Abstract
Background
The present study aimed to report the outcomes of acute and subacute arthroscopic bony Bankart repairs in collision athletes.
Methods
We reviewed 22 consecutive rugby players with traumatic anterior glenohumeral instability who underwent arthroscopic bony Bankart repair within 4 months of injury over a 2-year period. All lesions were less than 25% of the glenoid bony area.
Results
A significant improvement was noted at three months and was maintained at 28 months postoperatively. The mean Constant score improved from 61.5 to 84.1, the mean Oxford shoulder score decreased from 26.3 to 13.6 and the mean Oxford instability score decreased from 42.9 to 13.5. The mean satisfaction score was 8.3 out of 10 at final follow-up. All patients returned to their pre-injury sporting level. Twenty patients (91%) remained stable and asymptomatic, although two (9%) had recurrent instability after further traumatic sports injuries. One required a modified Latarjet procedure, whereas the other patient sustained a soft tissue Bankart lesion and had a revision arthroscopic repair.
Conclusions
Acute and sub-acute bony Bankart lesions in collision athletes can be addressed through arthroscopic repair with a satisfactory outcome and return to pre-injury level of sport
Keywords: arthroscopic bony Bankart, athlete, bony Bankart, collision, rugby
Introduction
A Bankart lesion is the avulsion of the antero-inferior capsule and labrum from the glenoid rim and is usually associated with a traumatic anterior glenohumeral dislocation in a young population.1,2 A traumatic anterior glenohumeral dislocation may also be associated with an avulsion fracture of the anterior glenoid rim. This is known as a bony Bankart lesion and the amount of bone loss is an important factor in recurrent glenohumeral instability.2–5
Bony defects of the glenoid rim with associated anterior instability have raised concerns about the efficacy of arthroscopic treatment. Previous reports have suggested that bone defects are not suitable for arthroscopic stabilization.6 If an arthroscopic stabilization is conducted without addressing these bony defects recurrent instability may persist.3,4,5–7
Several studies8–12 have described arthroscopic reduction and stabilization of bony Bankart lesions with satisfactory results in noncollision athletes, suggesting that bony Bankart lesions <25% of the glenoid surface can be treated using suture anchors, although there are no reports on the outcome of arthroscopic bony Bankart repair in collision athletes. The purpose of the present study was to evaluate the results and functional outcomes of the arthroscopic treatment of bony Bankart lesions with anterior glenoid bony defect of less than 25% in collision athletes. We hypothesized that arthroscopic bony Bankart repair can provide satisfactory outcomes in a high-level collision athletes.
Materials and methods
Clinical evaluation
We examined the operating records of the senior author and identified 22 collision athletes who had undergone arthroscopic stabilization of a bony Bankart lesion over a 2-year period. The inclusion criteria were collision athletes undergoing surgical repair who had sustained a single event subluxation or dislocation with a bony Bankart less than 25% of the glenoid and with minimum follow-up of 2 years. The reasons for this were based on the outcomes of Porcelain et al.13 who showed that bony Bankart repairs performed in less than 3 months after injury had a significantly lower recurrence rate than those performed more than 3 months after injury. Exclusion criteria were surgery more than 3 months after injury (patients were treated with a Latarjet procedure primarily in such cases), a bony Bankart more than 25% of the glenoid6 (primary repair if acute; Latarjet procedure if longer than 3 months since injury), patients with soft-tissue Bankart lesions, and patients with an associated nerve injury. Three patients were excluded because of co-existing nerve injury. Patients were evaluated using the Constant shoulder score,14 Oxford shoulder score15 and the Oxford instability score.16 Patient satisfaction was rated from 0 to 10. All patient data were collected and handled according to institutional guidelines.
Radiological evaluation
Plain radiographs were taken in anteroposterior and axillary views in all the cases. In six patients, ultrasound was performed by the senior author in office if a rotator cuff tear was suspected. All patients had a magnetic resonance imaging (MRI) arthrogram, with specific sequences to highlight bony lesions. Images were produced to provide en face views of the glenoid, allowing measurements. The bony lesions and glenoid bone loss was measured on the sagital-oblique and axial sequences. The bone loss was assessed on pre-operative compujted tomography (CT) or MRI to determine whether it was less than 25% of the glenoid using the method of Griffith et al.17 Postoperatively, anteroposterior and axillary view radiographs were taken at 3 weeks, 3 months and 1 year postoperatively. An additional CT scan was obtained for three patients to assess bony union.
