Abstract
Coronary artery aneurysms (CAAs) are relatively rare with an incidence varying from 1.4% to 5.3% of patients undergoing coronary angiography. Studies suggest that management of CAA can be guided by the absence or presence of significant coronary artery stenosis, with most concluding that CAA associated with stenosis of ≥70% should be managed surgically or with percutaneous intervention. However, given the paucity of cases described in the literature and lack of randomised control trials, no consensus exists on the natural history, prognosis or management of CAAs without significant concomitant stenosis. We present a case of medically managed atherosclerotic CAA without significant stenosis that was found to no longer be present on coronary angiography performed 11 years after initial diagnosis.
Keywords: interventional cardiology, cardiovascular medicine
Background
Coronary artery aneurysms (CAAs) are a relatively uncommon phenomenon predominantly caused by atherosclerotic disease. The majority of CAAs exist in vessels with significant coronary stenosis and, in this population, treatment with percutaneous intervention (PCI) or surgery is warranted. However, no consensus exists regarding ideal management of CAAs without concomitant stenosis although most studies agree that management should include antiplatelets with or without anticoagulants and optimisation of cardiac risk factors.
Case presentation
A 54-year-old male smoker with no significant medical history or other cardiac risk factors presented with chest pain in 2006. He was found to have a troponin rise with no ECG changes and was diagnosed with a non-ST elevation myocardial infarction (MI). A coronary angiogram was performed which revealed a CAA in the proximal to mid-left anterior descending (LAD) coronary artery measuring approximately 1.1 cm in diameter with 20% associated stenosis (figure 1). Diffuse irregularities were noted throughout the coronary arteries with no significant obstructive coronary artery disease. History and investigations were not suggestive of systemic vasculitis; therefore, the aetiology of the CAA was presumed to be atherosclerosis. Given the size of the CAA and lack of significant associated stenosis, the CAA was medically managed. He was given aspirin, clopidogrel, metoprolol, atorvastatin and ramipril.
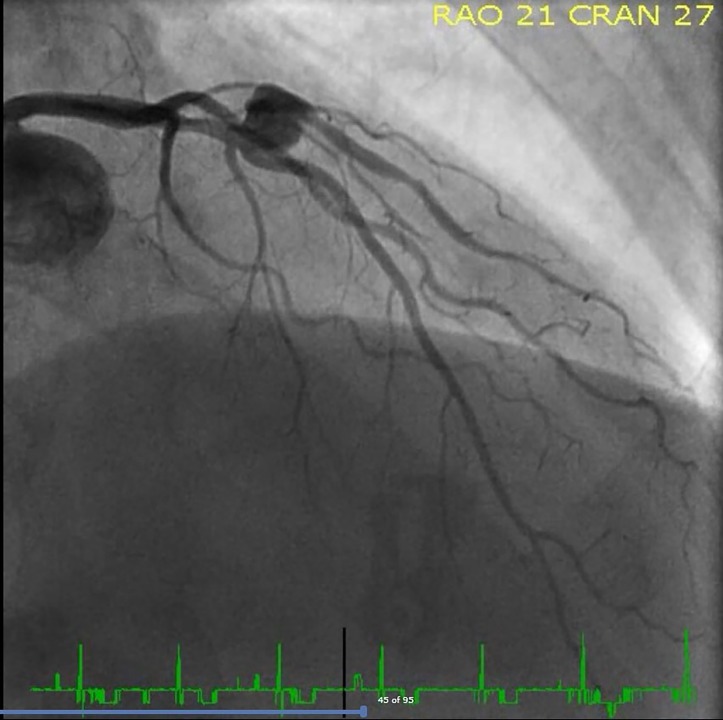
Figure 1.
2006 angiogram appearance of LAD CAA. CAA, coronary artery aneurysm; LAD, left anterior descending.
Outcome and follow-up
The patient remained stable and asymptomatic until March 2009 when he presented with a further episode of chest pain at rest and associated shortness of breath. He was Troponin-I negative with no ECG changes. Another coronary angiogram was performed at this time revealing a stable aneurysm (figure 2) with diffuse irregularities throughout the coronary arteries. Once more, the decision was made for ongoing medical therapy and observation.
