Abstract
The coexistence of acetabular dysplasia (AD) and femoroacetabular impingement (FAI) has not been well discussed. This study was performed to elucidate the prevalence and morphological features of AD with coexisting FAI-related findings in a Japanese population. Computed tomography images were retrospectively evaluated. AD was classified as definite or borderline. The morphological findings that defined cam deformity were an α angle of ≥55°, head–neck offset ratio (HNOR) of <0.13, pistol grip deformity positivity and herniation pit positivity. The morphological findings that defined pincer deformity were acetabular index of ≤0° and a retroverted acetabulum. In total, 128 hips (male, 64; female, 64) were analyzed. The prevalence of coexistence of AD and FAI-related findings was detected in 23.4% of hips (definite AD and FAI, 7.8%; borderline AD and FAI, 15.6%). The percentages of hips with AD containing cam or pincer deformities among all were 54.3% and 4.3%, respectively. The percentage of AD with coexisting cam and that of AD with coexisting combined deformities was significantly higher in men, respectively. On the other hand, the most major morphological feature of FAI detected in hips with AD was a HNOR of <0.13. The coexistence of AD and FAI-related findings was common in a Japanese population, and 65.2% of hips with AD had some FAI-related findings. In discussing and managing AD, we recommend paying attention to the coexistence with FAI-related findings, especially in men and in borderline AD. In such hips, the most notable parameter as a morphological feature of FAI is a reduced HNOR.
INTRODUCTION
Acetabular dysplasia (AD) is a well-recognized cause of osteoarthritis (OA) of the hip [1]. In Japan, AD is a major risk factor for OA [2], and the prevalence of AD is higher in Japanese than in Western populations [3]. Furthermore, definite AD and borderline AD are often distinguished in the clinical setting [4, 5]. Femoroacetabular impingement (FAI) has also been highlighted, and an association between FAI and hip OA has been identified [6, 7]. FAI has been thought to be divided into four categories: cam deformity, pincer deformity, combined deformities and sports impingement, where a hip with normal anatomy impinges in extreme positions in sporting activity.
The anatomical abnormalities associated with AD and FAI have been discussed as independent anatomical features. Several recent reports have described the coexistence of AD and FAI-related findings in patients with symptomatic AD or FAI [8–11]. However, the prevalence and morphological features of the coexistence of AD (especially borderline AD) and FAI-related findings are not well known in Japanese populations who are generally assumed to have AD rather than Western populations. The aim of this study was to investigate the detailed prevalence and morphological features of AD with coexisting FAI-related findings using multislice computed tomography (CT) images in a Japanese population.
MATERIALS AND METHODS
Patients and parameters
The ethics committee of our institution approved the study protocol. We conducted a retrospective patient-based study of patients who had undergone CT imaging of the chest, abdomen and pelvis. We reviewed all CT data from 1 July 2013–14 August 2013 in our institution. First, we selected the scans that had been ordered by other departments at our institution and confirmed that the CT examination had been performed for conditions unrelated to hip disorders based on the information in the clinical record. Next, we selected 65 consecutive patients irrespective of sex who fulfilled the criteria described below. The inclusion criteria for the present study were as follows: (1) involvement of the whole pelvis and both hip joints, (2) reconstructed axial slice thickness of ≤1 mm and (3) normal pelvic rotations and tilt (specified below in the section describing standardization of CT images). The exclusion criteria were as follows: (1) age of <20 years, (2) inability to clearly detect the center of the femoral head, such as in patients with an elliptical femoral head and (3) inability to correctly measure the parameters, such as clear hip OA that had the osteophyte formation, the loss of joint space and subchondral bone cysts [12].
Both hips were analyzed in each patient. Two male hips were excluded because of a metaphyseal bone tumor in each. As a result, 128 hips (64 male hips and 64 female hips) were evaluated. The examined parameters and findings were age, sex, center-edge (CE) angle [13], Sharp angle [14], acetabular index (AI) [15], acetabular version angle [16], α angle [17], head–neck offset ratio (HNOR) [18], herniation pit (HP) [19] and pistol grip deformity (PGD) [20, 21].
CE angle, Sharp angle and AI were measured on a slice of the femoral head center in the coronal plane (Fig. 1). The acetabular anteversion angle was measured in four axial slices (Fig. 2). We defined an acetabulum with a negative acetabular anteversion angle in any slice (A1, A2, A3 or A4) as a retroverted acetabulum (RA) [22]. RA of these slices was representing crossover sign positive on plain radiograph. The α angle and HNOR were measured in multiple radial slices, namely clockwise system, using previously described methods [23–25] (Fig. 3). We defined an HP as a cystic-like lesion underneath the anterior cortex at the anterosuperior femoral head–neck junction with a clear demarcation [26] and a diameter of >3 mm [27] (Fig. 4). HP was evaluated at the above-described multiradial slices. The presence of a PGD was subjectively determined using reconstructed three-dimensional CT images (Fig. 5). AD was classified into definite AD and borderline AD. Definite AD was defined as a CE angle of <20° or a Sharp angle of >45°. Borderline AD was defined as a CE angle of 20° to <25° or a Sharp angle of >42° to 45° (hips already defined as definite AD were excluded). We investigated the prevalence of these morphological findings and then determined the prevalence of AD with coexisting radiological FAI. FAI was classified into cam and pincer deformities. Cam deformity was defined as an α angle of ≥55° [28], HP positivity [29], PGD positivity [29] or an HNOR of <0.13 [28]. Pincer deformity was defined as AI of ≤0° [29] or the presence of an RA. Hips with both cam and pincer deformities were considered to have a combined deformity. Prevalence was defined as the proportion of hips that fulfilled a specific definition among all of the hips in this study.
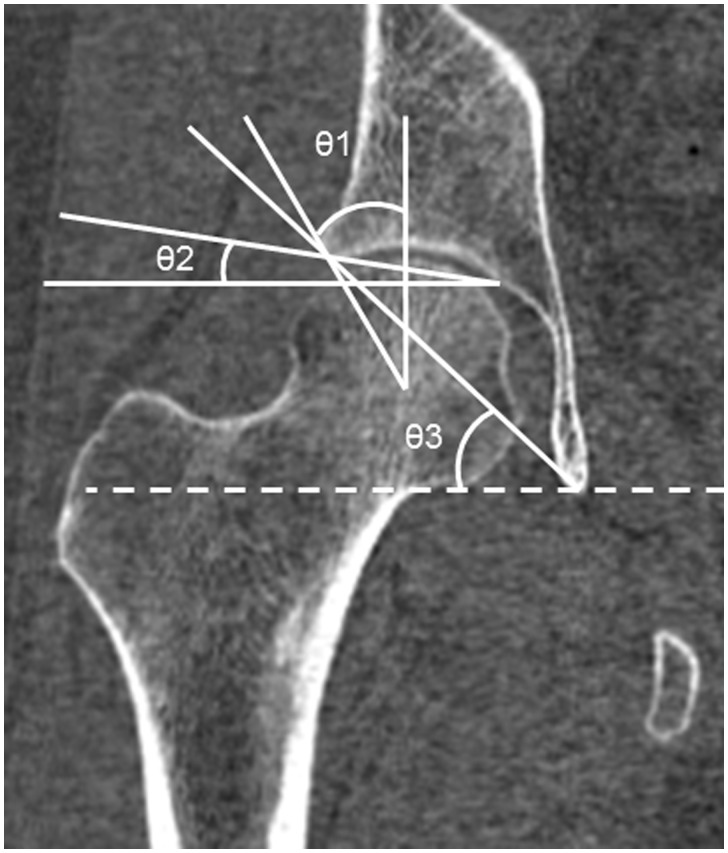
Fig. 1.