Examination under anaesthesia
Shoulders were evaluated in the operating room after the administration of the general anaesthetic and intrascalene block. The range of movement and the stability of the shoulder were assessed. As described by Cofield et al.,18 translation was graded as grade 0 if there was no translation; grade I if translation was up to the glenoid rim; grade II translation was beyond glenoid rim but with spontaneous reduction; and grade III translation was beyond glenoid rim without spontaneous reduction.
Operative rechnique
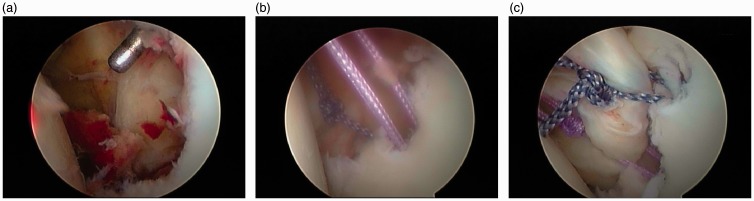
All of the operations were performed as outpatient procedures. The operative technique described by Sugaya et al.12 was used, with suture anchors above and below the bony lesion. Additional suture anchors were added as necessary. Biodegradable anchors and high-strength sutures were used in all cases (Fig. 1).
Figure 1.
Serial arthroscopic images of a representative left shoulder (posterior viewing portal) showing a large displaced bony Bankart lesion (a) and the suture-anchor repair (b, c), using the technique described.
Postoperative rehabilitation
Postoperatively, the patients underwent a sports-specific rehabilitation programme developed by the senior author in conjunction with professional rugby clubs. It is based on functional goals and incorporates early sports-specific exercises, with a safe progression through each phase of rehabilitation. A sling immobilizer was used for comfort only. Active assisted range of motion is commenced immediately postoperatively in the safe zone as determined at surgery. Closed chain exercises are also started immediately postoperatively, including isometrics. Progression to active range of motion exercises was determined by patient comfort and ease, without forcing or pushing the range. This was usually achievable by 4 weeks. Open chain exercises and progression of light resistance exercises was introduced under strict supervision once active range was easy and comfortable. Sports specific exercises within a safe range were also introduced within the first 4 weeks. Simulated falling and drop-bag tackling started once strength was 75% to 80% of the opposite side or pre-injury and almost full active range of motion achieved. Progression and return to play was based on satisfactory rehabilitation progression including a strength of over 80% compared to pre-injury, successful tackle training, falls training, wrestling and skills assessment.
Statistical analysis
Statistical analysis was performed using Medcalc, version 10.1 (Medcalc, Mariakerke, Belgium). Differences between the pre-operative and postoperative Constant, Oxford Shoulder and Oxford Instability Scores were analyzed with the Mann–Whitney U-test (p < 0.05).
Results
The mean follow-up was 28 months (range 24 months to 35 months). Table 1 shows the patient demographics. The mean time from injury to surgery was 1.7 months (range 0.2 months to 3.1 months). Two patients had a previous history of previous open Bankart repair and one had a previous superior labral anterior posterior tear (SLAP) repair of the same shoulder. All patients had antero-inferior instability and eight patients had pain. None were able to play.
Table 1.
Clinical details of the patients (n = 22 patients).
| Clinical features | |
|---|---|
| Mean age (range) | 29.7 years (17 years to 66 years) |
| Sex (%) | 21 Male (95%) |
| 1 Female (5%) | |
| Dominant arm (%) | 10 (45%) |
| Level of sport participation (%) | 13 Professional (59%) |
| 9 Recreational (41%) |
Findings of the examination under anesthesia and diagnostic arthroscopy lesions are shown in Tables 2 and 3, respectively. Hill–Sachs lesions19 were not engaging in any of these cases and were small (with an average of less than 3 mm in depth and 2 cm in diameter). All of the SLAP tears were type II, according to Snyder’s classification.20 All of these associated lesions were repaired arthroscopically at the same time.
