We examined whether more granular data improved insights into county-level HIV/hepatitis C virus (HCV) outbreak vulnerability in Tennessee relative to recent national models. Sixteen counties unranked in prior analyses were identified as vulnerable. Importantly, opioid prescribing patterns significantly influenced increased risk for HIV/HCV.
Keywords: HIV, HCV, opioid epidemic, dimension reduction, county-level vulnerability
Abstract
Background
Knowing which factors contribute to county-level vulnerability to a human immunodeficiency virus (HIV)/hepatitis C virus (HCV) outbreak, and which counties are most vulnerable, guides public health and clinical interventions. We therefore examined the impact of locally available indicators related to the opioid epidemic on prior national models of HIV/HCV outbreak vulnerability.
Methods
Tennessee’s 95 counties were the study sample. Predictors from 2012 and 2013 were used, mirroring prior methodology from the US Centers for Disease Control and Prevention (CDC). Acute HCV incidence was the proxy measure of county-level vulnerability. Seventy-eight predictors were identified as potentially predictive for HIV/HCV vulnerability. We used multiple dimension reduction techniques to determine predictors for inclusion and Poisson regression to generate a composite index score ranking county-level vulnerability for HIV/HCV.
Results
There was overlap of high-risk counties with the national analysis (25 of 41 counties). The distribution of vulnerability reinforces earlier research indicating that eastern Tennessee is at particularly high risk but also demonstrates that the entire state has high vulnerability.
Conclusions
Prior research placed Tennessee among the top states for opioid prescribing, acute HCV infection, and greatest risk for an HIV/HCV outbreak. Given this confluence of risk, the Tennessee Department of Health expanded upon prior work to include more granular, local data, including on opioid prescribing. We also explored nonfatal and fatal overdoses. The more complete statewide view of risk generated, not only in eastern counties but also in the western corridor, will enable local officials to monitor vulnerability and better target resources.
Prescription opioid misuse and abuse have been at the center of a national epidemic of overdose deaths in recent years in the United States. Opioid prescribing rates, which peaked around 2010, have only declined slightly since then, and a national public health emergency has recently been declared by the federal government [1–3]. Since 2012, illicit drugs including heroin and fentanyl have become cheaper and often easier to obtain than prescription drugs and are particularly widespread in economically depressed communities with recently increasing mortality [4]. During this time, age-adjusted opioid-related mortality in the United States has skyrocketed from 3 per 100000 in 2000 to >10.4 per 100000 in 2015 [1].
Tennessee has one of the highest rates of opioid prescribing in the United States [5, 6] and, even in the face of interventions such as closing “pill mills” and the establishment of a prescription drug monitoring program, the rate of overdose deaths among persons who inject drugs (PWID) has consistently increased. The progression from prescription opioids to the use of illicit drugs, particularly injectable heroin, is well documented, with approximately 75% of heroin users reporting that their initial drug use was through prescription [4].
The use of both prescription and illicit opioids among PWID has important implications for the co-occurring epidemics of human immunodeficiency virus (HIV), hepatitis C virus (HCV), and neonatal abstinence [7]. With respect to HIV, 10% of new diagnoses in the United States occur in PWID [8]. In 2014, 765 Tennesseans were newly diagnosed with HIV, among whom 29 (3.8%) were exclusively PWID: 12 (1.5%) were men who have sex with men who were also PWID, and 7 (0.9%) were men or women with a PWID partner [9]. According to the most recent US Centers for Disease Control and Prevention (CDC) National Surveillance Data, Tennessee ranked fourth highest among US states for acute HCV case rates, about 63% higher than the national rate [10]. Tennessee, along with 3 other states in the central Appalachian region of the country, experienced a 364% increase in reported acute HCV among individuals aged ≤30 years between 2006 and 2012 [11]. Case rates were twice as high in nonurban compared with urban areas, and approximately 73% of individuals reported being past or present injection drug users [11]. Between 2003 and 2013, Tennessee experienced a 15-fold increase in the number of reported neonatal abstinence syndrome cases [12].
The well-documented HIV outbreak in Scott County, Indiana, between 2014 and 2015 was ultimately demonstrated to have been caused by shared needles and injection paraphernalia associated with PWID using oxymorphone [13]. Of the 181 cases, 92% of individuals with HIV were HCV coinfected [13]. Over concern that this type of outbreak could recur, the CDC developed a vulnerability index to identify other counties at similar risk for a syndemic of drug overdose, HIV, and HCV. The index included predictive variables that tried to emulate Scott County’s characteristics, including racial, socioeconomic, drug overdose, prescription opioid sales (measured as the morphine milligram equivalent [MME]), and buprenorphine prescribing potential characteristics. Among the 220 US counties identified by CDC as the most vulnerable, 41 were in Tennessee, primarily in rural communities [14].
We therefore sought to better understand the vulnerability of Tennessee counties to an HIV/HCV outbreak similar to the one in Scott County, Indiana, by developing an expanded predictor variable list that included additional local data related to the opioid epidemic that are available to most state officials.
METHODS
Study Design
An ecologic study design was used. County-level indicators were collected from the 2010 US Census, Tennessee state- specific indicators from the CDC, and surveillance data from Tennessee Department of Health (TDH) programs (Table 1). Data were collected for 2012 and 2013 to mirror the methodology used by Van Handel et al. [14] We retained all 15 variables from the CDC study and included 63 additional variables in the current analysis.
Table 1.