Measurement of CE angle, Sharp angle and AI. These angles were measured on a slice of femoral head center in the coronal plane. θ1, θ2, and θ3 is CE angle, Sharp angle and AI, respectively. CE angle was measured as the angle between the line joining the lateral aspect of the acetabulum and the femoral head center, and the line perpendicular to the line parallel to the transverse axis of the pelvis. Sharp angle was measured as the angle between the line joining the lateral aspect of the weight bearing zone and the inferior point of teardrop, and the line parallel to the transverse axis of the pelvis. AI was measured as the angle between the line joining the medial and lateral aspects of the weight bearing zone, and the line parallel to the transverse axis of the pelvis.
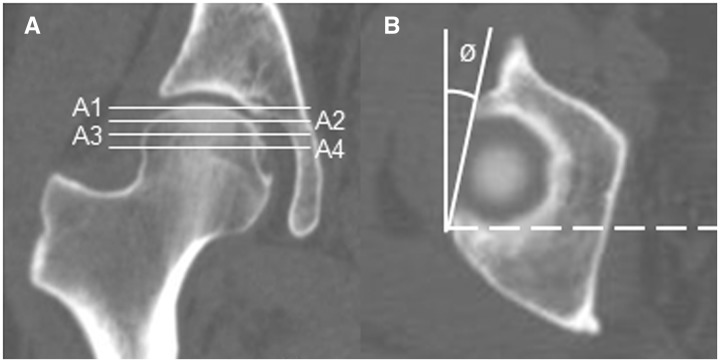
Fig. 2.
Measurement of the acetabular version angle in four axial slices. (A) Reference plane for measuring the acetabular version angle. Each line represents one of the four slices; a slice at the level of the superior margin of the femoral head (slice A1), a slice 5 mm below the superior margin of the femoral head (slice A2), a slice 10 mm below the superior margin of the femoral head (slice A3) and a slice 15 mm below the superior margin of the femoral head (slice A4). (B) Axial slice of A1. Angle ø is the acetabular version angle.
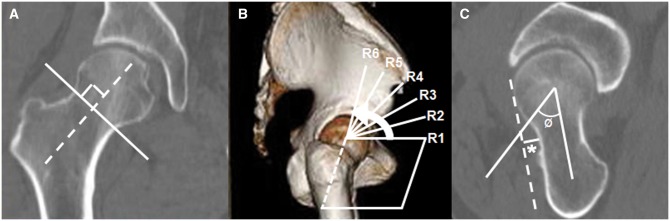
Fig. 3.
Measurement of the α-angle and HNOR in multiple radial slices (clockwise system). (A) Reference plane for measuring the α-angle and HNOR. The dotted line is the axis through the center of the femoral neck. It is adjusted to be parallel to the femoral neck–shaft angle. The solid line is the reference plane for radial angle reconstruction. (B) The reconstructed three-dimensional image demonstrates superimposed radial reference lines at 15° intervals. R1 (3:00 o’clock) is the oblique axial slice (dotted line in A). R2 (2:30 o’clock) is a plane rotated 15° from R1. R3 (2:00 o’clock) is a plane rotated 30° from R1. R4 (1:30 o’clock) is a plane rotated 45° from R1. R5 (1:00 o’clock) is a plane rotated 60° from R1. R6 (12:30 o’clock) is a plane rotated 75° from R1. (C) Angle ø is the α-angle. The α-angle is the angle between the line joining the center of the femoral head and the center of the femoral neck, and the line from the center of the femoral head to the point where the spherical image of the femoral head is lost. The HNOR was calculated by dividing the anterior offset (asterisk) by the maximum diameter of the femoral head of each slice. The anterior offset is the thickness of the femoral head that lies anterior to a line passing the anterior wall of the femoral neck that is parallel to a line crossing the center of the femoral head and neck.
Fig. 4.
We defined an HP as a cystic-like lesion underneath the anterior cortex at the anterosuperior femoral head–neck junction with clear demarcation and a diameter of >3 mm. A HP (arrow) was evaluated in multiradial six slices.
Fig. 5.
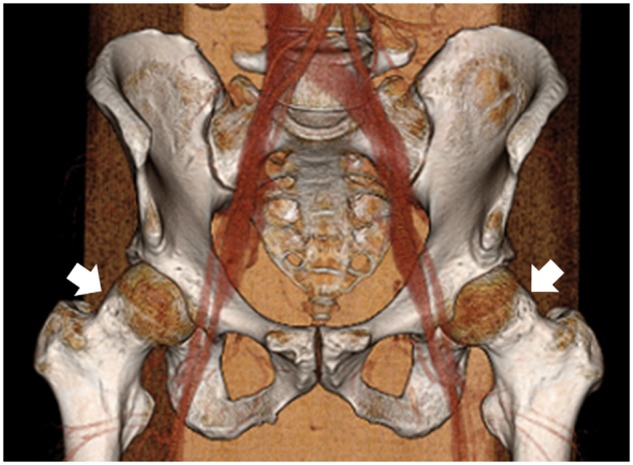
The presence of a PGD was subjectively judged on reconstructed three-dimensional reconstructed computed tomography images. This case was judged to be PGD-positive bilaterally (arrow).
Radiological examination and standardization of CT images
All CT images were axial and sequential and were obtained in the supine position without gantry tilt (120 kV, 160 mA, 0.5 s) using a Toshiba Aquilion CX (Toshiba Medical Systems Corporation, Tokyo, Japan). The data were reconstructed under conditions suitable for bone evaluation using AquariusNet Viewer software (TeraRecon Inc., San Francisco, CA, USA). We used the three-dimensional reconstructed CT images to confirm the pelvic rotation and tilt. We confirmed (1) the rotation in the coronal plane (confirmed whether the teardrop line was horizontal), (2) the rotation in the axial plane (examined whether any horizontal distance was present between the tip of the coccyx and the pubic symphysis [30]) and (3) the neutral pelvic tilt (investigated the distance between the upper border of the symphysis and the midportion of the sacrococcygeal joint, as described previously [29, 30]). In this study, 32 mm ± 10 mm in men and 47 ± 10 mm in women were considered neutral [30].