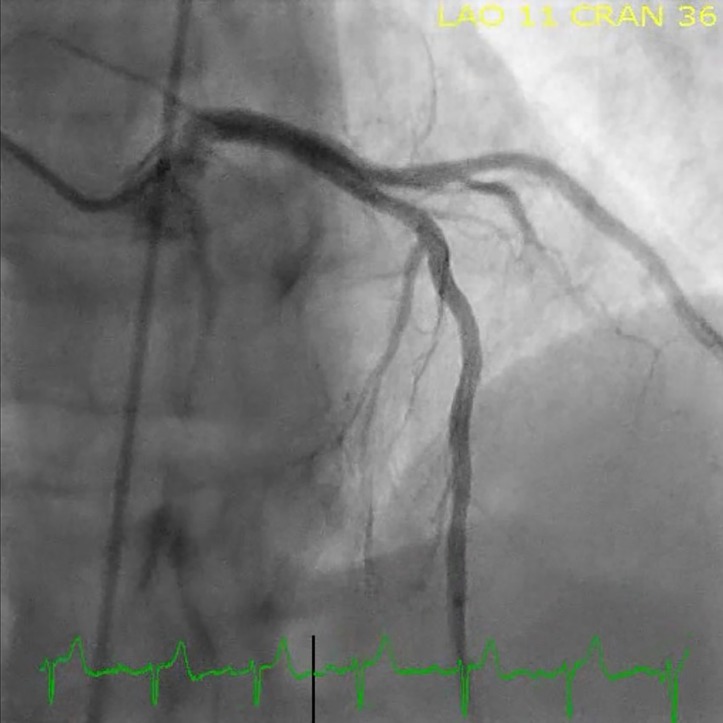
Figure 2.
2009 angiogram appearance of LAD CAA. CAA, coronary artery aneurysm; LAD, left anterior descending.
The patient remained asymptomatic until March 2017 when he began experiencing shortness of breath and mild chest pains. An echocardiogram was performed and showed a normal left ventricle size and systolic function (EF 67%), with no significant valvular disease. Coronary angiography at this time showed the previously described aneurysm in the LAD was no longer present (figure 3), with no appreciable stenosis around the area where the aneurysm had been present. We presume the aneurysm had thrombosed over time. Of note, a small proximal diagonal branch adjacent to the prior location of the aneurysm was no longer seen.
Figure 3.
LAD in 2017 without CAA. CAA, coronary artery aneurysm; LAD, left anterior descending.
Discussion
CAA is defined as a localised dilation with a diameter more than 50% of adjacent segments.1 Atherosclerosis is the most common cause of CAA in adults with other causes including Kawasaki disease, congenital malformations, trauma, infection, autoimmune conditions, dissection and angioplasty.2 Patients who are found to have CAA on catheterisation usually present with chest pain suggestive of angina, positive exercise stress tests or evidence of previous MI.2
The majority of CAAs exist in vessels with significant coronary stenosis (≥70% stenosis).3 Treatment modalities include medical management, PCI or surgery, with most studies agreeing that CAA associated with significant stenosis should be managed with PCI or surgery.1 3 CAA without severe occlusive disease is particularly rare and there is no consensus on the most appropriate treatment for these patients.
