Abstract
Undiagnosed HIV infection is common among men who have sex with men (MSM) and transgender women (TW) in Latin America. We examined uptake of a partner notification (PN) model among MSM and TW in Tijuana, Mexico. Forty-six HIV-positive MSM/TW enrolled as index patients, and reported 132 MSM/TW sexual partners for PN. Of notified partners (90/132), 39% declined eligibility screening or participation, 39% tested for HIV, and of those 28% were newly-diagnosed HIV-positive. Partners who were seen by the index patient more than once in the past four months and those who primarily had sex with the index patient in one of their homes were more likely to be notified via PN (76% vs. 50%; p=0.01 and 86% vs. 64%, p=0.02, respectively). Lower than expected PN uptake was associated with problems identifying index patients, obtaining reliable partner contact information, and engaging notified partners.
Keywords: PARTNER NOTIFICATION, HIV TESTING, HIV INFECTION, MSM, TRANSGENDER WOMEN, MEXICO
INTRODUCTION
Strategies that support early diagnosis of HIV infection, initiation of antiretroviral therapy (ART), and viral suppression could dramatically reduce HIV transmission (1, 2). However, the effectiveness of these strategies depends on the state of engagement in the HIV care continuum (i.e., proportion of people living with HIV who are diagnosed, linked to care, retained in care, and virally suppressed) at the population level (3). Undiagnosed HIV infection is particularly concerning not only because diagnosis is the critical first step to engaging in care, but also because diagnosis is associated with reduced sexual risk behavior (4–6) and HIV transmission (7).
Men who have sex with men (MSM) and transgender women (TW) continue to be disproportionately affected by HIV infection. In Latin America, where HIV epidemics are concentrated among key populations, the odds of HIV infection among MSM are approximately 33 times that of reproductive-aged adults in the general population (8). In Argentina, Brazil, El Salvador, Peru, and Uruguay, the odds of HIV infection among TW range from 23 to 92 times that of reproductive-aged adults in those countries (9). Despite growing access to ART in Latin America, poor HIV testing coverage, as well as HIV-related stigma and discrimination toward lesbian, gay, bisexual, and transgender (LGBT) persons, remain significant barriers to improving engagement in the HIV-care continuum, particularly among key populations, such as MSM, people who inject drugs, sex workers, and transgender persons (10–12). Data from Mexico and Peru suggest the prevalence of undiagnosed HIV infection among MSM and TW may be as high as 90% (13, 14), and underscore the urgent need for effective strategies to increase HIV testing and diagnosis.
Partner notification (PN) is a standard public health strategy employed in high-income settings, such as the US and Western Europe (15, 16). The goal of PN is to control the spread of HIV and other sexually-transmitted infections (STIs) by identifying and treating undiagnosed individuals within the sexual networks of newly-diagnosed index patients (17). PN is intended to prevent reinfection of index patients (for STIs) and to facilitate early diagnosis, linkage to care, and treatment among their newly-diagnosed sexual partners (18–20). PN thus has the potential to reduce HIV/STI transmission at the population level (18, 20). The World Health Organization’s 2016 Guidelines on HIV Self-Testing and Partner Notification were developed to increase uptake of HIV PN and HIV-testing services by trained lay persons around the globe. These guidelines support the United Nations target goal to diagnose 90 percent of persons living with HIV infection by 2020 (12).
PN involves contacting the sexual partners of index patients, notifying them of their potential exposure to HIV/STIs, and advising them to seek HIV/STI testing and treatment if necessary (21). The US Centers for Disease Control and Prevention (CDC) promotes four PN strategies (CDC Passport to Partner Services)(22), including: 1) patient referral (index patient notifies partners); 2) provider referral (provider or other trained healthcare worker notifies partners); 3) contract referral (index patient agrees to notify partners, but if notifications do not take place within an agreed upon time period [e.g., 1–2 weeks], the provider will notify partners); and 4) dual referral (index patient and provider work together to notify partners).
Studies of PN in Africa, Asia, Latin America, and the Caribbean have reported that HIV/STI patients’ attitudes toward PN range from positive (e.g., viewed as facilitating early diagnosis and treatment of infected partners) to negative (e.g., embarrassment, guilt, shame) (23, 24). In studies conducted in the US, China, and Australia, the most common barriers to PN for all referral strategies include index patients’ lack of contact information for their sexual partners, reluctance to disclose their HIV serostatus, and fear of stigma, abuse, or discrimination (25–28).
In studies evaluating health department data gathered in the Netherlands, Peru, and the US, insufficient contact information for sexual partners was identified as a major challenge to the success of provider referral among MSM and TW (21, 29–31), particularly for sexual partners met online or in other anonymous settings (30–32). Other challenges associated with PN for MSM described in studies conducted in Canada and the US, include HIV-positive index patients’ refusals to provide information on sexual partners, and sexual partners who had moved away or died (4, 33). Cross-sectional survey data evaluating PN via patient referral in the US, United Kingdom, and the Netherlands have identified additional barriers that may make provider referral more attractive, particularly in the context of HIV infection. These include HIV-positive index patients’ lack of knowledge about how to notify sexual partners (17, 20, 30, 32, 34), concerns about sexual partners’ negative reactions (anger, rejection, violence, dissolution of relationship), and fears surrounding the involuntary disclosure of HIV status or other personal information, such as sexual orientation or infidelity (17, 20, 35).
Several studies, including eight randomized controlled trials (RCT) conducted in the US, have demonstrated the effectiveness of provider referral for diagnosing HIV/STIs (17, 36–41). Provider referral is generally considered more effective (defined by either greater testing of exposed partners or diagnosis of HIV/STIs) than patient referral (17, 40–43). However, only a few studies have examined the effectiveness of PN for HIV/STIs in low- to middle-income countries (LMIC), namely Cameroon, Malawi, Kenya, and Tanzania (44–47). Most LMIC lack a standardized protocol for PN (19, 44), and implementation of PN programs varies from country to country (18). Although patient referral is the most common PN strategy in LMIC because it is less costly and labor intensive (23), findings from studies conducted in sub-Saharan Africa support the effectiveness of provider referral in LMIC (44, 46, 48). Nevertheless, limited resources have resulted in general reliance upon patient referral for HIV/STI PN in Latin America (49), where PN via provider referral has not yet been evaluated.
Tijuana, Mexico is a city of approximately 1.7 million adjacent to San Diego, California. Although the number of TW living in Tijuana is unknown, it has been estimated that as many as 17,000 MSM live in the city (50). The largest annual number of newly-diagnosed HIV infections in Mexico occurs among MSM (51, 52), yet many in Tijuana are poorly engaged in the HIV care continuum (11).
In a pilot study that informed the development of the present study, HIV testing of 191 MSM and TW in Tijuana yielded an HIV prevalence of 20%, and 89% of those who tested positive were unaware of their HIV serostatus (14). Nearly 40% of the sample reported no prior HIV testing, which was associated with more condomless anal sex, non-gay identification, less “outness”, and greater internalized homophobia (53). Taken together, these findings suggest the need for strategies to better engage high-risk MSM and TW in HIV testing, such as a provider-referral PN model that provides the opportunity to undergo HIV testing.
PN is not routinely employed as a public health strategy to control the spread of HIV/STIs in Mexico nor has its uptake been evaluated among key populations in the country, including MSM and TW. The overall goal of this study was to examine the uptake of a PN model (primarily provider referral) by describing PN outcomes and identifying participant and partner characteristics associated with the notification of reported sexual partners. The PN model was based on the CDC passport to partner services (22), and used trained lay persons to conduct provider referral, as promoted by the WHO’s Guidelines on HIV Self-Testing and Partner Notification (12). The PN model aimed to increase HIV testing and the diagnosis of previously-unidentified HIV infections among MSM and TW in a non-clinical setting in Tijuana. Systematic evaluation of the uptake of a provider-referral model of PN, including information on participant and partner characteristics associated with successful PN, has the potential to inform the development, implementation, and optimization of larger-scale PN programs for MSM and TW in Tijuana and similar locations in Mexico.
