Abstract
Background
Parkinson's disease (PD) patients experience cognitive impairment which has been related to reduced quality of life and functional disability. These symptoms usually progress until dementia occurs. Some studies have been published assessing the efficacy of cognitive treatments on improving cognition, functional outcome, and producing changes in brain activity.
Objective
A critical review was performed to present up-to-date neurorehabilitation effects of cognitive rehabilitation in PD, with special emphasis on the efficacy on cognition, quality of life aspects, brain changes, and the longitudinal maintenance of these changes.
Results
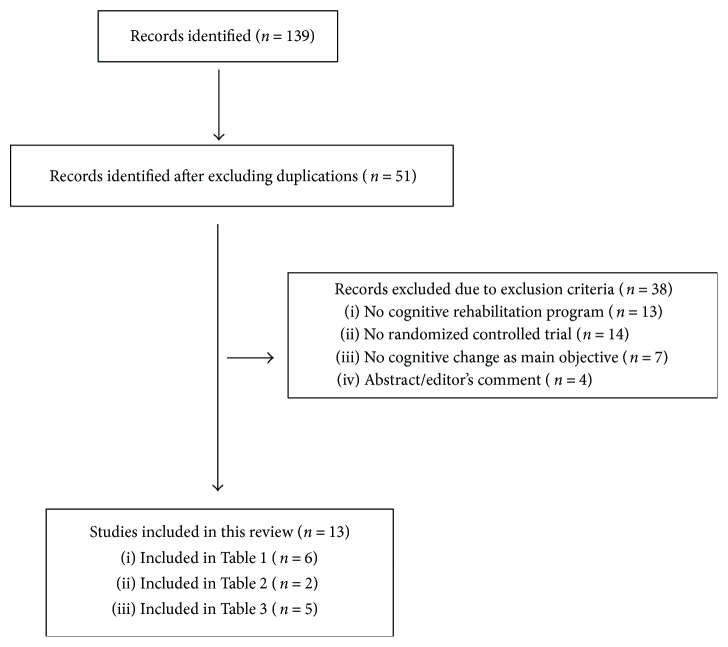
After exclusions, 13 studies were reviewed, including 6 randomized controlled trials for the efficacy on cognition, 2 randomized controlled trials regarding the brain changes after cognitive training, and 5 studies which evaluated the long-term effects of cognitive treatments.
Conclusions
Cognitive rehabilitation programs have demonstrated to be effective on improving cognitive functions, but more research is needed focusing on the efficacy on improving behavioral aspects and producing brain changes in patients with PD. Moreover, there is a need of randomized controlled trials with long-term follow-up periods.
1. Introduction
Parkinson's disease (PD) is a common neurodegenerative disease, being most of the cases diagnosed at around 60 years [1]. Traditionally, PD has been considered a motor disorder, and the core motor symptoms are rigidity, tremor, bradykinesia (akinesia), and postural instability. In addition, freezing of gait (difficulty to initiate or continue walking) and flexed posture have been included in the cardinal motor symptoms of the disease [2]. Nowadays, it is known that this neurodegenerative process produces a wide range of motor and nonmotor symptoms in PD patients; hence, PD is considered a multiple system neurodegenerative disorder [3]. Among these nonmotor symptoms, cognitive impairment is an important nonmotor symptom due to its prevalence among PD patients (20–50%) [4, 5]. In addition, PD patients might develop cognitive impairment from the early stages of the disease [4, 5]. These cognitive deficits may deteriorate with the progression of the disease until dementia occurs [6, 7]. The analysis of cognitive impairment and dementia in PD patients is relevant because both have shown relationship with reduced quality of life and functional disability in PD patients [8, 9].
These cognitive impairments in PD have been related to grey matter (GM) atrophy, white matter (WM) alterations, brain functional connectivity (FC), and brain activation alterations. PD patients with Mild Cognitive Impairment (MCI) diagnosis have shown GM volume reduction in the frontal, temporal, and parietal lobes, but also in the hippocampus, amygdala, and putamen [10, 11]. Additionally, PD patients with MCI have shown widespread cerebral WM deterioration [11–13]. Interestingly, WM alterations have been found to appear before GM volume reduction in PD patients, which highlights the importance to explore the relationship between WM indexes and cognitive impairment [14]. In addition, cognitive deficits have also been related to functional brain alterations, showing altered FC and brain activation values both during resting state and during cognitive tasks inside the scanner [15, 16].
With the progression of the disease, cognitive deficits usually deteriorate until dementia occurs after 10 to 20 years [6, 17]. A study followed newly diagnosed PD patients over time and found that after 20 years, dementia was present in up to 80% of PD patients [6]. In addition, recent studies showed that the presence of MCI diagnosis in PD patients contributes to the development of dementia [7], and results support that MCI could be considered as a prodromal stage for dementia in PD [18]. Cognitive deterioration is accompanied by GM volume loss [19], WM alterations [20], and functional brain changes [21, 22]. When dementia occurs in PD patients, cortical degeneration has been extended to frontal, temporal, parietal, and occipital areas [23].
Due to the relevance of cognitive deficits, therapeutic strategies are needed to treat cognitive decline. A common cognitive rehabilitation program could be described as a behavioral treatment for cognitive impairment which focused on cognitive abilities and daily living activities, which is based on the restoration, compensation, and optimization of the cognitive functions [24, 25]. Cognitive rehabilitation programs have demonstrated their efficacy on improving cognition in different studies in PD. Several reviews [26–28] and meta-analyses [29, 30] have been published in the field. The efficacy of cognitive rehabilitation on improving cognition has been shown, but these reviews and meta-analyses highlight the importance of continuing with research focused on the efficacy of the cognitive rehabilitation approach in PD.