Statistical methods
Data are expressed as mean ± standard deviation. All statistical analyses were performed using StatView version 5.0 (SAS Institute, Cary, NC, USA). The significance of differences between men and women was evaluated using the Wilcoxon rank-sum test and χ2 test. Values of P < 0.05 were considered to indicate statistical significance. The 95% confidence interval (CI) was estimated based on the score test for prevalences. To evaluate the intraobserver reliability and interobserver reliability between the two observers (senior orthopedic surgeons) who were blinded to the each other’s results, the intraclass correlation coefficients (ICCs) of the CE angle, Sharp angle, AI, acetabular version angle, α angle and HNOR were evaluated using SPSS statistics 22.0 for Windows (IBM Corp., Armonk, NY, USA) at least 2 weeks apart. Observer agreement was considered unacceptable if the value was less than 0.40, moderate if the value was 0.41–0.60, substantial if the value was 0.61–0.80, and almost perfect if the value was greater than 0.80.
RESULTS
Table I shows the mean age and parameters of all patients and of men and women. Table II shows the prevalence of each type of AD and FAI-related findings in all patients, men and women. Overall, AD was detected in 35.9% of hips (46/128) [29.7% (19/64) in men, 42.2% (27/64) in women; P = 0.140] (data not shown). A total of 76.6% of hips (98/128) met at least one criterion of the definition of cam or pincer deformity [89.1% (57/64) in men, 64.1% (41/64) in women; P < 0.001] (data not shown).
Table I.
Mean age and data for each parameter in all patients, men and women
| All subjects (128 hips) | Males (64 hips) | Females (64 hips) | P-value | |
|---|---|---|---|---|
| Age (years) | 56.3±15.8 (21–84) | 57.2±16.1(21–83) | 55.5±15.48 (31–84) | 0.520* |
| CE angle (°) | 31.6±7.0 (15.4–47.8) | 32.3±6.5 (17.6–45.7) | 30.9±7.3 (15.4–47.8) | 0.315* |
| Sharp angle (°) | 40.1 ± 6.9 (31.8–54.8) | 39.3 ± 4.1 (31.8–54.8) | 40.9 ± 3.3 (31.9–49.1) | 0.003* |
| Acetabular index (°) | 6.7±9.2 (−7.9–22.8) | 6.6±11.3 (−7.5–22.8) | 6.8±6.4 (−7.9–22.3) | 0.195* |
| Acetabular version | ||||
| A1 (°) | 9.0±8.6 (−14.9–31.3) | 7.8±9.9 (−7.2–29.0) | 10.3±8.8 (−14.9–31.3) | 0.043* |
| A2 (°) | 12.0±9.0 (−10.6–34.0) | 9.9±8.6 (−7.5–34.0) | 14.0±8.8 (−10.6–32.7) | 0.003* |
| A3 (°) | 16.7±8.7 (−7.5–33.4) | 15.1±8.1 (−1.3–33.3) | 18.2±9.1 (−7.5–33.4) | 0.025* |
| A4 (°) | 19.6±7.8 (−3.8–35.6) | 18.2±6.8 (1.51–35.6) | 20.9±8.5 (−3.8–35.6) | 0.030* |
| α-angle | ||||
| R1 (°) | 40.3±5.1 (21.6–55.0) | 41.6±5.0 (30.5–55.0) | 39.0±5.0 (21.6–48.7) | 0.011* |
| R2 (°) | 42.8±5.7 (30.8–60.3) | 44.0±6.1 (30.8–60.3) | 41.7±4.9 (31.6–52.9) | 0.025* |
| R3 (°) | 46.0±5.9 (32.3–64.6) | 46.9±6.5 (32.3–64.6) | 45.0±5.1 (33.9–58.2) | 0.130* |
| R4 (°) | 48.5±5.9 (35.9–68.6) | 49.0±6.5 (35.9–68.6) | 47.9±5.2 (39.2–63.9) | 0.413* |
| R5 (°) | 49.0±6.9 (34.7–75.0) | 51.4±7.0 (39.2–75.0) | 47.7±5.9 (34.7–72.1) | <0.001* |
| R6 (°) | 46.9±7.4 (33.1–74.7) | 49.5±7.4 (34.1–74.7) | 44.3±4.9 (33.1–53.7) | <0.001* |
| HNOR | ||||
| R1 | 0.245±0.03 (0.159–0.371) | 0.243±0.03 (0.159–0.333) | 0.248±0.04 (0.165–0.371) | 0.504* |
| R2 | 0.241±0.07 (0.123–0.349) | 0.245±0.09 (0.123–0.305) | 0.236±0.04 (0.156–0.349) | 0.784* |
| R3 | 0.205±0.04 (0.080–0.336) | 0.211±0.05 (0.080–0.307) | 0.200±0.04 (0.115–0.336) | 0.099* |
| R4 | 0.167±0.05 (0.036–0.323) | 0.165±0.05 (0.036–0.306) | 0.168±0.04 (0.113–0.323) | 0.628* |
| R5 | 0.140±0.03 (0.054–0.270) | 0.136±0.03 (0.057–0.248) | 0.145±0.03 (0.054–0.270) | 0.113* |
| R6 | 0.141±0.03 (0.056–0.263) | 0.132±0.03 (0.056–0.191) | 0.150±0.03 (0.065–0.263) | 0.002* |
| HP positive | 17.2% (10.6%–23.7%) | 24.6% (17.14%–32.06%) | 9.2% (6.65%–11.75%) | 0.019† |
| PGD positive | 14.0% (7.98%–20.01%) | 20.0% (13.07%–26.92%) | 12.3% (17.32%–28.68%) | 0.041† |
Data are presented as mean ± standard deviation (range) or as percentage (95% CI). CE angle, center-edge angle; HNOR, head–neck offset ratio; HP, herniation pit; PGD, pistol grip deformity. A1, axial slice at the level of the superior margin of the femoral head; A2, axial slice 5 mm below the superior margin of the femoral head; A3, axial slice 10 mm below the superior margin of the femoral head; A4, axial slice 15 mm below the superior margin of the femoral head; R1, oblique axial plane through the center of the femoral neck, adjusted to be parallel to the femoral neck–shaft angle (3:00 o’clock); R2, radial plane cranially rotated 15° from R1 (2:30 o’clock); R3, radial plane cranially rotated 30° from R1 (2:00 o’clock); R4, radial plane cranially rotated 45° from R1 (1: 30 o’clock); R5, radial plane cranially rotated 60° from R1 (1: 00 o’clock); R6, radial plane cranially rotated 75° from R1 (12:30 o’clock).
Male versus female, evaluated with the Wilcoxon rank-sum test. P-values of <0.05 were considered statistically significant.