METHODS
Study Population
Proyecto Enlaces (Project Links), the parent study, is a longitudinal study designed to compare the effectiveness of PN versus venue-based recruitment for identifying previously-undiagnosed HIV infections among MSM and TW in Tijuana (primary outcome). Venue-based recruitment entailed HIV screening at venues identified during our formative research as those that MSM and TW frequent to meet sexual partners, such as bars and nightclubs. During venue-based recruitment, Proyecto Enlaces staff trained to conduct rapid HIV testing approached venue patrons to inform them about the study. Interested individuals were screened for eligibility and, if eligible, were invited to undergo rapid HIV testing on-site (under a tent set up outside venues by project staff for privacy) or at the Proyecto Enlaces office at their earliest convenience.
PN was conducted from April through December 2015, and began with recruitment in healthcare settings of HIV-positive index patients who met the following eligibility criteria: (a) male or transgender female, (b) over the age of 18, (c) reported condomless anal sex with a male or transgender female in the past four months, (d) reported being diagnosed with HIV within the past two months, (e) willing to undergo confirmatory HIV testing, (f) willing and able to provide contact information for sexual partners in the past four months, and (g) reported living in Tijuana (or another city in Mexico within close geographic proximity to Tijuana).
Due to challenges identifying eligible index patients diagnosed with HIV within the past two months, in June 2015, index patient eligibility criteria were expanded to include individuals who reported being diagnosed with HIV more than one year ago, but not currently in care, as prior work suggests that behavior change following HIV diagnosis (e.g., decreased condomless anal sex) may not be maintained over time (5).
Eligibility criteria for HIV testing of sexual partners identified via PN were the same as those for index patients with four exceptions: sexual partners (a) were not required to be Tijuana residents, (b) reported anal sex (with or without a condom) with a male or transgender female in the past four months, (c) reported no previous HIV diagnosis, and (d) were willing to undergo HIV testing at the study office (a non-clinical setting). Sexual partners of index patients who were diagnosed with HIV were also eligible to report partners for PN and will henceforth be referred to as partner-based index patients.
Cisgender (i.e., gender identity matches assigned sex at birth) female sexual partners of index patients were not traced nor enrolled in Proyecto Enlaces (see Study Limitations). However, Proyecto Enlaces staff were trained to counsel HIV-positive MSM and TW about the need for notifying cisgender female partners of their possible exposure to HIV, and of referring cisgender female partners for HIV testing at free clinics in Tijuana.
Potential index patients were identified at several healthcare settings in Tijuana, including Centros Ambulatorios de Prevención y Atención en SIDA e Infecciones de Transmisión Sexual (CAPASITS), Tijuana’s main government-funded HIV treatment clinic where HIV-positive patients are provided free HIV treatment, psychological services, nursing care, counseling by social workers, and medication adherence workshops (54). Other healthcare settings in Tijuana included two private clinics (e.g., Salud Digna), nine private laboratories that perform HIV tests, and three nongovernmental organizations (NGOs) (e.g., PrevenCasa) that offer support groups and other services, including free HIV/STI testing to key populations.
In all healthcare settings, posters and flyers advertising the study were placed in waiting rooms and invited interested individuals to contact the Proyecto Enlaces office for more information about the study. Proyecto Enlaces staff also routinely visited healthcare clinics and NGOs to make announcements about the study in their waiting rooms or at support group meetings and screen interested individuals for study eligibility.
At CAPASITS, which was the main source of recruitment in a healthcare setting, clinic staff also informed their HIV-positive patients about Proyecto Enlaces and made referrals by means of ‘Consent to Contact’ forms. The forms were completed by interested patients and kept secure at the clinic until they were picked up by Proyecto Enlaces staff on a weekly basis. The staff used the completed forms to contact interested patients and then screened them for study eligibility.
Upon providing verbal consent, all potential index patients participated in a 10-minute telephone screening interview that queried demographic characteristics, sexual orientation, anal sex with a man or transgender woman in the past four months, history of HIV/AIDS diagnosis, and willingness to undergo a confirmatory HIV test
Although the staff at all healthcare settings were supportive of Proyecto Enlaces, their involvement in Proyecto Enlaces did not extend beyond roles described above. None of the healthcare settings from which index patients were recruited, including CAPASITS, offered provider-based PN services to their HIV-positive patients. Proyecto Enlaces staff, who were all lay people, were housed in a leased building and functioned independently of staff in healthcare settings.
In June 2015, index patients were recruited from newly-diagnosed individuals identified via venue-based recruitment, which was simultaneously being conducted to address the primary objective of the parent study (described above). Recruitment challenges that led to this change in our PN approach were: 1) fewer people than expected were identified at healthcare settings or referred by CAPASITS; 2) many referrals from CAPASITS were ineligible to serve as index patients; and 3) many referrals from CAPASITS were not interested in the study. Between June and December 2015, MSM and TW index patients were recruited through 22 venues, including bars and nightclubs (7), public squares or plazas (4), streets or parks (4), public bathrooms (2), gay-oriented festivals (2), sex shop (1), gymnasium (1), and cinema (1). Fifty-eight percent of index patients were identified through venue-based recruitment, and the remaining 42% were recruited through healthcare settings.
Staff Training in PN
All Proyecto Enlaces staff had some university or higher education, experience working with sexual and gender minorities in Tijuana, and received training and certification to provide HIV prevention counseling and testing from the local health department. PN was conducted by cisgender male and cisgender female staff, with all of the male staff identifying as gay men. Prior to launching the study, staff were trained in PN for HIV using materials adapted from information available on the CDC’s Passport to Partner Services website (www.learnpartnerservices.org)(22).
Staff training began with an overview of PN activities, an in-depth discussion of the essential principles of PN (e.g., client-centered, confidential, voluntary, and non-coercive), and strategies to maximize communication skills (e.g., effective listening, solicitation of feedback) and minimize barriers to effective communication (e.g., jargon, sexual or cultural bias). Staff were then trained to complete the PN process, including standard protocols for contacting sexual partners (via the telephone, Internet, field visits, and text messaging), confirming the identity of contacted individuals, conducting the initial interview with index patients and partner-based index patients (described below), eliciting names and contact information for recent sexual partners, and making referrals to community-based organizations that provide medical and psychosocial services. Procedures were practiced through role play techniques and problem-solving exercises.
Proyecto Enlaces staff were also trained in third-party encounters, delivery of letters in situations where a sexual partner could not be reached in person (e.g., sealed envelope marked confidential with mention only of an important personal matter asking them to contact Proyecto Enlaces at their earliest convenience), as well as referrals to community services and linkage to care. Staff were also trained to preserve the privacy and confidentiality of index patients and sexual partners identified via PN, and to respond appropriately to any adverse emotional or behavioral reactions from notified sexual partners.
PN Procedures
Eligible index patients were entered sequentially (non-randomized) into the PN arm of Proyecto Enlaces, which was the exclusive focus of the present study. To maximize the identification of MSM and TW with previously-undiagnosed HIV infection, provider referral was the main PN strategy employed in Proyecto Enlaces, with the option of either patient or contract referral. Specifically, index patients and partner-based index patients who preferred to notify their partners on their own, were given the option to do so and were asked to refer their partners to the study office for HIV testing (patient referral). They were further informed that Proyecto Enlaces staff would notify their partners if they did not call or visit the office within two weeks (contract referral). Issues covered in the initial interview (post-enrollment) with index patients and partner-based index patients included: disease comprehension, the importance of PN, the PN process, confidentiality of all information collected, and potential consequences of failing to notify sexual partners (e.g., potential delay in treatment for a partner infected with HIV who the index patient did not notify). Proyecto Enlaces staff also explained that participants’ identities would not be revealed to their sexual partners during the PN process. Next, Proyecto Enlaces staff elicited names, contact information (e.g., telephone, home address, email, place of work), and identifying characteristics (e.g., height, weight, body type, eye color, hair color) for all male and transgender female sexual partners in the past four months. Referral cards for HIV testing were provided for distribution to cisgender female sexual partners.