Table 2.
Findings during the examination under anaesthesia for the 22 patients.
| Finding | Number of patients |
|---|---|
| Anterior translation | |
| Grade I | 2 |
| Grade II | 2 |
| Grade III | 5 |
| Posterior translation | |
| Grade I | 0 |
| Grade II | 0 |
| Grade III | 1 |
| Multi-directional laxity | |
| With sulcus | 1 |
| Without sulcus | 8 |
Table 3.
Associated injuries identified during arthroscopic assessment of the 22 patients.
| Pathological finding | Number of patients |
|---|---|
| Hill–Sachs lesion | 15 |
| Reverse Hill–Sachs lesion | 1 |
| Posterior labral tear | 8 |
| SLAP tear | 7 |
| PASTA lesion | 2 |
| Full-thickness rotator cuff tear | 1 |
| Biceps tear | 1 |
SLAP, superior labral anterior posterior tear; PASTA, partial articular supraspinatus tendon avulsion.
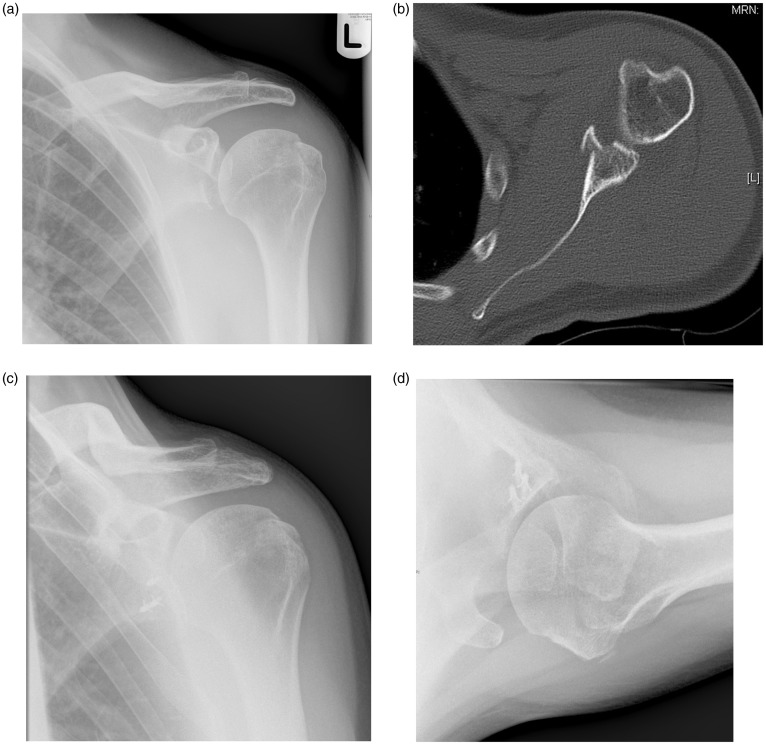
At final review, the patient satisfaction score was 8.3 (range 7 to 10) out of 10. All of the patients regained full range of motion at 6 months and 21 (95%) of the patients had returned to their previous level of activity that time. Figure 2 shows an example of the pre-operative and postoperative radiographs of the bony Bankart repair.
Figure 2.
(a, b) Pre-operative radiograph and representative axial computed tomography slice showing a large displaced bony Bankart lesion. (c, d) Postoperative radiographs at 6 months showing the lesion reduced and healed.
Outcome scores are presented in Table 4. A significant improvement was noticed in the Constant Score and in the Oxford Instability Score at 3 months (p = 0.02 and 0.03, respectively). The Oxford Shoulder Score had improved significantly at six months (p = 0.01). These improvements were maintained for the Constant Score (p = 0.05), the Oxford Shoulder Score (p = 0.001) and the Oxford Instability Score (p = 0.0001) at 18 months. No significant difference was observed between the professional and recreational collision athletes with respect to their final Constant Score (p = 0.8), Oxford Shoulder Score (p = 0.41) or the Oxford Instability Score (p = 0.3).
Table 4.
