Abstract
Statement of the Problem:
Temporomandibular joint disorders (TMD) may show a poor correlation between their clinical findings and radiological characteristics.
Purpose:
The aim of this study was to assess the osseous alterations of temporomandibular joint (TMJ) in symptomatic and asymptomatic subjects by employing cone beam computed tomography (CBCT) images.
Materials and Method:
In this study, CBCT images of 120 temporomandibular joints in 30 patients with TMJ disorder and 30 age- and sex-matched individuals without TMJ complaints were evaluated. Osteoarticular derangements of the joint were assessed by two experienced examiners. Data was statistically analyzed with SPSS software using chi-square test (p <0.05).
Results:
Out of 120 CBCT images (60 in each group), at least one osseous change was observed in 90% and 86.7% joints in symptomatic and asymptomatic subjects, respectively. There were no significant differences between symptomatic and asymptomatic subjects regarding frequency of osteoarticular changes including flattening (73.3% vs. 75%), irregularity (36.7% vs. 48.3%), sclerosis (20% vs. 8.3%), cyst (3.3% vs. 3.3%), erosion (13.3% vs. 21.7%), hypoplasia (3.3% vs. 5%), ankylosis (1.7% vs. Zero), osteophyte (43.3% vs. 40%), decrease joint space (3.3% vs. 3.3%), and increase joint space (5% vs. 5%). (p> 0.05)
Conclusion:
By employing CBCT as a modern diagnostic imaging tool, findings of this study revealed that the frequency of various temporomandibular joint alterations on CBCT images is comparable in patients with and without TMD complaints, suggesting that some people with TMJ structural damage may not display clinical manifestations. Moreover, CBCT imaging might not be necessary for TMD patients and more attention should be given to clinical examination.
Keywords: Temporomandibular joint , Temporomandibular joint disorder , Cone beam computed tomography
Introduction
Temporomandibular joint disorders (TMD) are a group of musculoskeletal conditions, which are considered the main cause of non-dental originated orofacial pain. These disorders comprise the second most common musculoskeletal pain condition following, low back pain.[1] Its prevalence has been reported to have a wide range from 16.3 to 68% in the adolescences[2] and up to 43% in general adult population.[3]
TMD is a disease of multifactorial origin. Studies have shown that these conditions are associated with anxiety and depression, parafunctional oral habit, poor socioeconomic level, and genetic factors.[4-5] Women are more likely to develop TMD, probably due to the influence of behavioral, hormonal, anatomic, and psychosocial causes.[6]
TMD is characterized by a various sign and symptoms directly related to the joint, which are pain or tenderness in the region of the temporomandibular joint (TMJ) and pre-auricular areas, limitation in the mouth opening, or TMJ sounds during jaw movement.[7] A variety of less-common complaints such as tinnitus, depression, otolaryngological symptoms such as hearing impairment or loss, ear plugging sensation and earache, difficulties in swallowing, and vertigo might also be present in some patients.[5,8]
Previous studies reported that a number of patients with TMJ disorders might undergo anatomical changes in bony and/or soft tissues of temporomandibular joint.[9] TMJ anatomy could be evaluated by means of various techniques including panoramic radiography, transcranial radiography, cone-beam computed tomography (CBCT), and magnetic resonance imaging (MRI).[10] CBCT is a reliable modality for the assessment of the osseous defects of the TMJ.[11] CBCT is comparable to computed tomography (CT) in accuracy, however; CBCT requires less radiation exposure and therefore is preferable to CT.[12] CBCT imaging of the TMJ can provide a lot of information about osseous changes including osteophyte, erosion, flattening, subchondral bone sclerosis, ankylosis and pseudocysts.[13]
Materials and Method
This study was conducted on the subjects who sought treatment for TMD at Oral Medicine Department of Dental School, Shiraz University of Medical Sciences and then referred to Oral Radiology Department of this school for x-ray imaging. The local Ethical Committee of Shiraz Dental School approved the protocol of study.