Notification Procedures
Proyecto Enlaces staff contacted the sexual partners of index patients and partner-based index patients in person or via telephone using the contact information collected. Staff were provided with a sample script for approaching sexual partners reported for PN, but were trained to use their own words to the extent needed to establish rapport with the person being notified. Staff contact with the sexual partners involved the following steps: confirm the identity of the person using locating or descriptive information, introduce self and assure a private setting, provide the notification, display a sense of urgency and concern for person’s health to encourage testing, respond with sensitivity to the person’s reaction and address any concerns or issues (e.g., How did you get my name?), inform the person that they may be eligible for HIV testing at the Proyecto Enlaces office, and screen for eligibility. If the sexual partner was not eligible, Proyecto Enlaces staff provided them with a referral to local HIV-testing services. For those who were eligible and willing, an appointment for HIV testing at the Proyecto Enlaces office was scheduled.
Study Procedures
Eligible index patients were enrolled in Proyecto Enlaces and provided a blood sample to confirm their HIV-positive status via immunofluorescence assay at the San Diego County Public Health Laboratory (SDCPHL). Eligible sexual partners identified through PN were enrolled in Proyecto Enlaces and underwent rapid HIV testing (Advanced Quality HIV ½ Test Kits, Intec Products, Inc., Xiamen, China), as well as pre- and post-test counseling according to Mexican National Guidelines (55). Study participation was complete for those whose rapid HIV test result was negative. However, those whose rapid HIV-test result was positive provided blood samples for confirmatory HIV testing at SDCPHL.
Proyecto Enlaces staff then conducted the initial PN interview, elicited sexual partner information, and administered a study questionnaire to all index patients and rapid HIV-test positive sexual partners. Confirmatory HIV-test results were delivered to index patients and rapid HIV-test positive sexual partners at a follow-up visit (approximately two weeks later), and confirmed HIV-positive index patients and sexual partners (i.e., partner-based index patients) were referred to CAPASITS for HIV care and treatment. At that time, Proyecto Enlaces staff began the PN process and attempted to notify the sexual partners of all confirmed HIV-positive index patients and partner-based index patients (except when they opted to notify partners on their own), and screen them for their eligibility to enroll in Proyecto Enlaces. Ineligible sexual partners were referred to local HIV-testing centers for testing.
All participants provided written informed consent and were compensated for their time and travel. Study procedures were approved by Institutional Review Boards at the University of California, San Diego and Xochicalco University in Tijuana.
Data Collection
Trained interviewers, native to Tijuana and with extensive experience working with sexual and gender minorities, administered the study questionnaire to participants in a private room using computer-assisted personal-interviewing (CAPI) technology. The questionnaire collected information on socio-demographics (age; gender identity; race/ethnicity; sexual orientation; duration of residence in Tijuana; education; employment; monthly income), history of incarceration, history of deportation from the US, illicit drug use in the past month (marijuana; methamphetamine; cocaine; ecstasy; amyl nitrites; heroin; tranquilizers), illicit drug and alcohol use before or during sexual intercourse in the past four months, as well as egocentric sexual network data.
The egocentric sexual network survey is based on a social network approach to the diffusion of social influences and disease transmission (56). In this study, egocentric networks are made up of HIV-positive index patients or partner-based index patients (egos) and their sexual partners (alters) (57). The survey began by asking participants to provide a name or nickname for up to 20 sexual (anal or vaginal) partners in the past four months, which included up to 20 of the male and transgender female sexual partners elicited for PN. Next, participants were asked a series of questions about each partner to elicit the following: (1) socio-demographics (age; gender; race/ethnicity; location of residence), (2) HIV status (HIV-positive; HIV-negative; unknown), (3) whether the participant perceived the partner to be the source of their HIV infection, (4) relationship type (spouse or primary partner; boyfriend/girlfriend; friend; acquaintance; casual partner; anonymous partner; paid partner; other), (5) frequency of interaction in the past four months, (6) whether the partnership was ongoing, (7) primary location of sexual intercourse in the past four months, and (8) HIV-related risk behaviors practiced with the partner in the past four months (frequency of condomless sexual intercourse; illicit drug and alcohol use before or during sexual intercourse and types of drugs used [marijuana; methamphetamine; cocaine; ecstasy; amyl nitrites; heroin; other]).
Statistical analysis
Descriptive statistics were calculated to characterize HIV-positive index patients and partner-based index patients. To evaluate uptake of our PN model among MSM and TW in Tijuana, we calculated NNTInew, which was defined as the number of HIV-positive MSM and TW that would need to be interviewed to diagnose one HIV infection (46). NNTInew was calculated by dividing the number of HIV-positive MSM and TW from whom we elicited sexual partner information for PN by the number of previously-undiagnosed HIV infections detected among their sexual partners. Finally, we conducted a partner-level analysis to examine participant (index patients and partner-based index patients) and partner characteristics associated with the notification of reported partners. To account for the potential correlation in notification outcomes among partners reported by the same participant (i.e., partners nested within the same participant), we performed this analysis using logistic generalized linear mixed models (GLMMs) with individual random effects. Analyses were conducted using SAS 9.4 (SAS Institute, Inc.; Cary, NC).
RESULTS
From April to December 2015, Proyecto Enlaces enrolled 36 HIV-positive index patients (median time since diagnosis = 7.6 days; interquartile range [IQR] = 1.1–16.2) who were recruited from venues (e.g., bars, nightclubs, parks) frequented by MSM and TW in Tijuana to meet sexual partners (58%), CAPASITS (39%), and NGO-based support groups for people living with HIV (3%). Index patients had a median age of 28 years (IQR = 23–35) and mostly identified as Hispanic (97%), male (83%), and gay (78%) or bisexual (17%) (Table 1). Nearly 50% completed at least high school and 81% reported an average monthly income >3,500 Mexican pesos (~180 USD). Any illicit drug use in the past four months was reported by 47% of index patients, with methamphetamine (31%), marijuana (28%), and amyl nitrite (11%) use being most common.
Table I.
Characteristics of HIV-positive MSM and TW index patients and partner-based index patients in Tijuana, Mexico.