The main objective of the present study is to perform a critical review to present up-to-date neurorehabilitation effects of cognitive rehabilitation in PD. The first objective was to examine the efficacy of cognitive rehabilitation programs on cognition and behavioral aspects. The second objective was to review the evidence of the brain changes found after cognitive treatments. Finally, the present study analyzed the long-term effects of cognitive rehabilitation in PD.
2. Methods
2.1. Review Strategy
Studies were included from inception to December 2017. Focusing on the first objective of this critical review, which was to analyze those randomized controlled trials focused on the efficacy of cognitive rehabilitation programs on cognition, we selected only those studies that fulfilled the following criteria: (1) randomized controlled trials; (2) PD patients underwent a cognitive rehabilitation program; (3) the main objective was to investigate the change in cognition; and (4) studies including a PD control group. Among the studies that fulfilled these specific criteria, we also reported (if included in the studies) the results of the efficacy on behavioral or mood aspects, such as depression, apathy, functional disability, and quality of life aspects.
Regarding the second objective of the present review, the efficacy of cognitive rehabilitation programs in producing brain changes in PD was determined based on the following criteria: (1) randomized controlled trials; (2) PD patients underwent a cognitive rehabilitation program; (3) studies including a PD control group; and (4) brain changes were evaluated.
Finally, focusing on the last objective of the present study, the review about the long-term effects of cognitive rehabilitation programs was based on the following criteria: (1) PD patients underwent a cognitive rehabilitation program; (2) a longitudinal follow-up evaluation was performed; and (3) the main objective was to investigate the change in cognition at follow-up. In this specific section, we included both randomized controlled trials and nonrandomized trials, due to the scarce number of published studies and to have a wider perspective.
Databases included were PubMed, Medline, and Google Scholar. The search terms were specified to be found in the title of the studies. The terms were (1) Parkinson's disease/Parkinson disease; (2) cognitive rehabilitation/cognitive training/cognitive remediation; (3) attention rehabilitation/attention training/attention remediation; (4) executive training/executive rehabilitation/executive remediation; (5) memory training/memory rehabilitation/memory remediation; (6) randomized controlled trial/randomized controlled trial; and (7) cognition. The search term combinations in the databases were (1) + (2); (1) + (3); (1) + (4); (1) + (5); and (1) + (6) + (7).
A summary of study selection is shown in Figure 1. The results of the selected studies were divided into 3 different sections. First, the studies evaluating the cognitive and behavioral changes are shown in Table 1. Then, Table 2 shows the studies that assessed the brain changes after cognitive rehabilitation in PD. In addition, the longitudinal effects of cognitive rehabilitation programs are shown in Table 3. In Tables 1 and 3, different characteristics of the studies are shown, such as the sample size, characteristics of the cognitive rehabilitation program used, cognitive domains analyzed, significant results found, and limitations of each study. In Table 2, MRI acquisition, preprocessing, and analysis specifications are included for each study, along with the brain significant results and the study limitations.
Figure 1.
Summary of studies identified and included in the review.
Table 1.
Summary of the randomized controlled trials in assessing the efficacy of cognitive rehabilitation programs in PD.
| Authors | Sample | H&Y | Cognitive rehabilitation program | Tests1 | Predictors of greater improvement | MRI (Table 2) | Results | Long-term follow-up (Table 3) | Limitations/risk of bias | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Duration | Paper-pencil—P Computerized—C |
Cogn. domains trained | Format | |||||||||
| París et al. [35] |
28 PD
16 CR 12 ACG |
1–3 |
12 sessions
4 weeks 3 times/week 45 min/session |
CR—“SmartBrain tool” (P + C) ACG— speech therapy |
(i) Attention (ii) WM (iii) Memory (iv) Psychomotor speed (v) EF (vi) Visuospatial ability (vii) Language (viii) Calculation skills (ix) Culture |
Group + home | (i) Attention (ii) WM (iii) EF (iv) Processing speed (v) Verbal memory (vi) Visual memory (vii) Visuoconstruction (viii) Visuospatial ability (ix) Verbal fluency (x) Depression (xi) Quality of life (xii) Daily living activities |
— | — |
Improvements
(i) Attention/WM (ii) Information processing speed (iii) Visual memory (iv) Visuospatial ability (v) Visuoconstructive ability (vi) Semantic fluency (vii) EF |
— | Small sample size |
|
| ||||||||||||
| Edwards et al. [34] |
74 PD
32 CR 42 CG |