Thirty patients, diagnosed with TMJ disorder who met the RDC/TMD criteria, were recruited in the symptomatic (study) group.[15] These individuals were referred to the Department of Maxillofacial Radiology for treatment of TMD and they required CBCT for accurate diagnosis and further investigations. The symptomatic group included 21 females and 9 males aged 20 to 42 years (mean 33/4 years) with clinical signs and symptoms of TMD based on RCD/ TMD criteria including:
Pain or ache in the jaw, temples, face, preauricular area or inside the ear at rest or during function
Pain reported by the subject in response to palpation of three of the following muscle sites (right side and left side count as a separate sites for each muscle): posterior temporalis, middle temporalis, anterior temporalis, origin of masseter, insertion of masseter, posterior mandibular region, submandibular region, lateral pterygoid area, and tendon of the temporalis; and at least one of the painful sites must be on the same side as the complaint of pain
Pain-free unassisted mandibular opening ˂40mm
Maximum assisted opening (passive stretch) ˂ 5mm greater than pain-free unassisted opening.
Presence of click or crepitation in joints, and disc displacement with reduction and disharmonic movements of joints[15]
All participants had a full complement of permanent teeth from incisors to first molars in each quadrant, with or without third molar with normal (class I) occlusion. The asymptomatic group included 30 individuals (19 females and 11 males) who had no TMD symptoms and had negative history of occlusal or masticatory disorders. The age of the patients in the control group ranged from 15 to 34 years. Subjects in control group were referred to our department for reasons other than TMJ problems and needed CBCT imaging for indications other than TMJ disorders such as evaluating bone thickness, possible risk of fenestration, supernumerary teeth, and evaluation of the paranasal sinuses, replacing the second molars with implants, and removal of impacted wisdom teeth. TMJ area was detectable in these images and participants were matched for age and gender with symptomatic group. All subjects have voluntarily taken part in this study. They were given adequate information about the study procedures and the general aims of the study. They were reassured that their information would be kept confidential and only the results of the study would be reported without mentioning their names. After collecting informed consents from subjects or their legal guardians, physical examination and history taking were performed for all subjects by two residents under supervision of two professors to detect any pain or tenderness in TMJ, as well as in masticatory, head, and neck muscles. TMJ sounds were evaluated by using a stethoscope and recorded as no sound or clicks/crepitation. Mouth opening dysfunctions, identified by examiner or reported by the patients were recorded. Positive history of trauma, surgery or any congenital anomalies in the head and neck region, severe bruxism, attrition and generalized wear faucets on teeth were considered as exclusion criteria.
CBCT images of bilateral TMJs were taken from TMJ of both sides. Images were acquired using New Tom VGi scanner (New Tom GRsrl; Verona, Italy) with a field of view 15cm × 15cm at a 0.02mm voxel resolution with the scanning parameter of 120 kVp, 3.8 mA, and 40 seconds exposure time.The subjects were standing and were biting their teeth into maximum intercuspal position. Their heads were positioned with the Frankfurt plane parallel to the floor.
CBCT images of bilateral TMJs were taken from TMJ of both sides. Images were acquired using New Tom VGi scanner (New Tom GRsrl; Verona, Italy) with a field of view 15cm × 15cm at a 0.02mm voxel resolution with the scanning parameter of 120 kVp, 3.8 mA, and 40 seconds exposure time.The subjects were standing and were biting their teeth into maximum intercuspal position. Their heads were positioned with the Frankfurt plane parallel to the floor.
CBCT data of all participants in both groups were evaluated in axial, coronal, and sagittal sections by two expert oral radiologists; however, the authors have decided to present the sagittal images in this report for consistency. For determining the plan of reference, we used the same protocol as that of Tabrizi et al.[16] for making axial, coronal, and sagittal slices through TMJ. The axial section of the condylar process that had the widest mediolateral diameter on the left and right side condyles was chosen as the reference view. A line parallel to the long axis of the condylar process was drawn and sagittal images were reconstructed as 0.5mm slice interval and slice thickness. Both observers were blinded. Each observer evaluated the CBCT results twice with one-week interval separately. In case of disagreement, a third radiologist was asked, to help reach an agreement on final diagnosis. The images were checked for following osseous changes:
Flattening of the articular surface (a flat bony contour deviating from the convex form) (Figure 1a)
Irregularity (Figure 1b)
Sclerosis ( an area of increased density of cortical bone extending into the bone marrow) (Figure 1c)
Ely cyst (small round radiolucent area with regular margins surrounded by varying area of increased density which are deep to the articulating surfaces) (Figure 2a)
Surface erosion (an area of decreased density of the cortical bone and adjacent subcortical bone) (Figure 2b)
Condylar hypoplasia (failure of condyle to obtain normal size because of congenital and developmental abnormalities or acquired diseases that affect condylar growth) (Figure 2)
Ankylosis (intra capsular fibrous adhesions and/or fusion of the articular components by osseous mass formation)
Osteophyte (marginal bony outgrowths on the condyle) (Figure 3a)
Decreased joint space (Figure 3b) and increased joint space (increase radiolucency between condyle and temporal bone) (Figure 3c) · were also evaluated.
