Abstract
Purpose
To describe the intraoperative multicatheter implantation technique for accelerated partial breast irradiation (APBI) delivered with high-dose-rate brachytherapy (HDR-BT). Secondarily, to evaluate outcomes and toxicity in a series of 83 patients treated with this technique at our institution.
Material and methods
Retrospective analysis of a series of patients treated with HDR-BT APBI after intraoperative multicatheter interstitial implant between November 2006 and June 2017 at our institution. We assessed cosmesis, toxicity, overall survival (OS), and disease-free survival (DFS).
Results
Eighty-three patients were included: 59 patients (71.1%) with primary early-stage breast cancer and 24 (28.9%) with locally recurrent breast cancer. Tumorectomy was performed in all cases, with intraoperative tumor margin assessment and sentinel node biopsy. Median age was 82 years (range, 44-92). The total prescribed dose was 32 Gy (8 treatment fractions) in 60 patients (72.3%), and 34 Gy (10 fractions) in 23 patients (27.7%). Median follow-up was 40 months (range, 1-136 months). Three-year OS and DFS in the recurrent and primary cancer groups were 87% vs. 89%, and 96 % vs. 97.8%, respectively. Five patients died from non-cancer related causes. No local relapses were observed. Rates of acute and late toxicity were low in both groups. The cosmesis was good or excellent in most of patients treated for primary disease; in patients who underwent salvage brachytherapy for local recurrence, cosmesis was good in 49 patients and fair in 6.
Conclusions
This technique, although time-consuming, achieves good local disease control with a satisfactory toxicity profile in both early-stage and local recurrent breast cancer patients. It may be especially suitable for frail patients.
Keywords: APBI, brachytherapy, breast cancer, intraoperative, multicatheter technique, relapse, second treatment
Purpose
Accelerated partial breast irradiation (APBI) is usually performed as a post-lumpectomy radiotherapy technique for women with early-stage breast cancer to deliver treatment exclusively to the tumor bed. Historically, adjuvant whole-breast irradiation (WBI) after lumpectomy has been considered the standard therapeutic approach, with rates of overall survival and locoregional control comparable to mastectomy alone [1]. However, recent data published by Strnad et al. clearly determine the non-inferiority of the partial irradiation approach in the treatment of early breast cancer [2]. The rationale for partial breast irradiation is supported by data from three randomized trials demonstrating that most recurrences following lumpectomy alone, occur adjacent to the lumpectomy cavity [3,4,5] and therefore, WBI might be unnecessary. For this reason, interest in APBI, which targets only the area surrounding the tumor site, has increased in recent years [6,7].
One of the main benefits of APBI is that it reduces the total treatment time from 3-6 weeks to less than a week, which improves patients’ satisfaction and overall quality of life, especially for those patients who live far from radiation centers. APBI can also lower the radiation doses to the healthy surrounding organs and tissues, thus reducing toxicity and improving cosmesis. In addition, cost-effectiveness ratio for APBI is lower than for WBI [8].
Several APBI techniques have been developed as alternatives to the more conventional post-operative approaches [9,10,11], including single-entry intracavitary devices, multi-lumen balloons, and external beam radiation therapy with low energy X-ray. Nevertheless, the most widely used technique with the longest history and follow-up is interstitial multicatheter brachytherapy [12,13]. In the conventional approach to interstitial multicatheter brachytherapy, the percutaneous catheters are inserted 2-3 weeks after breast surgery, when the resected tissue has already been analyzed and the complete pathological report is available. At our institution, we have proposed an alternative approach to all patients who live far from the treatment center or who are frail: implantation of the catheter during tumor resection to perform perioperative APBI. The objective of this approach is to avoid the need for a second surgical procedure. This approach is also used to treat recurrent disease as a second conservative treatment.
Intraoperative multicatheter implantation delivered with high-dose-rate (HDR) brachytherapy (MC-HDR) provides excellent coverage to the entire tumor bed. In addition, compared to post-operative brachytherapy, the intraoperative approach allows for direct visualization of the tumor bed and, consequently, more accurate placement of the catheters. At our institution, we perform computed tomography (CT) scan 48-72 hours post-operative to minimize the risk of movement or displacement. Published reports on this intraoperative approach are scant, despite the important advantages over post-operative catheter implantation [14]. However, Gurram et al. found no difference in implant quality between intraoperative and post-operative catheter implants, but they recommended the intraoperative technique due to the advantage of direct visualization of the tumor cavity [15].
In this context, the main objectives of the present study were: 1. To describe in detail the intraoperative technique of interstitial multicatheter implantation; and 2. To evaluate the advantages of this approach compared to conventional post-operative catheter insertion and to competing IORT techniques. In addition, we report outcomes and toxicity in a series of 83 patients treated with this technique at our institution.