1–3 |
36 sessions
3 months 3 times/week 1 h/session |
CR—“InSight version of SOPT” (C) | (i) Information processing speed | Home | (i) Speed of processing (self-reported) (ii) Perception of cognitive and everyday functioning (self-reported) (iii) Depression |
<Age at PD diagnosis >Disease duration |
— |
Improvements
(i) Speed of processing |
— | No ACG Only 1 domain trained Self-reported test for cognition and functionality |
|
| ||||||||||||
| Cerasa et al. [33] |
15 PD
8 CR 7 ACG |
1–3 |
12 sessions
6 weeks 2 times/week 1 h/session |
CR—“RehaCom” (C) ACG—visuomotor coordination tapping task. In-house software (C) |
(i) Attention (ii) Information processing |
Group | (i) Attention/processing speed (ii) EF (iii) WM (iv) Spatial memory (v) Verbal memory (vi) Visuospatial orientation (vii) Verbal fluency (viii) Depression (ix) Anxiety (x) Quality of life |
— | Yes |
Improvements
(i) Attention/processing speed (ii) WM |
— | Small sample size |
|
| ||||||||||||
| Zimmermann et al. [37] |
39 PD
19 CR 20 ACG |
2a |
12 sessions
4 weeks 3 times/week |
CR—“CogniPlus” (C) ACG—“Nintendo Wii” (C) |
(i) Attention (ii) Working memory (iii) EF |
Group | (i) Attention (ii) WM (iii) EF (iv) Episodic memory (v) Visuoconstruction |
(i) WM score (ii) Flexibility score |
— | (i) ACG improved attention compared to CR | — | Small sample size No change in functionality evaluated |
| Petrelli et al. [32] |
65 PD
22 CR-NV 22 CR-MT 21 CG |
1–3 | 12 sessions 6 weeks 2 times/week 90 min/session |
P “NEUROvitalis”—NV P “mentally fit”—MF |
NV
(i) Attention (ii) Memory (iii) EF MF (i) Attention (ii) Memory (iii) Creativity |
Group + individual | (i) Attention (ii) Memory (iii) EF (iv) Visuoconstruction (v) Depression (vi) Quality of life |
— | — |
Improvements
NV versus CG (i) Working memory (ii) Short-term memory Improvements MF versus CG (i) Depression Improvements NV versus MT (i) Working memory |
12 months | Small sample size No ACG |
|
| ||||||||||||
| Peña et al. [31] |
42 PD
20 PD-CR 22 PD-ACG |
1–3 | 39 sessions 13 weeks 3 times/week 1 h/session |
CR—“REHACOP” (P) ACG—occupational activities (P) |
(i) Attention (ii) Memory (iii) Language (iv) EF (v) Social cognition (vi) PS |
Group | (i) Processing speed (ii) Memory (iii) Executive functions (iv) Social cognition (v) Functional disability (vi) Apathy (vii) Depression |
— | Yes |
Improvements
PD-CR versus PD-ACG (i) Processing speed (ii) Visual memory (iii) Social cognition (iv) Functional disability |
18 months | Small sample size |
ACG = active control group; CG = control group; CR = cognitive rehabilitation; EF = executive functions; HC = healthy controls; H&Y = Hoehn and Yahr; MRI = magnetic resonance image; PD = Parkinson's disease; WM = working memory. 1Tests assessing mood, clinical, and functionality aspects are shown in italics. aMedian.
Table 2.
Summary of randomized controlled trials in assessing brain changes related to cognitive rehabilitation programs in PD.
| Authors | MRI sample | H&Y | Cognitive rehabilitation program | MRI acquisition/preprocessing/analysis | MRI statistical analysis | MRI results | Correlation with cognitive measures | Limitations/risk of bias |
|---|---|---|---|---|---|---|---|---|
| Cerasa et al. [33] |
15 PD
8 CR 7 ACG |
1–3 | RehaCom computer program Training: (i) Attention (ii) Information processing |
Resting-state fMRI/ICA in FSL/FC analysis | ANOVA (group × time) Region of interests Dorsolateral PFC Ventrolateral PFC ACC Sup + inf parietal left Caudate Cerebellum |
Increased functional activity: (i) Left dorsolateral PFC (executive network) (ii) Superior parietal left (attention network) |
— | Small sample size Only one type of MRI acquisition |
|
| ||||||||
| Díez-Cirarda et al. [38] (cognitive results in [31]) |
30 PD
15 CR 15 ACG |
1–3 | “REHACOP” program Training: (i) Attention (ii) Memory (iii) Language (iv) EF (v) Social cognition |
Resting-state fMRI/ROI-to-ROI approach in CONN toolbox | ANOVA (group × time) Paired t-test Whole brain |
Increased FC between BA9L-BA20L and BA9R-BA20L | Yes | Small sample size and reduced at long-term follow-up Memory fMRI paradigm results at FWE uncorrected |
| Memory fMRI paradigm/model-based approach in SPM | Increased brain activation Learning task: left frontal inferior lobe |
|||||||
| Increased brain activation Memory task: left middle temporal lobe | ||||||||
| Diffusion weighted/TBSS in FSL | — | |||||||
| T1 weighted/VBM in FSL | — | |||||||
ACC = anterior cingulate cortex; ACG = active control group; BA = Brodmann area; CR = cognitive rehabilitation; EF = executive functions; FC = functional connectivity; fMRI = functional magnetic resonance imaging; FSL = FMRIB Software Library; H&Y = Hoehn and Yahr; ICA = independent component analysis; MRI = magnetic resonance image; PD = Parkinson's disease; PFC = prefrontal cortex; TBSS = tract-based spatial statistics; VBM = voxel-based morphometry.
Table 3.
Summary of cognitive rehabilitation studies in PD with longitudinal follow-up evaluation.