Figure1.
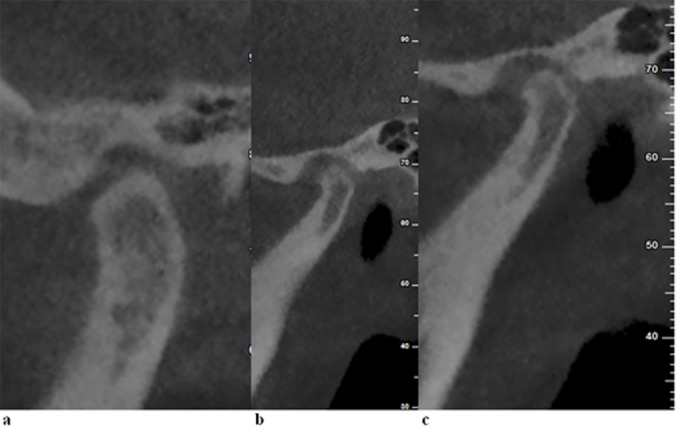
a: Flattening of the articular surface, b: Irregular TMJ space, Loss of continuity of cortex of the condyle, c: Sclerosis of cortical bone
Figure2.
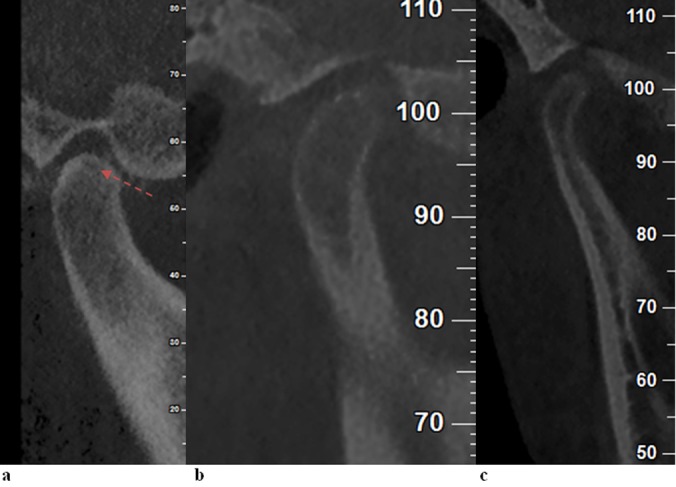
a: Ely cyst, b: Endosteal erosion, c: Condylar hypoplasia
Figure3.
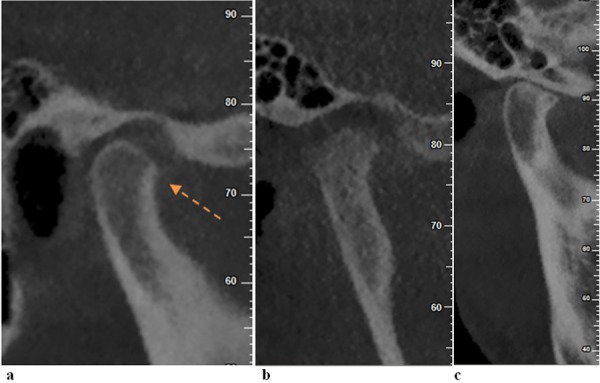
a: Osteophyte, b: Increased joint space, erosion of all aspects of the condyle, Osteophyte, c: Decreased joint space and significant osteophyte
We compared the width of the joint space with the normal range of TMJ space based on the Christiansen’s report in 1987.[17] .