| Index Patient (N=36) | Partner-based Index Patienta (N=9) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Hispanic ethnicity | 35 | 97.2 | 8 | 88.9 |
| Gender identity | ||||
| Male | 30 | 83.3 | 9 | 100.0 |
| Transgender female (male to female) | 6 | 16.7 | 0 | 0.0 |
| Sexual orientation | ||||
| Gay/homosexual | 28 | 77.8 | 6 | 66.7 |
| Heterosexual | 2 | 5.6 | 1 | 11.1 |
| Bisexual | 6 | 16.7 | 2 | 22.2 |
| ≥ High school education | 17 | 47.2 | 5 | 55.6 |
| Employed | 23 | 63.9 | 5 | 55.6 |
| Average monthly income >3500 pesos (~180 USD) | 29 | 80.6 | 4 | 57.1 |
| Ever spent time in jail | 9 | 25.0 | 4 | 44.4 |
| Ever deported from the United States | 5 | 14.3 | 3 | 37.5 |
| Any illicit drug use (past month) | 17 | 47.2 | 4 | 44.4 |
| Methamphetamine | 11 | 30.6 | 4 | 44.4 |
| Marijuana | 10 | 27.8 | 3 | 33.3 |
| Amyl nitrite (poppers) | 4 | 11.1 | 1 | 11.1 |
| Ecstasy | 2 | 5.6 | 1 | 11.1 |
| Tranquilizers | 2 | 5.6 | 1 | 11.1 |
| Cocaine | 1 | 2.8 | 0 | 0.0 |
| Heroin | 1 | 2.8 | 0 | 0.0 |
| Consumed 6 or more drinks on one occasion (past year) | 23 | 63.9 | 6 | 66.7 |
| Alcohol use before/during sex (past 4 months) | 30 | 83.3 | 9 | 100.0 |
| Illicit drug use before/during sex (past 4 months) | 15 | 41.7 | 5 | 55.6 |
| Met sexual partners online (past 4 months)b | 9 | 31.0 | 4 | 44.4 |
| Median | IQR | Median | IQR | |
| Age (years) | 28.0 | 23.0, 35.0 | 28.0 | 24.0, 31.0 |
| Duration of residence in Tijuana (years) | 11.0 | 1.5, 21.0 | 11.0 | 0.7, 27.0 |
| Number of male/transgender female sexual partners (past 4 months) | 3.5 | 1.0, 13.5 | 3.0 | 3.0, 4.0 |
Numbers may not sum to column total due to missing data; percentages may not sum to 100 due to rounding or omission of one category for binary variables.
Abbreviations: MSM=men who have sex with men; TW=transgender women; USD=US dollars; IQR=interquartile range.
One partner-based index patient did not complete the survey;
Seven index patients and one partner-based index patient missing data.
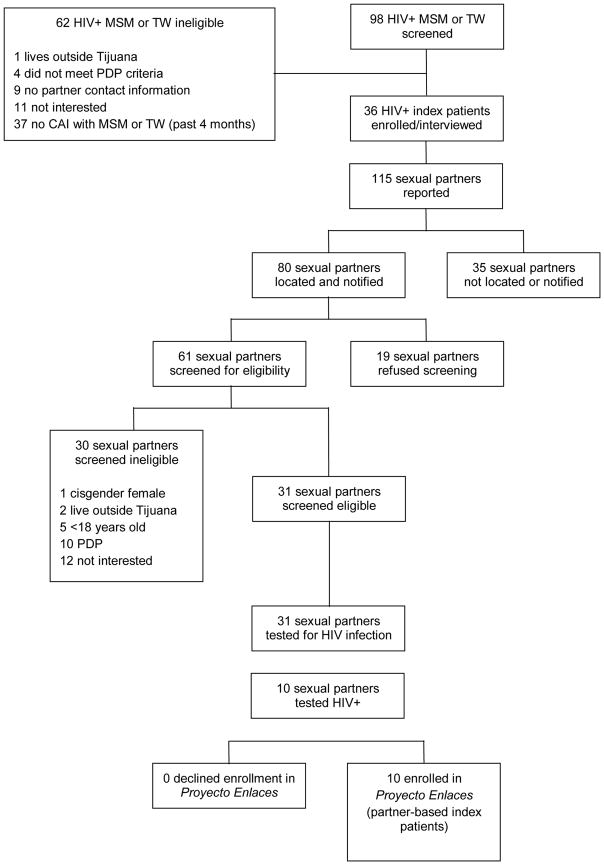
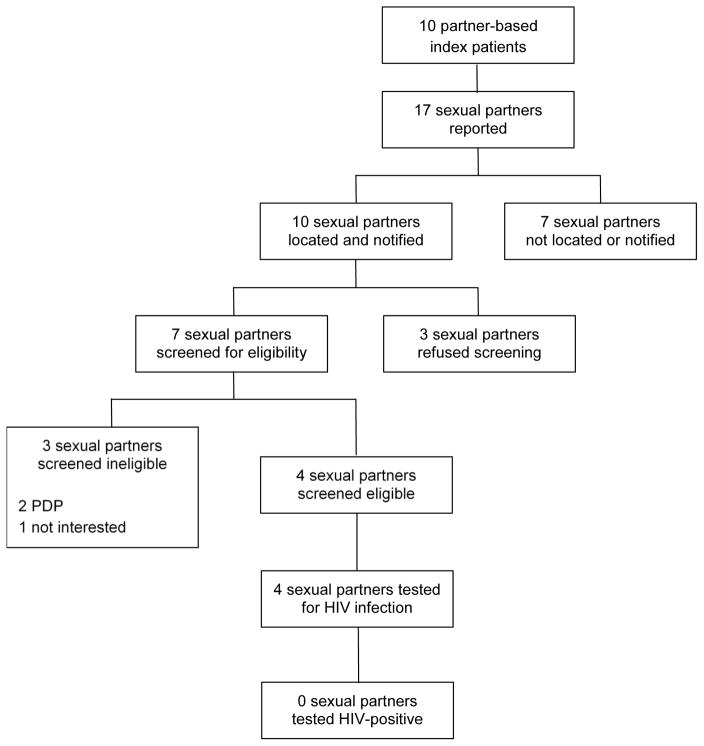
Index patients listed 115 male and transgender female sexual partners (median = 2; IQR = 1–4) for PN (Figure 1), and opted for provider referral and patient referral for 108 (94%) and seven (6%) sexual partners, respectively. After two weeks, one index patient who had opted for patient referral asked Proyecto Enlaces staff to assist him in notifying his four sexual partners. This was the only case of contract referral. PN via these strategies led to the notification of 80 sexual partners (70%) of their possible exposure to HIV (Figure 1). Among notified sexual partners, 61 (76%) agreed to be screened for eligibility and of those 31 (51%) were eligible for enrollment and underwent HIV testing, which led to the identification of 10 previously-undiagnosed HIV infections. Of these newly-diagnosed sexual partners (i.e., partner-based index patients), six reported at least one male or transgender female sexual partner (n = 17; median = 3; IQR = 3–3) who was distinct from the index patient that led to their identification via PN (Figure 2). All partner-based index patients opted for provider referral, which led to the notification of 10 (59%) sexual partners of their possible exposure to HIV. Among these sexual partners, seven (70%) agreed to be screened for eligibility and of those four (57%) were eligible for enrollment and underwent HIV testing. None of those tested were diagnosed with HIV infection. Thus, 4.6 HIV-positive MSM and TW were interviewed to identify one previously-undiagnosed HIV infection (NNTInew = 46 index patients and partner-based index patients interviewed/10 previously-undiagnosed HIV infections identified).
Figure 1.
Partner Notification Outcomes for HIV+ MSM and TW Index Patients and Sexual Partners in Tijuana, Mexico. Abbreviations: MSM = men who have sex with men; TW = transgender women; CAI = condomless anal intercourse; PDP = previously diagnosed HIV-positive.
Figure 2.
Partner Notification Outcomes for HIV+ MSM and TW Partner-Based Index Patients and Sexual Partners in Tijuana, Mexico. Abbreviations: MSM = men who have sex with men; TW = transgender women; PDP = previously diagnosed HIV-positive.
During the egocentric sexual network survey, index patients and partner-based index patients provided information on 88% (116/132) of the sexual partners they reported for PN (Table 2). Reported sexual partners were predominately male (98%), Hispanic (95%), and residents of Tijuana (89%). Nearly two-thirds (61%) of these partners were identified as casual partners, and participants reported condomless anal intercourse in the past four months with 78% of these partners. Participants saw 68% of partners more than once in the past four months, and participants expected to have sex with 39% of partners again. Overall, 68% (90/132) of partners were notified of their possible exposure to HIV. In most cases, partners were not notified because participants provided unreliable (i.e., outdated, incomplete, or inaccurate) (60%; 25/42) or no (24%; 10/42) contact information for their partners. Compared to partners who were not notified, a greater proportion of notified partners were residents of Tijuana (94% vs. 77%; F test statistic = 6.12; p-value = 0.02), were reported by participants who identify as male (94% vs. 74%; F test statistic = 7.23; p-value = 0.01), were seen by the participant who reported them more than once in the past four months (76% vs 50%; F test statistic = 6.28; p-value = 0.01), and primarily had sex with the participant in the past four months in the participant or partner’s home (86% vs. 64%; F test statistic = 5.70; p-value = 0.02).
