Abstract
Background:
Various surgical techniques are available to reduce chronic instability of the lateral ankle ligament complex. The most effective method for these procedures remains controversial. This report presents a surgical technique that is similar to the Broström procedure and uses a modified, nonaugmented repair technique.
Materials and Methods:
38 soldiers with a history of chronic lateral ankle instability and poor ankle function underwent plication of the anterior talofibular ligament-lateral capsule complex with transosseous fixation of the calcaneofibular ligament through a fibular bone tunnel between 2004 and 2007. This study included 33 men and 5 women with a mean age of 25.6 years (range 18–36 years) at the time of surgery. Each patient was confirmed to have a history of chronic lateral ankle instability after an inversion injury, and symptoms had been noted for at least 1 year. The patients were followed up with stress radiographs, American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot functional score, and the Sefton assessment system. The mean followup period was 77.6 months (range 66-89 months).
Results:
At the last evaluation, the talar tilt reduced from an average of 13.9° ± 2.4° before surgery to 3.8° ± 1.8° after surgery, and anterior drawer displacement reduced from 9.6 ± 2.9 mm to 2.3 ± 1.6 mm. The mean AOFAS ankle-hindfoot scale score for functional stability increased from 71.6 ± 4.0 points preoperatively to 95.6 ± 4.0 points postoperatively. As evaluated by the Sefton assessment system, 36 patients (95%) reported an excellent or good functional outcome. All patients resumed normal daily activities and active military duty after the surgery.
Conclusion:
The procedure described here could be considered a viable alternative option to anatomic reconstruction such as the modified Broström procedure and might be appropriate for the general population.
Keywords: Chronic lateral ankle instability, modified Broström procedure, nonaugmented repair
MeSH terms: Ankle injuries, ankle lateral ligaments, calcaneofibular ligament, chronic ankle instability
Introduction
Ankle sprain with lateral ankle ligament injury is the most common injury in sports.1 Usually, application of excessive inversion force when the foot is plantar flexed, affects the anterolateral capsule first, followed by the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL), depending on the increasing stress.2 The primary antagonist to inversion and translation of ankle plantar in flexion is the ATFL, while the major contributor to subtalar joint stability is the CFL.3,4 The ATFL and CFL act synergistically: The ATFL is stretched in the plantar flexed ankle and the CFL and PTFL are stretched in the dorsiflexed ankle. Lateral ankle stability chiefly depends on the ATFL and CFL.5
Management of acute injuries includes rest, icing, compression, elevation, and protection, followed by rehabilitation with peroneal muscle strengthening and proprioceptive training. Although conservative management protocols are often the first choice of treatment and are effective, recurrent sprains may lead to ligament attenuation or complete tearing. These patients are likely to develop an instability pattern.6 Symptoms such as recurrent ankle sprains, difficulty in ambulation on uneven ground, and pain during an activity of instability, may significantly affect daily activities, work, or exercise. Furthermore, osteochondral lesions of the talar dome and subsequent ankle osteoarthritis have been reported as long term complications of chronic lateral instability.7,8
Operative reconstruction not only maintains the stability of the ankle, but may also prevent these complications.9 Since the reconstruction procedure of nonaugmented, direct repair of the torn ends of the ATFL and CFL by midsubstance suturing was first described by Broström in 1966,10 that and several subsequent modifications have all resulted in satisfactory outcomes. Multiple studies have reported that nearly 90% of patients exhibit good to excellent outcomes.11,12,13,14,15,16,17 The common advantages of these procedures include its simplicity and reliability with few complications, as it is performed with the original ligament tissue and does not require the normal tendon to be sacrificed. Furthermore, this procedure restores the native ankle anatomy, joint kinematics, and stability, while preserving subtalar motion and ankle function. Therefore, the Broström technique or its modifications are believed to be the first choice of treatment when surgical intervention is necessary.18 Our modification of this popular technique makes use of plication of the ATFL-lateral capsule complex with transosseous fixation of an advanced CFL through a fibular bone tunnel. The ATFL-lateral capsule complex plication is technically simpler and easier to perform. Meanwhile there is less fracture risk for the distal fibula during the transosseous fixation of the CFL due to the creation of only a single bone tunnel. We believe that this hybrid technique can accomplish the goal of anatomic reconstruction, which is sufficiently stable and easily reproducible.