Study Variable Descriptions, Sources, and Descriptive Statistics
| Variable | Description | Mean | Median | Range | |
|---|---|---|---|---|---|
| 1 | FIPS code | This is the 5-digit FIPS code associated with the county. | NA | NA | NA |
| Source: https://www.census.gov/geo/reference/codes/cou.html | |||||
| 2 | County name | The name of the county. | NA | NA | NA |
| Source: https://www.census.gov/geo/reference/codes/cou.html | |||||
| 3 | Mental health services | Mental health providers include psychiatrists, psychologists, and licensed clinical social workers specializing in mental healthcare. The rate was calculated as the number of mental health providers per 100000 population. 2012 and 2013 data were collected and averaged to create the numerator for this measure. | 60.3 | 38.7 | 0.0–319.37 |
| Source: CMS, National Provider Identification, 2014; https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html | |||||
| 4 | Percentage uninsured | The number of persons without health insurance coverage was divided by total civilian noninstitutionalized population. The 2012 and 2013 data were collected and averaged for each county. | 14.30% | 14.30% | 6.05%–21.2% |
| Source: American Community Survey—Table ID S2701 | |||||
| 5 | Percentage with vehicle accessa | The number of households with a vehicle available divided by the total estimated number of households per county. The 2012 and 2013 data were collected and averaged for each county. | 94.10% | 94.30% | 87.78%–97.67% |
| Source: American Community Survey—Table ID B08141 | |||||
| 6 | Percentage with no high school diploma | The number of persons aged ≥25 years with less than a 12th grade education (including individuals with 12 grades but no diploma) divided by the estimated county population aged ≥25 years. The 2012 and 2013 data were collected and averaged for each county. | 16.40% | 15.80% | 5.4%–34.55% |
| Source: American Community Survey—Table ID S1501 | |||||
| 7 | Population per square mile (log) | The population per square mile per county. The 2012 and 2013 data were collected and averaged for each county; modeled as log base 10. | 1.9 | 1.8 | 1.28–3.09 |
| Source: American Community Survey—Table ID B01003 | |||||
| 8 | Population per square mile | The population per square mile per county. 2012 and 2013 data were collected and averaged for each county | 139.7 | 68.9 | 19.08–1243.24 |
| Source: American Community Survey—Table ID B01003 | |||||
| 9 | Per capita income, log10a | The mean income per person in the county; derived by dividing the total income of all people aged ≥15 years by the total population. 2012 and 2013 data were collected and averaged for each county; modeled as log base 10. | 4.3 | 4.3 | 4.1–4.61 |
| Source: American Community Survey—Table ID B19301 | |||||
| 10 | Per capita income | The mean income per person in the county; derived by dividing the total income of all people aged ≥15 years by the total population. 2012 and 2013 data were collected and averaged for each county. | 20726.1 | 20106 | 12352–41281 |
| Source: American Community Survey—Table ID B19301 | |||||
| 11 | Percentage living in poverty | Poverty levels were defined by the Census Bureau, which uses a set of money income thresholds that vary by family size and composition to determine who is in poverty. If a family’s total income is less than the family’s threshold, then that family and every individual in it is considered in poverty. The number of persons in poverty was divided by the estimated total county population. 2012 and 2013 data were collected and averaged for each county to create the numerator. | 19.30% | 19.10% | 5.75%–31.75% |
| Source: American Community Survey—Table ID B17003 | |||||
| 12 | Percentage of population that is non-Hispanic white | The number of persons who reported they were not Hispanic or Latino and were of white race alone divided by the estimated total county population. 2012 and 2013 data were collected and averaged for each county. | 87.40% | 91.20% | 38.5%–98.6% |
| Source: American Community Survey—Table ID S2702 | |||||
| 13 | Percentage of the population that is unemployed | The number of civilian persons unemployed and actively seeking work divided by the estimated total civilian population aged ≥16 years. 2012 and 2013 data were collected and averaged for each county. | 11.30% | 11.30% | 5.05%–19% |
| Source: American Community Survey—–Table ID S2702 | |||||
| 14 | NCHS rural–urban classification | Counties were categorized into 1 of 6 categories based on OMB’s February 2013 delineation of metropolitan statistical areas and micropolitan statistical areas. The categories are (1) large central metro, (2) large fringe metro, (3) medium metro, (4) small metro, (5) micropolitan, and (6) non-core. | NA | NA | 1–6 |
| Source: CDC; https://www.cdc.gov/nchs/data_access/urban_rural.htm | |||||
| 15 | Is there highway access? | At least 1 interstate or major US highway exit in or within 5 miles of the county border. (1 = yes) | 0.8 | 1 | 0–1 |
| Source: Esri maps and data, 2014 file; http://www.esri.com/data/data-maps | |||||
| 16 | Is there an urgent care facility? | Urgent care is defined as the delivery of ambulatory medical care outside of a hospital emergency department on a walk-in basis without a scheduled appointment. This indicator was dichotomized to yes (at least 1 urgent care facility) or no (no urgent care facility). Only 2012 data were available. | 0.4 | 0 | 0–1 |
| Source: HSIP; https://gii.dhs.gov/HIFLD/hsip-guest (Note: you have to sign up/apply for access to this data) | |||||
| 17 | Premature deathsa | A count of the premature deaths that occurred with a county. 2012 and 2013 data were collected and averaged for each county. | 976.6 | 553 | 89–12580 |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 18 | Years of potential life lost | Years of potential life lost before age 75 per 100000 population (age-adjusted). 2012 and 2013 data were collected and averaged for each county. | 9889.7 | 9887 | 3683.8–15541.7 |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 19 | Adults reporting poor/ fair healtha | Percentage of adults reporting fair or poor health (age-adjusted). 2012 and 2013 data were collected and averaged for each county. | 22.4% | 22.3% | 13.7%–30.1% |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 20 | Poor physical health days | Number of physically unhealthy days reported in past 30 days (age-adjusted). 2012 and 2013 data were collected and averaged for each county. | 4.8 | 4.8 | 3.4–5.7 |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 21 | Poor mental health days | Number of mentally unhealthy days reported in past 30 days (age-adjusted). 2012 and 2013 data were collected and averaged for each county. | 4.7 | 4.7 | 3.8–5.3 |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 22 | Injury-related deaths | The number of deaths related to injuries in a county per 100000 population. 2012 and 2013 data were collected and averaged for each county. | 263.4 | 141 | 23–3293 |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 23 | Rate of injury-related deaths | The rate of injury deaths per 100000 population, per county. 2012 and 2013 data were collected and averaged for each county. | 92.9 | 93.6 | 43.01–170.15 |