Male versus female, evaluated with χ2 test. P-values of <0.05 were considered statistically significant.
Table II.
Detailed prevalence of AD and FAI-related findings in all patients, men, and women
| All subjects (128 hips) | Males (64 hips) | Females (64 hips) | P-value* | |
|---|---|---|---|---|
| Definite AD | ||||
| CE angle <20° | 6.3% (8/128) | 3.1% (2/64) | 9.4% (6/64) | 0.144 |
| [3.2%–11.8%] | [0.9%–10.7%] | [4.4%–19.0%] | ||
| Sharp angle >45° | 7.8% (10/128) | 6.3% (4/64) | 9.4% (6/64) | 0.439 |
| [4.3%–13.8%] | [2.5%–15.0%] | [4.4%–19.0%] | ||
| Total | 11.7% (15/128) | 7.8% (5/64) | 15.6% (10/64) | 0.169 |
| [7.2%–18.4%] | [3.4%–17.0%] | [8.7%–26.4%] | ||
| Borderline AD | ||||
| 20°≤ CE angle <25° | 12.5% (16/128) | 12.5% (8/64) | 12.5% (8/64) | 1 |
| [7.8%–19.3%] | [6.5%–22.8%] | [6.5%–22.8%] | ||
| 42°< Sharp angle ≤45° | 21.9% (28/128) | 15.6% (10/64) | 28.1% (18/64) | 0.087 |
| [15.6%–29.8%] | [8.7%–26.4%] | [18.6%–40.1%] | ||
| Total | 24.2% (31/128) | 21.9% (14/64) | 26.6% (17/64) | 0.536 |
| [17.6%–32.3%] | [13.5%–33.4%] | [17.3%–38.5%] | ||
| Cam deformity | ||||
| α angle ≥55° | 28.9% (37/128) | 40.6% (26/64) | 17.2% (11/64) | 0.003 |
| [21.8%–37.3%] | [29.5%–52.9%] | [9.9%–28.2%] | ||
| HNOR <0.13 | 58.6% (75/128) | 65.6% (42/64) | 51.6% (33/64) | 0.106 |
| [49.9%–66.9%] | [53.4%–76.1%] | [39.6%–63.4%] | ||
| PGD positive | 14.1% (18/128) | 20.3% (13/64) | 7.8% (5/64) | 0.041 |
| [9.1%–21.1%] | [12.3%–31.7%] | [3.4%–17.0%] | ||
| HP positive | 17.2% (22/128) | 25.0% (16/64) | 9.4% (6/64) | 0.016 |
| [11.6%–24.7%] | [16.0%–36.8%] | [4.4%–19.0%] | ||
| Total | 68.0% (87/128) | 79.7% (51/64) | 56.3% (36/64) | 0.004 |
| [59.5%–75.4%] | [68.3%–87.7%] | [44.1%–67.7%] | ||
| Pincer deformity | ||||
| Acetabular index ≤0° | 18.0% (23/128) | 20.3% (13/64) | 15.6% (10/64) | 0.489 |
| [12.3%–25.5%] | [12.3%–31.7%] | [8.7%–26.4%] | ||
| RA | 12.5% (16/128) | 17.2% (11/64) | 7.8% (5/64) | 0.108 |
| [7.8%–19.3%] | [9.9%–28.2%] | [3.4%–17.0%] | ||
| Total | 28.9% (37/128) | 37.5% (24/64) | 20.3% (13/64) | 0.031 |
| [21.8%–37.3%] | [26.7%–49.7%] | [12.3%–31.7%] | ||
| Combined deformity | 20.3% (26/128) | 28.1% (18/64) | 12.5% (8/64) | 0.028 |
| [14.3%–28.1%] | [18.6%–40.1%] | [6.5%–22.8%] | ||
Data are shown as percentage [95% CI]. AD, acetabular dysplasia; FAI, femoroacetabular impingement; CE, center-edge angle; PGD, pistol grip deformity; HP, herniation pit; HNOR, head–neck offset ratio; RA, retroverted acetabulum.
Male versus female, evaluated with χ2 test. P-values of <0.05 were considered statistically significant.
Table III shows the prevalence of each combination of the coexistence of AD and FAI-related deformities. Figure 6 was the representative case of definite AD with coexisting cam deformity. The prevalence of borderline AD with coexisting FAI (15.6%, 20/128) was times higher than that of definite AD with coexisting FAI (7.8%, 10/128). Altogether, the coexistence of AD and any type of FAI-related deformity was detected in 23.4% (30/128) of all hips. The prevalence of AD with a coexisting cam deformity was higher than that of AD with a coexisting pincer deformity regardless of sex. No significant difference was observed in any combination of AD and FAI-related deformity between men and women.
Table III.
Prevalence of each combination of coexistence of AD and FAI-related deformities
| All subjects (128 hips) | Males (64 hips) | Females (64 hips) | P-value* | |
|---|---|---|---|---|
| Definite AD and FAI-related deformities | 7.8% (10/128) | 7.8% (5/64) | 7.8% (5/64) | 1 |
| [4.3%–13.8%] | [3.4%–17.0%] | [3.4%–17.0%] | ||
| Definite AD + cam deformity | 6.3% (8/128) | 4.7% (3/64) | 7.8% (5/64) | 0.465 |
| [3.2%–11.8%] | [1.6%–12.9%] | [3.4%–17.0%] | ||
| Definite AD + pincer deformity | 0% (0/128) | 0% (0/64) | 0% (0/64) | – |
| [0%–2.9%] | [0%–5.7%] | [0%–5.7%] | ||
| Definite AD + combined deformity | 1.6% (2/128) | 3.1% (2/64) | 0% (0/64) | 0.154 |
| [0.4%–5.5%] | [0.9%–10.7%] | [0%–5.7%] | ||
| Borderline AD and FAI-related deformities | 15.6% (20/128) [10.3%–22.9%] | 20.3% (13/64) [12.3%–31.7%] | 10.9% (7/64) [5.4%–20.9%] | 0.144 |
| Borderline AD + cam deformity | 13.3% (17/128) [8.5%–20.2%] | 17.2% (11/64) [9.9%–28.2%] | 9.4% (6/64) [4.4%–19.0%] | 0.193 |
| Borderline AD + pincer deformity | 1.6% (2/128) | 1.6% (1/64) | 1.6% (1/64) | 1 |
| [0.4%–5.5%] | [0.3%–8.3%] | [0.3%–8.3%] | ||
| Borderline AD + combined deformity | 0.8% (1/128) | 1.6% (1/64) | 0% (0/64) | 0.315 |
| [0.1%–4.3%] | [0.3%–8.3%] | [0%–5.7%] | ||
| AD in total (definite and borderline) and FAI-related deformities | 23.4% (30/128) | 28.1% (18/64) | 18.7% (12/64) | 0.210 |
| [16.9%–31.5%] | [18.6%–40.1%] | [11.1%–30.0%] | ||
| AD in total (definite and borderline) + cam deformity | 19.5% (25/128) | 21.9% (14/64) | 17.2% (11/64) | 0.504 |
| [13.6%–27.2%] | [13.5%–33.4%] | [9.9%–28.2%] | ||
| AD in total (definite and borderline) + pincer deformity | 1.6% (2/128) | 1.6% (1/64) | 1.6% (1/64) | 1 |
| [0.4%–5.5%] | [0.3%–8.3%] | [0.3%–8.3%] | ||
| AD in total (definite and borderline) + combined deformity | 2.3% (3/128) | 4.7% (3/64) | 0% (0/64) | 0.079 |
| [0.8%–6.7%] | [1.6%–12.9%] | [0%–5.7%] |
Data are shown as percentage [95% CI]. AD, acetabular dysplasia; FAI, femoroacetabular impingement.