Table II.
Participant (HIV+ index patients and partner-based index patients) and sexual partner characteristics by the notification status of sexual partners reported for PN by MSM and TW participants in Tijuana, Mexico.
| Sexual Partner not notified | Sexual partners notified | Total | F value; p-valuea | ||||
|---|---|---|---|---|---|---|---|
| Participant characteristics | (N=42) | (N=90) | (N=132) | ||||
| n | % | n | % | n | % | ||
| Participant type | 0.58; 0.45 | ||||||
| Index patient | 35 | 83.3 | 80 | 88.9 | 115 | 87.1 | |
| Partner-based index patient | 7 | 16.7 | 10 | 11.1 | 17 | 12.9 | |
| Hispanic ethnicity | 40 | 95.2 | 88 | 97.8 | 128 | 97.0 | 0.42; 0.52 |
| Male gender identity | 31 | 73.8 | 85 | 94.4 | 116 | 87.9 | 7.23; 0.01 |
| Sexual orientation | 1.19; 0.31 | ||||||
| Gay/homosexual | 31 | 73.8 | 79 | 87.8 | 110 | 83.3 | |
| Heterosexual | 4 | 9.5 | 3 | 3.3 | 7 | 5.3 | |
| Bisexual | 7 | 16.7 | 8 | 8.9 | 15 | 11.4 | |
| ≥ High school education | 26 | 61.9 | 46 | 51.1 | 72 | 54.5 | 0.72; 0.40 |
| Employed | 21 | 50.0 | 58 | 64.4 | 79 | 59.9 | 1.85; 0.18 |
| Average monthly income >3500 pesos (~180 USD) | 30 | 75.0 | 64 | 73.6 | 94 | 74.0 | 0.04; 0.83 |
| Ever spent time in jail for an offense | 11 | 26.2 | 14 | 15.6 | 25 | 18.9 | 0.83; 0.37 |
| Ever deported from the United States | 5 | 12.5 | 16 | 18.8 | 21 | 16.8 | 0.10; 0.75 |
| Any illicit drug use (past month) | 21 | 50.0 | 34 | 37.8 | 55 | 41.7 | 1.57; 0.21 |
| Consumed 6 or more drinks on one occasion (past year) | 24 | 57.1 | 56 | 62.2 | 80 | 60.6 | 0.16; 0.69 |
| Median | IQR | Median | IQR | Median | IQR | ||
| Age (years) | 24.0 | 23.0, 31.0 | 28.0 | 23.0, 35.0 | 28.0 | 23.0, 33.0 | 0.56; 0.46 |
| Duration of residence in Tijuana (years) | 13.0 | 5.0, 20.0 | 12.0 | 1.0, 22.0 | 12.0 | 1.5, 2.0.0 | 0.45; 0.50 |
| Number of male/transgender female sexual partners (past 4 months) | 15.0 | 4.0, 42.0 | 7.0 | 3.0, 12.0 | 8.5 | 3.0, 15.0 | 1.91; 0.17 |
| Sexual partner characteristics | (N=36) | (N=80) | (N=116) | ||||
| n | % | n | % | n | % | ||
| Hispanic ethnicity | 33 | 91.7 | 77 | 96.3 | 110 | 94.8 | 0.17; 0.68 |
| Male gender identity | 34 | 94.4 | 80 | 100.0 | 114 | 98.3 | e |
| Primary place of residence in Tijuana | 26 | 76.5 | 74 | 93.7 | 100 | 88.5 | 6.12; 0.02 |
| Perceived source of HIV infection | 3 | 9.4 | 18 | 26.1 | 21 | 20.8 | 2.94; 0.09 |
| Relationship type | 1.75; 0.16 | ||||||
| Primary partnerb | 6 | 16.7 | 27 | 33.8 | 33 | 28.5 | |
| Casual partnerc | 23 | 63.9 | 48 | 60.0 | 71 | 61.2 | |
| Anonymous partner | 4 | 11.1 | 3 | 3.8 | 7 | 6.0 | |
| Trade partner | 3 | 8.3 | 2 | 2.5 | 5 | 4.3 | |
| Saw partner >1 time (past 4 months) | 18 | 50.0 | 61 | 76.3 | 79 | 68.1 | 6.28; 0.01 |
| Ongoing partnershipd | 9 | 25.0 | 35 | 44.9 | 44 | 38.6 | 3.37; 0.07 |
| Primarily had sex in the participant or partner’s home (past 4 months) | 23 | 63.9 | 69 | 86.3 | 92 | 79.3 | 5.70; 0.02 |
| Any condomless anal intercourse (past 4 months) | 26 | 72.2 | 64 | 80.0 | 90 | 77.6 | 1.14; 0.29 |
| Alcohol use before/during sex (past 4 months) | 8 | 22.2 | 12 | 15.0 | 20 | 17.2 | 0.34; 0.56 |
| Illicit drug use before/during sex (past 4 months) | 11 | 30.6 | 21 | 26.3 | 32 | 27.6 | 0.08; 0.77 |
| Median | IQR | Median | IQR | Median | IQR | ||
| Median age (years) | 26.0 | 22.0, 32.5 | 28.0 | 24.0, 35.5 | 28.0 | 23.0, 34.5 | 0.32; 0.58 |
Numbers may not sum to column total due to missing data; percentages may not sum to 100 due to rounding or omission of one category for binary variables.
Abbreviations: MSM=men who have sex with men; TW=transgender women; PN=partner notification; USD=US dollars; IQR=interquartile range
Type III test of fixed effects from logistic generalized linear mixed models (GLMMs) with individual random effects to account for the correlation between sexual partners reported by the same individual.
Principal sexual partner, spouse, or boyfriend.
Non-principal sexual partner, friend, or acquaintance.
Participant expects to have sex with partner again.
Model did not converge.
Of partners notified, 39% (35/90) were unwilling to screen for eligibility or participate in the study. Although the reasons partners were unwilling to screen or participate were not assessed from the participants’ perspectives, Proyecto Enlaces staff reported three main barriers to provider-based PN among MSM and TW in Tijuana: 1) lack of or limited contact information for sexual partners reported for PN; 2) many sexual partners were suspicious of the intentions of Proyecto Enlaces staff and expressed concerns about how they had acquired their contact information; and; 3) many sexual partners were itinerant; they had no fixed address, moved around the city, stayed in hotels or migrant shelters, and did not have a landline or mobile phone. Even in cases where sexual partners had access to a phone, they often did not answer phone calls or respond to text messages, or their telephone numbers were no longer active, leaving them untraceable. In addition, many HIV-positive MSM and TW were not interested in participating in the study as index patients.
DISCUSSION
We examined uptake of a PN model for HIV infection among MSM and TW in Tijuana, Mexico. Ninety-eight HIV-positive MSM and TW were referred to Proyecto Enlaces from a healthcare setting or were identified through venue-based recruitment. A lower than expected number met eligibility criteria and enrolled in the study as an index patient (n=36). Index patients and partner-based index patients (n=10) provided information on 132 sexual partners for PN. Sixty-eight percent of sexual partners were notified, but of those, 39% refused to screen for eligibility or participate in the study, resulting in a PN uptake lower than that observed in other studies in LMIC (45, 47). We also found that on average 4.6 HIV-positive MSM and TW needed to be interviewed to identify one previously-undiagnosed HIV infection. This NNTInew is comparable to those reported by prior evaluations of PN for HIV case finding in the context of generalized epidemics in Cameroon (3.2) and Malawi (4.4) where most index patients were married women who were able to provide reliable contact information for their sexual partners (44, 46).