The statistical analyses were performed by adopting SPSS (version 15, IBM, USA) using chi-square test to verify the differences in frequencies of joint derangements between symptomatic and asymptomatic groups. Statistical significance was set at 0.05.
Results
The study sample comprised of 9 males (30%) and 21 females (70%) in symptomatic group and 11 males (36.7%) and 19 females (63.3%) in asymptomatic group. Totally, 120 CBCT images were evaluated (60 in each group). At least one osseous change was observed in 54/60 (90%) joints of symptomatic subjects and 52/60 (86.7%) joints of asymptomatic subjects.
Table 1 summarizes the frequencies of TMJ alterations in subjects with and without complaints. The most frequently detected alteration was flattening, followed by irregularity and osteophyte in both groups. Chi-square test revealed no significant difference between symptomatic and asymptomatic groups regarding the frequency of osteoarthritic changes, including flattening (73.3% vs. 75%; p= 0.835), irregularity (36.7% vs. 48.3%; p= 0.196), sclerosis (20% vs. 8.3%; p= 0.067), cyst (3.3% vs. 3.3%; p= 1.000), erosion (13.3% vs. 21.7%; p= 0.230), hypoplasia (3.3% vs. 5%; p= 0.648), ankylosis (1.7% vs. Zero; p= 0.315), osteophyte (43.3% vs. 40%; p= 0.711), decreased joint space (3.3% vs. 3.3%; p= 1.000) and increased joint space (5% vs. 5%; p= 1.000).
Table 1.
Frequency of osseous changes in patients with TMD and asymptomatic group
| Derangement | Asymptomatic | TMD | p Value* |
|---|---|---|---|
| Flattening | 45(75%) | 44(73.3%) | 0.835 |
| Irregularity | 29(48.3%) | 22(36.7%) | 0.196 |
| Sclerosis | 5(8.3%) | 12(20%) | 0.067 |
| Cyst | 2(3.3%) | 2(3.3%) | 1.000 |
| Erosion | 13(21.7%) | 8(13.3%) | 0.230 |
| Hypoplasia | 3(5%) | 2(3.3%) | 0.648 |
| Ankylosis | 0 | 1(1.7%) | 0.315 |
| Osteophyte | 24(40%) | 26(43.3%) | 0.711 |
| Decrease joint space | 2(3.3%) | 2(3.3%) | 1.000 |
| Increase joint space | 3(5%) | 3(5%) | 1.000 |
Chi-square test
Discussion
In this study, CBCT method was used for evaluation of bony changes of TMJ. Conventional radiographs such as panoramic radiography have inadequate diagnostic validity in temporomandibular osseous alterations;[18-19] little information of bony TMJ structures might be provided by MRI;20 and CT examinations expose patients to higher doses of radiation.[12]
This study compared the incidence of TMJ alteration in patients with and without TMD-related complaints. The osseous changes were detected in 90% and 86.7% of joints in symptomatic and asymptomatic groups, respectively. In a study enrolled on children with TMJ dysfunction by Sanchez-Woodworth et al.[21] using multidirectional tomography to both joints, arthrography, computed tomography (CT), or magnetic resonance (MR) of one or both joints the frequency of alteration of the TMJ was reported in 85% of patients. Similarly, Wiberg and Wänman[22] found a high prevalence (66%) of temporomandibular joint alteration based on TMJ tomography in young patients with signs and symptoms of temporomandibular disorders. In another study performed by Price et al.,[23] the incidental findings of TMD have been reported to be 15.4% in CBCT images. MRI study on asymptomatic volunteers by Katzberg et al.[24] showed a 33% prevalence of disc displacement. Although a different imaging modality was used in that study, the reported prevalence was lower than the CBCT findings in asymptomatic group of the current study. The unequivocal accuracy of CBCT in bony changes would explain this difference.