Material and methods
Between November 2006 and June 2017, 83 patients (59 patients with early-stage primary breast cancer and 24 with recurrent breast cancer) were treated with intraoperative MC-HDR brachytherapy for APBI at the Catalan Institute of Oncology, Barcelona, Spain. We retrospectively analyzed the outcomes of these patients. The study was conducted in accordance with our institutional protocols. Written informed consent was obtained from each patient before starting the procedure.
All patients underwent tumorectomy with a resection margin that included sufficient normal breast tissue to ensure tumor-free margins. Sentinel node biopsy (SNB) was performed in all cases, except for patients with recurrent disease who had undergone axillary lymph node dissection for the primary tumor.
Candidates for APBI were those who met the criteria for APBI [16,17,18], and those patients who refused mastectomy after developing a local recurrence following conservative surgery and adjuvant WBI and thus, were receiving a second treatment. Consequently, eligibility criteria for intraoperative MC-HDR were as follows: unicentric, unifocal tumor with negative margins and negative SNB; breast anatomy suitable for multicatheter implantation; locally-recurrent disease or frail/elderly patients in whom the decision to perform APBI with MC-HDR was made prior to surgery to avoid the risks associated with a second procedure (due to frailty).
Follow-up, consisting of complete clinical examinations, was performed according to the following schedule: initially, at 2 months post-treatment, then every 6 months for the first two years, and annually thereafter. All the patients underwent an annual mammography.
Implant technique and treatment delivery
The tumorectomy was performed under general anesthesia. Six metallic clips were inserted into the tumor bed limits as described by Major et al. [19]. Next, the resected tumor and SNB (if performed) were sent to the laboratory for assessment. After intraoperative pathological confirmation (achieved within 15 minutes after tumor resection in most cases) of the negative sentinel lymph node and negative tumor margins, metallic needles were manually inserted around the open cavity, using a plastic guide template with needle holes to achieve geometric distribution. Previously, all entry and exit points were marked on the skin surface to plan the needle distribution. The needles were spaced to form equilateral triangles of 1.6 cm and inserted in two to four planes, beginning in the inferior plane to ensure sufficient radiation coverage to the deep tumor cavity under direct visualization; applicators in the superior planes were implanted only after closure of the surgical cavity. The needles were then replaced by plastic tubes and attached with buttons at both ends (Figures 1 and 2). The number of applicators and tubes used varied according to the tumor cavity size and breast anatomy.
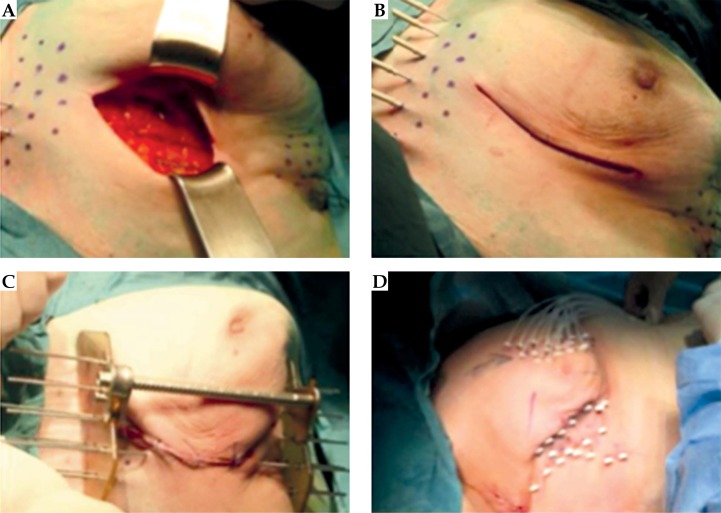
Fig. 1.
A) Needle application ensuring deep tumor bed coverage. B) Needles inserted in the inferior plane and sutured skin. C) Needle implantation in the middle and superior planes with the help of plastic template and metallic bridge. D) Needles replaced with plastic tubes, and button fixation of extremities
Fig. 2.
Needle substitution by plastic tubes in a rescue implant during oncoplastic surgery
A computed tomography (CT) scan with 2 mm slice thickness was performed in the Radiation Oncology Department after the definitive pathologic findings from the surgical specimen were available (usually within 3 to 5 days after surgery). The Oncentra system (Elekta Company, Veenendaal, The Netherlands) was used for treatment planning. The planning target volume (PTV) was defined according to the surgical margins to assure a total margin of 20 mm around the tumor boundaries. In cases in which the PTV overlapped the skin and/or chest wall, a margin of 5 mm was cropped out of these structures [20].
Patients were treated with HDR-BT with a 192Ir source delivered in 2-3 fractions per day, with a minimum of 6 hours separation between fractions. In all cases, brachytherapy started within days after surgery. Patients were offered one of two options: either to remain hospitalized in the Brachytherapy Unit during the entire course of treatment, or to return to the center twice a day to receive treatment.