| Source: Calculated from: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 24 | Percentage of adults who smoke | Percentage of adults who are current smokers. 2012 and 2013 data were collected and averaged for each county. | 23.40% | 23.30% | 16.2%–28.9% |
| Source: County Health Rankings; http://www.countyhealthrankings.org/app/tennessee/2017/measure/outcomes/1/map | |||||
| 25 | Teen birth ratea | Rate per 1000 of births among female teenagers. Only 2013 data were available. | 48.8 | 49 | 11.0–90.0 |
| Source: American Community Survey—Table ID S1301 | |||||
| 26 | Primary care providers | A count of the number of primary care providers in a county. Only 2013 data were used. | 49.7 | 14 | 0–742 |
| Source: CMS, National Provider Identification, 2014; https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html | |||||
| 27 | Rate of primary care providers | The rate of primary care providers per 100000 population. Only 2013 data were used. | 46.2 | 41.8 | 0.0–164.55 |
| Source: CMS, National Provider Identification, 2014; https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html | |||||
| 28 | Percentage of population with a disability | The percentage of the population of a county that has a disability. 2012 and 2013 data were collected and averaged for each county. | 20% | 20% | 7%–29% |
| Source: American Community Survey—Table ID DP05 | |||||
| 29 | Population estimates | The estimated population for each county. 2012 and 2013 data were collected and averaged for each county. | 67134.8 | 31643.5 | 5101.5–931178 |
| Source: American Community Survey—Table ID DP05 | |||||
| 30 | Population decline 2000–2012 | A measure of population decline at the county level between 2000 and 2012 (1 = population has declined) | 0.1 | 0 | 0–1 |
| Source: American Community Survey—Table ID P001 | |||||
| 31 | Total housing units | The total number of housing units for each county. 2012 and 2013 data were collected and averaged for each county. | 29650.8 | 14327.5 | 2611.5–399106.5 |
| Source: American Community Survey—Table ID S2501 | |||||
| 32 | Occupied housing units | The number of occupied housing for each county. 2012 and 2013 data were collected and averaged for each county. | 26021.2 | 11993.5 | 2088.5–342732.5 |
| Source: American Community Survey—Table ID S2501 | |||||
| 33 | Vacant housing units | The number of vacant housing units for each county. 2012 and 2013 data were collected and averaged for each county. | 3629.6 | 2004 | 335.5–56374 |
| Source: American Community Survey—Table ID S2501 | |||||
| 34 | Crowded housing units | Crowded housing units are defined by having >1 person per bedroom for a given residence. This measure is the average percentage of homes that were defined as being crowded. 2012 and 2013 data were collected and averaged for each county. | 0 | 0 | 0.45%–4% |
| Source: American Community Survey—Table ID S2501 | |||||
| 35 | Percentage of Female-headed households | The percentage of female-headed households (divorced, widowed, never married, and >18 years of age). 2012 and 2013 data were collected and averaged for each county. | 10% | 10% | 7.5%–20% |
| Source: American Community Survey—Table ID S2501 | |||||
| 36 | Number of mobile homes | The number of mobile homes in a county. 2012 and 2013 data were collected and averaged for each county. | 2921.4 | 2496.5 | 244–9361.5 |
| Source: American Community Survey—Table ID DP04 | |||||
| 37 | Percentage of mobile homes | The percentage of the total housing units that were mobile homes. This was calculated by dividing the total number of mobile homes by the total number of housing units. | 20% | 20% | 1%–34% |
| Source: American Community Survey—Table ID DP04 | |||||
| 38 | Homes with no phone service | The average number of homes without phone service in a county. 2012 and 2013 data were collected and averaged for each county. | 700.1 | 371.5 | 27–9173 |
| Source: American Community Survey—Table ID DP04 | |||||
| 39 | Percentage of homes with no phone service | The average percentage of the total housing units that did not have phone service. 2012 and 2013 data were collected and averaged for each county. | 0 | 0 | 1%–11% |
| Source: American Community Survey—Table ID DP04 | |||||
| 40 | Population aged 18–29 | The average number of people aged 18–29 in a county. 2012 and 2013 data were collected and averaged for each county. | 10858.9 | 4452.7 | 563.73–162956.15 |
| Source: American Community Survey—Table ID S1501 | |||||
| 41 | Percentage of population aged 18–29 | The percentage of those aged 18–29 in a county. This was calculated by dividing the population aged 18–29 by the estimated population. | 10% | 10% | 1%–22% |
| Source: American Community Survey—Table ID S1501 | |||||
| 42 | Gini coefficient | Summary measure of income inequality. Values range from 0 to 1, with higher scores indicating greater inequality. 2012 and 2013 data were collected and averaged for each county. | 0.4 | 0.4 | 0.38–0.54 |
| Source: American Community Survey—Table ID B19083 | |||||
| 43 | Residents who were never married | The number of people aged ≥18 years who report never being married. 2012 and 2013 data were collected and averaged for each county. | 15246.2 | 5954.2 | 343.69–285450.77 |
| Source: American Community Survey—Table ID S1201 | |||||
| 44 | Percentage of population never married | The percentage of the population of a county that was never married. This was calculated by dividing the number of residents who were never married by the estimated population. | 20% | 20% | 8%–39% |
| Source: American Community Survey—Table ID S1201 | |||||
| 45 | Total church adherents | The total number of church adherents of any faith or denomination in a county. Only 2013 data were available. | 37077.3 | 15639 | 1729–588132 |
| Source: Association of Religious Data Archive; http://www.thearda.com/ | |||||
| 46 | Church membership | The percentage of the population of a county that attends religious services. This was calculated by dividing the total church adherents by the estimated population. | 50% | 50% | 23%–86% |
| Source: Association of Religious Data Archive; http://www.thearda.com/ | |||||
| 47 | Specialty care providers | A count of the number of specialty care providers (gastroenterologists, hepatologists) in a county. Only 2013 data were utilized. | 5 | 1 | 0–113 |