The high frequency of bony changes in the asymptomatic group may have happened due to the unwanted selection of individuals with problems in anatomic regions close to TMJ, though they have not presented TMJ complaints. Actually, the evaluated asymptomatic subjects in our study were not a sample of normal population but patients with dental or facial disorders other than TMJ. This finding may suggest that the disorders involving such structures may be associated with the development of bony changes in TMJ. In accordance to this finding, Edwards et al.[25] reported that TMJ alterations represented 12.6% of incidental findings in CBCT of 427 orthodontic patients. Previous studies demonstrated a prevalence of 3.9% to 6.2% of TMJ changes in CBCT images of patients assessed for dental implant.[26-27] In addition, the high prevalence of bony changes among the asymptomatic group could be attributed to compensatory potential of TMJ. Since the joint encompasses various adaptive mechanisms, the structural damages may be asymptomatic or minimally apparent for a long time.[28]
Our findings highlight a similar incidence of structural alterations between symptomatic patients and asymptomatic subjects. Corresponding to our results, Okur et al.[29] evaluated the TMJ by using CT and reported no significant difference in joint space between patients with TMD complaints and asymptomatic group. Wiese et al.[30] revealed that clinical complains of patients with TMJ disorders were not associated with findings in TMJ tomograms. This shows that the results yielded by different studies, which employed different imaging modalities are consistent.
Concerning the osseous changes, no significant differences were found between TMD patients and asymptomatic groups in the current study, which employed CBCT as its diagnostic tool. This finding could emphasize that clinical manifestations of TMJ disorders display a poor correspondence to internal derangements identified in radiographic images. In line with this finding, Petersson, in a review study, stated that radiological findings of the TMJ might not constantly correlate to clinical findings in patients with TMJ disorders.[31] Moreover, Palconet et al.[32] reported a poor correlation between structural changes on CBCT images and clinical signs and symptoms in TMJ disorders. Magnusson et al.[33] in a series of panoramic radiographies corresponding to patients with TMJ disorder, reported clinically-relevant radiographic findings related to the TMJ in 25% of cases, while 11% showed relevant X-ray findings not related to TMJ disorder. In contrast, Cevidanes et al.[34] found that patients with painful TMJ had a significantly higher frequency of degenerative condylar changes compared to asymptomatic individuals.
The most frequent joint derangement in symptomatic group was flattening (73.3%) followed by osteophyte (43.3%), which was in contrast with findings of Nah et al.[35] who reported sclerosis (30.2%) and surface erosion (29.3%) as the two most frequent bony changes. Our findings and the results of these studies confirmed that a combination of physiologic and degenerative mechanism may participate in development of bony changes in TMJ, since Edwards et al.[25] notified flattening and subchondral sclerosis as physiologic remodeling, while condylar erosions and osteophyte formation as active degeneration. Osteophytes occur in advanced stages of degenerative changes when the body adjusts itself to repair the joint. Alkhader et al.[36] reported a frequency of 14% for osteophyte in CBCT of patients with TMD. Future studies with larger samples of the study would be recommended.
Conclusion
In conclusion, there is a high prevalence of bony changes visible on CBCT imaging in all subjects, with or without TMD. Findings of this study revealed that the incidence of various TMJ derangements on CBCT images were comparable between symptomatic patients with TMJ disorder and asymptomatic individuals, suggesting that CBCT imaging might not be necessary for TMD patients and more attention should be given to clinical examination.
Footnotes
Conflict of interests: None to declare.
