10.1161/01.STR.0000155688.18207.33. [DOI] [PubMed] [Google Scholar]
- 20.Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28(1):71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Henkel V, Mergl R, Kohnen R, Maier W, Moller HJ, Hegerl U. Identifying depression in primary care: a comparison of different methods in a prospective cohort study. BMJ. 2003;326(7382):200–201. doi: 10.1136/bmj.326.7382.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han C, Jo SA, Kwak JH, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008;49(2):218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 23.EuroQol GroupEuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 24.Nolan CM, Longworth L, Lord J, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71(6):493–500. doi: 10.1136/thoraxjnl-2015-207782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee YK, Nam HS, Chuang LH, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. 2009;12(8):1187–1193. doi: 10.1111/j.1524-4733.2009.00579.x. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization . The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Sydney, Australia: Health Communications Australia; 2000. [Accessed on October 20, 2017]. Availabel from: http://iris.wpro.who.int/handle/10665.1/5379. [Google Scholar]
- 27.Schneider C, Jick SS, Bothner U, Meier CR. COPD and the risk of depression. Chest. 2010;137(2):341–347. doi: 10.1378/chest.09-0614. [DOI] [PubMed] [Google Scholar]
- 28.Hamalainen J, Kaprio J, Isometsa E, et al. Cigarette smoking, alcohol intoxication and major depressive episode in a representative population sample. J Epidemiol Community Health. 2001;55(8):573–576. doi: 10.1136/jech.55.8.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinden NJ, Stockley RA. Systemic inflammation and comorbidity in COPD: a result of ‘overspill’ of inflammatory mediators from the lungs? Review of the evidence. Thorax. 2010;65(10):930–936. doi: 10.1136/thx.2009.130260. [DOI] [PubMed] [Google Scholar]
- 30.Mineur YS, Picciotto MR. Nicotine receptors and depression: revisiting and revising the cholinergic hypothesis. Trends Pharmacol Sci. 2010;31(12):580–586. doi: 10.1016/j.tips.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-shair K, Kolsum U, Dockry R, Morris J, Singh D, Vestbo J. Biomarkers of systemic inflammation and depression and fatigue in moderate clinically stable COPD. Respir Res. 2011;12:3. doi: 10.1186/1465-9921-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eagan TM, Ueland T, Wagner PD, et al. Systemic inflammatory markers in COPD: results from the Bergen COPD cohort study. Eur Respir J. 2010;35(3):540–548. doi: 10.1183/09031936.00088209. [DOI] [PubMed] [Google Scholar]
- 33.Lacasse Y, Rousseau L, Maltais F. Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2001;21(2):80–86. doi: 10.1097/00008483-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Shin C, Kim Y, Park S, et al. Prevalence and associated factors of depression in general population of Korea: results from the Korea National Health and Nutrition Examination Survey, 2014. J Korean Med Sci. 2017;32(11):1861–1869. doi: 10.3346/jkms.2017.32.11.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cho MJ, Seong SJ, Park JE, et al. Prevalence and correlates of DSM-IV mental disorders in South Korean adults: the Korean Epidemiologic Catchment Area Study 2011. Psychiatry Investig. 2015;12(2):164–170. doi: 10.4306/pi.2015.12.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ford DE, Erlinger TP. Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2004;164(9):1010–1014. doi: 10.1001/archinte.164.9.1010. [DOI] [PubMed] [Google Scholar]