| Source: CMS, National Provider Identification, 2014; https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html | |||||
| 48 | Rate of specialty care providers | The rate of specialty care providers (gastroenterologists, hepatologists) per 100000 population, per county. | 4.2 | 2 | 0.0–33.2 |
| Source: CMS, National Provider Identification, 2014; https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand/DataDissemination.html | |||||
| 49 | Drug trafficking “hot zone” | Was the county identified as a “drug trafficking hot zone” by the department of justice? (1 = yes) | 0.3 | 0 | 0–1 |
| Source: Drug Enforcement Agency—High Intensity Drug Trafficking Areas; https://www.dea.gov/ops/hidta.shtml | |||||
| 50 | Drug-related crimes | The number of drug crimes (distribution and selling charges, possession and concealing charges) in a county. This includes only narcotic drugs. 2012 and 2013 data were collected and averaged for each county. | 485.3 | 159 | 10.0–9584 |
| Source: Tennessee Incident Based Reporting System; http://www.tncrimeonline.com/ | |||||
| 51 | Violent crimes | The number of violent crimes (murder, forcible rape, aggravated assault, robbery) in a county. 2012 and 2013 data were collected and averaged for each county. | 418.1 | 109 | 2.5–12072 |
| Source: Tennessee Incident Based Reporting System; http://www.tncrimeonline.com/ | |||||
| 52 | Theft crimes | The number of theft crimes (pickpocketing, purse snatching, shoplifting, from buildings, from coin machines, from motor vehicles, of motor vehicle parts, of motor vehicles) in a county. 2012 and 2013 data were collected and averaged for each county. | 1705.9 | 549.5 | 40.5–33801 |
| Source: Tennessee Incident Based Reporting System; http://www.tncrimeonline.com/ | |||||
| 53 | Drug coalition? | Is there a drug coalition present within the county? (1 = yes) | 0.5 | 1 | 0–1 |
| Source: List of Drug Coalitions, requested from Tennessee Department of Health, Prescription Drug Overdose Program | |||||
| 54 | Total MMEb for all drugs | The total morphine milligram equivalent for all drugs with a conversion factor, per county. 2012 and 2013 data were collected and averaged for each county. | 110656792.8 | 65716853.2 | 8196158.7–750503671.2 |
| Source: Tennessee Controlled Substance Monitoring Database, Patient and Prescription Tables, from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 55 | MME rate for analgesicsa | The MME rate per 100000 population for analgesics. 2012 and 2013 data were collected and averaged for each county. | 1696.8 | 1648.8 | 449.21–3917.51 |
| Source: Tennessee Controlled Substance Monitoring Database, Patient and Prescription Tables, from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 56 | MME rate for MATc drugs | The MME rate per 100000 population for drugs indicated for medication assisted treatment. 2012 and 2013 data were collected and averaged for each county. | 424.7 | 284.7 | 37.42–2229.61 |
| Source: Tennessee Controlled Substance Monitoring Database, Patient and Prescription Tables, from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 57 | Multiple provider episodes | The number of people who went to ≥5 doctors and had ≥5 opioid prescriptions filled with 180 days. The county of residence for the doctor shopper is captured. 2012 and 2013 data were collected and averaged for each county. | 101.8 | 55 | 0–1225 |
| Source: Tennessee Controlled Substance Monitoring Database, Patient and Prescription Tables, from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 58 | Deaths related to all drugs | The count of all deaths attributed to any kind of drug. The county of residence for the person who died is captured. 2012 and 2013 data were collected and averaged for each county. | 11.9 | 6 | 0.5–133 |
| Source: Death Certificate Data from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 59 | Deaths related to heroin and opioids onlya | The count of all deaths attributed to heroin or opioids. The county of residence for the person who died is captured. 2012 and 2013 data were collected and averaged for each county. | 8.2 | 3.5 | 0–119 |
| Source: Death Certificate Data from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 60 | Rate of death, all drugs | The rate, per 100000, of the number of deaths related to all drugs. | 19.8 | 19.1 | 2.9–55.13 |
| Source: Death Certificate Data from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 61 | Rate of death, heroin and opioids only | The rate, per 100000, of the number of deaths related to heroin and opioids. | 12.5 | 11.9 | 0.0–55.13 |
| Source: Death Certificate Data from Tennessee Department of Health, requested from Prescription Drug Overdose Program | |||||
| 62 | Certified pain management clinics | The count of certified pain clinics per county. This does not capture pain clinics that are not registered. Only 2013 data were used. | 3.3 | 1 | 0–35 |
| Source: License Data from Tennessee Department of Health, requested from Controlled Substance Monitoring Database, Regulation and Enforcement | |||||
| 63 | Nonfatal overdoses, all drugs | The rate of nonfatal overdoses, per 100000 population, that resulted in a hospitalization or emergency department visit regardless of the drug type that caused the overdose by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 358.8 | 355.1 | 158.23–588.58 |
| Source: Hospital Discharge Data, from Tennessee Department of Health; https://www.tn.gov/health/article/statistics-hdds | |||||
| 64 | Nonfatal overdoses, opioids only | The rate of nonfatal overdoses, per 100000 population, that resulted in a hospitalization or emergency department visit for opioids only, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 57.7 | 52.1 | 0.0–169.88 |
| Source: Hospital Discharge Data, from Tennessee Department of Health; https://www.tn.gov/health/article/statistics-hdds | |||||
| 65 | Nonfatal overdoses, heroin only | The rate of nonfatal overdoses that resulted in a hospitalization or emergency department visit for heroin only, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 1.5 | 0 | 0.0–14.93 |
| Source: Hospital Discharge Data, from Tennessee Department of Health; https://www.tn.gov/health/article/statistics-hdds | |||||
| 66 | Buprenorphine providers | A count of all buprenorphine providers in a county, regardless of the DATA-2000 waiver possessed. Only 2013 data were used. | 6 | 1 | 0–101 |
| Source: SAMHSA Buprenorphine Treatment Practitioner Locator; https://www.samhsa.gov/medication-assisted-treatment/physician-program-data/treatment-physician-locator | |||||
| 67 | Rate of buprenorphine providers | A per capita estimate of buprenorphine providers, by county. | 5.5 | 2.9 | 0.0–51.88 |