References
- 1.Velly AM, Schiffman EL, Rindal DB, Cunha-Cruz J, Gilbert GH, Lehmann M, et al. The feasibility of a clinical trial of pain related to temporomandibular muscle and jointdisorders: the results of a survey from the Collaboration on Networked Dental and Oral Research dental practice-based research networks. J Am Dent Assoc. 2013; 144: e1–e10. doi: 10.14219/jada.archive.2013.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sena MF, Mesquita KS, Santos FR, Silva FW, Serrano KV. Prevalence of temporomandibular dysfunction in children and adolescents. Rev Paul Pediatr. 2013; 31: 538–545. doi: 10.1590/S0103-05822013000400018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adèrn B, Stenvinkel C, Sahlqvist L, Tegelberg Å. Prevalence of temporomandibular dysfunction and pain in adult general practicepatients. Acta Odontol Scand. 2014; 72: 585–590. doi: 10.3109/00016357.2013.878390. [DOI] [PubMed] [Google Scholar]
- 4.Blanco Aguilera A, Gonzalez Lopez L, Blanco Aguilera E, De la Hoz Aizpurua JL, Rodriguez Torronteras A, Segura Saint-Gerons R, et al. Relationship between self-reported sleep bruxism and pain in patients with temporomandibular disorders. J Oral Rehabil. 2014; 41: 564–572. doi: 10.1111/joor.12172. [DOI] [PubMed] [Google Scholar]
- 5.Ferendiuk E, Zajdel K, Pihut Incidence of otolaryngological symptoms in patients with temporomandibular jointdysfunctions. Biomed Res Int. 2014; 2014: 824684. doi: 10.1155/2014/824684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mazzetto MO, Rodrigues CA, Magri LV, Melchior MO, Paiva G. Severity of TMD related to age, sex and electromyographic analysis. Braz Dent J. 2014; 25: 54–58. doi: 10.1590/0103-6440201302310. [DOI] [PubMed] [Google Scholar]
- 7.Lee HS, Baek HS, Song DS, Kim HC, Kim HG, Kim BJ, et al. Effect of simultaneous therapy of arthrocentesis and occlusal splints on temporomandibular disorders: anterior disc displacement without reduction. J Korean Assoc Oral Maxillofac Surg. 2013; 39: 14–20. doi: 10.5125/jkaoms.2013.39.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weber P, Corrêa EC, Bolzan Gde, P Ferreira, Fdos S, Soares JC, Silva AM. Chewing and swallowing in young women with temporomandibular disorder. Codas. 2013; 25: 375–380. doi: 10.1590/s2317-17822013005000005. [DOI] [PubMed] [Google Scholar]
- 9.Larheim TA. Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint. Cells Tissues Organs. 2005; 180: 6–21. doi: 10.1159/000086194. [DOI] [PubMed] [Google Scholar]
- 10.Zhang ZL, Cheng JG, Li G, Shi XQ, Zhang JZ, Zhang ZY, et al. Detection accuracy of condylar bony defects in Promax 3D cone beam CT images scanned with different protocols. Dentomaxillofac Radiol. 2013; 42: 20120241. doi: 10.1259/dmfr.20120241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shetty US, Burde KN, Naikmasur VG, Sattur AP. Assessment of condylar changes in patients with temporomandibular joint pain using digital volumetric tomography. Radiol Res Pract. 2014; 2014 doi: 10.1155/2014/106059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zain-Alabdeen EH, Alsadhan RI. A comparative study of accuracy of detection of surface osseous changes in the temporomandibular joint using multidetector CT and cone beam CT. Dentomaxillofac Radiol. 2012; 41: 185–191. doi: 10.1259/dmfr/24985971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.dos Anjos Pontual ML, Freire JS, Barbosa JM, Frazão MA, dos Anjos Pontual A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac Radiol. 2012; 41: 24–29. doi: 10.1259/dmfr/17815139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cağlayan F, Tozoğlu U. Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol. 2012; 18: 159–163. doi: 10.4261/1305-3825.DIR.4341-11.2. [DOI] [PubMed] [Google Scholar]
- 15.Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112: 453–462. doi: 10.1016/j.tripleo.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Tabrizi R, Shahidi S, Bahramnejad E, Arabion H. valuation of Condylar Position after Orthognathic Surgery for Treatment of Class IIVertical Maxillary Excess and Mandibular Deficiency by Using Cone-Beam Computed Tomography. J Dent (Shiraz) 2016; 17: 318–325. [PMC free article] [PubMed] [Google Scholar]
- 17.Christiansen EL, Chan TT, Thompson JR, Hasso AN, Hinshaw DB Jr, Kopp S. Computed tomography of the normal temporomandibular joint. Scand J Dent Res. 1987; 95: 499–509. doi: 10.1111/j.1600-0722.1987.tb01966.x. [DOI] [PubMed] [Google Scholar]