Male versus female, evaluated with χ2 test. P-values of <0.05 were considered statistically significant.
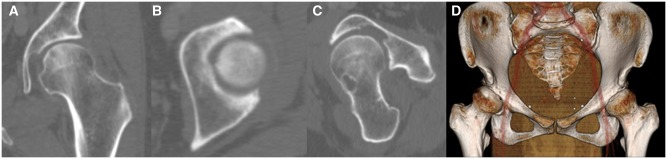
Fig. 6.
The representative case of the hip of AD with coexisting FAI-related findings. This case was 50 years old women, left hip was defined as a hip of borderline AD with coexisting cam deformity. (A) CE angle, Sharp angle and AI was 21°, 44° and 20°, respectively. (B) The acetabular version angle was 7° at a slice at the level of the superior margin of the femoral head (slice A1). (C) The α-angle and HNOR at a slice of R4 (1:30 o’clock) was 57° and 0.125, respectively. HP was also positive. (D) PGD was negative. According to the CE and Sharp angle, this hip was defined as a borderline AD. On the other hand, this hip was also defined as a cam deformity due to α-angle > 55°, HNOR < 0.13 and HP positive. However, this hip did not coexist with a pincer deformity, because the AI was over 0° and acetabular version angle was not negative.
Table IV shows the percentage of each type of AD with coexisting cam, pincer and combined deformities compared with total AD (definite and borderline). The percentage of AD with a coexisting cam deformity (54.3%, 25/46) was much higher than that of AD with coexisting pincer (4.3%, 2/46). The percentage of AD without coexisting FAI-related findings was 34.8% (16/46); in other words, 65.2% of hips (30/46) with AD had some FAI-related findings.
Table IV.
Corresponding percentage of each type of AD with coexisting cam, pincer and combined deformities and without coexisting FAI-related findings compared with all numbers of each type of AD in all patients
| With coexisting cam deformity | With coexisting pincer deformity | With coexisting combined deformity | Without coexisting FAI-related findings | |
|---|---|---|---|---|
| Definite AD (n = 15) | 53.3% (8/15) | 0% (0/15) | 13.3% (2/15) | 33.3% (5/15) |
| [30.1%–75.2%] | [0%–20.4%] | [3.7%–37.9%] | [15.2%–58.3%] | |
| Borderline AD (n = 31) | 54.8% (17/31) | 6.5% (2/31) | 3.2% (1/31) | 35.5% (11/31) |
| [37.8%–70.8%] | [1.8%–20.7%] | [0.6%–16.2%] | [21.1%–53.1%] | |
| AD in total (definite and borderline) (n = 46) | 54.3% (25/46) | 4.3% (2/46) | 6.5% (3/46) | 34.8% (16/46) |
| [40.2%–67.8%] | [1.2%–14.5%] | [2.2%–17.5%] | [22.7%–49.2%] |
Data are shown as percentage [95% CI]. AD, acetabular dysplasia; FAI, femoroacetabular impingement.
Table V shows the detailed percentage of each type of AD with coexisting cam, pincer and combined deformities in men and women compared with total AD. There was no combination of AD and FAI-related findings which showed that the corresponding percentage in women was higher than that in men. The percentages of total AD with a coexisting cam deformity and total AD with a coexisting combined deformity were significantly higher in men than women (P = 0.0272 and P = 0.0327, respectively). Conversely, the percentages of total AD without coexisting FAI-related findings were significantly higher in women (P = 0.0004).
Table V.
Comparison of corresponding percentage of AD with coexisting cam, pincer and combined deformities and without coexisting FAI-related findings compared with all numbers of each type of AD between men and women
| With coexisting cam deformity | With coexisting pincer deformity | With coexisting combined deformity | Without coexisting FAI-related findings | |||||
|---|---|---|---|---|---|---|---|---|
| Definite AD (n = 5 in male, n = 10 in female) | Male | Female | Male | Female | Male | Female | Male | Female |
| 60% (3/5) | 50% (5/10) | 0% (0/5) | 0% (0/10) | 40% (2/5) | 0% (0/10) | 0%(0/5) | 50%(5/10) | |
| [23.1%–88.2%] | [23.7%–76.3%] | [0%–43.4%] | [0%–27.8%] | [11.8%–76.9%] | [0%–27.8%] | [0%–43.3%] | [23.7%–76.3%] | |
| −P=0.7144− | − | −P=0.0317− | −P=0.0528− | |||||
| Borderline AD (n = 14 in male, n = 17 in female) | Male | Female | Male | Female | Male | Female | Male | Female |
| 78.6% (11/14) | 35.3% (6/17) | 7.1% (1/14) | 5.9% (1/17) | 7.1% (1/14) | 0% (0/17) | 7.1% (1/14) | 58.8% (10/17) | |
| [52.4%–92.4%] | [17.3%–58.7%] | [1.3%–31.5%] | [1.0%–27.0%] | [1.3%–31.5%] | [0%–18.4%] | [1.3%–31.5%] | [36.0%–78.4%] | |
| −P=0.0032− | −P=0.8869− | −P=0.3113− | −P=0.00276− | |||||
| AD in total (n = 19 in male, n = 27 in female) | Male | Female | Male | Female | Male | Female | Male | Female |
| 73.7% (14/19) | 40.7% (11/27) | 5.3% (1/19) | 3.7% (1/27) | 15.8% (3/19) | 0% (0/27) | 5.3% (1/19) | 55.6% (15/27) | |
| [51.2%–88.2%] | [24.5%–59.3%] | [0.9%–24.6%] | [0.7%–18.3%] | [5.5%–37.6%] | [0%–12.5%] | [0.9%–24.6%] | [37.3%–72.4%] | |
| −P=0.0272− | −P=0.7984− | −P=0.0327− | −P=0.0004− | |||||
Data are shown as percentage [95% CI]. AD, acetabular dysplasia; FAI, femoroacetabular impingement. P values were evaluated with the χ2 test. P values of <0.05 were considered statistically significant.