Functional scores for the 22 patients.
| Assessment | Constant Score | Oxford Shoulder Score | Oxford Instability Score |
|---|---|---|---|
| Pre-operatively | 61.5 (46.1 to 77.0) | 26.3 (18.0 to 34.6) | 42.9 (36.7 to 49.0) |
| Pre-operatively 3 months | 83.1 (74.0 to 92.1) | 20.2 (15.9 to 24.4) | 22.3 (9.6 to 23.6) |
| Pre-operatively 6 months | 80.7 (64.2 to 97.2) | 18.5 (13.7 to 23.2) | 26.0 (13.2 to 38.7) |
| Final review | 84.1 (71.0 to 96.9) | 13.6 (9.1 to 18.0) | 13.5 (9.7 to 17.2) |
All scores are mean values with the 95% confidence intervals. Higher scores are favourable with the Constant Score, whereas lower scores are favourable with the Oxford scores.
Our recurrent instability rate (defined as subluxation or dislocation) was 9% (2 of 22). Two patients had a significant re-injury during play less than 12 months after surgery. One professional had a re-tear of the anterior labrum and associated type II SLAP tear 11 months after surgery, which was repaired arthroscopically. The previous bony repair was intact and the patient remained asymptomatic afterwards. Another professional player had a large recurrent bony Bankart lesion with glenoid deficiency 8 months after surgery. This may have been the result of incomplete union of the initial fixation, although the recurrent bony injury appeared larger and related to cystic changes of the PLLA [poly(l)lactic acid] anchors. A modified Laterjet procedure was performed and he returned to international rugby. A third patient, an amateur player, had a re-injury during a rugby tackle 16 months after surgery. His shoulder remained stable, with normal imaging. He did not require further surgical treatment and returned to sport.
Discussion
The importance of glenoid rim osseous defects in shoulder stability is known.2–7,10,21 The prevalence of bony Bankart lesions in recurrent shoulder instability is reported as high as 50%.10,22 Although some report failure of delayed arthroscopic treatment in the presence of established bone loss,3,6 repair of acute or sub-acute bony Bankart lesions have been more successful.8–12,23 Various arthroscopic techniques show promise for successful treatment of bony Bankart lesions.9,13,22–24 Furthermore, a histological analysis of the bone fragment by Fuji et al.25 has shown that the fragment seemed to be viable and could be used to treat the defect, showing that mobilization and fixation of these lesions can produce good results.
Reported rates of recurrence of instability after surgical treatment in noncollision athletes have included 3% at 4 years of follow-up in 65 patients,23 5% in 42 patients at a mean follow-up of 34 months,10 and 9.5% recurrent subluxation and 4.8% re-dislocation rates in 21 patients at a mean follow-up of 34 months.8 Although our instability rate was 9% within 12 months of surgery, both of these patients sustained a further traumatic event. This is consistent with the recurrence rate and mechanism seen in collision athletes treated with open stabilization.26 By contrast, in a prior series by Burkhart and De Beer,6 the collision athletes with bone loss leading to an inverted pear-shaped glenoid, the recurrence rate was 89% after open Bankart repair, leading to the recommendation of coracoid transfer. Other recent series such as Larrain et al.27 address arthroscopic reconstruction in collision athletes but include a mixed group of acute and chronic instability and do not clearly identify the results in the group of athletes with bone defects under 25% of the glenoid.
Similar to those reports that include pre-operative shoulder scores, the functional improvement in this series of patients is significant. Porcellini et al.13 reported a change in Rowe score from 59 points to 92 points, whereas Sugaya et al.10 reported a change in Rowe score from 34 points to 94 points. Although this series used different outcome measures, a similar substantial improvement was observed. All of the athletes in our series returned to sport at their pre-injury level of play compared to 84% in the series by Sugaya et al.10
The strengths of the present study include uniform surgical technique, pre- and postoperative scoring with validated instruments, and a clearly-defined patient population. Limitations include a small cohort and medium-term follow-up. A longer-term clinical follow-up is required to determine how the procedure performs in this challenging patient group. We also acknowledge other important factors in surgical decision-making in athletes, such as time of season, position, level of participation and joint laxity, as well as surgeon and facility factors. These should be included in the shared surgical decision-making process with the athlete.