In studies of MSM conducted in high-income countries, the reported NNTIs were higher than we observed in Tijuana with NNTIs of 9.6 and 36.2 (in areas with ≥50% of HIV cases among MSM) in Canada and the US, respectively (4, 58). However, our low NNTI is likely a better reflection of the high prevalence of HIV among MSM and TW in this setting and the small number of identified index patients than the success of PN as a method for identifying undiagnosed HIV infection in this setting (37). Despite numerous efforts to boost index patient enrollment via the inclusion of previously-diagnosed HIV-positive MSM and TW not engaged in care, and the expansion of recruitment to venues frequented by MSM and TW, Proyecto Enlaces staff experienced major difficulties identifying MSM and TW to serve as index patients, primarily because they had limited success: 1) obtaining referrals from CAPASITS and other healthcare settings; and 2) identifying individuals at venues frequented by MSM and TW who were interested in participating as index patients. Overall, during the 9-month period that Proyecto Enlaces implemented PN (primarily provider referral), only 27% (35/132) of sexual partners reported for PN actually enrolled in the study and underwent HIV testing, thus yielding lower than expected enrollment and uptake of our PN model.
Similar to previous evaluations of PN, the primary obstacle Proyecto Enlaces staff faced in conducting PN among MSM and TW in Tijuana was the lack of reliable contact information provided for sexual partners (4, 29, 30, 32). In prior work with MSM, this barrier to PN was associated with the popularity of Internet dating websites and mobile dating apps, which often resulted in sexual encounters that lacked exchange of personal information (59). Although we did not collect information on where participants met sexual partners reported for PN, 34% of index patients and partner-based index patients met sexual partners online in the past four months, which may explain why some were unable to provide reliable contact information for their sexual partners. This is further supported by fact that successful notification was more common among partners living in Tijuana, partners with whom participants had been in contact more than once in the past four months, and partners with whom most sexual contact in the past four months occurred in the participant or partner’s home.
More specifically, our findings suggest that PN is most successful when the participant’s relationship to the sexual partner reported for PN is characterized by some degree of familiarity and/or stability, which is consistent with findings from previous studies (37, 44, 46, 47). Given that 61% of sexual partners reported for PN were characterized as casual partners, the challenges Proyecto Enlaces staff faced in implementing PN may be explained by the fact that the types of sexual partners for whom PN may be most successful are least prevalent among MSM and TW in Tijuana, suggesting the need for alternative methods of PN that do not rely on the level of familiarity between sexual partners in this setting.
Barriers to PN, cited by MSM in previous studies, were also reported to Proyecto Enlaces staff by index patients and partner-based index patients, and included lack of contact information for sexual partners, concerns about sexual partners’ negative reactions to HIV disclosure, fear of stigma and discrimination, as well as concerns about involuntary disclosure of HIV status or other personal information (17, 20, 30, 32, 34, 35). In addition, some index patients and partner-based index patients in our sample reported feelings of mistrust toward field staff, particularly during their initial encounter with them. The extent to which mistrust of research was the underlying issue in the lack of partner contact information is unknown in the present study; however, this particular challenge, if suspected, might be addressed by increased training for field staff in communication skills specific to the target population (e.g., how to build rapport quickly) and repeated training of staff (34). These barriers to provider-based PN suggest the need for alternative methods to increase uptake of PN and improve HIV testing and identification of previously-undiagnosed HIV infection among MSM and TW.
Another factor contributing to PN’s low uptake among MSM and TW in Tijuana was the high rate of refusal to screen or participate in the study among notified sexual partners. Low uptake may have been influenced by cultural norms as well as the social and sexual practices of MSM and TW in this context. Proyecto Enlaces staff reported that sexual partners were often upset and angry when contacted in person. Although Proyecto Enlaces staff made every effort not to reveal the reason for contacting sexual partners to third-parties, cultural norms supporting prejudice against the LGBT community as well as HIV-related stigma and discrimination may have shaped sexual partners’ fears that neighbors and co-workers would become suspicious and spread rumors if they were seen speaking with Proyecto Enlaces staff. Similarly, other researchers have described the importance of cultural and social contexts (35), as well as the role of stigma and discrimination as barriers to provider PN in LMIC (34, 35, 60). In response to these challenges, patient referral might be considered more acceptable to this population. However, the fact that only 6% (7/115) of participants opted for patient referral over provider referral suggests that it may not be acceptable in this setting either, and thus may not improve uptake nor HIV case finding via PN among MSM and TW in Tijuana.
Government programs and campaigns to reduce stigma toward MSM and TW may enhance uptake of PN among MSM and TW in Mexico and other LMIC. However, since social change takes time, there is an immediate need to develop and evaluate innovative, culturally-acceptable PN strategies. Van Aar et al. (32) described the value of technology-enabled PN strategies, including the use of email, text messages, Internet PN websites, and chat rooms where private messages can be posted. Many of these strategies were used by Proyecto Enlaces staff with lower than expected degrees of success. This experience underscores the point that despite multiple means of partner contact tracing, including both modern (e.g., Internet, email, social media, text messages, websites) and traditional (e.g., field visits) approaches, availability and reliability of contact information, along with acceptability of contact tracing in the target population, are paramount to the success of PN (61).
Study Limitations
Due to considerable challenges associated with identifying eligible index patients, notifying partners, and testing notified partners, Proyecto Enlaces discontinued PN in January 2016. Despite this decision, we support future studies of PN among MSM and TW in Mexico, making it important to consider our findings in light of study limitations. First, this study focused exclusively on PN for HIV among MSM and TW in a limited geographic area of Mexico. Although the findings suggest that PN for HIV has low uptake among MSM and TW in Tijuana, barriers to PN and factors associated with notification might be different for MSM and TW in other locations throughout Mexico and other LMIC. The uptake of PN could also be different for other high-risk groups in Mexico that were not included in this study, such as people who inject drugs and sex workers. Another shortcoming of this study is that we did not assess factors that could help to explain low uptake for PN among MSM and TW, which might include minimal HIV symptoms or fear of stigma and discrimination associated with HIV infection. Uptake of our PN model might also have been influenced by our in-person approach to locating sexual partners in the community, which was associated with reports of mistrust of Proyecto Enlaces staff and research in general.
Future studies should examine the acceptability of partner contact tracing in the community, as well as sexual partners’ perceptions of study staff and their behaviors. Moreover, the enrollment criteria for this study was oriented to a research study, and not a community-based PN program. Future studies should examine the feasibility of PN programs among MSM and TW in Mexico, and thereby include all sexual partners of this risk population, including cisgender female sexual partners who were excluded from the present study. Also, only a limited number of partnership factors were measured and examined in relation to successful notification. Additional factors, such as trust and communication between partners, and degree of commitment to the partner (20, 35) should be considered in future studies. Furthermore, we did not gather data or attempt to examine how Mexican laws, policies and government regulations affected uptake of PN for HIV among MSM and TW in Tijuana (18). Finally, due to the small number of TW index patients and partner-based index patients included in our sample, we were unable to examine differences in PN uptake between MSM and TW, which merits investigation in future research.
CONCLUSION
Our findings suggest that PN as implemented in Proyecto Enlaces had low uptake among MSM and TW in Tijuana. However, additional research is needed to determine whether the recruitment and participation challenges we identified can be overcome to expand PN initiatives among MSM and TW, in order to increase HIV testing and diagnosis, as well as support other aspects of their engagement in the HIV care continuum.