| Authors | Sample | H&Y | Cognitive rehabilitation program | Tests1 | MRI (Table 2) | Results (pre- and posttreatment) | Long-term follow-up (T0/T1/T2) | Limitations/risk of bias | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Duration | Paper-pencil—P Computerized—C |
Cogn. domains trained | Format | ||||||||
| Nonrandomized/noncontrolled trials | |||||||||||
| Sinforiani et al. [39] | 20 PD | 1.5 ± 0.6 |
12 sessions
6 weeks + 12 h MT |
C “TNP” |
(i) Attention (ii) Abstract reasoning (iii) Visuospatial |
Group | (i) MMSE (ii) Digit span (iii) Corsi's test (iv) Babcock's story (v) FAS phonetic (vi) Raven matrix (vii) WCST (viii) Stroop test |
— |
Improvements:
(i) Babcock (recall) (ii) FAS phonetic (iii) Raven matrix |
6 months without training: maintenance (no statistical data)
(i) Babcock (recall) (ii) FAS phonetic (iii) Raven matrix |
No CG No differentiation of the efficacy of motor or cognitive training No statistical data at follow-up |
|
| |||||||||||
| Reuter et al. [40] |
222 PD
Gr A—CR = 71 Gr B—CR-TT = 75 Gr C—CR-TT-MT = 76 (plus psychoeducation with caregivers) |
2–4 |
14 sessions
4 weeks 4 times/week 60 min/session |
P + C Group A: cognitive training Group B: cognitive + transfer training Group C: cognitive + transfer + motor training |
(i) Attention (ii) Concentration (iii) EF (iv) WM (v) Memory (vi) Processing speed |
Individual | (i) ADAS-Cog (ii) SCOPA-Cog (iii) EF-BADS (iv) PS-PASAT (v) Depression (vi) Anxiety (vii) PDQ-39 |
— |
Improvements in all groups:
(i) ADAS-Cog (ii) BADS (iii) PASAT Greater improvements in group C: (i) ADAS-Cog (ii) SCOPA-Cog (iii) BADS (iv) PASAT |
6 months with home training: group C performed more training sessions (T2 > T0)
(i) ADAS-Cog (ii) SCOPA-Cog (iii) BADS (iv) PASAT |
No ACG No PDQ-39 scores at baseline Different number of sessions between posttreatment and long-term evaluation |
|
| |||||||||||
| Adamski et al. [45] |
6 PD-CR
12 HC-CR 7 HC-CG |
— |
16 sessions
4 weeks 4 times/week 45 min/session |
C “BrainStim” |
(i) WM (ii) Encoding (iii) Recall (iv) EF (v) Visuospatial ability |
Group | (i) Attention (ii) WM (iii) Short-term memory (iv) Long-term memory (v) PS (vi) EF (vii) Depression (viii) Fatigue |
— |
Improvements in PD group:
(i) Short-term memory (ii) Long-term memory Improvements in HC groups: (iii) Diverse cognitive domains |
3 months without training: PD group increased (T2 > T0)
(i) Short-term memory |
Small sample size No PD-ACG Baseline differences between groups |
|
| |||||||||||
| Randomized controlled trials | |||||||||||
| Petrelli et al. [42] |
65 PD
22 CR-NV 22 CR-MF 21 CG |
1–3 |
12 sessions
6 weeks 2 times/week 90 min/session |
P “NEUROvitalis”—NV P “mentally fit”—MF |
NV
(i) Attention (ii) Memory (iii) EF MF (i) Attention (ii) Memory (iii) Creativity |
Group + individual | (i) Attention (ii) Memory (iii) EF (iv) Visuoconstruction (v) Depression (vi) Quality of life |
— |
Improvements in NV versus CG:
(i) Working memory (ii) Short-term memory Improvements in MF versus CG: (i) Depression Improvements in NV versus MT: (i) Working memory |
12 months without training: NV group maintenance (T2 = T0)
(i) MMSE (ii) DemTect |
Small sample size No ACG Long-term evaluation with screening tests |
|
| |||||||||||
| Díez-Cirarda et al. [41] |
42 PD
20 PD-CR 22 PD-ACG |
1–3 |
39 sessions
13 weeks 3 times/week 60 min/session |
CR—“REHACOP” (P) ACG—occupational activities (P) |
(i) Attention (ii) Memory (iii) Language (iv) EF (v) Social cognition (vi) PS |
Group | (i) PS (ii) Memory (iii) Executive functions (iv) Social cognition (v) Functional disability (vi) Apathy (vii) Depression |
Yes |
Improvements in PD-CR versus PD-ACG:
(i) PS (ii) Visual memory (iii) Social cognition (iv) Functional disability (v) Brain functional changes |
18 months without training: PD-CR increased (T2 > T0):
(i) Verbal memory (ii) Visual memory (iii) EF (iv) ToM (v) Functional disability (vi) Brain functional activity |
Small sample size Absence of CG at follow-up |
ACG = active control group; CG = control group; CR = cognitive rehabilitation; EF = executive functions; FAS = phonetic fluency test; HC = healthy controls; H&Y = Hoehn and Yahr; MMSE = minimental state examination; MRI = magnetic resonance image; MT = motor training; TT = transfer training; PD = Parkinson's disease; PS = processing speed; WCST = Wisconsin card sorting task; WM = working memory. 1Tests assessing mood, clinical, and functionality aspects are shown in italics.
3. Results
3.1. Efficacy on Improving Cognition and Behavioral Aspects
A summary of the included cognitive rehabilitation studies in PD is shown in Table 1. Studies were included if they followed guidelines for randomized controlled trials, the intervention was a cognitive rehabilitation program, and the main objective of the study was to improve cognition. As previously reported in other reviews and meta-analyses, cognitive rehabilitation improves cognition in PD [27, 29, 30]. However, there is a need for studies with larger samples and double-blind randomized controlled trials to reach generalized conclusions in PD.
A less studied aspect of cognitive rehabilitation is its efficacy on improving mood symptoms or functional disability related to the disease. Following the review-specific criteria, among the randomized controlled trials in PD, only five studies have evaluated the change in functionality and mood aspects [31–35] and two of them found positive effects [31, 32] (Table 1). Petrelli et al. compared a structured and a nonstructured cognitive training program in PD patients and found that the symptoms of depression were reduced only in those PD patients that attended the nonstructured cognitive program [32]. Peña et al. found that functional disability scores were reduced in the experimental group (3 months of cognitive training) compared to the active control group [31]. On the contrary, París et al. evaluated the change in quality of life, depressive symptoms, and activities of daily life after attending a cognitive rehabilitation program [35]. No significant changes were found in any scale, and authors related the absence of significant changes in quality of life to the short time of training (12 sessions in 1 month). In the same line, PD patients in the study of Cerasa et al. also attended a cognitive training program during 12 sessions and showed no significant changes in mood status [33]. However, in the study of Edwards et al., PD patients attended a cognitive training program during a longer period of time (3 months), but patients showed no changes in behavioral measures [34]. Among clinical symptoms of the disease, the change in depressive symptoms has been usually assessed in cognitive training studies in PD, but despite some significant changes, the overall results point to the absence of efficacy in reducing depression symptomatology after treatment [30]. However, these studies excluded patients with depression diagnosis or with severe symptoms of depression prior to participation. Therefore, this criterion could have influenced the absence of significant changes. With all, the mechanisms that make possible the improvement in quality of life aspects after a cognitive rehabilitation program are not clear. The duration of treatment and degree of structuration of the sessions could be two relevant variables to take into account when assessing transfer effects to clinical variables, but other variables seem to influence this process. Interestingly, in schizophrenia studies, the presence of a therapist during the training sessions and the group format of the training program have been suggested to influence the results on mood symptoms [36]. The cognitive sessions carried in a group format enhance social interactions between participants, and the presence of a therapist may increase the motivation and give positive feedback to the patients, which could have an impact in the affective state of patients. In fact, the two PD studies that found transfer effects to functional aspects or depressive symptoms performed a group-based cognitive training, and the training was guided by a qualified therapist [31, 32].