Materials and Methods
38 soldiers who underwent unilateral reconstruction of the lateral ligaments of the ankle by a single experienced orthopedic surgeon between 2004 and 2007 constitute this retrospective study. This study included 33 men and 5 women with a mean age of 25.6 years (range 18–36 years) at the time of surgery. Each patient was confirmed to have a history of chronic lateral ankle instability after an inversion injury, to have undergone a program of nonoperative management consisting of physiotherapy and home exercise, and experienced limitations in sports and daily life activities. All patients had recurrent symptoms, such as give-way weakness or a sensation of instability during daily activities and in sports that resulted in pain, swelling, and interference with their normal activities. In all patients, symptoms had been noted for at least 1 year, but for not more than 10 years. Physical examination with both the anterior drawer and inversion stress tests of the index ankles showed laxity in comparison with that of the contralateral ankle. All patients were skeletally mature and had not undergone a prior ankle surgery. Patients were included in this study if they had no prior surgery or advanced osteoarthritic change in the affected ankle, no previous fractures, an uninjured contralateral ankle, a properly aligned foot, and no neuromuscular disorder. Standing radiographs of the ankle, preoperative and followup stress radiographs in two planes were obtained for all patients using a Telos GA-II/E stress radiography device with standardized measurement of anterior talar translation and talar tilt with 150 N of applied force, as described in Karlsson et al.19
Operative procedure
The anesthetized patient was asked to lie in a supine position and a large sandbag was placed underneath the buttock on the side where the surgery was being performed, and a thigh tourniquet control was placed. Thereafter, a 3 cm slightly curved incision was made from the distal fibula tip toward the 5th metatarsal base to expose the anterolateral ankle joint. Next, full-thickness skin flaps were made and a dissection was performed to expose the anterolateral capsule, distal fibula, and peroneal tendons. The lateral capsule ligament complex (anterolateral capsule and ATFL) was transected at its midpoint and redundant or scar tissue was excised. The joint was inspected for loose bodies or osteochondral lesions, and hypertrophic synovium or fibrous tissue was removed by arthroscopy before the repair procedures.
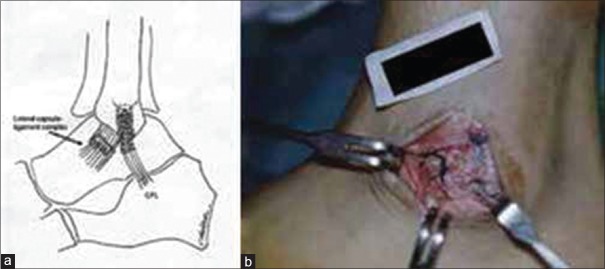
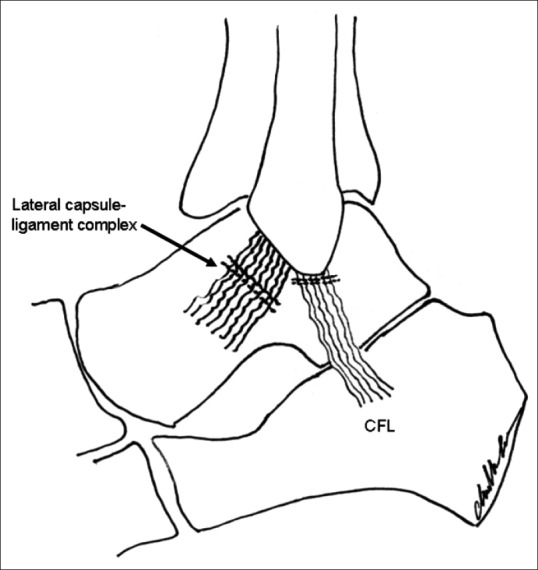
Thereafter, the peroneal tendons were retracted posteriorly to expose the CFL, which allowed for subsequent identification of the CFL insertion site [Figure 1]. The CFL was often attenuated or even avulsed from its insertion in the fibula. The CFL was then cut from the insertion point and advanced with 2-0 Ethibond sutures using the Bunnell technique. A short bony tunnel along the original CFL axis was created from the distal to the proximal direction in the distal fibular by removing some cancellous bone from the fibular attachment of the CFL using a 2.0-mm drill bit. Then, the bony tunnel was dilated using a 3.0-mm drill bit followed by a 4.0-mm drill bit [Figure 2]. Care was taken to not damage the cortex of the proximal end of the bony tunnel of the fibula by creating an approximately 2-cm cannulated structure through the fibular attachment of the CFL. Under tension with the ankle in slight dorsiflexion and the foot slightly everted, the CFL was advanced and inserted into the bony tunnel with transosseous suture fixation. Some of the cancellous bone that was removed before drilling was then grafted into the bony tunnel. After CFL reconstruction, the incised ATFL-lateral capsule complex was imbricated in a pants-over-vest fashion with 2-0 Ethibond sutures [Figure 3]. The wound was then irrigated and hemostasis was obtained. The closure was performed in layers and the tourniquet was released. Thereafter, the ankle was immobilized using a posterior molded splint with the ankle and foot in a neutral position.