Acknowledgments
This research was funded by a National Institute on Drug Abuse (NIDA) grant R01DA037811 to TP. Preparation of this manuscript was supported by a NIDA K01DA040543 Mentored Research Scientist Development Award to HAP.
Footnotes
Compliance with Ethical Standards
Ethical approval
All research methods were reviewed and approved by the Institutional Review Boards at the University of California, San Diego and Xochicalco University in Tijuana, Mexico. All procedures were conducted in accordance with the 1964 Helsinki Declaration and its amendments.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Informed consent
Written informed consent was obtained from all individual participants included in this study.
References
- 1.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 3.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57:1164–71. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 4.Bergman J, Gratrix J, Pillay T, et al. Intensive HIV partner notification is effective in identifying new and previously diagnosed HIV infections in Edmonton, Canada. AIDS Patient Care STDS. 2015;29:419–22. doi: 10.1089/apc.2015.0033. [DOI] [PubMed] [Google Scholar]
- 5.Gorbach PM, Weiss RE, Jeffries R, et al. Behaviors of recently HIV-infected men who have sex with men in the year postdiagnosis: effects of drug use and partner types. J Acquir Immune Defic Syndr. 2011;56:176–82. doi: 10.1097/QAI.0b013e3181ff9750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States. Implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 7.Edelman EJ, Gordon KS, Hogben M, et al. Sexual partner notification of HIV infection among a National United States-based sample of HIV-infected men. AIDS Behav. 2014;18:1898–903. doi: 10.1007/s10461-014-0799-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4:e339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:214–22. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 10.Piñeirúa A, Sierra-Madero J, Cahn P, et al. The HIV care continuum in Latin America: challenges and opportunities. Lancet Infect Dis. 2015;15:833–9. doi: 10.1016/S1473-3099(15)00108-5. [DOI] [PubMed] [Google Scholar]
- 11.Smith LR, Patterson TL, Magis-Rodriguez C, et al. Engagement in the HIV care continuum among key populations in Tijuana, Mexico. AIDS Behav. 2016;20:1017–25. doi: 10.1007/s10461-015-1186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) [Accessed 16 Aug 2017];Guidelines on HIV Self-testing and Partner Notification. 2016 Dec; Available at http://www.who.int/hiv/pub/vct/hiv-self-testing-guidelines/en/ [PubMed]
- 13.Chow JY, Konda KA, Borquez A, et al. Peru’s HIV care continuum among men who have sex with men and transgender women: opportunities to optimize treatment and prevention. Int J STD AIDS. 2016;27:1039–48. doi: 10.1177/0956462416645727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pitpitan EV, Goodman-Meza D, Burgos JL, et al. Prevalence and correlates of HIV among men who have sex with men in Tijuana, Mexico. J Int AIDS Soc. 2015;18:19304. doi: 10.7448/IAS.18.1.19304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hogben M. Partner notification for sexually transmitted diseases. Clin Infect Dis. 2007;44(Suppl 3):S160–74. doi: 10.1086/511429. [DOI] [PubMed] [Google Scholar]
- 16.Rayment M, Curtis H, Carne C, et al. An effective strategy to diagnose HIV infection: findings from a national audit of HIV partner notification outcomes in sexual health and infectious disease clinics in the UK. Sex Transm Infect. 2017;93:94–9. doi: 10.1136/sextrans-2015-052532. [DOI] [PubMed] [Google Scholar]
- 17.Hogben M, McNally T, McPheeters M, Hutchinson AB. The effectiveness of HIV partner counseling and referral service in increasing identification of HIV-positive individuals. A systematic review. Am J Prev Med. 2007;33:S89–100. doi: 10.1016/j.amepre.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 18.Garcia de Olalla P, Molas E, Barberá MJ, et al. Effectiveness of a pilot partner notification program for new HIV cases in Barcelona, Spain. PLoS One. 2015;10:e0121536. doi: 10.1371/journal.pone.0121536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hosseinipour MC, Rosenberg NE. HIV partner notification: possible and essential. J Sex Transm Dis. 2013;40:915–6. doi: 10.1097/OLQ.0000000000000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ward H, Bell G. Partner notification. Medicine. 2014;42:314–7. doi: 10.1016/j.mpmed.2014.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Aar F, Schreuder I, van Weert Y, Spijker R, Gotz H, Op de Coul E. Current practices of partner notification among MSM with HIV, gonorrhoea and syphilis in the Netherlands: an urgent need for improvement. BMC Infect Dis. 2012;12:114. doi: 10.1186/1471-2334-12-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) [Accessed on 25 Mar 2016];Passport to Partner Services. Available at http://www.cdc.gov/std/training/passport-partner-services.htm.
- 23.Alam N, Chamot E, Vermund SH, Streatfield K, Kristensen S. Partner notification for sexually transmitted infections in developing countries: a systematic review. BMC Public Health. 2010;10:19. doi: 10.1186/1471-2458-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang AL, Peng RR, Tucker JD, Cohen MS, Chen XS. Partner notification uptake for sexually transmitted infections in China: a systematic literature review. Sex Transm Infect. 2012;88:386–93. doi: 10.1136/sextrans-2011-050275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hurt CB, Beagle S, Leone PA, et al. Investigating a sexual network of black men who have sex with men: implications for transmission and prevention of HIV infection in the United States. J Acquir Immune Defic Syndr. 2012;61:515–21. doi: 10.1097/QAI.0b013e31827076a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCarthy M, Haddow LJ, Furner V, Mindel A. Contact tracing for sexually transmitted infections in New South Wales, Australia. Sex Health. 2007;4:21–5. doi: 10.1071/sh06019. [DOI] [PubMed] [Google Scholar]
- 27.Ruan Y, Pan SW, Chamot E, et al. Sexual mixing patterns among social networks of HIV-positive and HIV-negative Beijing men who have sex with men: a multilevel comparison using roundtable network mapping. AIDS Care. 2011;23:1014–25. doi: 10.1080/09540121.2010.542127. [DOI] [PubMed] [Google Scholar]
- 28.Tobin KE, Muessig KE, Latkin CA. HIV seropositive drug users’ attitudes towards partner notification (PCRS): results from the SHIELD study in Baltimore, Maryland. Patient Educ Couns. 2007;67:137–42. doi: 10.1016/j.pec.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hogben M, Paffel J, Broussard D, et al. Syphilis partner notification with men who have sex with men: a review and commentary. J Sex Transm Dis. 2005;32:S43–7. doi: 10.1097/01.olq.0000180565.54023.bf. [DOI] [PubMed] [Google Scholar]
- 30.Mimiaga MJ, Reisner SL, Tetu AM, et al. Partner notification after STD and HIV exposures and infections: knowledge, attitudes, and experiences of Massachusetts men who have sex with men. Public Health Rep. 2009;124:111–19. doi: 10.1177/003335490912400114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perez-Brumer AG, Oldenburg CE, Segura ER, Sanchez J, Lama JR, Clark JL. Anonymous partnerships among MSM and transgender women (TW) recently diagnosed with HIV and other STIs in Lima, Peru: an individual-level and dyad-level analysis. J Sex Transm Dis. 2016 Feb 24; doi: 10.1136/sextrans-2015-052310. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Aar F, van Weert Y, Spijker R, Götz H, Op de Coul E. Partner notification among men who have sex with men and heterosexuals with STI/HIV: different outcomes and challenges. Int J STDS AIDS. 2015;26:565–73. doi: 10.1177/0956462414547398. [DOI] [PubMed] [Google Scholar]