Moreover, detecting variables that predict the efficacy of cognitive treatments is an important aspect to take into account in order to understand the cognitive rehabilitation process, which could guide researchers to develop more effective programs and clinicians to personalize treatments for patients (Table 1). Despite the large amount of studies assessing the efficacy of cognitive rehabilitation in PD, few studies have investigated the predictors of the efficacy of cognitive treatments in PD. These PD studies found that lower age at diagnosis and longer disease duration were predictors of higher degree of cognitive improvements after rehabilitation [34], but higher scores in working memory and flexibility at baseline were related with lower degree of improvements after rehabilitation [37].
3.2. Changes in Brain Activity after Cognitive Rehabilitation
Little is known about the neurobiological effects of cognitive rehabilitation programs in PD. To date, literature is scarce about the presence of cerebral changes associated with cognitive rehabilitation programs assessed with structural and functional MRI techniques in PD. Table 2 summarized the main findings of the two randomized controlled trials in evaluating brain changes after a cognitive rehabilitation program in PD.
One study evaluated the effects of group-based attention rehabilitation on brain functional activity in PD patients [33]. PD patients were included in the trial if they had attention impairment but no other cognitive domain impaired. At pre- and post-treatment assessments, patients underwent an extensive neuropsychological assessment and resting-state fMRI were acquired. PD patients were randomly divided into experimental group and active control group. The experimental group received attention rehabilitation using “RehaCom” computer program, while the control group attended in-house software which focused on visuomotor coordination. The attention rehabilitation consisted in computer-assisted tasks which trained attention and information processing during 6 weeks. Specifically, attention rehabilitation tasks were focused on concentration and attention tasks and vigilance program and divided attention from the RehaCom software. After rehabilitation, PD patients showed improvements in attention and processing speed tasks and increased brain activation in the left dorsolateral prefrontal cortex (part of the executive resting-state network) and the left superior parietal cortex (part of the attentional resting-state network) [33] (Table 2).
A later study in PD patients evaluated the changes in brain activity after a 3-month integrative cognitive rehabilitation program [38]. PD patients underwent an extensive neuropsychological assessment at pre- and post-treatment. Regarding MRI acquisition, GM and WM changes were analyzed as well as brain activity changes during resting-state and during a memory paradigm. The cognitive rehabilitation program used was the REHACOP, a paper/pencil rehabilitation program, which trained attention, processing speed, memory, language, executive functions, and social cognition during 3 months. PD patients after cognitive rehabilitation showed increased brain FC between frontal and temporal lobes and increased brain activation during the memory paradigm in frontal and temporal areas (see Table 2). No brain structural changes were found after rehabilitation. These brain FC and activation values at post-treatment showed correlations with post-treatment cognitive performance in PD patients from the experimental group. Specifically, during resting state, FC values between frontal and temporal lobes at post-treatment correlated with executive function performance at post-treatment. Additionally, during the learning fMRI task, the brain activation values after treatment correlated with the visual memory performance at post-treatment [38].
These studies suggest that brain activity changes are possible after a cognitive rehabilitation program in PD. Further studies are needed to replicate and complement these findings.
3.3. Long-Term Effects of Cognitive Rehabilitation
Furthermore, the ultimate goal of cognitive treatments is to ensure that benefits are maintained over long periods of time, but little is known about the maintenance of cognitive improvements over time in PD patients, and a few studies have evaluated it [39–42, 45]. A summary of these studies is shown in Table 3.
The first study to evaluate the long-term effects of cognitive rehabilitation was published in 2004 by Sinforiani et al. and showed that PD patients attending a cognitive training program combined with motor training during one month showed maintenance of the cognitive benefits after 6 months [39]. However, the study did not include statistical analyses for the follow-up period. Moreover, this study did not include a control group; therefore, we cannot conclude that these possible benefits were related to the cognitive or motor training or the combination of treatments.
Another study in PD compared three training groups: “group A” which attended cognitive training, “group B” which attended cognitive training and transfer training, and “group C” which attended cognitive, transfer, and motor training [40] (Table 3). The authors found that the three groups benefited from training, but those PD patients that attended cognitive training combined with transfer training and physical activity benefited significantly more in the short term. Moreover, over the next 6 months, patients from “group C” were more motivated to spend more time training at home compared to the other groups and showed greater maintenance of cognitive improvements after 6 months [40]. However, because patients from group C spent more hours in training at home over the next 6 months compared to the other groups, these results may be influenced by the difference of hours spent in training. Finally, this study also included an intervention therapy with caregivers focusing on psychoeducation, which helped the patients to continue the training tasks at home [40] (Table 3).
A later study in PD assessed the long-term effects of cognitive rehabilitation for a longer period of time (12 months) [42]. At baseline, these PD patients were randomized to a structured cognitive rehabilitation program (NEUROvitalis), to a nonstructured cognitive rehabilitation program (mentally fit), or to a control group. After 12 months from post-treatment, PD patients that attended NEUROvitalis training program showed reduced cognitive performance compared to post-treatment, but scores were similar compared to baseline. Moreover, the risk of conversion to MCI was found higher in the control group than in any of the cognitive training groups. Regarding depression, the “mentally fit” group was the only group that showed significant reduction in depressive symptoms after training, but these changes were not maintained at follow-up (Table 3). With all, the authors concluded that a structured cognitive treatment could prevent cognitive decline [42].