Figure 1.
Diagramatic representation of the lateral capsule-ligament complex was transected in its mid-portion and the redundant or scar tissue was excised. The calcaneofibular ligament insertion points were divided and the calcaneofibular ligament was cut from the insertion point
Figure 2.
Peroperative photograph showing calcaneofibular ligament was advanced with the Bunnell suture technique. A short bony tunnel along the original calcaneofibular ligament axis was created from the fibular attachment of the calcaneofibular ligament using the 2.0-mm, 3.0-mm, and 4.0-mm drill bits
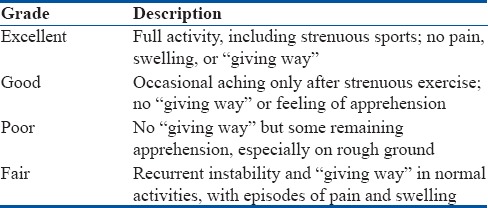
Figure 3.
Diagramatic representation (a), peroperative photograph (b) showing that after the advanced calcaneofibular ligament was inserted into the bony tunnel with transosseous suture fixation, the incised anterior talofibular ligament-lateral capsule complex was imbricated in a pants-over-vest suture
The ankle was immobilized with the posterior splint for 2 weeks and maintained in a nonweight bearing position. After removal of the wound dressing and sutures, a short leg-walking splint was applied, and active range of motion exercises were performed for the treated ankle for another 4 weeks. At 6 weeks postoperatively, the walking splint was removed and the ankle was protected by a soft orthosis. Physiotherapy, including proprioceptive training, progressive strengthening, and flexibility exercises were then initiated. Three months postoperatively, patients were allowed to practice straight line running and gentle jogging with a soft brace. Patients were allowed to participate in a full range of sports activities by 6 months postoperatively; however, the use of an ankle support during heavy exercise, such as while playing basketball or tennis, was advised for an additional 6 months.
Patients were assessed using the American Orthopaedic Foot and Ankle Society ankle-hindfoot scale (AOFAS score) as the functional score, the scoring system developed by Sefton et al. for the evaluation of subjective satisfaction [Table 1], and stress radiographs of the talar tilt and anterior talar displacement.19,20,21 Results of the Sefton assessment identify patients with “excellent” results as those who are capable of full activity, including strenuous sports and do not experience pain, swelling, or ankle instability. Patients with “good” results were those who had pain only after strenuous exercise; however, with no instability or feelings of apprehension. Patients with “fair” results were those who felt some residual instability and exhibited apprehension while walking, although it was comparatively reduced after surgery. Patients with “poor” results were those who experienced recurrent instability and give-way weakness during normal activities with episodes of pain and swelling. Such patients may require surgery again. Postoperative AOFAS score evaluation, Sefton assessment, and stress radiography were performed at an average followup period of 77.6 months (range 66–89 months).
Table 1.
Sefton grading system
Statistical analysis
Statistical analysis of the data was performed with using a paired t-test. A P ≤ 0.05 was assumed to indicate statistical significance.
Results
Between 2004 and 2007, the procedure was performed on 42 ankles, of which 38 ankles completed followup. The mean surgical time measured from the placement to removal of the tourniquet was 45 min (range 38–56). The average followup period was 77.6 months (range 66–89 months).
The average preoperative AOFAS ankle-hindfoot scale score was 71.6 ± 4.0 points (range 63–79 points). The average 77.6-month followup period score was 95.6 ± 4.0 points (range 84–100 points), and the difference was statistically significant (P < 0.001). Results of the Sefton assessment showed that 27 patients had excellent results, 9 had good results, and 2 had fair results. After surgery, all patients not only resumed daily activities, but also participated in their organized physical fitness training programs and could meet the standards of the physical fitness, such as the 3000 m run for men and the 1500 m run for women. No patient complained of lasting pain in the lateral aspect of the operated ankle.