| Source: SAMHSA Buprenorphine Treatment Practitioner Locator; https://www.samhsa.gov/medication-assisted-treatment/physician-program-data/treatment-physician-locator | |||||
| 68 | Substance abuse treatment beds | The number of beds available in adult substance abuse treatment facilities registered with the state mental health board (does not include some for-profit sites). Only 2013 data were used. | 20.2 | 0 | 0–443 |
| Source: Facility Capacity data from Tennessee Department of Mental Health and Substance Abuse funded treatment centers, requested from TDMHSA | |||||
| 69 | Substance abuse treatment beds, per capita | The per capita rate of substance abuse treatment beds, by county. | 22.1 | 0 | 0.0–572.64 |
| Source: Facility Capacity Data from TDMHSA-funded treatment centers, requested from TDMHSA | |||||
| 70 | Methadone clinics | The number of methadone clinics per county. Only 2013 data were used. | 0.1 | 0 | 0–3 |
| Source: License data from TDMHSA | |||||
| 71 | Admissions for injection drug use treatmenta | The sum of all the people who entered treatment for 1 of the following conditions in a state-funded substance abuse treatment facility: (1) addiction to prescription opioids; (2) addiction to methamphetamines; (3) addiction to heroin; (4) addiction to other prescription drugs. 2012 and 2013 data were collected and averaged for each county. | 101.8 | 55 | 0–1225 |
| Source: Admissions data from TDMHSA-funded treatment centers, requested from TDMHSA | |||||
| 72 | Neonatal abstinence syndrome cases | The number of neonatal abstinence syndrome cases per county. 2012 and 2013 data were collected and averaged for each county. | 9.9 | 3 | 0–104 |
| Source: Tennessee Department of Health, requested from Family Health and Wellness Program | |||||
| 73 | Rate of HIV incidence | The rate of new HIV diagnoses, per 100000 population, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 6.2 | 4.5 | 0.0–35.95 |
| Source: eHARS—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
| 74 | Rate of HIV prevalencea | The rate, per 100000 population, of living diagnosed HIV cases, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 129.4 | 98 | 0.0–652.4 |
| Source: eHARS—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
| 75 | HIV cases related to injection drug usea | The count of any living diagnosed HIV cases related to injection drug use, by county. 2012 and 2013 data were collected and averaged for each county. | 0.1 | 0.1 | 0.0–0.55 |
| Source: eHARS—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
| 76 | Rate of sexually transmitted diseasesa | The rate of STDs (gonorrhea, chlamydia) per 100000 population by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 396.8 | 321.4 | 79.76–1321.87 |
| Source: PRISM—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
| 77 | Rate of syphilis infections | The rate of syphilis (primary, secondary, early and late latent) cases per 100000 residents, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 1.7 | 0.9 | 0.0–11.99 |
| Source: PRISM—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
| 78 | Rate of acute hepatitis C infections | The rate of acute hepatitis C infection cases per 100000 residents, by county. 2012 and 2013 data were collected and averaged for each county to calculate the numerator for this measure. | 3.2 | 1.1 | 0.0–28.6 |
| Source: NEDSS-based system—Tennessee Department of Health, requested from HIV/STD/Viral Hepatitis Surveillance Program | |||||
Abbreviations: CDC, Centers for Disease Control and Prevention; CMS, Centers for Medicare and Medicaid Services; DATA-2000, Drug Addiction Treatment Act of 2000; eHARS, enhanced HIV/AIDS reporting syndrome; FIPS, Federal Information Processing Standard; HIV, human immunodeficiency virus; HSIP, Homeland Security Infrastructure Program; MAT, medication-assisted treatment; MME, morphine milligram equivalent; NA, Not Applicable; NCHS, National Center for Health Statistics; NEDSS, National Electronic Disease Surveillance System; OMB, Office and Management and Budget; PRISM, Patient Reporting Investigation Surveillance Manager; SAMHSA, Substance Abuse and Mental Health Services Administration; STD, sexually transmitted disease; TDMHSA, Tennessee Department of Mental Health and Substance Abuse.
aVariable was significant in the final model of this study.
bMME is a conversion tool that was developed so that different opioid medications could be compared using a like measure. Opioid medications can now be compared against a single standard for comparison and risk evaluation.
cMAT is the use of medications in combination with counseling for the treatment of substance abuse disorders. Prescription drugs indicated for MAT, namely buprenorphine, work as partial agonists. More information can be found at: https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine.
Setting
Tennessee’s 95 counties comprised the study sample. Predictors were collected and analyses conducted at the county level.
Primary Outcome
County-level vulnerability to an HIV or HCV outbreak was indicated by the incidence of acute HCV from 2012 to 2013. HCV incidence was defined as newly diagnosed cases meeting a confirmed case definition for acute HCV, indicated by positive serology (HCV antibody and/or RNA nucleic acid amplification), indication of signs and symptoms for HCV, with jaundice and/or an elevated alanine aminotransferase level (>400 U/L).
Quantitative Variables
Seventy-eight county-level predictors were identified through author consensus as potentially predictive of high risk for HIV/HCV transmission. Many indicators initially collected (Table 1) as counts were used to derive rates. Continuous variables with large ranges, such as the MME, were log-transformed or otherwise normalized to improve coefficient interpretability. Income and population measures were log-transformed, as rates were not appropriate in these 2 instances.
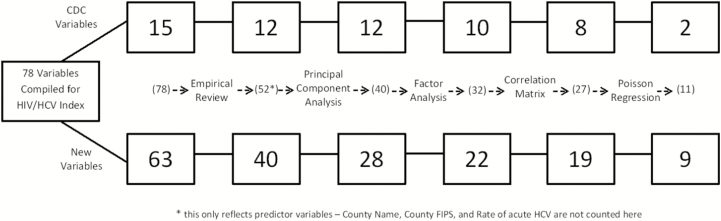
Given the sample size (n = 95) and large number of potential predictors (n = 78), we implemented dimension reduction techniques in sequential stages to cluster predictors into groups that reduced correlations and explained the most variance: (1) empirical review conducted by the authors; (2) principal components analysis; (3) factor analysis; and (4) correlation tests. Supplemental data contains additional information on dimension reduction steps. All dimension reduction and regression analysis in stages 2–4 were conducted using R software version 3.3.1 (www.r-project.org); factor analysis was done using the “psych” package. Each step in the dimension reduction process assessed the relatedness of the predictor variables to other predictors. A final list of minimally correlated indicators was generated and used to model the rate of acute HCV infections.