Regarding the maintenance of neuroimaging changes, to date, only one study has been published assessing the longitudinal effects of cognitive rehabilitation [41]. PD patients attended a 3-month cognitive rehabilitation program and showed increased brain connectivity and activation in the frontal and temporal lobes after treatment. These patients underwent a neuropsychological and neuroimaging assessment after 18 months from post-treatment. The results showed that not only improvements in cognitive performance and functionality were maintained after 18 months but also increased FC was found at follow-up [41]. In addition, PD patients also showed maintenance of the increased brain activation during the memory paradigm at long-term compared to baseline, but the level of activation at long-term was reduced compared to post-treatment. This study showed promising findings regarding the maintenance of brain changes in a neurodegenerative disease; however, the sample size was small, and the control group was not evaluated in the long term. The results need to be replicated.
These few studies suggest the maintenance of cognitive improvements after attending a cognitive rehabilitation program in PD patients (Table 3). However, literature is scarce in this pathology and more research needs to be done, especially including neuroimaging assessment at follow-up.
4. Discussion
The studies on the efficacy of cognitive rehabilitation programs in PD suggest that cognitive rehabilitation programs are effective in improving cognition but further research is needed in this field to clarify its efficacy on functional disability and brain activity changes. Also, very little is known about the long-term maintenance of cognitive changes after rehabilitation. There are few cognitive rehabilitation studies in PD which followed the Consolidated Standards of Reporting Trials (CONSORT) guidelines for randomized controlled trials. These make more difficult to find conclusive findings. Future studies should implement these guidelines in order to improve the research quality and validity of findings.
All randomized controlled trials in PD for cognitive rehabilitation programs point to the efficacy in improving cognition. However, most of them highlighted the small sample size as a limitation, which makes it difficult to generalize the findings. Additionally, all of them used different types of cognitive training programs, with different duration and type of exercises. One of the future steps to be taken towards understanding the efficacy of cognitive rehabilitation is identifying the characteristics that make an integrative cognitive rehabilitation program effective against cognitive impairment. A review of cognitive rehabilitation concluded that better results may be obtained in a group-based format compared to an individual format [28]. However, while most of the rehabilitation studies in PD are group-based, this question has not been directly addressed. In addition, a recent meta-analysis compared the efficacy of standardized with tailored (individualized) cognitive interventions, but found that there were insufficient studies for a statistical comparison [29]. Furthermore, other variables are also to be defined, such as the most appropriate number of sessions, their frequency, and the duration of the treatment. Also, the number of cognitive domains trained may also influence the results. Moreover, predictors of the efficacy of cognitive treatments are useful in the disease to adequate cognitive treatment to the patient. Very few studies have evaluated this aspect, and research is needed in the field.
Regarding patients' characteristics, most of the randomized controlled trials in PD have been performed with PD patients at the early Hoehn and Yahr stages of the disease. Future studies should also include PD patients at more advanced stages to evaluate whether cognitive treatments could also benefit these patients. Interestingly, a study protocol was recently published addressing the efficacy of a cognitive rehabilitation in PD patients with dementia, but results are pending [43].
Moreover, transfer effects to clinical aspects have been found in some cognitive rehabilitation studies in PD; however, other studies found no significant changes. The mechanisms that make possible to transfer benefits to clinical variables are unknown. There is an urgent need of studies analyzing this subject. The last goal of cognitive rehabilitation programs is to improve quality of life of patients. Future studies should also include clinical and functionality scales in pre- and post-treatment neuropsychological assessments.
On the other hand, promising findings have been found regarding brain changes after treatment in PD, which support the efficacy of cognitive rehabilitation programs in the disease. Results showing brain connectivity and activation increments after a cognitive treatment of less than 3 months in patients with a neurodegenerative disease are relevant in the field of neurorehabilitation. Future studies should include the MRI acquisition as part of the protocol assessment to evaluate brain changes after treatment and replicate the findings.
All these changes have been analyzed at follow-up, and some studies found maintenance of these improvements. Future randomized controlled trials should include follow-up periods in order to replicate previous findings and assess whether the improvements after training could be maintained over time. It would be also interesting to examine the maintenance of these changes in PD patients with and without booster sessions.
Another aspect to be taken into account during the rehabilitation process of the patient is the role of the caregiver. Some cognitive rehabilitation studies have included an intervention which focused on psychoeducation with the caregivers of the PD patients [40, 44]. The psychoeducation usually addresses aspects of the disease, patients' care management, information about help aids, and the importance of the self-care [40, 44]. These studies found that the caregivers gain self-confidence and felt more confident to take care of the person with the disease.
In conclusion, cognitive rehabilitation programs have demonstrated to be effective in improving cognitive functions and may also improve functional disability and produce brain changes in patients with PD. In addition, to provide a complete or integrative treatment, the combination of cognitive training with other types of trainings or the intervention with the caregivers should be further analyzed. More research should be performed in the field, with a view to reaching generalized conclusions and including cognitive rehabilitation in the standard of care of PD patients.
Acknowledgments
The authors thank ASPARBI (Parkinson's Disease Association in Biscay) and all the patients involved in the study. This study was supported by the Department of Health of the Basque Government (2011111117), the Ministerio de Economía y Competitividad (PSI2012-32441), and the Department of Education and Science of the Basque Government (Equipo A) (IT946-16).
Disclosure
This article is a contribution to the special issue entitled Neurorehabilitation: Neural Plasticity and Functional Recovery 2018.