Conclusions
Acute and sub-acute bony Bankart lesions in collision athletes can be addressed through arthroscopic repair of the bony fragment with capsulo-ligamentous complex and can produce a satisfactory functional outcome and return to pre-injury level of sport.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
All patients sign consent forms to agree to the use of their anonymized data for scientific and research purposes. The return of the questionnaire was further confirmation of implied consent.
References
- 1.Bankart AS. Recurrent or habitual dislocation of the shoulder-joint. Br Med J 1923; 2: 1132–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair: apparent causes of failure and treatment. J Bone Joint Surg Am 1984; 66: 159–168. [PubMed] [Google Scholar]
- 3.Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med 1998; 26: 41–45. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006; 88: 1755–1763. [DOI] [PubMed] [Google Scholar]
- 5.Tauber M, Resch H, Forstner R, Raffl M, Schauer J. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg 2004; 13: 279–285. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill–Sachs lesion. Arthroscopy 2000; 16: 677–694. [DOI] [PubMed] [Google Scholar]
- 7.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on antero-inferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000; 82: 35–46. [DOI] [PubMed] [Google Scholar]
- 8.Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with an inverted pear glenoid. Results in patients with bone loss of the anterior glenoid. Am J Sports Med 2007; 35: 1276–1283. [DOI] [PubMed] [Google Scholar]
- 9.Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy 2002; 18: 764–769. [DOI] [PubMed] [Google Scholar]
- 10.Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am 2005; 87: 1752–1760. [DOI] [PubMed] [Google Scholar]
- 11.Sugaya H, Kon Y, Tsuchiya A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy 2005; 21: 635–635. [DOI] [PubMed] [Google Scholar]
- 12.Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. Surgical technique. J Bone Joint Surg Am 2006; 88(Suppl 1): 159–169. [DOI] [PubMed] [Google Scholar]
- 13.Porcellini G, Paladini P, Campi F, Paganelli M. Long-term outcome of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med 2007; 35: 2067–2072. [DOI] [PubMed] [Google Scholar]
- 14.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin. Orthop 1987; 214: 160–164. [PubMed] [Google Scholar]
- 15.Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996; 78: 593–600. [PubMed] [Google Scholar]
- 16.Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br 1999; 81: 420–426. [DOI] [PubMed] [Google Scholar]
- 17.Griffith JF, Antonio GE, Tong CWC, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. Am J Roent 2003; 180: 1423–1430. [DOI] [PubMed] [Google Scholar]
- 18.Cofield RH, Nessler JP, Weinstabl R. Diagnosis of shoulder instability by examination under anesthesia. Clin Orthop Relat Res 1993; 291: 45–53. [PubMed] [Google Scholar]
- 19.Hill HA, Sachs MD. The grooved defect of the humeral head: a frequently unrecognized complication of dislocations of the shoulder joint. Radiology 1940; 35: 690–700. [Google Scholar]
- 20.Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy 1990; 6: 274–279. [DOI] [PubMed] [Google Scholar]
- 21.Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy 2004; 20: 169–174. [DOI] [PubMed] [Google Scholar]
- 22.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003; 85: 878–884. [DOI] [PubMed] [Google Scholar]
- 23.Cameron SE. Arthroscopic reduction and internal fixation of an anterior glenoid fracture. Arthroscopy 1998; 14: 743–746. [DOI] [PubMed] [Google Scholar]
- 24.Wilson F, Hinov V, Adams G. Arthroscopic repair for anterior shoulder instability with a Bigliani type I glenoid rim fracture. Arthroscopy 2002; 18: E32–E32. [DOI] [PubMed] [Google Scholar]
- 25.Fujii Y, Yoneda M, Wakitani S, Hayashida K. Histologic analysis of bony Bankart lesions in recurrent anterior instability of the shoulder. J Shoulder Elbow Surg 2006; 15: 218–223. [DOI] [PubMed] [Google Scholar]
- 26.Fabre T, Abi-Chahla ML, Billaud A, Geneste M, Durandeau A. Long-term results with Bankart procedure: a 26-year follow-up study of 50 cases. J Shoulder Elbow Surg 2010; 19: 318–323. [DOI] [PubMed] [Google Scholar]
- 27.Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavon F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy 2006; 22: 1283–1289. [DOI] [PubMed] [Google Scholar]