Empirical review included project team discussion of each item in Table 1. Indicators that were similar, better explained by other measures, or had little variance between counties were removed. This discussion resulted in the removal of 23 of the 78 indicators. Three indicators (county name, county Federal Information Processing Standard [FIPS] code, and acute HCV rate) were excluded because they were identifiers or the outcome, leaving 52 predictors for dimension reduction.
Principal components analysis was used to remove correlated variables by clustering predictors [15], yielding 8 components that explained 74% of the model’s variance. This step resulted in the removal of 12 variables. Components were interpreted based on strength of correlation, either positive or negative.
Factor analysis was used to examine the underlying data structure for further data reduction [16]. A “very simple structure” test, which applied a goodness-of-fit test [17], yielded 4 factors from the 40 remaining predictors. Using this 4-factor structure, 8 additional variables were removed.
The remaining 32 variables were assessed for statistically significant associations using a correlation matrix. Five additional predictors were significantly correlated with other variables and were removed, leaving a final set of 27 predictors. Figure 1 summarizes the dimension reduction process and sources of the variables included in the final regression analysis used to create composite risk scores. The 27 predictors that remained were used to model acute HCV infection rates as a proxy for vulnerability to an HIV/HCV outbreak.
Figure 1.
Study variables, by source, retained at each step of dimension reduction and regression with stepwise insertion. Abbreviations: CDC, Centers for Disease Control and Prevention; FIPS, Federal Information Processing Standards; HCV, hepatitis C virus; HIV, human immunodeficiency virus.
The goal was to create a parsimonious model, retaining variables only at the P < .05 level. Multivariable Poisson regression with county population as an offset [18] yielded 27 predictors that were included in the final model, 10 of which had a statistically significant effect. Stepwise insertion was performed, with the closest nonsignificant variable added to a regression model with predictors that were significant [13]. One predictor was added back in the final model using this stepwise approach.
Vulnerability Score and Ranking
The vulnerability score was developed using significant indicators to compute each county’s index score [13]. Counties were then ranked from highest to lowest, where higher scores indicated increased vulnerability. To account for model uncertainty, we conducted simulations using random and weighted population distributions and regression coefficients from the analysis [13]. The weights used for the sample included the regression coefficient estimates and their respective standard errors to allow for variation in the sample calculations. A total of 10000 samples were drawn and vulnerability ranking was calculated for each county. Observations were then aggregated and ranked, generating 90% confidence intervals [13]. Vulnerability ranking calculations and sample simulations were conducted using “proc surveyselect” in SAS version 9.4 software (SAS Institute, Cary, North Carolina).
RESULTS
Of 11 variables included in the final model, 2 were socioeconomic: (1) vehicle access (percentage of adults with a vehicle) and (2) per capita income (mean income per person aged ≥15 years). Eight variables were health outcome indicators: (1) premature death (count of accidental deaths in a county); (2) teen birth rate per 1000; (3) HIV prevalence rate per 100000; (4) count of HIV cases involving PWID; (5) rate of gonorrhea and chlamydia (combined) per 100000; (6) rate of death related to either heroin or opioids per 100000; (7) admission to substance abuse treatment facilities for injectable substances, which we use as a proxy for the prevalence of PWID; and (8) percentage of adults reporting poor or fair health in the last 30 days. One variable measured opioid prescriptions in the county (rate of MME for prescription pain medications per 100000). Three variables (rate of heroin/opioid death, premature deaths, and per capita income) were protective (Table 2).
Table 2.
Regression Coefficients, Standard Deviations, and Significance Level for Variables Used in Composite Index
| Variable | Coefficient | Standard Deviation | Significance (P Value) |
|---|---|---|---|
| Percentage with vehicle access | 0.2007 | 0.06238 | <.01 |
| Per capita income, log10 | –5.377 | 1.933 | <.01 |
| Premature deaths | –0.0008 | 0.00025 | <.001 |
| Teen birth rate | 0.02066 | 0.007217 | <.01 |
| Rate of HIV prevalence | 0.005201 | 0.0007627 | <.001 |
| HIV cases related to injection drug use | 8.845 | 2.265 | <.001 |
| Rate of sexually transmitted diseases | 0.002199 | 0.000535 | <.001 |
| MME rate for analgesics | 0.0003960 | 0.000112 | <.001 |
| Deaths related to heroin and opioids only | –0.01905 | 0.008865 | <.05 |
| Admissions for injection drug use prevalence | 0.003144 | 0.001156 | <.01 |
| Adults reporting poor/fair health | 0.103 | 0.04856 | <.05 |
Abbreviations: HIV, human immunodeficiency virus; MME, morphine milligram equivalent.
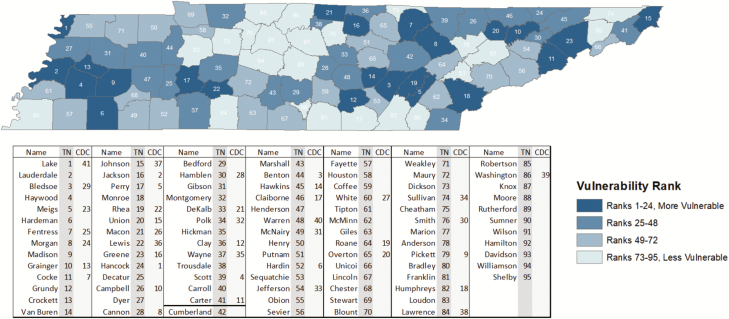
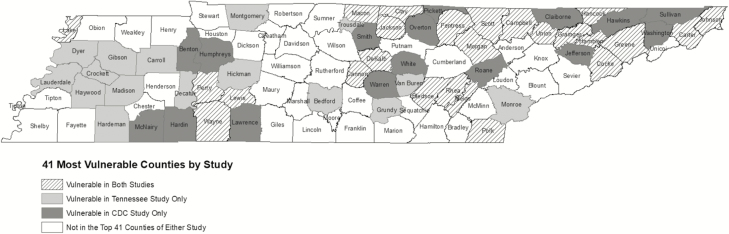
The counties with highest vulnerability were found to be distributed across the state (Figure 2). In the most vulnerable quartile of counties (n = 24), 6 were in the west, 8 in the middle, and 10 in the eastern region of the state. Of 41 counties identified by CDC as at highest risk, 25 also appeared in the top 41 in our Tennessee-specific analysis [13]. Thus, 16 counties were not considered at high risk by CDC but were in our own analysis. Of 25 counties that were considered at high risk and among the top 41 in both analyses, there was considerable divergence in rank between the prior study and our own, sometimes substantially. For example, the highest-risk county in the Tennessee analysis was only ranked 41st in CDC’s assessment. Figure 3 contains a map showing where the counties that were included in both analyses fall, as well as those that are Tennessee-specific (mostly in the western part of the state), and those unique to the CDC analysis (mainly in the eastern part of the state). The distribution of vulnerability reinforces earlier research indicating that eastern Tennessee is at particularly high risk, but also demonstrates clearly that the entire state has regions of high vulnerability.