Table VI shows the corresponding percentages of the combinations of the coexistence of each type of AD and each FAI-related finding compared with all hips. The most major features of cam deformities coexisting with definite AD and borderline AD were an HNOR of <0.13. On the other hand, the major feature of pincer deformities coexisting with definite AD and borderline AD were RA. No significant differences were found in the corresponding percentages of the coexistence of each type of AD and each FAI-related finding between men and women.
Table VI.
Corresponding percentage of combination of coexistence with each type of AD and each FAI-related finding compared with all hips with coexistence of each type of AD (definite or borderline) and each FAI-related deformity (cam or pincer deformity)
| All subjects | Males | Females | P-value* | |
|---|---|---|---|---|
| Definite AD + cam deformity | ||||
| Definite AD + α angle ≥55° | 40% (4/10) | 40.0% (2/5) | 40.0% (2/5) | 1 |
| [16.8%–68.7%] | [11.8%–76.9%] | [11.8%–76.9%] | ||
| Definite AD + HNOR < 0.13 | 100% (10/10) | 100% (5/5) | 100% (5/5) | – |
| [72.2%–100%] | [56.6%–100%] | [56.6%–100%] | ||
| Definite AD + PGD positive | 10% (1/10) | 20% (1/5) | 0% (0/5) | 0.292 |
| [1.8%–40.4%] | [3.6%–62.4%] | [0%–43.3%] | ||
| Definite AD + HP positive | 20% (2/10) | 20% (1/5) | 20% (1/5) | 1 |
| [5.7%–51.0%] | [3.6%–62.4%] | [3.6%–62.4%] | ||
| Definite AD + pincer deformity | ||||
| Definite AD + acetabular index ≤0° | 0% (0/2) | 0% (0/2) | (0/0) | – |
| [0%–65.8%] | [0%–65.8%] | |||
| Definite AD + RA | 100% (2/2) | 100% (2/2) | (0/0) | – |
| [34.2%–100%] | [34.2%–100%] | |||
| Borderline AD + cam deformity | ||||
| Borderline AD + α angle ≥55° | 55.6% (10/18) | 41.7% (5/12) | 83.3% (5/6) | 0.094 |
| [33.7%–75.4%] | [19.3%–68.0%] | [43.6%–97.0%] | ||
| Borderline AD + HNOR < 0.13 | 88.9% (16/18) | 83.3% (10/12) | 100% (6/6) | 0.249 |
| [67.2%–96.9%] | [55.2%–95.3%] | [61.0%–100%] | ||
| Borderline AD + PGD positive | 27.8% (5/18) | 25.0% (3/12) | 33.3% (2/6) | 0.709 |
| [12.5%–50.9%] | [8.9%–53.2%] | [9.7%–70.0%] | ||
| Borderline AD + HP positive | 22.2% (4/18) | 33.3% (4/12) | 0% (0/6) | 0.109 |
| [9.0%–45.2%] | [13.8%–60.9%] | [0%–39.0%] | ||
| Borderline AD + pincer deformity | ||||
| Borderline AD + acetabular index ≤0° | 33.3% (1/3) | 0% (0/2) | 100% (1/1) | 0.083 |
| [6.1%–79.2%] | [0%–65.8%] | [20.7%–100%] | ||
| Borderline AD + RA | 66.7% (2/3) | 100% (2/2) | 0% (0/1) | 0.083 |
| [20.8%–93.9%] | [34.2%–100%] | [0%–79.3%] | ||
Data are shown as percentage [95% CI]. AD, acetabular dysplasia; FAI, femoroacetabular impingement; PGD, pistol grip deformity; HP, herniation pit; HNOR, head–neck offset ratio; RA, retroverted acetabulum.
Male versus female, evaluated with χ2 test. P-values of <0.05 were considered statistically significant.
The ICCs of the intraobserver and interobserver reliability of all parameters were almost perfect (≥0.80).
DISCUSSION
AD and FAI have been thoroughly discussed as a cause of hip OA [1, 2, 6, 7]. However, the prevalence and morphological features of the coexistence of AD and FAI have not been well discussed. In the present study, we showed the prevalence of AD with coexisting pincer, cam and combined deformities, and also the frequency with which FAI-related findings coexist with definite and borderline AD in asymptomatic Japanese population. To the best of our knowledge, there is scarce literature on this topic.
Several authors have discussed the coexistence of cam deformity and AD in symptomatic populations. Ida et al. [9] reported the frequency of cam deformity in hips with symptomatic AD. They found that 40% of patients with AD had radiological evidence of cam deformity (α angle of >55°) on lateral roentgenograms. On the other hand, Clohisy et al. [8] found that femoral head asphericity was present in 72% and reduced head–neck offset was also presented in 75% of symptomatic AD. Furthermore, Wyles et al. [11] reported that patients with coexisting AD and cam deformity developed hip OA more rapidly rather than patients with AD. From this study, we are agreed to these previous reports showed the high prevalence of coexistence of AD and cam-related findings, and clinical importance of them. However, previous studies have evaluated the coexistence of AD and cam-related findings only using simple plain radiographs. In the present study, we revealed the coexistence of several FAI-related findings and AD (including borderline) using multislice CT images and also compared the results between men and women. We emphasized the prevalence of borderline AD with coexisting cam deformity was 15.6%, which was two times higher than that of definite AD with coexisting cam deformity. Therefore, we consider that more attention should be given to the coexistence of borderline AD and cam deformity. Furthermore, the percentage of hips with AD and a coexisting cam deformity was significantly higher in men than women. Therefore, we also suppose that more attention should be given to the coexistence of AD and cam deformity especially in men. Additionally, we showed that the most major feature of cam-related findings detected in definite and borderline AD in Japanese hips was reduced HNOR.
The percentage of hips with definite AD with coexisting pincer-related findings compared with all hips with definite AD was 0%, and the prevalence of borderline AD with coexisting pincer-related findings compared with all hips with borderline AD was only 6.5%. Fujii et al. [10] reported that an RA was observed in 18% of Japanese patients with symptomatic AD. They showed that AD with an RA was associated with an earlier onset of pain than AD with anteversion. However, Troelsen et al. [31] reported that an RA was found in one-third of hips with AD when assessed on weight-bearing pelvic radiographs. They also reported that the prevalence of an RA may be underestimated if the evaluated images are obtained from patients in the supine position. Therefore, we might have underestimated the coexistence of AD and pincer-related findings in the present study because we used CT images and excluded the pelvis anteriorly rotated rather than normal range from present study. Although the percentage of AD with coexisting pincer deformity was lower than that of AD with coexisting cam deformity, we had better understand that the coexistence of pincer deformity in men was slightly higher than that in women. In such hips, we should pay more attention to a RA as a morphological finding of pincer deformity.