- 37.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry. 2014;171(4):426–435. doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartels M, Cacioppo JT, van Beijsterveldt TC, Boomsma DI. Exploring the association between well-being and psychopathology in adolescents. Behav Genet. 2013;43(3):177–190. doi: 10.1007/s10519-013-9589-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bebbington P, Dunn G, Jenkins R, et al. The influence of age and sex on the prevalence of depressive conditions: report from the National Survey of Psychiatric Morbidity. Int Rev Psychiatry. 2003;15(1–2):74–83. doi: 10.1080/0954026021000045976. [DOI] [PubMed] [Google Scholar]
- 40.Vestbo J, Prescott E, Almdal T, et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. 2006;173(1):79–83. doi: 10.1164/rccm.200506-969OC. [DOI] [PubMed] [Google Scholar]
- 41.Ischaki E, Papatheodorou G, Gaki E, Papa I, Koulouris N, Loukides S. Body mass and fat-free mass indices in COPD: relation with variables expressing disease severity. Chest. 2007;132(1):164–169. doi: 10.1378/chest.06-2789. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Comparison of each PHQ-9 item in patients with COPD and non-COPDa
| PHQ-9 items | Non-COPD (N=2,224) | COPD (N=211) | P-value |
|---|---|---|---|
| PHQ1 (little interest or pleasure in doing things) | 0.30±0.70 | 0.24±0.64 | 0.21 |
| PHQ2 (feeling down, depressed, or hopeless) | 0.26±0.62 | 0.16±0.47 | 0.02 |
| PHQ3 (trouble falling or staying asleep, or sleeping too much) | 0.53±0.90 | 0.43±0.84 | 0.10 |
| PHQ4 (feeling tired or having little energy) | 0.63±0.91 | 0.49±0.85 | 0.04 |
| PHQ5 (poor appetite or overeating) | 0.26±0.65 | 0.19±0.60 | 0.18 |
| PHQ6 (feeling bad about yourself, or that you are a failure or have let yourself or your family down) | 0.18±0.54 | 0.21±0.60 | 0.54 |
| PHQ7 (trouble concentrating on things, such as reading the newspaper or watching television) | 0.12±0.47 | 0.12±0.46 | 0.98 |
| PHQ8 (moving or speaking so slowly that other people could have noticed, or the opposite, being so fidgety or restless that you have been moving around a lot more than usual) | 0.08±0.38 | 0.06±0.30 | 0.44 |
| PHQ9 (thoughts that you would be better off dead or hurting yourself in some way) | 0.10±0.41 | 0.06±0.31 | 0.21 |
| Total score | 2.46±3.50 | 1.95±3.07 | 0.04 |
Note:
Data are presented as mean ± SD.
Abbreviation: PHQ-9, Patient Health Questionnaire-9.
Table S2.
Comparison of each PHQ-9 items in early COPD subjects with or without depressiona
| PHQ-9 items | Without depression (N=181) | With depression (N=30) | P-value |
|---|---|---|---|
| PHQ1 (little interest or pleasure in doing things) | 0.11±0.42 | 1.0±1.1 | <0.01 |
| PHQ2 (feeling down, depressed, or hopeless) | 0.77±0.90 | 0.06±0.23 | <0.01 |
| PHQ3 (trouble falling or staying asleep, or sleeping too much) | 0.23±0.59 | 1.6±1.16 | <0.01 |
| PHQ4 (feeling tired or having little energy) | 0.29±0.61 | 1.7±1.06 | <0.01 |
| PHQ5 (poor appetite or overeating) | 0.11±0.46 | 0.70±0.99 | <0.01 |
| PHQ6 (feeling bad about yourself, or that you are a failure or have let yourself or your family down) | 0.07±0.32 | 1.03±1.07 | <0.01 |
| PHQ7 (trouble concentrating on things, such as reading the newspaper or watching television) | 0.07±0.29 | 0.43±0.94 | <0.01 |
| PHQ8 (moving or speaking so slowly that other people could have noticed, or the opposite, being so fidgety or restless that you have been moving around a lot more than usual) | 0.02±0.17 | 0.30±0.65 | <0.01 |
| PHQ9 (thoughts that you would be better off dead or hurting yourself in some way) | 0.01±0.10 | 0.37±0.72 | <0.01 |
| Total score | 0.97±1.25 | 7.90±3.96 | <0.01 |
Note:
Data are presented as mean ± SD.
Abbreviation: PHQ-9, Patient Health Questionnaire-9.