- 33.Udeagu CN, Bocour A, Shepard CW. For partner services, do we need “face-time” or FaceTime?: trends in relative proportion of in-person notifications and HIV testing after introduction of a telephone option for HIV exposure notification by public health. J Sex Transm Dis. 2014;41:671–3. doi: 10.1097/OLQ.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 34.Adams OP, Carter AO, Redwood-Campbell L. Understanding attitudes, barriers and challenges in a small island nation to disease and partner notification for HIV and other sexually transmitted infections: a qualitative study. BMC Public Health. 2015;15:455. doi: 10.1186/s12889-015-1794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clark JL, Perez-Brumer A, Salazar X. “Manejar la Situacion”: partner notification, partner management, and conceptual frameworks for HIV/STI control among MSM in Peru. AIDS Behav. 2015;19:2245–54. doi: 10.1007/s10461-015-1049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahrens K, Kent CK, Kohn RP, et al. HIV partner notification outcomes for HIV-infected patients by duration of infection, San Francisco, 2004 to 2006. J Acquir Immune Defic Syndr. 2007;46:479–84. doi: 10.1097/qai.0b013e3181594c61. [DOI] [PubMed] [Google Scholar]
- 37.Brewer DD. Case-finding effectiveness of partner notification and cluster investigation for sexually transmitted diseases/HIV. J Sex Transm Dis. 2005;32:78–83. doi: 10.1097/01.olq.0000153574.38764.0e. [DOI] [PubMed] [Google Scholar]
- 38.Golden MR, Dombrowski JC, Wood RW, Fleming M, Harrington RD. A controlled study of the effectiveness of public health HIV partner notification services. AIDS. 2009;23:133–5. doi: 10.1097/QAD.0b013e32831fb52f. [DOI] [PubMed] [Google Scholar]
- 39.Marcus JL, Bernstein KT, Klausner JD. Updated outcomes of partner notification for human immunodeficiency virus, San Francisco, 2004–2008. AIDS. 2009;23:1024–6. doi: 10.1097/QAD.0b013e32832921a7. [DOI] [PubMed] [Google Scholar]
- 40.Mathews C, Coetzee N, Zwarenstein M, et al. A systematic review of strategies for partner notification for sexually transmitted diseases, including HIV/AIDS. Int J STD AIDS. 2002;13:285–300. doi: 10.1258/0956462021925081. [DOI] [PubMed] [Google Scholar]
- 41.Landis SE, Schoenbach VJ, Weber DJ, et al. Results of a randomized trial of partner notification in cases of HIV infection in North Carolina. N Engl J Med. 1992;326:101–6. doi: 10.1056/NEJM199201093260205. [DOI] [PubMed] [Google Scholar]
- 42.Macke BA, Maher JE. Partner notification in the United States: an evidence-based review. Am J Prev Med. 1999;17:230–42. doi: 10.1016/s0749-3797(99)00076-8. [DOI] [PubMed] [Google Scholar]
- 43.Trelle S, Shang A, Nartey L, Cassell JA, Low N. Improved effectiveness of partner notification for patients with sexually transmitted infections: systematic review. BMJ. 2007;334:354. doi: 10.1136/bmj.39079.460741.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brown LB, Miller WC, Kamanga G, et al. HIV partner notification is effective and feasible in sub-Saharan Africa: opportunities for HIV treatment and prevention. J Acquir Immune Defic Syndr. 2011;56:437–42. doi: 10.1097/qai.0b013e318202bf7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cherutich P, Golden MR, Wamuti B, et al. Assisted partner services for HIV in Kenya: a cluster randomized controlled trial. Lancet HIV. 2017;4:e74–82. doi: 10.1016/S2352-3018(16)30214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Henley C, Forgwei G, Welty T, et al. Scale-up and case-finding effectiveness of an HIV partner services program in Cameroon: an innovative HIV prevention intervention for developing countries. J Sex Transm Dis. 2013;40:909–14. doi: 10.1097/OLQ.0000000000000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kahabuka C, Plotkin M, Christensen A, et al. Addressing the first 90: a highly effective partner notification approach reaches previously undiagnosed sexual partner in Tanzania. AIDS Behav. 2017;21:2551–60. doi: 10.1007/s10461-017-1750-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Armbruster B, Helleringer S, Kalilani-Phiri L, Mkandawire J, Kohler HP. Exploring the relative costs of contact tracing for increasing HIV case finding in sub-Saharan countries. J Acquir Immune Defic Syndr. 2011;58:e29–36. doi: 10.1097/QAI.0b013e31822a9fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clark JL, Segura ER, Perez-Brumer AG, et al. Potential impact and acceptability of Internet partner notification for men who have sex with men and transgender women recently diagnosed with STD in Lima, Peru. J Sex Transm Dis. 2014;41:43–5. doi: 10.1097/OLQ.0000000000000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.USAID-Mexico. [Accessed 2013 Jul 23];HIV/AIDS Health Profile. 2010 Available at: http://transition.usaid.gov/our_work/global_health/aids/Countries/lac/mexico_profile.pdf.
- 51.Beyrer C, Abdool Karim Q. The changing epidemiology of HIV in 2013. Curr Opin HIV AIDS. 2013;8:306–10. doi: 10.1097/COH.0b013e328361f53a. [DOI] [PubMed] [Google Scholar]
- 52.Geibel S, Tun W, Tapsoba P, Kellerman S. HIV vulnerability of men who have sex with men in developing countries: Horizons studies, 2001–2008. Public Health Rep. 2010;125:316–24. doi: 10.1177/003335491012500222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pines HA, Goodman-Meza D, Pitpitan EV, et al. HIV testing among men who have sex with men in Tijuana, Mexico: a cross-sectional study. BMJ Open. 2016;6:e010388. doi: 10.1136/bmjopen-2015-010388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Centios Ambulatorios de Prevención Atención en SIDA e ITS CAPASITS. [Accessed on 11 Aug 2017];HIV & Ambulatory CARE and Prevention Clinics. http://www.censida.salud.gob.mx/interior/capasits/bcalif_capasits.html.
- 55. [Accessed on 11 Nov 2017];Mexican National Guidelines on pre- and post-testing HIV counseling. Available at: https://www.gob.mx/censida/articulos/guias-y-manuales-censida?idiom=es.
- 56.Latkin CA, Knowlton AR. Social network assessments and interventions for health behavior change: a critical review. Behav Med. 2015;41:90–7. doi: 10.1080/08964289.2015.1034645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lui H. Egocentric network and condom use among mid-age female sex workers in China: a multilevel modeling analysis. AIDS Patient Care STDS. 2016;30:155–65. doi: 10.1089/apc.2015.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Golden MR, Hogben M, Potterat JJ, Handsfield HH. HIV partner notification in the United States: a national survey of program coverage and outcomes. J Sex Transm Dis. 2004;31:709–12. doi: 10.1097/01.olq.0000145847.65523.43. [DOI] [PubMed] [Google Scholar]
- 59.Kobrak P, Ponce R, Zielony R. New arrivals to New York City: vulnerability to HIV among urban migrant young gay men. Arch Sex Behav. 2015;44:2014–53. doi: 10.1007/s10508-015-0494-4. [DOI] [PubMed] [Google Scholar]
- 60.Clark JL, Long CM, Giron JM, et al. NIMH Collaborative HIV/STD Prevention Trial. Partner notification for sexually transmitted diseases in Peru: knowledge, attitudes, and practices in a high-risk community. J Sex Transm Dis. 2007;34:309–13. doi: 10.1097/01.olq.0000240289.84094.93. [DOI] [PubMed] [Google Scholar]
- 61.Udeagu CN, Bocour A, Shah S, Ramos Y, Gutierrez R, Shephard CW. Bringing HIV partner services into the age of social media and mobile connectivity. J Sex Transm Dis. 2014;41:631–6. doi: 10.1097/OLQ.0000000000000181. [DOI] [PubMed] [Google Scholar]