We employed two parameters for the definition of AD in the present study. As a result, we detected definite AD in 11.7% of the Japanese hip joints in this study, which is relatively higher than in previous Asian studies based on plain radiograph examination (Inoue et al. [3], 8.1%; Umer et al. [32], 7.3%). However, direct comparison of our results with their results is difficult because the evaluation methods were different. We recognize that these angles showed discrepancy between CT images and plain radiographs. Actually, Chadayammuri et al. [33] reported discrepancies in the CE angle between plain radiographs and CT images. They found that the CE angle measured on CT images was 2.1° larger than that of measured on plain radiographs. Considering these facts, our results might overestimate the prevalence of AD rather than the studies that measured these parameters using plain radiograph. However, we believe that CT images are more suitable than plain radiographs with respect to correct measurement of AD parameters because we can more easily detect the bony morphological features of the acetabulum, especially the lateral point of the acetabular dome, and we can also accurately evaluate the acetabular bony coverage in the center of the femoral head. Furthermore, the ICCs for the interobserver reliability of the CE angle and Sharp angle were 0.83 and 0.94 in this study, respectively. Mast et al. [34] and Tan et al. [35] reported that the ICCs for the interobserver reliability of the CE angle evaluated on plain radiographs were 0.73 and 0.51, respectively. We believe that CT images allow for calculation of a more accurate prevalence of AD than do plain radiographs.
In the present study, we defined a CE angle of <20° as indicative of definite AD and a CE angle of 20° to <25° as indicative of borderline AD. These cut-off values have been widely utilized in the literature [4, 5]. We also defined a Sharp angle of >45° as indicative of definite AD and a Sharp angle of >42° to 45° as indicative of borderline AD. A Sharp angle of >45° has been widely used to define the presence of definite AD in the literature [5]. However, few reports have described the cut-off of Sharp angle for the definition of borderline AD. Paliobeis and Villar [4] reported that a Sharp angle of >39° to 42° was indicative of borderline AD and that a Sharp angle of >42° was indicative of definite AD. If we had used these definitions in the present study, the prevalence of borderline AD as diagnosed by a Sharp angle of >39° to 42° would have been 28.9%, and that of definite AD as diagnosed by a Sharp angle of >42° would have been 29.7%; the prevalence of total AD would have been 58.6%. However, these prevalences are much higher than those defined using the CE angle in our study and much higher than the previously reported prevalences of definite AD [3, 32]. Sharp [14] originally reported that angles of 39°–42° were within the upper limit of normality. Therefore, we defined a Sharp angle of >45° as indicative of definite AD and a Sharp angle of >42° to 45° as indicative of borderline AD in the present study. On the other hand, we did not define AD using AI in the present study. Namely, we did not distinguish between ‘flat roof (short roof) dysplasia’ and ‘sloping roof dysplasia’ [36, 37]. Brockwell et al. [36] suggested that a sloping roof dysplasia was so-called primary dysplasia or classical dysplasia which has instability and a flat roof dysplasia was essentially taking with cam impingement. They described that a flat roof dysplasia was brought by the impingement between iliac acetabular epiphysis and cam deformity in adolescence. In the present study, we did not discuss these morphologies of AD. If we classified and discussed these morphologies of AD, we believed that the results would be different.
This study has some limitations. First, it was not population-based, but patient-based. This is an inescapable limitation of this study. However, our aim in this study was not to simply investigate the prevalence of AD with coexisting radiological FAI but to evaluate its prevalence using detailed multislice and multiplane examinations. Therefore, we investigated the patients’ CT images from scans that had been requested by other departments at our institution for evaluation of conditions unrelated to hip disorders. Second, we excluded clear hip OA in order to precisely measure morphological parameters. We understand that AD and FAI are generally thought to be lead to hip OA. Therefore, we recognized that this might lead to potential selection bias and an underestimation of the prevalence of AD or FAI. Third, the sample size was relatively small, and this study was performed in a single hospital. We recognize that it might be incorrect to generalize our results to region throughout Japan. Finally, we employed four parameters to define cam deformity, and we employed two parameters to define pincer deformity. We recognize that the prevalence of AD with coexisting FAI-related findings would be different if we had employed other parameters for definition of FAI-related deformities or altered the number of parameters used to define cam or pincer deformity. For example, a HP is generally thought to be a predictor of FAI [29, 25]. However, Kim et al. [27] indicate that a HP may have limited significance as a predictor of FAI. Furthermore, α angle would be naturally more than 55°, if PGD was existed. Therefore, we supposed that the results would be different, if HP and PGD positivity were excluded as a parameter from cam deformity. And then we recalculated the results in that situation. As a result, a total of 74.2% of hips met at least one criterion of the definition of cam or pincer deformity, and the prevalence of coexistence of AD and FAI-related findings was estimated in 22.6% of hips (definite AD and FAI, 7.8%; borderline AD and FAI, 14.8%). And then, 63.0% of the hips with AD had some FAI-related findings. In this manner, the prevalence and other percentages did not generally change, if HP and PGD positivity were excluded from the parameter of cam deformity.
Although, AD and FAI were originally independent concepts, we consider that simultaneous evaluation of AD and FAI would be informative from the viewpoint of preventing the progression of hip OA. Actually, we found that only 34.8% of hips with AD were free from the coexistence of FAI-related findings when we investigated AD using multislice CT images in Japan. Furthermore, we revealed that the major and notable parameter of a cam deformity detected in hips with AD was a HNOR. We consider that it is important to correctly evaluate the coexistence of AD and radiological FAI-related findings when discussing morphological disorders of the hip joint. However, it still remains unclear what additional procedure (debridement, labral fixation or osteochodroplasty of cam lesion) is needed and suitable when we perform acetabular osteotomy for AD with coexisting FAI [38]. Further research will be needed to indicate how to manage FAI-related findings coexisting with AD.