Conflicts of Interest
Natalia Ojeda and Javier Peña are coauthors and copyright holders of the REHACOP cognitive rehabilitation program, published by Parima Digital, S.L. (Bilbao, Spain). María Díez-Cirarda and Naroa Ibarretxe-Bilbao have no conflicts of interest to report.
References
- 1.Hirsch L., Jette N., Frolkis A., Steeves T., Pringsheim T. The incidence of Parkinson’s disease: a systematic review and meta-analysis. 2016;46(4):292–300. doi: 10.1159/000445751. [DOI] [PubMed] [Google Scholar]
- 2.Xia R., Mao Z.-H. Progression of motor symptoms in Parkinson’s disease. 2012;28(1):39–48. doi: 10.1007/s12264-012-1050-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tolosa E., Gaig C., Santamaria J., Compta Y. Diagnosis and the premotor phase of Parkinson disease. 2009;72(7) Supplement 2:S12–S20. doi: 10.1212/WNL.0b013e318198db11. [DOI] [PubMed] [Google Scholar]
- 4.Muslimovic D., Post B., Speelman J. D., Schmand B. Cognitive profile of patients with newly diagnosed Parkinson disease. 2005;65(8):1239–1245. doi: 10.1212/01.wnl.0000180516.69442.95. [DOI] [PubMed] [Google Scholar]
- 5.Yarnall A. J., Breen D. P., Duncan G. W., et al. Characterizing mild cognitive impairment in incident Parkinson disease: the ICICLE-PD study. 2014;82(4):308–316. doi: 10.1212/WNL.0000000000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hely M. A., Reid W. G. J., Adena M. A., Halliday G. M., Morris J. G. L. The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. 2008;23(6):837–844. doi: 10.1002/mds.21956. [DOI] [PubMed] [Google Scholar]
- 7.Hoogland J., Boel J. A., de Bie R. M. A., et al. Mild cognitive impairment as a risk factor for Parkinson’s disease dementia. 2017;32(7):1056–1065. doi: 10.1002/mds.27002. [DOI] [PubMed] [Google Scholar]
- 8.Leroi I., McDonald K., Pantula H., Harbishettar V. Cognitive impairment in Parkinson disease: impact on quality of life, disability, and caregiver burden. 2012;25(4):208–214. doi: 10.1177/0891988712464823. [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal E., Brennan L., Xie S., et al. Association between cognition and function in patients with Parkinson disease with and without dementia. 2010;25(9):1170–1176. doi: 10.1002/mds.23073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melzer T. R., Watts R., MacAskill M. R., et al. Grey matter atrophy in cognitively impaired Parkinson’s disease. 2012;83(2):188–194. doi: 10.1136/jnnp-2011-300828. [DOI] [PubMed] [Google Scholar]
- 11.Duncan G. W., Firbank M. J., Yarnall A. J., et al. Gray and white matter imaging: a biomarker for cognitive impairment in early Parkinson’s disease? 2016;31(1):103–110. doi: 10.1002/mds.26312. [DOI] [PubMed] [Google Scholar]
- 12.Zheng Z., Shemmassian S., Wijekoon C., Kim W., Bookheimer S. Y., Pouratian N. DTI correlates of distinct cognitive impairments in Parkinson’s disease. 2014;35(4):1325–1333. doi: 10.1002/hbm.22256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsui H., Nishinaka K., Oda M., Niikawa H., Kubori T., Udaka F. Dementia in Parkinson’s disease: diffusion tensor imaging. 2007;116(3):177–181. doi: 10.1111/j.1600-0404.2007.00838.x. [DOI] [PubMed] [Google Scholar]
- 14.Rektor I., Svátková A., Vojtíšek L., et al. White matter alterations in Parkinson’s disease with normal cognition precede grey matter atrophy. 2018;13(1, article e0187939) doi: 10.1371/journal.pone.0187939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cabeza R., Nyberg L. Imaging cognition II: an empirical review of 275 PET and fMRI studies. 2000;12(1):1–47. doi: 10.1162/08989290051137585. [DOI] [PubMed] [Google Scholar]
- 16.Christopher L., Strafella A. P. Neuroimaging of brain changes associated with cognitive impairment in Parkinson’s disease. 2013;7(2):225–240. doi: 10.1111/jnp.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams-Gray C. H., Mason S. L., Evans J. R., et al. The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. 2013;84(11):1258–1264. doi: 10.1136/jnnp-2013-305277. [DOI] [PubMed] [Google Scholar]
- 18.Johnson D. K., Langford Z., Garnier-Villarreal M., Morris J. C., Galvin J. E. Onset of mild cognitive impairment in Parkinson disease. 2016;30(2):127–133. doi: 10.1097/WAD.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramírez–Ruiz B., Martí M. J., Tolosa E., et al. Longitudinal evaluation of cerebral morphological changes in Parkinson’s disease with and without dementia. 2005;252(11):1345–1352. doi: 10.1007/s00415-005-0864-2. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y., Wu I. W., Tosun D., Foster E., Schuff N., the Parkinson’s Progression Markers Initiative Progression of regional microstructural degeneration in Parkinson’s disease: a multicenter diffusion tensor imaging study. 2016;11(10, article e0165540) doi: 10.1371/journal.pone.0165540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang C., Tang C., Feigin A., et al. Changes in network activity with the progression of Parkinson’s disease. 2007;130(7):1834–1846. doi: 10.1093/brain/awm086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Segura B., Ibarretxe-Bilbao N., Sala-Llonch R., et al. Progressive changes in a recognition memory network in Parkinson’s disease. 2013;84(4):370–378. doi: 10.1136/jnnp-2012-302822. [DOI] [PubMed] [Google Scholar]