Telos GA-II/E stress radiographs indicated that talar tilt reduced from an average of 13.9 ± 2.4° (range 10°–22°) before surgery to 3.8° ±1.8° (range 2°–9°) after surgery, and the anterior drawer displacement improved from an average of 9.6 ± 2.9 mm (range 6–15 mm) before surgery to 2.3 ± 1.6 mm (range 1–7 mm) after surgery. Both differences were statistically significant (P < 0.001). No patient showed evidence of degenerative arthritis at the time of final followup.
Postoperative physical examination at followup showed that the range of motion for dorsiflexion and plantar flexion was unrestricted for relative measurements compared to the uninjured side. Injured ankles had a mean minimal loss of range of motion (<5°) for dorsiflexion and plantar flexion compared with healthy ankles. One ankle was found to have tenosynovitis of the peroneal longus tendon intraoperatively, therefore, the pulley was thickened with a partial fissure for the peroneal longus, and the tendon was debrided and tabularized using a running, braided suture. This patient complained of retrocalcaneal pain and soreness while playing basketball at 18 months after surgery though the pain was reduced by 33 months after surgery. He was still pleased with the result and changed his sports to swimming and jogging. A grade 1°–2° anterior drawer test without excessive lateral inversion was noted in two patients postoperatively. However, both exhibited generalized ligamentous laxity, as evidenced by a positive thumb to forearm test and elbow hyperextension, and were inclined to have a lower postoperative AOFAS ankle-hindfoot scale scores (85 and 86 points). These two patients had fair results postoperatively according to the Sefton criteria. No complications of wound healing, infection, fibular fracture during surgery, or nerve injury occurred in any patient.
Discussion
An ideal ankle ligament reconstruction restores the normal anatomy and function of the ligaments and corrects both talar tilt and anterior drawer instability without resulting in a loss of a talocrural and subtalar range of motion. The key to achieving these goals is the maintenance of the ligament insertion points and fiber structure.21 These goals are achieved in the procedure described in this report. Compared with anatomical reconstruction procedures, the tenodesis procedure results in abnormal subtalar and talocrural joint kinematics and increases the risk of ankle stiffness, which induces long term complications of chronic pain or further subtalar arthrosis and increases the difficulty of walking in rough terrain.22,23 Imbrication of the anterolateral capsule-ATFL complex and preservation of the original CFL and normal peroneal function results in near-normal proprioception. This also helps achieve better functional stability.24 The CFL in chronic lateral ankle instability generally healed in continuity and was most often attenuated in midsubstance and lengthened.25 We advanced the originally scarred CFL and overcame the lengthening problem to create an anatomical reconstruction by use of the bone tunnel technique by letting the nonfunctional ligaments restore their tensile strength and regain their functions.
Surgical techniques for attaching tendon grafts or original ligaments to ankle bones that have been described previously include fixation of bone suture anchors and the use of interference screws.13,26,27,28 Several key factors affect the mechanical stability of a suture-anchor threaded with a defined suture, such as the pullout strength of the anchor, the tensile strength of the suture, and the interaction of the anchor and suture at the suture-anchor interface.29 The biomechanical tests of Giza et al. and Li et al. have reported that there is no statistical difference in strength and stiffness for a suture-anchor compared with that of a bone tunnel construct for an anatomic repair of the lateral ligaments of the ankle. We know that transosseous tunnel fixation has the advantages of a larger contact area of the tendon with bone that can advance tendon healing in the bone tunnel and is less expensive than other implantation procedures.30,31,32 We performed surgery on two ankles in which the CFL was avulsed from the calcaneus insertion during the period of data collection. The procedure was performed similarly; however, the fixation was performed with the interference screw at the calcaneus. Due to the fewer number of cases that exhibited this condition and the different fixation methods of CFL, these two patients were excluded from the current study. For tendon grafts that use interference screws, graft fibers may be directly damaged by the sharp edges of the screws and the acute angle at the tunnel entrance. In addition, interference screws may block the growth of the tendon graft-bone tunnel interface.33 Our current procedure uses a transosseous tunnel technique that enhances tissue healing and is simple to perform. Lower costs and a lack of residual hardware are additional advantages.