The majority of studies including patients with CAA without associated significant stenosis focus on comparing treatment modalities and have found that medical management is more appropriate than surgical or PCI therapy. Medical management of CAA generally involves cardiac risk factor optimisation and use of antiplatelets with or without anticoagulants to reduce the risk of serious complications of CAA including thrombosis, rupture and distal embolisation.4 Surgical therapy usually includes coronary artery bypass grafting (CABG) with or without aneurysmal ligation or excision. Patients with CAA who have surgery tend to have good outcomes; however, the need for surgery in patients without concomitant artery stenosis is unclear.4 5
Analysis of the Coronary Artery Surgery Study (CASS) registry, comprising of 20 087 patients who had coronary artery angiography, found no difference in 5-year follow-up for MI and survival rates in patients with non-significant coronary artery stenosis and medically treated CAA compared with patients with non-significant coronary stenosis without CAA.6 Further, when comparing outcomes after CABG, several investigators found no difference in short-term survival in patients who had significant stenosis (≥70%) versus those who also had significant stenosis and concomitant CAA. These results suggest that surgical therapy should be indicated only for those patients who have significant stenosis independent of their aneurysmal status.2 3 6–8
However, another retrospective analysis of 3900 patients referred for coronary angiography found that of those with CAA without significant coronary stenosis, 38.7% had a history of previous MI; the infarct in all cases was related to the aneurysmal artery.2While this was markedly lower than rates of previous MI in patients with significant obstructive disease alone (64.2%) and in patients with significant obstructive disease and CAA (61.6%), the measurable incidence of MI suggests medical therapy and optimisation of cardiac risk factors is warranted.2 Thirty-one patients with CAA in this study did not have significant stenosis and all were medically managed with most receiving antiplatelets, beta blockers and nitrates. Two-year follow-up of these patients found a favourable prognosis with zero patients having MI, sudden cardiac death or requiring surgery or PCI suggesting medical management is appropriate treatment.2
The progression of CAA without significant stenosis has not been well defined; the large studies highlighted previous have compared treatment outcomes in these patients rather than examining the natural course of the pathology. Our case contributes to the evidence that, in the absence of significant stenosis, medical therapy with cardiac risk factor optimisation, antiplatelets and/or anticoagulants may be the most appropriate choice for CAA. The case highlights that over a long follow-up period (11 years), the natural course of a CAA may result in thrombosis of the CAA without causing significant acute or chronic obstruction of the coronary artery.
Learning points.
A coronary artery aneurysm (CAA) is defined as a localised dilation with a diameter more than 50% of adjacent segments.
The majority of CAAs exist in vessels with significant coronary stenosis (≥70% stenosis).
CAAs can cause serious complications including thrombosis, rupture and distal embolisation.
We present a case of CAA without concomitant coronary stenosis resolving with medical management.
Medical management of CAA, comprising cardiac risk factor optimisation and use of antiplatelet or anticoagulant therapy, should be considered in place of surgical management for CAA without concomitant coronary stenosis.
Footnotes
Contributors: RR prepared the draft with important contributions from MN. Final submission approved by both authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Syed M, Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis 1997;40:77–84. 10.1016/S0033-0620(97)80024-2 [DOI] [PubMed] [Google Scholar]
- 2. Demopoulos VP, Olympios CD, Fakiolas CN, et al. The natural history of aneurysmal coronary artery disease. Heart 1997;78:136–41. 10.1136/hrt.78.2.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bricker DL, Rittmann DV. Arteriosclerotic aneurysms of the coronary arteries: surgical treatment. Tex Heart Inst J 1987;14:23–30. [PMC free article] [PubMed] [Google Scholar]
- 4. Rath S, Har-Zahav Y, Battler A, et al. Fate of nonobstructive aneurysmatic coronary artery disease: angiographic and clinical follow-up report. Am Heart J 1985;109:785–91. 10.1016/0002-8703(85)90639-8 [DOI] [PubMed] [Google Scholar]
- 5. Baman TS, Cole JH, Devireddy CM, et al. Risk factors and outcomes in patients with coronary artery aneurysms. Am J Cardiol 2004;93:1549–51. 10.1016/j.amjcard.2004.03.011 [DOI] [PubMed] [Google Scholar]
- 6. Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation 1983;67:134–8. 10.1161/01.CIR.67.1.134 [DOI] [PubMed] [Google Scholar]
- 7. Aintablian A, Hamby RI, Hoffman I, et al. Coronary ectasia: incidence and results of coronary bypass surgery. Am Heart J 1978;96:309–15. 10.1016/0002-8703(78)90041-8 [DOI] [PubMed] [Google Scholar]
- 8. Hartnell GG, Parnell BM, Pridie RB. Coronary artery ectasia. Its prevalence and clinical significance in 4993 patients. Br Heart J 1985;54:392–5. 10.1136/hrt.54.4.392 [DOI] [PMC free article] [PubMed] [Google Scholar]