In conclusion, we found that the coexistence of AD and FAI-related findings was common in Japanese population, and 65.2% of hips with AD had some FAI-related findings. The prevalence of borderline AD with coexisting FAI was much higher than that of definite AD with coexisting FAI, and the percentage of AD with coexisting FAI-related findings in men was higher rather than that in women. We also found that AD with coexisting cam-related findings was considerably more common than AD with coexisting pincer-related findings, and the most notable parameter as a morphological feature of cam deformity detected in such hips was a HNOR.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Murphy SB, Ganz R, Muller ME.. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict outcome. J Bone Joint Surg Am 1995. Jul; 77: 985–9. [DOI] [PubMed] [Google Scholar]
- 2. Takeyama A, Naito M, Shiramizu K, Kiyama T.. Prevalance of femoroacetabular impingement in Asian patients with osteoarthritis of the hip. Int Orthop 2009. Oct; 33: 1229–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Inoue K, Wicart P, Kawasaki T. et al. Prevalence of hip osteoarthritis and acetabular dysplasia in French and Japanese adults. Rheumatology (Oxford) 2000; 39: 745–8. [DOI] [PubMed] [Google Scholar]
- 4. Paliobeis CP, Villar RN.. The prevalence of dysplasia and femoroacetabular impingement. Hip Int 2011 Mar–Apr; 21: 141–5. [DOI] [PubMed] [Google Scholar]
- 5. Jacobsen S. Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology. Acta Orthop Suppl 2006; 77: 1–37. [PubMed] [Google Scholar]
- 6. Jäger M, Wild A, Westhoff B, Krauspe R.. Femoroacetabular impingement coursed by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci 2004; 9: 256–63. [DOI] [PubMed] [Google Scholar]
- 7. Agricola R, Waarsing JH, Arden NK. et al. Cam impingement of the hip: a risk for hip osteoarthritis. Nat Rev Rheumatol 2013; 9: 630–4. [DOI] [PubMed] [Google Scholar]
- 8. Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL.. Incidence and characteristics of femoral head deformities in the dysplastic hip. Clin Orthop Relat Res 2009; 467: 128–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ida T, Nakamura Y, Hagio T, Naito M.. Prevalence and characteristics of cam-type femoroacetabular deformity in 100 hips with symptomatic acetabular dysplasia: a case control study. J Orthop Surg Res 2014; 9: 93.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fujii M, Nakashima Y, Yamamoto T. et al. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am 2010; 92: 895–903. [DOI] [PubMed] [Google Scholar]
- 11. Wyles CC, Heidenreich MJ, Jeng J. et al. The John Charnley Award; redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orhop Relat Res 2017; 475: 336–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lepage-Saucier M, Thiery C, Larbi A. et al. Femoroacetabular impingement: normal values of the quantitative morphometric parameters in asymptomatic hips. Eur Radiol 2014; 24: 1707–14. [DOI] [PubMed] [Google Scholar]
- 13. Wiberg G. Studies on dysplastic acetabulum and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand 1939; 83(Suppl. 58): 33. [Google Scholar]
- 14. Sharp IK. Acetabular dysplasia.The acetabular angle. J Bone Joint Surg Br 1961; 43: 268–72. [Google Scholar]
- 15. Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag, 1987: 120p [Google Scholar]
- 16. Perreira AC, Hunter JC, Laird T, Jamali AA.. Multilevel measurement of acetabular version using 3-D CT-generated models: implications for hip preservation surgery. Clin Orthop Relat Res 2011; 469: 552–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nötzli HP, Wyss TF, Stoecklin CH. et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84: 556–60. [DOI] [PubMed] [Google Scholar]
- 18. Eijer H, Leunig M, Mahomed N, Ganz R.. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int 2001; 11: 37–41. [Google Scholar]
- 19. Pitt MJ, Graham AR, Shipman JH, Birkby W.. Herniation pit of the femoral neck. AJR Roentgenol 1982; 138: 1115–21. [DOI] [PubMed] [Google Scholar]
- 20. Stulberg SD, Cordell LD, Harris WH. et al. Unrecognised childhood disease: a major cause of idiopathic osteoarthritis of the hip. The Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby; 1975: 212.
- 21. Harris WH. Aetiology of osteoarthritis of the hip. Clin Orthop Relat Res 1986. Dec; 213: 20–33. [PubMed] [Google Scholar]
- 22. Reynolds D, Lucas J, Klaue K.. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 1999; 81: 281–8. [DOI] [PubMed] [Google Scholar]
- 23. Rakhra KS, Sheikh AM, Allen D, Beaulé PE.. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res 2009; 467: 660–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mimura T, Kawasaki T, Itakura S. et al. Prevalence of radiological femoroacetabular impingement in Japanese hip joints: detailed investigation with computed tomography. J Orthop Sci 2015; 20: 649–56. [DOI] [PubMed] [Google Scholar]
- 25. Mimura T, Mori K, Itakura S. et al. Prevalence of pincer, cam, and combined deformities in Japanese hip joints evaluated with the Japanese Hip Society diagnostic guideline for femoroacetabular impingement: a CT-based study. J Orthop Sci 2017; 22: 105–11. [DOI] [PubMed] [Google Scholar]
- 26. Panzer S, Esch U, Abdulazim AN, Augat P.. Herniation pits and cystic-appearing lesions at the anterior femoral neck: an anatomical study by MSCT and maicroCT. Skeletal Radiol 2010; 39: 645–54. [DOI] [PubMed] [Google Scholar]
- 27. Kim JA, Park JS, Jin W, Ryu K.. Herniation pits in the femoral neck: a radiological indicator of femoroacetabular impingement. Skeletal Radiol 2011; 40: 167–72. [DOI] [PubMed] [Google Scholar]
- 28. Van Houcke J, Yan WP, Yan CH. et al. Prevalence of radiographic parameters predisposing to femoroacetabular impingement in young asymptomatic Chinese and white subjects. J Bone Joint Am 2015; 97: 310–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tannast M, Siebenrock KA, Anderson SE.. Femoroacetabular impingement: radiographic diagnosis: what the radiologist should know. AJR Am J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 30. Siebenrock KA, Kalbermatten DF, Ganz R.. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 2003; 407: 241–8. [DOI] [PubMed] [Google Scholar]
- 31. Troelsen A, Rømer L, Jacobsen S. et al. Clinical acetabular retroversion is common in developmental dysplasia of the hip as assessed by the weight bearing position. Acta Orthop 2010; 81: 436–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Umer M, Thambyah A, Tan WT, Das De S.. Acetabular morphometry for determining hip dysplasia in the Singaporean population. J Orthop Surg (Hong Kong) 2006; 14: 27–31. [DOI] [PubMed] [Google Scholar]
- 33. Chadayammuri V, Garabekyan T, Jesse MK. et al. Measurement of lateral acetabular coverage: a comparison between CT and plain radiography. J HIP Preserv Surg 2015. Oct 22; 2: 392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mast NH, Impellizzeri F, Keller S, Leunig M.. Reliability and agreement of measure used in radiographic of the adult hip. Clin Orthop Relat Res 2011; 469: 188–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tan L, Aktas S, Copuroglu C. et al. Reliability of radiological parameters measured on anteriposterior pelvis radiographs of patients with developmental of the hips. Acta Orthop Belg 2001. Oct; 67: 347–79. [PubMed] [Google Scholar]
- 36. Brockwell J, O’Hara JN, Young DA.. Acetabular dysplasia: aetiological classification In: McCarthy JC, Villar RN, Noble PC (eds). Hip Joint Restoration. New York: Springer International, 2017, pp. 631–9. [Google Scholar]
- 37. Klaue K, Durnin CW, Ganz R.. The acetabular rim sundrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991; 73: 423–9. [DOI] [PubMed] [Google Scholar]
- 38. Goronzy J, Franken L, Hartmann A. et al. What were the results of surgical treatment of hip dysplasia with concomitant cam deformity? Clin Orhop Relat Res 2017; 475: 1128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]