- 18.Poveda-Roda R, Bagan J, Carbonell E, Margaix M. Diagnostic validity (sensitivity and specificity) of panoramic X-rays in osteoarthrosisof the temporomandibular joint. Cranio. 2015; 33: 189–194. doi: 10.1179/2151090314Y.0000000018. [DOI] [PubMed] [Google Scholar]
- 19.Imanimoghaddam M, Madani A, Talebzadeh MR, Bagherpour A, Alimohammadi M. The Relationship between Osseous Changes of the Temporomandibular Joint and RDC/TMD Groups in CBCT Images Teeth. J Dent Mater Tech. 2014; 3: 151–157. [Google Scholar]
- 20.Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009; 135: 495–501. doi: 10.1016/j.ajodo.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez-Woodworth RE, Katzberg RW, Tallents RH, Guay JA. Radiographic assessment of temporomandibular joint pain and dysfunction in the pediatric age-group. ASDC J Dent Child. 1988; 55: 278–281. [PubMed] [Google Scholar]
- 22.Wiberg B, Wänman A. Signs of osteoarthrosis of the temporomandibular joints in young patients: a clinical and radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86: 158–164. doi: 10.1016/s1079-2104(98)90118-4. [DOI] [PubMed] [Google Scholar]
- 23.Price JB, Thaw KL, Tyndall DA, Ludlow JB, Padilla RJ. Incidental findings from cone beam computed tomography of the maxillofacial region: a descriptive retrospective study. Clin Oral Implants Res. 2012; 23: 1261–1268. doi: 10.1111/j.1600-0501.2011.02299.x. [DOI] [PubMed] [Google Scholar]
- 24.Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996; 54: 147–153. doi: 10.1016/s0278-2391(96)90435-8. [DOI] [PubMed] [Google Scholar]
- 25.Edwards R, Alsufyani N, Heo G, Flores-Mir C. The frequency and nature of incidental findings in large-field cone beam computed tomography scans of an orthodontic sample. Prog Orthod. 2014; 15: 37. doi: 10.1186/s40510-014-0037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pette GA, Norkin FJ, Ganeles J, Hardigan P, Lask E, Zfaz S, et al. Incidental findings from a retrospective study of 318 cone beam computed tomography consultation reports. Int J Oral Maxillofac Implants. 2012; 27: 595–603. [PubMed] [Google Scholar]
- 27.Allareddy V, Vincent SD, Hellstein JW, Qian F, Smoker WR, Ruprecht A. Incidental findings on cone beam computed tomography images. Int J Dent. 2012; 2012: 871532. doi: 10.1155/2012/871532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Molinari F, Manicone PF, Raffaelli L, Raffaelli R, Pirronti T, Bonomo L. Temporomandibular joint soft-tissue pathology, I: Disc abnormalities. Semin Ultrasound CT MR. 2007; 28: 192–204. doi: 10.1053/j.sult.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Okur A, Ozkiris M, Kapusuz Z, Karaçavus S, Saydam L. Characteristics of articular fossa and condyle in patients with temporomandibular joint complaint. Eur Rev Med Pharmacol Sci. 2012; 16: 2131–2135. [PubMed] [Google Scholar]
- 30.Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A, et al. Association between temporomandibular joint symptoms, signs, and clinicaldiagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain. 2008; 22: 239–251. [PubMed] [Google Scholar]
- 31.Petersson A. What you can and cannot see in TMJ imaging--an overview related to the RDC/TMD diagnostic system. J Oral Rehabil. 2010; 37: 771–778. doi: 10.1111/j.1365-2842.2010.02108.x. [DOI] [PubMed] [Google Scholar]
- 32.Palconet G, Ludlow JB, Tyndall DA, Lim PF. Correlating cone beam CT results with temporomandibular joint pain of osteoarthriticorigin. Dentomaxillofac Radiol. 2012; 41: 126–130. doi: 10.1259/dmfr/60489374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magnusson T, Karlsson C. Clinical impact of radiological examinations of patients with suspectedtemporomandibular disorders. Swed Dent J. 2002; 26: 67–74. [PubMed] [Google Scholar]
- 34.Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110: 110–117. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nah KS. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012; 42: 249–253. doi: 10.5624/isd.2012.42.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alkhader M, Ohbayashi N, Tetsumura A, Nakamura S, Okochi K, Momin MA, et al. Diagnostic performance of magnetic resonance imaging for detecting osseousabnormalities of the temporomandibular joint and its correlation with cone beam computed tomography. Dentomaxillofac Radiol. 2010; 39: 270–276. doi: 10.1259/dmfr/25151578. [DOI] [PMC free article] [PubMed] [Google Scholar]