- 23.Mak E., Su L., Williams G. B., O'Brien J. T. Neuroimaging correlates of cognitive impairment and dementia in Parkinson’s disease. 2015;21(8):862–870. doi: 10.1016/j.parkreldis.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 24.Bahar-Fuchs A., Clare L., Woods B. Cognitive training and cognitive rehabilitation for persons with mild to moderate dementia of the Alzheimer’s or vascular type: a review. 2013;5(4):p. 35. doi: 10.1186/alzrt189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wykes T., Spaulding W. D. Thinking about the future cognitive remediation therapy—what works and could we do better? 2011;37(Supplement 2):S80–S90. doi: 10.1093/schbul/sbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hindle J. V., Petrelli A., Clare L., Kalbe E. Nonpharmacological enhancement of cognitive function in Parkinson’s disease: a systematic review. 2013;28(8):1034–1049. doi: 10.1002/mds.25377. [DOI] [PubMed] [Google Scholar]
- 27.Biundo R., Weis L., Fiorenzato E., Antonini A. Cognitive rehabilitation in Parkinson’s disease: is it feasible? 2017;32(7):840–860. doi: 10.1093/arclin/acx092. [DOI] [PubMed] [Google Scholar]
- 28.Walton C. C., Naismith S. L., Lampit A., Mowszowski L., Lewis S. J. G. Cognitive training in Parkinson’s disease: a theoretical perspective. 2017;31(3):207–216. doi: 10.1177/1545968316680489. [DOI] [PubMed] [Google Scholar]
- 29.Lawrence B. J., Gasson N., Bucks R. S., Troeung L., Loftus A. M. Cognitive training and noninvasive brain stimulation for cognition in Parkinson’s disease: a meta-analysis. 2017;31(7):597–608. doi: 10.1177/1545968317712468. [DOI] [PubMed] [Google Scholar]
- 30.Leung I. H. Cognitive training in Parkinson disease. 2015;85:1–9. doi: 10.1212/WNL.0000000000002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peña J., Ibarretxe-Bilbao N., García-Gorostiaga I., Gomez-Beldarrain M. A., Díez-Cirarda M., Ojeda N. Improving functional disability and cognition in Parkinson disease: randomized controlled trial. 2014;83(23):2167–2174. doi: 10.1212/WNL.0000000000001043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Petrelli A., Kaesberg S., Barbe M. T., et al. Effects of cognitive training in Parkinson’s disease: a randomized controlled trial. 2014;20(11):1196–1202. doi: 10.1016/j.parkreldis.2014.08.023. [DOI] [PubMed] [Google Scholar]
- 33.Cerasa A., Gioia M. C., Salsone M., et al. Neurofunctional correlates of attention rehabilitation in Parkinson’s disease: an explorative study. 2014;35(8):1173–1180. doi: 10.1007/s10072-014-1666-z. [DOI] [PubMed] [Google Scholar]
- 34.Edwards J. D., Hauser R. A., O'Connor M. L., Valdés E. G., Zesiewicz T. A., Uc E. Y. Randomized trial of cognitive speed of processing training in Parkinson disease. 2013;81(15):1284–1290. doi: 10.1212/WNL.0b013e3182a823ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.París A. P., Saleta H. G., de la Cruz Crespo Maraver M., et al. Blind randomized controlled study of the efficacy of cognitive training in Parkinson’s disease. 2011;26(7):1251–1258. doi: 10.1002/mds.23688. [DOI] [PubMed] [Google Scholar]
- 36.Cella M., Preti A., Edwards C., Dow T., Wykes T. Cognitive remediation for negative symptoms of schizophrenia: a network meta-analysis. 2017;52:43–51. doi: 10.1016/j.cpr.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 37.Zimmermann R., Gschwandtner U., Benz N., et al. Cognitive training in Parkinson disease: cognition-specific vs nonspecific computer training. 2014;82(14):1219–1226. doi: 10.1212/WNL.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 38.Díez-Cirarda M., Ojeda N., Peña J., et al. Increased brain connectivity and activation after cognitive rehabilitation in Parkinson’s disease: a randomized controlled trial. 2017;11(6):1640–1651. doi: 10.1007/s11682-016-9639-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sinforiani E., Banchieri L., Zucchella C., Pacchetti C., Sandrini G. Cognitive rehabilitation in Parkinson’s disease. 2004;38:387–391. doi: 10.1016/j.archger.2004.04.049. [DOI] [PubMed] [Google Scholar]
- 40.Reuter I., Mehnert S., Sammer G., Oechsner M., Engelhardt M. Efficacy of a multimodal cognitive rehabilitation including psychomotor and endurance training in Parkinson’s disease. 2012;2012:15. doi: 10.1155/2012/235765.235765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Díez-Cirarda M., Ojeda N., Peña J., et al. Long-term effects of cognitive rehabilitation on brain, functional outcome and cognition in Parkinson’s disease. 2018;25(1):5–12. doi: 10.1111/ene.13472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Petrelli A., Kaesberg S., Barbe M. T., et al. Cognitive training in Parkinson’s disease reduces cognitive decline in the long term. 2015;22(4):640–647. doi: 10.1111/ene.12621. [DOI] [PubMed] [Google Scholar]
- 43.Hindle J. V., Watermeyer T. J., Roberts J., et al. Cognitive rehabilitation for Parkinson’s disease dementia: a study protocol for a pilot randomised controlled trial. 2016;17(1):p. 152. doi: 10.1186/s13063-016-1253-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.A’Campo L. E. I., Spliethoff-Kamminga N. G. A., Macht M., Roos R. A. C., The EduPark Consortium Caregiver education in Parkinson’s disease: formative evaluation of a standardized program in seven European countries. 2010;19(1):55–64. doi: 10.1007/s11136-009-9559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adamski N., Adler M., Opwis K., Penner I. K. A pilot study on the benefit of cognitive rehabilitation in Parkinson’s disease. 2016;9(3):153–164. doi: 10.1177/1756285616628765. [DOI] [PMC free article] [PubMed] [Google Scholar]