In studies of modified Broström repair techniques by Karlsson et al. and Girard et al.,19,34 poor outcomes were more commonly associated with patients who were overweight, had a long standing ligamentous insufficiency (10 years), exhibited generalized hypermobility, and underwent revision surgery. Since the concept of the procedure discussed herein is similar to that of the direct repair of ligaments that is used in the modified Broström procedure by the aforementioned authors, we did not perform our procedure on patients who had a prior failed lateral ankle ligament surgery, a history of chronic lateral ankle instability that was >10 years, or body weight >100 kg. Although we only found two patients in the current study that had a relatively lower postoperative AOFAS ankle-hindfoot scale scores, both exhibited generalized ligamentous laxity. However, they were still pleased with the results and returned to their preinjury levels of activity. As for patients with generalized hypermobility, our procedure not only directly repaired or advanced the ATFL and CFL, but also imbricated the anterolateral capsule and shortened the CFL to an adequate length. Thus, this procedure can be an alternative surgery for chronic lateral ankle insufficiency.
In our study, the diagnosis of chronic lateral ankle instability was primarily made by complete history taking, detailed physical examination, and plain radiography. Although some problems are encountered with stress radiographs such as different techniques of stress application, inadequate muscle relaxation, and the coexistence of subtalar instability and generalized hypermobility. Previous studies reported that stress radiographs of the ankle and the calcaneocuboid joint can be read reliably if the proposed measurement techniques are applied.35,36 Moreover, stress radiography was able to quantify the talar tilt and anterior drawer displacement for the index ankles. Thus, it supplied simple, useful, and more objective measurements of mechanical laxity.
One patient with peroneal tenosynovitis at the time of surgery had a relatively lower postoperative AOFAS ankle-hindfoot scale score (84 points). For ankles with chronic lateral instability, DIGiovanni et al. reported that peroneal tenosynovitis was the most common associated injury (77%, 47 of 61 patients),37 while Strauss et al. reported peroneal tendon injuries occurred with the highest frequency (28%, 51 of 180 patients) in association with extra-articular injuries.38 Both authors emphasized the poor postoperative results of ligament reconstruction in the presence of associated injuries and the importance of preoperative screening for associated injuries. As posteromedial or medial pathologic lesions of the ankle may be missed during the inspection at anterolateral arthrotomy, we now routinely examine the ankle with arthroscopy at the time of open ligament reconstruction in recent years.
The present inside-out technique with transosseous suture fixation of the advanced CFL enabled the surgery to be performed with a limited incision of around 3 cm in length. It also has a rapid and short learning curve. The total tourniquet time, including wound closure, was 45 min (range 38–56 min), and this is a relatively lower surgical time than that of other procedures, such as 67 min (range 36–96 min) of total tourniquet time for the modified Broström procedure and 93 min (range 67–114 min) for the Chrisman–Snook procedure, as reported by Hennrikus et al.39
There are some limitations of the current study. Further long term or controlled comparative studies are needed to predict long term success, especially for patients with generalized hypermobility. It is unclear, based on the current study, whether the strength and stiffness of the advanced CFL and at the ligament graft-bone tunnel junction will continue to develop over time. We do not know whether the ankle or subtalar arthrosis wound occurs over the long term with over tightening of the anterolateral capsule-ATFL complex or CFL in the procedure; however, patients did not exhibit restriction motion of the ankle or subtalar joint in our series. Future in vitro biomechanical studies with cadaveric specimens would be an interesting avenue of exploration.