A modified Paris system was used for dosimetric purposes [21]. The treatment planning parameters were established as follows: at least 90% of the defined PTV was to receive 100% of the prescribed dose (coverage ratio ≥ 0.9); maximum dose to the skin: ≤ 70% of the prescribed dose; D90 > 100%, V150 < 50%, with a dose non-compliance ratio (DNR) < 0.35 (which was achieved in 86% of cases).
All patients who underwent MC-HDR from November 2006 through September 2012, received 10 fractions of 3.4 Gy in accordance with the technique described by Vicini et al. [22]. However, due to the participation of our center in the GEC-ESTRO randomized trial [2], the treatment scheme was changed in October 2012 to 8 fractions of 4 Gy each (the same scheme recommended by the GEC-ESTRO randomized phase III trial). Therefore, the fractionation schedule varied slightly among the study sample. Nevertheless, the equivalent total dose in 2 fractions (EQD2), with a tumor α/β ratio value of 4, was similar in both schemes (41.93 Gy and 42.67 Gy, respectively), with a biological effective dose (BED) of 62.9 Gy and 64 Gy, respectively.
In the present report, we describe not only the technical data for the procedure, but also treatment outcomes in terms of overall survival (OS), disease-free survival (DFS), local control, cosmesis, and the toxicity profile for all patients (both primary breast cancer and local recurrence).
Results
Eighty-four patients underwent intraoperative interstitial multicatheter implant followed by HDR brachytherapy within 2-3 days after implantation. In one case, the intraoperative biopsy revealed a positive SNB and consequently, definitive intraoperative brachytherapy was abandoned; instead, the intraoperative implant was converted to a boost to the tumor bed (3 fractions of 5 Gy), and the patient received conventional post-operative WBI 2-3 weeks after surgery. That patient was excluded from the final analysis. Therefore, our retrospective analysis included the remaining 83 patients.
Median follow-up was 40 months (range, 1-136). Median age was 82 years (range, 44-92) and 71.1 % of patients (59/83 patients) were ≥ 70 years. Relevant demographic and tumor characteristics are provided in Table 1.
Table 1.
Patient demographic and tumor characteristics
| Parameter | n (%) |
|---|---|
| Age (years) | |
| Median | 82 |
| Range | 44-92 |
| 44-59 | 10 |
| 60-69 | 15 |
| >70 | 59 |
| T stage | |
| pTis | 6 (7.2) |
| pT1 | 28 (33.7) |
| pT2 | 25 (30.2) |
| Local relapse | 24 (28.9) |
| N stage | |
| pN0 (sn) | 81 (97.6) |
| pN1mi (sn) | 2 (2.4) |
| Histological subtype | |
| Ductal invasive | 65 (78.4) |
| Carcinoma in situ | 7 (8.4) |
| Mucinous invasive | 5 (6) |
| Papilar invasive | 4 (4.8) |
| Lobular invasive | 1 (1.2) |
| Mixed infiltrating ductal-lobular | 1 (1.2) |
| Intrinsic subtype | |
| Luminal A | 38 (45.7) |
| Luminal B | 15 (18.2) |
| ErB2 overexpression | 4 (4.8) |
| “Basal like” | 2 (2.4) |
| Grading | |
| 1 | 26 (31.3) |
| 2 | 34 (40.9) |
| 3 | 12 (14.4) |
| Unknow | 11 (13.4) |
Fifty-nine patients (71.1%) had a diagnosis of primary breast cancer, and 24 (28.9%) had a locally recurrent disease after previous treatment with WBI to the same breast.
Most patients (65/83 patients, 78.3%) had infiltrating ductal carcinoma (Table 1). Of the 59 patients with primary breast cancer, 28 were classified as stage I, 25 as stage II, and 6 with stage Tis. 40.9% of patients had a grade 2 tumor, while 64.4% had luminal A disease. Tumor margins were ≥ 1 mm in all but one patient, who had a microscopically positive chest wall margin, considered unsuitable for margin expansion. We inserted a median of 17 tubes. In almost all cases (73/83 patients, 88%), 3 catheter planes were used. Sixty patients (72.3%) were treated according to the revised GEC-ESTRO treatment schedule (32 Gy in 8 treatment fractions), while 23 patients (27.7%) were treated with the original schedule (34 Gy in 10 fractions).
The mean V100 was 154 cm3, with a median of 161.25 cm3 (range, 54-295.4 cm3). Mean V150 was 46 cm3 and median V150 was 49 cm3 (range, 23.5-94.6 cm3). Treatment characteristics and parameters of the dosimetric analysis are provided in Table 2.
Table 2.