Figure 2.
Tennessee counties ranked by in-state vulnerability score from highest vulnerability (1) to lowest vulnerability (95). Abbreviations: CDC, Centers for Disease Control and Prevention national vulnerability rank; TN, Tennessee vulnerability rank.
Figure 3.
Top 41 unique and overlapping counties between the Tennessee in-state vulnerability index and the Centers for Disease Control and Prevention (CDC) national vulnerability index.
Eleven of 16 counties that did not remain in the Tennessee model, but were among the 41 highest risk counties in the prior CDC analysis, ranked among the highest in rates of fatal overdose (any drug), nonfatal overdose (opioids only), highest prescription rates for buprenorphine, and numbers of neonatal abstinence cases. Six of the 16 displaced counties were within 10 places of the 41-county cutoff point that was chosen for comparison. When looking at risk scores generated in this study, which ranged from 12.4 (least vulnerable) to 21.1 (most vulnerable), the midpoint (16.7) captured 52 counties, which included the 6 counties from the CDC analysis mentioned above.
Counties identified in our study as having high composite vulnerability also tended to score highly on individual indicators associated with vulnerability, even if they were not retained in our model. For instance, 26 counties ranked in the top 41 with the highest rates of MME and unemployment; 24 of 41 ranked highly on the largest percentage of uninsured adults; and almost half (21/41) were among those with the highest rates of nonfatal overdoses. Only 7 vulnerable counties ranked highly on the per capita income measure. The most vulnerable county in our study, Lake County, had the lowest per capita income in Tennessee. With regard to treatment, 11 counties ranked in the top 41 for greatest number of mental health services and buprenorphine providers. Low per capita income and lack of community services for mental health and addiction treatment were coupled with high rates of MME prescribed for pain, high unemployment, and lower rates of being insured. A sensitivity analysis showed that the relatively high ranking of counties with large prisons was robust to the removal of individuals who were diagnosed while incarcerated, indicating that the rankings distribution was not biased by the presence of prisons.
DISCUSSION
This analysis contextualizes the recent 2-fold increase in opioid deaths and >350% increase in acute HCV among younger individuals, >70% of whom were PWID in Tennessee [10]. Our ability to include granular data about the opioid epidemic, given the known interaction of opioids, HIV, and HCV as seen in Scott County, Indiana [12], provides additional information that TDH can use for outbreak response planning, resource allocation, and public health practice. A key finding of our work is that more than a third of variables that significantly predicted risk of acute HCV infections, the indicator we used as a proxy for outbreaks similar to that of Scott County, Indiana [12], were those associated with opioid use. They included MME rate for pain medicines, rate of deaths from heroin and opioids, prevalence of PWID, and number of HIV cases who were PWID. One finding, that rate of deaths from heroin and opioids and the number of premature deaths have a protective influence, did stand out. We hypothesize that death is a competing risk for HCV or HIV diagnosis, which may reduce the vulnerability ranking of counties with high mortality as higher-risk individuals are removed from the relevant “risk pool.”
Two of the measures in our composite index score, the MME rate for analgesics, a measure that standardizes the amount of opioids prescribed in a community, and the rate of deaths related to heroin and opioids, come from the Controlled Substance Monitoring Database, which is Tennessee’s mandatory prescription monitoring program. In practice, many state prescription monitoring programs are located within law enforcement rather than health departments, and it may be difficult for departments of health to access those data sources for analysis. The metrics used for this analysis are some that our state and many others routinely provide to CDC as part of our Prevention for States funding, and should therefore be available to many state officials. Methods for assessing MME-associated risk are evolving; consequently, investigators should engage in conversations with prescription drug overdose investigators about optimal ways to calculate and use those variables. This analysis highlights the benefits of using disparate and often siloed data systems beyond publicly available data to develop models that are optimal, descriptive, and available at the local level. In addition to US Census data, our vulnerability index contained protected data elements from 4 state agencies. To conduct this study, we collaborated with multiple government entities, including the Department of Health, the Department of Mental Health and Substance Abuse, the Prescription Drug Overdose Program, the Tennessee Bureau of Investigation, and the Vital Records section of TDH to ascertain which data elements were available, at which level (ie, person or county) and for which years. Our collaborative approach could therefore be adopted as a guide for other states to conduct their own vulnerability assessments.
Prior to this analysis, the burden of the 3 primary risks (HIV, HCV, and opioid use) was well known in eastern Tennessee; however, the combination of the 3 syndemic elements in this study highlights areas in the western corridor that were not previously a focus for programmatic intervention. With specific regard to opioid prescribing, state data show that not only do overdose deaths tend to cluster in the eastern corridor, but so do analgesic prescriptions. The vulnerable counties in western Tennessee identified in this study do not coincide with any of the counties that previously were identified with “county of concern” indicators using prescription opioid data alone, with the exception of the one indicator component that reflects high rates of outpatient visits for overdoses, including heroin. The integrated model therefore provides a more nuanced understanding of statewide risks.