The procedure reported herein is another modified, surgical option for the repair of chronic lateral ankle instability that has limited invasiveness. It provides satisfactory functional outcomes and mechanical stability, a shorter tourniquet time, and low morbidity, and retains the technical simplicity of the original Broström procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hershkovich O, Tenenbaum S, Gordon B, Bruck N, Thein R, Derazne E, et al. Alarge-scale study on epidemiology and risk factors for chronic ankle instability in young adults. J Foot Ankle Surg. 2015;54:183–7. doi: 10.1053/j.jfas.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Lohrer H, Nauck T. Augmented periosteal flap repair of the chronically unstable calcaneocuboid joint. A series of six cases. J Bone Joint Surg Am. 2006;88:1596–601. doi: 10.2106/JBJS.D.02548. [DOI] [PubMed] [Google Scholar]
- 3.Colville MR, Marder RA, Boyle JJ, Zarins B. Strain measurement in lateral ankle ligaments. Am J Sports Med. 1990;18:196–200. doi: 10.1177/036354659001800214. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto H, Yagishita K, Ogiuchi T, Sakai H, Shinomiya K, Muneta T. Subtalar instability following lateral ligament injuries of the ankle. Injury. 1998;29:265–8. doi: 10.1016/s0020-1383(97)00195-2. [DOI] [PubMed] [Google Scholar]
- 5.Ozeki S, Yasuda K, Kaneda K, Yamakoshi K, Yamanoi T. Simultaneous strain measurement with determination of a zero strain reference for the medial and lateral ligaments of the ankle. Foot Ankle Int. 2002;23:825–32. doi: 10.1177/107110070202300909. [DOI] [PubMed] [Google Scholar]
- 6.Gerstner Garces JB. Chronic ankle instability. Foot Ankle Clin. 2012;17:389–98. doi: 10.1016/j.fcl.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Takao M, Ochi M, Uchio Y, Naito K, Kono T, Oae K. Osteochondral lesions of the talar dome associated with trauma. Arthroscopy. 2003;19:1061–7. doi: 10.1016/j.arthro.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, Iwai M. Chondral injuries of the ankle with recurrent lateral instability: An arthroscopic study. J Bone Joint Surg Am. 2009;91:99–106. doi: 10.2106/JBJS.G.00087. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Hamilton G, Ford L. Associated intraarticular ankle pathologies in patients with chronic lateral ankle instability: Arthroscopic findings at the time of lateral ankle reconstruction. Foot Ankle Spec. 2011;4:284–9. doi: 10.1177/1938640011416355. [DOI] [PubMed] [Google Scholar]
- 10.Broström L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–65. [PubMed] [Google Scholar]
- 11.Krantz N, Giraud F, Miletic B, Girard J, Berton C, Duquennoy A, et al. Long term outcome of Duquennoy lateral ligament repair for chronic ankle instability: Repeated evaluated in the SME series at 3 and 25 years followup. J Bone Joint Surg Br. 2011;93:538. [Google Scholar]
- 12.Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84–9. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 13.Cottom JM, Rigby RB. The “all inside” arthroscopic Broström procedure: A prospective study of 40 consecutive patients. J Foot Ankle Surg. 2013;52:568–74. doi: 10.1053/j.jfas.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 14.Corte-Real NM, Moreira RM. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213–7. doi: 10.3113/FAI.2009.0213. [DOI] [PubMed] [Google Scholar]
- 15.Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: Functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37:488–94. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
- 16.Keller M, Grossman J, Caron M, Mendicino RW. Lateral ankle instability and the Brostrom-Gould procedure. J Foot Ankle Surg. 1996;35:513–20. doi: 10.1016/s1067-2516(96)80123-2. [DOI] [PubMed] [Google Scholar]
- 17.Ng ZD, Das De S. Modified Brostrom-Evans-Gould technique for recurrent lateral ankle ligament instability. J Orthop Surg (Hong Kong) 2007;15:306–10. doi: 10.1177/230949900701500313. [DOI] [PubMed] [Google Scholar]
- 18.Baumhauer JF, O’Brien T. Surgical considerations in the treatment of ankle instability. J Athl Train. 2002;37:458–62. [PMC free article] [PubMed] [Google Scholar]
- 19.Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988;70:581–8. [PubMed] [Google Scholar]