Treatment characteristics and dosimetric analysis
| Doses and fractionation | 34 Gy/10 Fr 32 Gy/8 Fr |
n = 23 (27.7%) n = 60 (72.3%) |
| No of catheter plans | Median | 3 |
| Range | 1-4 | |
| No of catheters | Median | 17 |
| Range | 9-18 | |
| Mean volume | V100 | 154 cm3 |
| V150 | 46 cm3 | |
| Median volume | V100 | 161.25 cm3 |
| V150 | 49 cm3 | |
| Minimum volume | V100 | 54 cm3 |
| V150 | 23.5 cm3 | |
| Maximum volume | V100 | 295.4 cm3 |
| V150 | 94.6 cm3 | |
| PTV volume | Mean | 130 cm3 |
| Range | 73-232.5 cm3 |
V100, V150 – volume of the anatomic volume receiving 100%, 150% of the prescribed dose, PTV – planning target volume
Disease control
The three-year OS in the whole sample (both primary cancer and local recurrence groups) was 95%. Notably, none of the five deaths were attributed to breast cancer, and no evidence of relapse was observed in any of those cases. The 3-year DFS rate for the whole sample was 97%, and no local failures were recorded.
The 3-year OS and DFS rates in the recurrent and primary cancer groups, respectively, were as follows: OS – 87% vs. 89%, and DFS – 96% vs. 97.8%.
Among the 24 patients treated for local recurrence, one was diagnosed with contralateral breast cancer four years after treatment, two (8.3%) experienced a second relapse (not local), and one presented positive regional lymph nodes and bone metastasis on a PET-CT scan performed one month after brachytherapy treatment, suggesting that the patient had been understaged at the time of surgery. The other recurrence occurred in a patient who presented with bone metastases 10.5 years after APBI (21 years after primary breast cancer diagnosis).
Toxicity and cosmetic outcomes
Of the 59 patients treated for primary breast cancer, acute toxicity (infectious mastitis) was observed in one patient (1.6%). Based on that case, we now routinely administer antibiotic therapy for all intraoperative approaches. Of the 24 patients treated for local recurrence, eight developed acute toxicity. Of these, 7 (31.9%) were infectious mastitis and 1 (4.3%) hematoma.
Six patients did not reach the minimum follow-up of 6 months to evaluate late toxicity; therefore, late toxicity was evaluated only in 77 patients (55 patients in the primary breast cancer group and 22 patients in the recurrence group). In the primary breast cancer group (n = 55), late toxicities were as follows: fibrosis ≥ G3 in 3 patients (5.6%), mastitis in 3 cases (5.5%), and hypochromic skin spots at the catheter entrance and exit points in 8 patients (14.8%). Late toxicities in the local recurrence group (n = 22) were as follows: fibrosis ≥ G3 in 15 patients (68%), mastitis in 6 cases (27.3%), and hypochromic skin spots at the catheter entrance and exit points in 8 patients (36.4%). Tables 3 and 4 provide the acute and late toxicity profile for both groups.
Table 3.
Toxicity profile: patients treated for primary breast tumor
| Percentage of patients | |
|---|---|
| Acute toxicity (59 patients) | |
| Infectious mastitis | 1.6 (n = 1) |
| Hematoma | 0 (n = 0) |
| Late toxicity (55 patients) | |
| Fibrosis G0-G2 | 94.4 (n = 52) |
| Fibrosis G3 | 5.6 (n = 3) |
| Fibrosis G4 | 0 (n = 0) |
| Mastitis | 5.5 (n = 3) |
| Hypochromic skin spots | 14.8 (n = 8) |
| Skin hyperpigmentation | 7.4 (n = 4) |
| Telangiectasia | 1.9 (n = 1) |
| Fat necrosis | 0 (n = 0) |
Table 4.
Toxicity profile: patients treated for breast local recurrence
| Percentage of patients | |
|---|---|
| Acute toxicity (23 patients) | |
| Infectious mastitis | 30.4 (n = 7) |
| Hematoma | 4.3 (n = 1) |
| Late toxicity (22 patients) | |
| Fibrosis G0-G2 | 31.9 (n = 7) |
| Fibrosis G3 | 50 (n = 11) |
| Fibrosis G4 | 18.1 (n = 4) |
| Mastitis | 27.3 (n = 6) |
| Hypochromic skin spots | 36.4 (n = 8) |
| Skin hyperpigmentation | 13.6 (n = 3) |
| Telangiectasia | 31.8 (n = 7) |
| Fat necrosis | 4.5 (n = 1) |
Cosmetic outcomes, determined according to on the 4-point Harvard breast cosmesis scale [23] were as follows: in the primary breast cancer group: excellent (6 patients, 11.1%), good (49 patients, 63%), fair (1 patient, 1.8%), and poor (0 patients); in 2 cases (4.9%), no cosmetic ratings were available. Cosmetic outcomes in the local recurrence group were: good (49 patients, 63%), fair (6 patients, 27.3%), and poor (7 patients, 32%); in 4 cases (7%), no cosmetic ratings were available. In the local recurrence group, no data were available regarding the cosmetic outcomes after primary treatment.