This study did have limitations. We relied on 2012–2013 data to expand on the CDC’s earlier research, which focused on this same date range [13]. Overdose deaths in Tennessee are known to be inconsistently captured and may therefore have been underascertained. We may have unmeasured confounders, measurement error (eg, admission to treatment for drugs commonly injected, though the best measure available, likely underestimates the burden of injection drug use in Tennessee), and over-/underfitting in the statistical model. There may be measurement error in our outcome due to variable acute HCV case reporting across counties in Tennessee. While acute HCV has been a reportable condition in Tennessee since the 1990s, during the study period, there was no formal, centralized surveillance system in place to review cases and verify case definition. This changed in recent years, with the establishment of the Viral Hepatitis Surveillance Program, but diagnoses prior to 2015 may be underreported. These limitations, however, do not undermine the importance of a more nuanced understanding of county-level vulnerability, which is a great strength of our study.
Two immediate next steps are recommended. First, more recent data should be examined to see if county-level risk remains consistent in Tennessee during an era in which the opioid and HCV epidemics are continuing to grow. Second, this information should be shared with local health departments around the state. Knowing the locations in which to expand screening activities, improve outreach and prevention efforts, conduct outbreak response exercises, and locate harm reduction services will be instrumental for public health planning.
While our results are likely generalizable only temporally within the state of Tennessee, our methodology is broadly applicable. The majority of data elements in Table 1 are publicly available while the remainder should be available to state officials and within the reach of health departments or other interested parties.
Prior research placed Tennessee among the top states for opioid prescribing, acute HCV infection, and greatest risk for an HIV/HCV outbreak [4, 10, 11, 13]. Given this confluence of disease risk, TDH expanded the prior HIV/HCV outbreak vulnerability study to include more granular, local data, including data on opioid prescribing. With data available on all counties, we were able to re-rank all 95 counties without using an artificial risk cut-point and, perhaps more importantly, explore the role of opioid prescribing patterns in increasing risk for poor health outcomes, including nonfatal and fatal overdoses. While the nature of the epidemic being investigated has changed in the ensuing years, and the generalizability of this analysis may be limited, our methodology is valid and informative, and it may be highly valuable to other public health practitioners.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. M. R. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis. The concept and design of the study was an effort by all listed authors. Acquisition of the data was led by M. R., though all authors suggested sources of data to be collected. Analysis of the data was handled by M. R. and P. F. R., and interpretation of the results was an effort by all authors. All authors took part in the drafting and critical revision of the manuscript.
Acknowledgments. The authors thank Michelle Van Handel, Phillip J. Peters, and John T. Brooks, all from the Centers for Disease Control and Prevention, for their encouragement, sharing of data, and technical assistance in the development of this research.
Financial support. Peter Rebeiro’s work on this project was supported in part by the NIH-funded Tennessee Center for AIDS Research (P30 AI110527).
Potential conflicts of interest. All authors: No reported conflicts of interest. The authors have completed the ICMJE Form for Disclosure of Potential Conflicts of Interest. Peter Rebeiro’s work on this project was supported in part by the NIH-funded Tennessee Center for AIDS Research (P30 AI110527). None of the authors had disclosures to report.
References
- 1. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016; 65:1445–52. [DOI] [PubMed] [Google Scholar]
- 2. Guy GP, Zhang K, Bohm M, et al. Vital signs: changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017; 66:697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. New York Times. Trump plans to declare opioid epidemic a national emergency Available at: https://www.nytimes.com/2017/08/10/us/politics/opioid-trump-emergency.html. Accessed 10 August 2017.
- 4. Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry 2014; 71:821–6. [DOI] [PubMed] [Google Scholar]
- 5. Sycamore Institute. The opioid epidemic in Tennessee: key policy milestones and indicators of progress Available at: http://www.sycamoreinstitutetn.org/2017/08/03/opioid-epidemic-tn-milestones-progress/. Accessed 10 October 2017.
- 6. Centers for Disease Control and Prevention. Opioid prescribing Available at: https://www.cdc.gov/vitalsigns/opioids/index.html. Accessed 10 October 2017.
- 7. Cicero TJ, Ellis MS, Kasper ZA. Increased use of heroin as an initiating opioid of abuse. Addict Behav 2017; 74:63–6. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention. HIV and injection drug use Available at: https://www.cdc.gov/vitalsigns/hiv-drug-use/CDC. Accessed 8 March 2017.
- 9. Enhanced HIV/AIDS Reporting Syndrome (eHARS). Tennessee HIV/AIDS reporting system Accessed 1 July 2017.
- 10. Centers for Disease Control and Prevention. Surveillance for viral hepatitis—United States, 2014 Available at: https://www.cdc.gov/hepatitis/statistics/2014surveillance/index.htm/CDC. Accessed 8 March 2017.
- 11. Zibbell JE, Iqbal K, Patel RC, et al. Centers for Disease Control and Prevention (CDC) Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years—Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep 2015; 64:453–8. [PMC free article] [PubMed] [Google Scholar]
- 12. Miller AM, Warren MD.. Neonatal abstinence syndrome surveillance annual report 2013. Nashville, Tennessee: Tennessee Department of Health, 2013. [Google Scholar]
- 13. Peters PJ, Pontones P, Hoover KW, et al. Indiana HIV Outbreak Investigation Team HIV infection linked to injection use of oxymorphone in Indiana, 2014-2015. N Engl J Med 2016; 375:229–39. [DOI] [PubMed] [Google Scholar]
- 14. Van Handel MM, Rose CE, Hallisey EJ, et al. County-level vulnerability assessment for rapid dissemination of HIV or HCV infections among persons who inject drugs, United States. J Acquir Immune Defic Syndr 2016; 73:323–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Joliffe I. Principal component analysis, 2nd ed. New York, New York: Springer, 2002. [Google Scholar]
- 16. Cattell R. The scientific use of factor analysis. New York: Plenum Press, 1978. [Google Scholar]
- 17. Revelle W, Rocklin T. Very simple structure: an alternative procedure for estimating the optimal number of interpretable factors. Multivariate Behav Res 1979; 14:403–14. [DOI] [PubMed] [Google Scholar]
- 18. Gelman A, Hill J.. Data analysis using regression and multilevel/hierarchical models. New York, New York: : Cambridge University Press, 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.