- 20.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 21.Sefton GK, George J, Fitton JM, McMullen H. Reconstruction of the anterior talofibular ligament for the treatment of the unstable ankle. J Bone Joint Surg Br. 1979;61-B:352–4. doi: 10.1302/0301-620X.61B3.113415. [DOI] [PubMed] [Google Scholar]
- 22.Rosenbaum D, Becker HP, Wilke HJ, Claes LE. Tenodeses destroy the kinematic coupling of the ankle joint complex. A three-dimensional in vitro analysis of joint movement. J Bone Joint Surg Br. 1998;80:162–8. doi: 10.1302/0301-620x.80b1.8014. [DOI] [PubMed] [Google Scholar]
- 23.Krips R, van Dijk CN, Halasi PT, Lehtonen H, Corradini C, Moyen B, et al. Long term outcome of anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: A multicenter study. Foot Ankle Int. 2001;22:415–21. doi: 10.1177/107110070102200510. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton WG, Thompson FM, Snow SW. The modified Brostrom procedure for lateral ankle instability. Foot Ankle. 1993;14:1–7. doi: 10.1177/107110079301400101. [DOI] [PubMed] [Google Scholar]
- 25.Liu SH, Jacobson KE. A new operation for chronic lateral ankle instability. J Bone Joint Surg Br. 1995;77:55–9. [PubMed] [Google Scholar]
- 26.Messer TM, Cummins CA, Ahn J, Kelikian AS. Outcome of the modified Broström procedure for chronic lateral ankle instability using suture anchors. Foot Ankle Int. 2000;21:996–1003. doi: 10.1177/107110070002101203. [DOI] [PubMed] [Google Scholar]
- 27.Jeys LM, Harris NJ. Ankle stabilization with hamstring autograft: A new technique using interference screws. Foot Ankle Int. 2003;24:677–9. doi: 10.1177/107110070302400904. [DOI] [PubMed] [Google Scholar]
- 28.Louden KW, Ambrose CG, Beaty SG, McGarvey WC, Clanton TO. Tendon transfer fixation in the foot and ankle: A biomechanical study evaluating two sizes of pilot holes for bioabsorbable screws. Foot Ankle Int. 2003;24:67–72. doi: 10.1177/107110070302400111. [DOI] [PubMed] [Google Scholar]
- 29.Rupp S, Georg T, Gauss C, Kohn D, Seil R. Fatigue testing of suture anchors. Am J Sports Med. 2002;30:239–47. doi: 10.1177/03635465020300021601. [DOI] [PubMed] [Google Scholar]
- 30.Giza E, Nathe R, Nathe T, Anderson M, Campanelli V. Strength of bone tunnel versus suture anchor and push-lock construct in Broström repair. Am J Sports Med. 2012;40:1419–23. doi: 10.1177/0363546512443947. [DOI] [PubMed] [Google Scholar]
- 31.Li HY, Hua YH, Wu ZY, Chen B, Chen SY. Strength of suture anchor versus transosseous tunnel in anatomic reconstruction of the ankle lateral ligaments: A biomechanical study. Arthroscopy. 2013;29:1817–25. doi: 10.1016/j.arthro.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad CS, Stewart AM, Izquierdo R, Bigliani LU. Tendon-bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med. 2005;33:1667–71. doi: 10.1177/0363546505278252. [DOI] [PubMed] [Google Scholar]
- 33.Singhatat W, Lawhorn KW, Howell SM, Hull ML. How four weeks of implantation affect the strength and stiffness of a tendon graft in a bone tunnel: A study of two fixation devices in an extraarticular model in ovine. Am J Sports Med. 2002;30:506–13. doi: 10.1177/03635465020300041001. [DOI] [PubMed] [Google Scholar]
- 34.Girard P, Anderson RB, Davis WH, Isear JA, Kiebzak GM. Clinical evaluation of the modified Brostrom-Evans procedure to restore ankle stability. Foot Ankle Int. 1999;20:246–52. doi: 10.1177/107110079902000407. [DOI] [PubMed] [Google Scholar]
- 35.Lohrer H, Nauck T, Arentz S, Schöll J. Observer reliability in ankle and calcaneocuboid stress radiography. Am J Sports Med. 2008;36:1143–9. doi: 10.1177/0363546507313091. [DOI] [PubMed] [Google Scholar]
- 36.Beynnon BD, Webb G, Huber BM, Pappas CN, Renström P, Haugh LD. Radiographic measurement of anterior talar translation in the ankle: Determination of the most reliable method. Clin Biomech (Bristol, Avon) 2005;20:301–6. doi: 10.1016/j.clinbiomech.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 37.DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809–15. doi: 10.1177/107110070002101003. [DOI] [PubMed] [Google Scholar]
- 38.Strauss JE, Forsberg JA, Lippert FG., 3rd Chronic lateral ankle instability and associated conditions: A rationale for treatment. Foot Ankle Int. 2007;28:1041–4. doi: 10.3113/FAI.2007.1041. [DOI] [PubMed] [Google Scholar]
- 39.Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability. A prospective, randomized comparison. Am J Sports Med. 1996;24:400–4. doi: 10.1177/036354659602400402. [DOI] [PubMed] [Google Scholar]