Discussion
In recent years, the body of evidence from randomized clinical trials supporting the use of APBI versus WBI has increased substantially. Consequently, APBI is currently an accepted alternative to WBI in selected patients [7,18], because it offers comparable survival rates, better cosmesis, and a less burdensome treatment [2,24,25,26]. In addition, recent analyses by Shah and Lanni have demonstrated that brachytherapy-based APBI reduces overall financial cost of treatment [27,28].
The present study provides a detailed description of the intraoperative approach to interstitial multicatheter implantation. We also provide outcomes and toxicity in a series of 83 patients treated with this approach, with results that are comparable to WBI in terms of low toxicity and excellent survival rates. Although five patient deaths occurred during the follow-up, the causes (i.e. for cardiovascular or pulmonary diseases) were unrelated to breast cancer or treatment. Notably, no cases of local relapse were observed. These findings support the effectiveness of intraoperative MC-HDR brachytherapy for APBI in the treatment of both locally recurrent and early-stage breast cancer.
The intraoperative implantation of multicatheters offers many advantages. First, it avoids the need for a second surgical intervention and the risks related. In addition, this procedure allows for direct visualization both operating bed and the implant site and, consequently, a more accurate placement. In addition, of the various APBI techniques, multicatheter interstitial BT has the longest track record, and two randomized phases 3 trials have demonstrated that it is comparable to WBI [2,29]. Another advantage of APBI is reduced treatment time versus WBI, which requires from 3 to 6 weeks of daily sessions, being inconvenient particularly for the elderly and for patients with mobility problems, or those who live far from the radiation therapy facility [30]. By contrast, not only does APBI reduce treatment time, but it guarantees excellent coverage of the tumor bed and decreases radiation doses to nearby organs and structures such as the lungs, heart, and ribs [31].
Interest in the use of IORT for APBI has increased in the last 10-15 years, with the emergence of techniques such as MammoSite balloon brachytherapy, Intrabeam IORT, and electron IORT [10]. Although these techniques have been embraced by many clinicians, their appearance has also resulted in important controversies due to the lack of a definitive pathological diagnosis before irradiation, and to the impossibility of ensuring complete coverage of the tumor bed and margins [32,33]. In this sense, conventional (i.e. post-operative) multicatheter brachytherapy offers an excellent alternative to both WBI and IORT, because it does not suffer from the aforementioned disadvantages.
Recently, Strnad et al. [2] reported results from the GEC-ESTRO phase 3 APBI trial that assessed APBI administered via exclusive multicatheter brachytherapy. The results demonstrated that this technique after breast-conserving surgery was as effective as adjuvant WBI in carefully selected, early-stage breast cancer patients, and that multicatheter brachytherapy for APBI was not inferior to WBI – in contrast to the results reported in the ELIOT and TARGIT trials, both of which failed to prove the non-inferiority of IORT to WBI [10,34].
The insertion of the catheters intraoperatively rather than post-operatively is what differentiates the technique described in the present article from the technique used in the GEC-ESTRO study. Theoretically, intraoperative implantation should provide a small advantage in terms of local control and toxicity due to better accuracy of the catheter placement offered by direct visualization of the operating bed. Moreover, as with conventional post-operative multicatheter brachytherapy, intraoperative MC-HDR avoids the drawbacks of other IORT techniques, which use instruments with a spherical applicator that do not conform the surgical cavity, thus leading to incomplete coverage. By contrast, intraoperative MC-HDR allows a precise implantation and irradiation around the tumor bed at 1-1.5 cm, providing excellent coverage of the entire tumor bed and margins. As our results show, at least 90% of the defined PTV received 100% of the prescribed dose (coverage index ≥ 0.9). PTV underdosing areas were only accepted to meet dose constraints of the skin and chest wall.
Another benefit of intraoperative MC-HDR is that treatment planning and radiotherapy delivery are performed only few days after surgery when the final pathological diagnosis becomes available, an approach that bridges the gap between other IORT techniques, in which the patient is irradiated before definitive pathological assessment.
Notwithstanding the long history and proven efficacy of interstitial multicatheter brachytherapy in APBI, only a few reports have described the intraoperative MC-HDR technique [14,35]. Sato et al. [14] provided in-depth description of this approach in a study conducted to assess the feasibility and safety of catheter insertion during tumorectomy. In that study, the authors report good tumor control with low toxicity rates in 157 patients who underwent intraoperative multicatheter implantation followed by HDR brachytherapy.
In the setting of local recurrent breast cancer, multicatheter interstitial brachytherapy after salvage tumorectomy has been shown to achieve good disease control. A multicentric retrospective study conducted by Hannoun-Levi as a part of the GEC-ESTRO breast cancer group [35], assessed 217 patients with locally recurrent breast cancer, many of whom (precise data not provided) underwent intraoperative catheter implantation. In that study, which included patients with unifocal tumors (any histological type) ≤ 35 mm in size, a maximum of 3 positive regional lymph nodes and no distant metastasis; five-year OS and local recurrence rates were 88.7% and 5.6%, respectively. Breast cosmesis was considered excellent or good in 85% of cases.
In our series, data on cosmetic outcomes and fibrosis were slightly worse than those reported in other studies. These results can be explained by the fact that the patients who showed the greatest toxicity were those treated for recurrence, who had already undergone surgery and adjuvant WBI, and thus had a greater risk of developing toxicity. By contrast, cosmesis in the patients treated for primary disease was either good or excellent in most cases. Although cosmesis was considered satisfactory in most of the patients who underwent APBI due to locally recurrent disease, our results suggest that patients with locally recurrent disease should be informed that cosmetic outcomes may be less than optimal. Nevertheless, patients (and clinicians) may consider this to be an acceptable trade-off given the good survival rates achieved with this treatment approach, especially given that the only alternative is mastectomy (with or without reconstructive surgery).
Importantly, we observed no local recurrences in our series, a finding that underscores the excellent tumor control achieved with this technique. However, given the relatively short follow-up in our series (median, 40 months), some recurrences may occur in the future. Indeed, Aristei et al. [36] recently reported long-term results of intra- and peri-operative interstitial multicatheter HDR implants for APBI. In that study, they described that although the rate for local relapses was quite low (1.8%) at 5 years, it went up to 6.6% at 10 years. That is one of the reasons why patients must be followed up for at least 10 years – not only to rule out local relapse, but also to evaluate accurately the incidence of secondary effects.
Toxicity rates in our sample were low in both groups. Although several cases of acute and chronic mastitis were observed, these were successfully managed with supportive therapy without the need of additional surgery. One option to further reduce the complication rate could be to decrease the V150. However, it is important to keep in mind that because APBI is only a partial breast treatment, the PTV should be well-covered. In addition, it is necessary to consider interobserver variations in the CTV definition, as demonstrated by Upreti et al. [37], especially when the cavity visualization index is low.
Study limitations
The main limitations of this study were its retrospective design, small sample size, and relatively short follow-up. Furthermore, we included patients with primary and recurrent tumors, which could be considered two different biologic diseases. This is why survival and toxicity data were analyzed separately in two groups. Another limitation is that the treatment scheme was not homogenous among all patients because we modified our treatment schedule during the study period, with just over half receiving 32 Gy (8 fractions) versus 34 Gy (10 fractions). Finally, it is also important to emphasize the complexity of this technique, which requires a high level of operator experience. For this reason, we believe this technique should only be performed in reference centers.
Conclusions
The present study provides a comprehensive description of the indications for intraoperative insertion of catheters for APBI. APBI using intraoperative interstitial multicatheter HDR, allows good tumor control in carefully selected patients; disease control rates are comparable to WBI, with low toxicity profile. Survival and local control rates are also good even in patients who undergoing salvage tumorectomy for local recurrence. However, in this patient subgroup, cosmesis may not be absolutely satisfactory, although the only alternative is mastectomy.
Among the various techniques for intraoperative APBI, we believe that interstitial multicatheter implantation merits more attention given its excellent theoretical and practical advantages over competing approaches. Intraoperative catheter insertion has the advantage of a greater accuracy in target implantation, a shortened interval between surgery and radiotherapy, and the avoidance of a second invasive procedure. This treatment modality may be especially suitable for elderly or frail patients with early-stage disease and for patients with locally recurrent breast cancer.
Disclosure
The authors report no conflict of interest.
References
- 1.Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366:2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 2.Strnad V, Ott OJ, Hildebrandt G, et al. 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet. 2016;387:229–238. doi: 10.1016/S0140-6736(15)00471-7. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–1241. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 4.Wickberg A, Holmberg L, Adami HO, et al. Sector resection with or without postoperative radiotherapy for stage I breast cancer: five-year results of a randomized trial. Uppsala-Orebro Breast Cancer Study Group. J Natl Cancer Inst. 1994;86:717–722. doi: 10.1093/jnci/86.9.717. [DOI] [PubMed] [Google Scholar]
- 5.Veronesi U, Marubini E, Mariani L, et al. Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol. 2001;12:997–1003. doi: 10.1023/a:1011136326943. [DOI] [PubMed] [Google Scholar]
- 6.Bitter SM, Heffron-Cartwright P, Wennerstrom C, et al. WBRT vs. APBI: an interim report of patient satisfaction and outcomes. J Contemp Brachytherapy. 2016;8:17–22. doi: 10.5114/jcb.2016.57816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Skowronek J, Wawrzyniak-Hojczyk M, Ambrochowicz K. Brachytherapy in accelerated partial breast irradiation (APBI) – review of treatment methods. J Contemp Brachytherapy. 2012;4:152–164. doi: 10.5114/jcb.2012.30682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harat A, Harat M, Makarewicz R. Whole breast irradiation vs. APBI using multicatheter brachytherapy in early breast cancer – simulation of treatment costs based on phase 3 trial data. J Contemp Brachytherapy. 2016;8:505–551. doi: 10.5114/jcb.2016.64919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Njeh CF, Saunders MW, Langton CM. Accelerated Partial Breast Irradiation (APBI): A review of available techniques. Radiat Oncol. 2010;5:90. doi: 10.1186/1748-717X-5-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Esposito E, Anninga B, Harris S, et al. Intraoperative radiotherapy in early breast cancer. Br J Surg. 2015;102:599–610. doi: 10.1002/bjs.9781. [DOI] [PubMed] [Google Scholar]
- 11.Williams NR, Pigott KH, Brew-Graves C, et al. Intraoperative radiotherapy for breast cancer. Gland Surg. 2014;3:109–119. doi: 10.3978/j.issn.2227-684X.2014.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamrava M, Kuske RR, Anderson B, et al. Outcomes of breast cancer patients treated with accelerated partial breast irradiation via multicatheter interstitial brachytherapy: The Pooled Registry of Multicatheter Interstitial Sites (PROMIS) Experience. Ann Surg Oncol. 2015;22(Suppl 3):S404–S411. doi: 10.1245/s10434-015-4563-7. [DOI] [PubMed] [Google Scholar]
- 13.Gabani P, Cyr AE, Zoberi JE, et al. Long-term outcomes of APBI via multicatheter interstitial HDR brachytherapy: Results of a prospective single-institutional registry. Brachytherapy. 2018;17:171–180. doi: 10.1016/j.brachy.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Sato K, Mizuno Y, Kato M, et al. Intraoperative Open-Cavity Implant for Accelerated Partial Breast Irradiation Using High-Dose Rate Multicatheter Brachytherapy in Japanese Breast Cancer Patients: A Single-Institution Registry Study. JCT. 2012;3:822–830. [Google Scholar]
- 15.Gurram L, Wadasadawala T, Joshi K, et al. Multi-catheter interstitial brachytherapy for partial breast irradiation: an audit of implant quality based on dosimetric evaluation comparing intra-operative versus post-operative placement. J Contemp Brachytherapy. 2016;8:116–121. doi: 10.5114/jcb.2016.59195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith BD, Arthur DW, Buchholz TA, et al. Accelerated Partial Breast Irradiation Consensus Statement from the American Society for Radiation Oncology (ASTRO) Int J Radiat Oncol Biol Phys. 2009;74:987–1001. doi: 10.1016/j.ijrobp.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 17.Polgár C, van Limbergen E, Pötter R, et al. Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: Recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group. Radiother Oncol. 2010;94:264–273. doi: 10.1016/j.radonc.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Shah Ch, Wobb J, Manyam B, et al. Accelerated partial breast irradiation utilizing brachytherapy: patient selection and workflow. J Contemp Brachytherapy. 2016;8:90–94. doi: 10.5114/jcb.2016.58083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Major T, Gutiérrez C, Guix B, et al. Recommendations from GEC ESTRO Breast Cancer Working Group (II): Target definition and target delineation for accelerated or boost partial breast irradiation using multicatheter interstitial brachytherapy after breast conserving open cavity surgery. Radiother Oncol. 2016;118:199–192. doi: 10.1016/j.radonc.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Strnad V, Hannoun-Levi JM, Guinot JL, et al. Recommendations from GEC ESTRO Breast Cancer Working Group (I): Target definition and target delineation for accelerated or boost Partial Breast Irradiation using multicatheter interstitial brachytherapy after breast conserving closed cavity surgery. Radiother Oncol. 2015;115:342–348. doi: 10.1016/j.radonc.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Strnad V, Potter R, Kovacs G. Practical Handbook of Brachytherapy. Bremen: UNI-MED, Verlag AG; 2014. [Google Scholar]
- 22.Vicini F, Beitsch PD, Quiet CA, et al. Three-year analysis of treatment efficacy, cosmesis, and toxicity by the American Society of Breast Surgeons MammoSite Breast Brachytherapy Registry Trial in patients treated with accelerated partial breast irradiation (APBI) Cancer. 2008;112:758–766. doi: 10.1002/cncr.23227. [DOI] [PubMed] [Google Scholar]
- 23.Vrieling C, Collette L, Bartelink E, et al. Validation of the methods of cosmetic assessment after breast-conserving therapy in the EORTC “boost versus no boost” trial. Int J Radiat Oncol Biol Phys. 1999;45:667–676. doi: 10.1016/s0360-3016(99)00215-1. [DOI] [PubMed] [Google Scholar]
- 24.Kuske RR, Winter K, Arthur DW, et al. Phase II trial of brachytherapy alone after lumpectomy for select breast cancer: toxicity analysis of RTOG 95-17. Int J Radiat Oncol Biol Phys. 2006;65:45–51. doi: 10.1016/j.ijrobp.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 25.Polgár C, Fodor J, Major T, et al. Breast-conserving treatment with partial or whole breast irradiation for low-risk invasive breast carcinoma – 5-year results of a randomized Trial. Int J Radiat Oncol Biol Phys. 2007;69:694–702. doi: 10.1016/j.ijrobp.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 26.Antonucci JV, Wallace M, Goldstein NS, et al. Differences in patterns of failure in patients treated with accelerated partial breast irradiation versus whole-breast irradiation: a matched-pair analysis with 10-year follow-up. Int J Radiat Oncol Biol Phys. 2009;74:447–452. doi: 10.1016/j.ijrobp.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 27.Lanni T, Keisch M, Shah C, et al. A cost comparison analysis of adjuvant radiation therapy techniques after breast-conserving surgery. Int J Radiat Oncol Biol Phys. 2013;19:162–167. doi: 10.1111/tbj.12075. [DOI] [PubMed] [Google Scholar]
- 28.Shah C, Lanni TB, Saini H, et al. Cost-efficacy of acceleration partial-breast irradiation compared with whole-breast irradiation. Breast Cancer Res Treat. 2013;138:127–135. doi: 10.1007/s10549-013-2412-6. [DOI] [PubMed] [Google Scholar]
- 29.Polgár C, Major T, Fodor J, et al. Accelerated partial-breast irradiation using high-dose-rate interstitial brachytherapy: 12-year update of a prospective clinical study. Radiother Oncol. 2010;94:274–279. doi: 10.1016/j.radonc.2010.01.019. [DOI] [PubMed] [Google Scholar]
- 30.Dragun AE, Huang B, Tucker TC, et al. Disparities in the application of adjuvant radiotherapy after breast-conserving surgery for early stage breast cancer. Cancer. 2010;117:2590–2598. doi: 10.1002/cncr.25821. [DOI] [PubMed] [Google Scholar]
- 31.Lettmaier S, Kreppner S, Lotter M, et al. Radiation exposure of the heart, lung and skin by radiation therapy for breast cancer: A dosimetric comparison between partial breast irradiation using multicatheter brachytherapy and whole breast teletherapy. Radiother Oncol. 2011;100:189–194. doi: 10.1016/j.radonc.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Vaidya JS, Wenz F, Bulsara M, et al. Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet. 2014;383:603–613. doi: 10.1016/S0140-6736(13)61950-9. [DOI] [PubMed] [Google Scholar]
- 33.Mackenzie P, Fyles A, Chung C. Radiotherapy for breast cancer, the TARGIT-A trial. Lancet. 2014;383:1717. doi: 10.1016/S0140-6736(14)60827-8. [DOI] [PubMed] [Google Scholar]
- 34.Shah C, Badiyan S, Khwaja S, et al. Evaluating radiotherapy options in breast cancer: does intraoperative radiotherapy represent the most cost-efficacious option? Clin Breast Cancer. 2014;14:141–146. doi: 10.1016/j.clbc.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 35.Hannoun-Levi JM, Resch A, Gal J, et al. Accelerated partial breast irradiation with interstitial brachytherapy as second conservative treatment for ipsilateral breast tumour recurrence: Multicentric study of the GEC-ESTRO Breast Cancer Working Group. Radiother Oncol. 2013;108:226–231. doi: 10.1016/j.radonc.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 36.Aristei C, Maranzano E, Lancellotta V, et al. Partial breast irradiation with interstitial multi-catheter high-dose-rate brachytherapy. Long term results of phase II prospective study. Radiother Oncol. 2017;124:208–213. doi: 10.1016/j.radonc.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 37.Upreti RR, Budrukkar A, Wadasadawala T, et al. Interobserver variations of target volume delineation and its impact on irradiated volume in accelerated partial breast irradiation with intraoperative interstitial breast implant. J Contemp Brachytherapy. 2017;9:139–145. doi: 10.5114/jcb.2017.66027. [DOI] [PMC free article] [PubMed] [Google Scholar]